Abstract
Background
The magnitude of the negative energy balance induced by exercise may be reduced due to compensatory increases in energy intake.
Objective
To address the question: Does increased exercise or physical activity alter ad-libitum daily energy intake or macronutrient composition in healthy adults?
Data Sources
PubMed and Embase were searched (January 1990–January 2013) for studies that presented data on energy and/or macronutrient intake by level of exercise, physical activity or change in response to exercise. Ninety-nine articles (103 studies) were included.
Study Eligibility Criteria
Primary source articles published in English in peer-reviewed journals. Articles that presented data on energy and/or macronutrient intake by level of exercise or physical activity or changes in energy or macronutrient intake in response to acute exercise or exercise training in healthy (non-athlete) adults (mean age 18–64 years).
Study Appraisal and Synthesis Methods
Articles were grouped by study design: cross-sectional, acute/short term, non-randomized, and randomized trials. Considerable heterogeneity existed within study groups for several important study parameters, therefore a meta-analysis was considered inappropriate. Results were synthesized and presented by study design.
Results
No effect of physical activity, exercise or exercise training on energy intake was shown in 59% of cross-sectional studies (n = 17), 69% of acute (n = 40), 50% of short-term (n = 10), 92% of non-randomized (n = 12) and 75% of randomized trials (n = 24). Ninety-four percent of acute, 57% of short-term, 100% of non-randomized and 74% of randomized trials found no effect of exercise on macronutrient intake. Forty-six percent of cross-sectional trials found lower fat intake with increased physical activity.
Limitations
The literature is limited by the lack of adequately powered trials of sufficient duration, which have prescribed and measured exercise energy expenditure, or employed adequate assessment methods for energy and macronutrient intake.
Conclusions
We found no consistent evidence that increased physical activity or exercise effects energy or macronutrient intake.
Introduction
Data from the 2009–2010 National Health and Nutrition Examination Survey (NHANES) suggest that 68.8% of those age ≥20 years are overweight (Body Mass Index [BMI]≥25 kg/m2) while 35.7% are obese (BMI≥30 kg/m2) [1] with approximately 51% of US adults predicted to be obese by 2030 Finkelstein [2]. Medical expenditures associated with the treatment of obesity and obesity related conditions are estimated at greater than $147 billion annually [2]. Data from the NHANES (2003–2008) indicated that among adults (18–54 years) approximately 75% of women and 54% of men expressed a desire to lose weight while 61% of women and 39% of men were actively pursuing weight control [3].
Exercise is recommended for weight management by several governmental agencies and professional organizations including the Association for the Study of Obesity [4], the Institute of Medicine [5], the U.S. Federal guidelines on physical activity [6], Healthy People 2020 [7] and the American College of Sports Medicine [8]. Compared with weight loss induced by energy restriction, weight loss achieved by exercise is composed predominantly of fat mass, while fat-free mass is preserved [9]–[11] and resting metabolic rate (RMR) is generally unchanged [12], [13], or slightly increased [14], [15], factors that may be associated with improved long term weight loss maintenance. However, several reports have demonstrated that the accumulated energy balance induced by an exercise intervention alone produces less of a negative energy balance than theoretically predicted for the imposed level of exercise-induced energy expenditure [16]–[18]. The energy balance induced by exercise training may be reduced due to compensatory changes in energy intake, non-exercise physical activity, or both [19]–[21]; thereby reducing the magnitude of observed weight loss. Although several narrative reviews regarding the impact of exercise on energy intake and appetite hormones have been conducted [22]–[29], we are aware of only one systematic review/meta-analysis on this topic. Schubert et al. [30] recently published a meta-analysis on the effect of acute exercise on subsequent energy intake that included only studies that assessed energy intake for ≤24 hours post-exercise in healthy (lean and/or obese), non-smoking individuals. To date, no systematic reviews on the effect of exercise and energy and macronutrient intake have been conducted that evaluated both the effects of acute exercise and exercise training and have included data from studies utilizing a variety of designs, e.g. cross-sectional, acute-crossover, non-randomized and randomized trials. Therefore, the aim of this systematic review was to identify and evaluate studies that have employed a variety of designs to assess the impact of both acute exercise and exercise training on energy and macronutrient intake. Results of this review will clarify our understanding of the association between exercise and energy intake and identify both exercise parameters including mode, frequency, intensity and duration and participant characteristics including age, gender, body weight, activity level that may impact this association. Such information will be useful for the design of weight management trials utilizing exercise, the potential identification of groups of participants for whom exercise may be most effective, and to identify areas for future investigation.
Methods
This systematic review was performed and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [31], [32].
Objectives
The objective of this systematic review was to address the question:
Does increased exercise or physical activity alter ad-libitum daily energy intake or macronutrient composition in healthy adults?
Eligibility Criteria
Primary source articles published in English in peer-reviewed journals were eligible for inclusion in this systematic review if data were presented on energy and/or macronutrient intake by level of exercise or physical activity or changes in energy or macronutrient intake in response to acute exercise or exercise training. Specific eligibility criteria included: Types of studies: Cross-sectional, acute/short-term (exercise duration ranging from a single 30-min exercise bout to daily exercise over 14 days), and both non-randomized and randomized trials. Types of participants: Healthy adults (age 18–65 years). Types of exercise interventions: Aerobic and resistance exercise. Types of outcome measures: No restrictions were placed on the assessment methods for the primary outcome (energy/macronutrient intake). Other criteria: There were no restrictions on the length of interventions or the types of comparisons. We included cross-sectional comparisons between participants differing by level of exercise or physical activity and longitudinal pre/post within group changes vs. non-exercise control or vs. a different level of exercise. Articles were excluded if they provided no data on energy or macronutrient intake by level of exercise or physical activity, manipulated or controlled energy intake, or were conducted in non-recreational athletes or individuals with chronic disease(s).
Information Sources
Studies were identified by searching electronic data bases, related article reference lists, and consulting with experts in the field. The search was applied to PubMed (1990-present) and adapted for Embase (1990-present). The last search was conducted on January 4, 2013. The search was developed as a collaborative effort of the research team in consultation with a Kansas University reference librarian and conducted by a co-author (SDH). No attempts were made to contact study investigators or sponsors to acquire any information missing from the published article.
Search Strategy
We used the following search terms in PubMed and Embase to identify potential articles with abstracts for review: exercise[ti (title), ab (abstract) ] or “physical activity”[ti,ab] or “energy expenditure”[ti,ab] OR “resistance training”[ti,ab] OR “strength training”[ti,ab]) AND (diets[ti,ab] OR diet[ti,ab] OR dieting[ti,ab] or “energy intake”[ti,ab] OR “energy restriction”[ti,ab] OR “nutrient composition”[ti,ab] OR “appetite”[ti,ab]). Additional search terms were applied to eliminate case reports and studies involving participants with chronic disease, and to retrieve studies published in English and conducted in adults (age 18–65 years). Word truncation and the use of wildcards allowed for variations in spelling and word endings.
Study Selection
Retrieved abstracts were independently assessed for eligibility for inclusion in the review by 2 investigators and coded as “yes”, “no” or “maybe.” All investigators who participated in eligibility assessments were trained regarding study inclusion/exclusion criteria and completed practice eligibility assessments on 50 test abstracts prior to actual coding. Eligibility assessments on the practice abstracts were reviewed by the primary author (JED) and any coding problems were discussed. Disagreements regarding eligibility for inclusion were resolved via development of consensus among all co-authors. Full text articles for abstracts coded as “yes” or “maybe” were retrieved and reviewed by 2 independent co-authors prior to inclusion in the review. An excel spread sheet was developed and used to track eligibility status.
Data Collection
Extracted data was entered into the University of Kansas secure, REDCap (Research Electronic Data Capture, Version 4.14.5) data base [33]. A REDCap data extraction form was developed, pilot tested on a sample of 10 studies (at least 2 studies of each of the 4 study designs included in this review), and revised accordingly. Relevant data were extracted from each manuscript by one author and verified by a second author. Disagreements were resolved by group discussion. Data extracted from each article included basic study information (design, sample size, groups compared, exercise or physical activity groups/intervention(s), participant characteristics (age, gender, BMI, minority status), energy and macronutrient assessment method, and results.
Risk of Bias in Individual Studies
Risk of bias for randomized trials was independently evaluated by two authors using the Cochrane risk of bias tool [34]. Risk of bias was assessed in the following domains: selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias. A third reviewer resolved any discrepancies in bias coding. Studies were not excluded on the basis of risk of bias.
Synthesis of Results
Articles were grouped by study design: cross-sectional, acute/short-term, non-randomized, and randomized trials. Considerable heterogeneity existed within study groups for several important study parameters. These parameters included: 1) participant characteristics (age, gender, BMI), 2) physical activity assessment methods (questionnaires, pedometers, accelerometers), 3) exercise prescriptions (mode, frequency, intensity, duration), 4) comparison groups (interventions: pre vs. post-exercise, exercise vs. non-exercise control, varying amounts), 5) intervention length, and 6) energy and macronutrient assessment methods (food frequency questionnaire, weighed and un-weighed food records, direct observation weigh and measure technique). A meta-analysis was therefore considered inappropriate. Results based on the extracted data were instead synthesized and presented grouped by study design.
Results
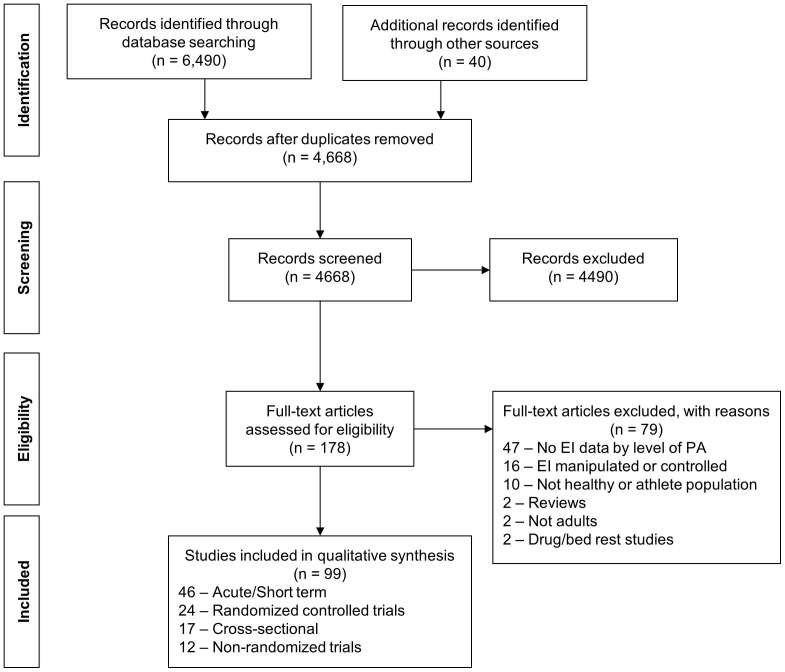
The initial database search plus hand searching identified 4,668 unique records of which 4,490 were excluded based on review of title and abstract. Full-text articles for the remaining 178 citations were reviewed of which 79 articles did not satisfy our inclusion criteria and were excluded. Thus 99 articles representing 101 studies were included in the review (Figure 1).
Figure 1. Flow diagram for identification, screening, assessing eligibility, and inclusion in systematic review.
Cross-Sectional Studies
The 17 cross-sectional studies identified comprised ∼17% of the total number of studies included in this review (Table 1).
Table 1. Cross-sectional/Correlational Studies.
| Study | Participants | Activity/Exercise Assessment | Comparison Group(s) | Dietary Assessment | Results |
| Butterworth et al. (1994) [50] | 34 women: Age = 29.7 (5.5); BMI = NR; % Fat = 22.7 (6.4) from skinfolds | Portable accelerometer 1 random day each wk over a 10 wk period. VO2 max on a treadmill. | NA: Correlational study | 10 repeated 24 hr diet records, randomly assigned, over a 10 wk period | EI per kg body weight was significantly correlated with energy expenditure. No significant correlations were found between nutrient intake/1,000 kcal and either VO2 max or mean 24-hour energy expenditure (kcal/day) |
| Camoes et al. (2008) [35] | Total Sample (1483 women & 921 men): Age = range 18–92; BMI = range 25.2–27.0 | EPIPorto PA questionnaire: included, occupational, domestic and leisure-time activities. | Sedentary: Less than 10% of EE at a moderate or high intensity level (4 METs) during occupational activities, leisure time or throughout the day. Active: All others. | Validated semi-quantitative food-frequency questionnaire assessing dietary intake over the previous year. | There were no significant differences in daily nutrient intake by activity group for women. Active men had significantly higher daily EI and lower PRO intake as a percent of EI than sedentary men. |
| D'Angelo et al. (2010) [41] | 51 women in a university required course: Age = NR; BMI = NR | International PA Questionnaire | 3 groups based on percentiles: Group 1 (n = 17) = 1st to 32nd % ile (0 min/wk); Group 2 (n = 17) = 33rd to 65th % ile = 95 (35.6) min/wk; Group 3 (n = 17) = 66th to 100th % ile = 231.7 (85.9) min/wk | 3-day food record (2 weekdays/1weekend day) | EI was significantly higher in group 3 compared to the 2 other groups. |
| Duvigneaud et al. (2007) [42] | 362 women: Age = 51.4 (12.9); BMI = 24.1(3.5); 485 men: Age = 50.2 (13.3); BMI = 25.4 (3.1) | Flemish PA Computerized Questionnaire. | 3 groups based on hrs/wk of sports participation: 0 (n = 129), <3.5 (n = 157), ≥3.5 (n = 199). | 3-day food record ( 2 week days/1 weekend day) | No significant between group differences for energy, PRO or CHO intake. Fat intake (kcal/day and % EI) was significantly lower in the group reporting ≥3.5 hrs/wk of sport participation vs. the 0 hrs/wk group. |
| Eaton et al. (1995) [36] | Total Sample (1206 women & 798 men; Minorities = 9.3%): Age = 37.4 (5.7); BMI = 26.1 (5.7) | “At least once a week, do you engage in any regular activity such as brisk walking, jogging, bicycling, etc., long enough to work up a sweat?” | No = sedentary, Yes and did 1–3 times/wk = moderately active. Yes and did 4–7/wk = very active. | Willett Food Frequency Questionnaire | No significant difference in EI between activity groups. The more active groups had higher intakes of PRO and CHO. Total fat, saturated fat, and the percentage of kcals from fat and saturated fat were lower in the active groups. |
| Gilliat-Wemberly et al. (2001) [14] | 32 women: Active (n = 18): Age = 42 (3); BMI = 21.6 (1.6) Sedentary (n = 14): Age = 42 (4); BMI = 22.8 (2.4) | Self-report | Active: Minimum of 6 hrs/wk and have maintained this level of activity for a minimum of 5 years. Sedentary: Exercise <2 hrs/wk and maintained this lifestyle for a least 5 years. | 7-day food record – calibrated scales used to weigh food. | Active women had significantly lower fat intake as a % of total kcal compared to their sedentary counterparts. No between group differences in EI or in PRO, CHO, fat, alcohol, caffeine, fiber (grams/day). |
| Hornbuckle et al. (2005) [43] | 69 women: Age = 51.4 (5.4); BMI = 30.9 (6.8) | 7-day pedometer | <5000 steps/day; 5000–7499 steps/day; >7500 steps/day | 3-day food record | No significant difference in EI between groups. |
| Jago et al. (2005) [49] | Total Sample (722 women & 469 men; Minorities = 24%): Age = 29.7 (5.1); BMI = 27.3 (6.7) | Compared to other people your age and sex, how would you rate your PA outside of work during the past year? | 1 = Physically inactive; 2; 3 = Moderately active; 4; 5 = Very active | Youth/Adolescent Food Frequency Questionnaire (YAQ) | There was a significant difference in total EI across the five activity groups after controlling for BMI, age, income, ethnicity, gender, and ethnicity by gender interaction terms. Pairwise comparisons indicated that this difference was significant between groups 3 and 5. There was also a significant difference in the percentage of EI from fat by activity level with group 2 consuming a larger proportion of energy from fat than group 4. No significant between group differences in either PRO or CHO consumption. |
| Lake et al. (2009) [37] | Total Sample (29 women; 44 men): Age = 18 (1.0); BMI = NR; Convenience sample of college students studying sport (24 men, 8 women) or non- sport (20 men, 21 women) subjects. | PA component of the ‘Youth NEWS’ (Neighbourhood Environment Walkability Survey) | Sport vs. non-sport students and categories of time spent in sedentary pursuits (homework, TV, DVD etc.) | The European Prospective Investigation of Cancer food frequency questionnaire. Assessed dietary intake over the past year. | Sport students had a significantly lower intake of fat and a significantly higher percentage energy from protein compared to the non-sports students. Sedentary behaviors were significantly associated with less healthy eating patterns. Higher total EI, higher fat percentage energy from fat and lower CHO intakes were significantly associated with more time spent watching DVDs on weekends. |
| Lee et al. (2010) [44] | 39,876 women (Minorities = ∼5%) Age by activity group: <7.5 MET-hrs/wk = 54.1 (6.8); 7.5<21 = 54.3 (6.9); ≥21 = 54.2 (6.9). BMI by activity group: <7.5 MET-hrs/wk = 26.9 (5.5); 7.5 to <21 = 25.5 (4.5); ≥21 = 24.5 (4.1) | College Alumni Health Study PA Questionnaire. | 3 Groups: 1) <7.5 MET-hrs/wk equivalent to <150 min/wk of moderate- intensity PA); 2) 7.5 to <21 MET-hrs./wk.; 3) ≥21 MET-hrs/wk.(equivalent to ≥420 min/wk moderate-intensity activity. | Willett Food Frequency Questionnaire. | No significant between group differences for EI, fat intake, or servings of fruits and vegetables by activity group. |
| Lissner et al. (1997) [45] | 361 women: Age: Sedentary = 50.4 (6.3); Somewhat Active = 48.1 (6.4); More Active = 48.9 (5.1); BMI: Sedentary = 25.7 (5.3); Somewhat Active = 24.3 (3.9); More active = 23.2 (3.3) | Gothenburg PA Questionnaire | 3 Groups: Sedentary = almost inactive; Somewhat active = engaged in at least 4 hrs. of activity/wk; More active = greater than 4 hrs/wk. | Food frequency questionnaire | No significant between group differences for EI or fat intake (g/day and % total EI) |
| Matthews et al. (1997) [47] | Total Sample (494 women, 425 men); Age: Women = 48.4 (10.6); Men = 49.8 (10.2). BMI: Women = 28.1 (5.9); Men = 27.8 (4.4) | Questionnaire: “Do you exercise on a regular basis?” and if yes asked about frequency (times/wk), duration (min/session) and mode. If no answer assumed they engaged in no explicit leisure time PA. | Inactive = 0 to 29 min/wk.; Active = 30 min or more/wk; Active sub-categories:>30 to 60 min/wk; 61 to 120 min/wk; ≥121 min/wk | 7-day or 24-hour diet recalls. | No significant difference in EI or macronutrient intake between the 4 activity groups. |
| Mulligan et al. (1990) [46] | 21 women: Non-runners (n = 5); Moderately active runners (n = 9); Very active runners (n = 7); Age by activity group: Non-runners = 30.6 (5.6); Moderately active runners = 37.2 (4.2); Very active runners = 29.8 (8.0) | Activity diary over 2 months and VO2 max. | Non-runners: distance/wk. = 0; VO2 max = 41.7 (8) ml/kg/min; Moderately active runners: 39.5 miles/wk.; VO2 max = 39.5 (10.1) ml/kg/min; Very active runners: 54.4 miles/wk.; VO2 max = 66.8 (7.5) ml/kg/min | Weigh and measure diet record collected over 24 hrs on 3 random consecutive days each wk over 2 months. | No significant between group differences in EI. |
| Perry et al. (1992) [48] | 70 women: Distance runners (n = 19); Recreational joggers (n = 19); Aerobic dancers (n = 17); Inactive controls (n = 15)). Age: Runners = 37.2 (9.0); Joggers = 32.6 (8.3); Aerobics = 32.2 (6.0); Controls = 33.3 (7.3). BMI: Runners = 21.7 (NR); Joggers = 20.4 (NR); Aerobics = 20.8 (NR); Controls = 22.3 (NR) | Recruited by activity level. | Long distance runners: Averaged at least 26 mi/wk, mean = 40 mi/wk; Recreational joggers: Averaged at least 6 mi/wk., mean = 16 mi/wk.; Aerobic dancers: Taught at least 6 aerobic dance classes/wk, mean = 9.4 hrs/wk.; Inactive controls: Exercised less than one time/wk and not on a regular basis. | One-day food record | EI was not significantly difference between groups. |
| Rintala et al. (2010) [38] | 16 twin pairs (7 monozygous, 9 dizygous; 11 male and 5 female pairs): Age = 60 (range 50–74); BMI: Inactive = 26.7 (3.5); Active = 21.5 (6.4) | Questionnaire: 3 structured questions; mean duration of one activity session with five response alternatives, monthly frequency of activity with six response alternatives and activity intensity based on the following question: “Is your PA during leisure time about as strenuous on average as: (i) walking, (ii) alternately walking and jogging, (iii) jogging, (iv) running?” | Active/inactive co-twins discordant for PA over a 32 year period. Inactive co-twins averaged 8.8 MET-hrs/day less activity than their active co-twin. | Food diary: 3 week days and 2 weekend days | No significant difference in absolute EI (kcal/day) between active and inactive co-twin. REI (kcal/kg) was significantly higher in active vs. inactive co-twins. No significant difference between active and inactive co-twins for either absolute (g/d) or relative intake (%EI) of PRO, CHO or fat. |
| Van Pelt et al. (2001) [40] | 137 men: Young sedentary (YS): n = 32; Old sedentary (OS): n = 34; Young active (YA) : n = 39; Old active (OA): n = 32. Age: YS = 26 (1); OS = 62 (1); YA = 27 (1); OA = 63 (1). BMI: YS = 24.2 (0.7); OS = 26.7 (0.7); YA = 22.7 (0.4); OA = 23.5 (0.3) | Recruited by activity level. | Active: Local runners and triathletes who placed in the top 25% of their age divisions in either 10-km running events or triathlon competitions. Sedentary: Performed no regular PA. | Food diary over 4 consecutive days (3 weekdays and 1 weekend day) | EI (kcal/day) was significantly higher in the YA vs. the YS but did not differ by activity level in older men. No significant between group difference for macronutrient intake (%fat, CHO or PRO) in either the young or old group. |
| Van Wallenghen et al. (2007) [39] | Total Sample (15 women, 14 men): Age: Sedentary = 26.0 (1.0); Active = 23.0 (1.0). BMI: Sedentary = 23.5 (0.8); Active = 23.1 (0.7) | Habitual PA including both planned exercise (jogging, cycling, etc.) and daily living-type activities (housework, yard work, etc.) was determined by self-reported time (min/wk) spent participating in moderate and vigorous PA. | Active = active subjects spent ≥150 min/wk engaged in moderate and/or vigorous PA for ≥2 years. | Self-reported 4-day food intake record. | EI (kJ/day) was significantly higher in the active group. The % energy from fat was lower in the active group, % energy from CHO was higher in the active group. No between group differences in % energy from PRO. |
Note, Values are means (standard deviation) unless otherwise noted. Abbreviations: PA = Physical Activity; CHO = carbohydrate; EE = energy expenditure; EI = energy intake; NR = not reported; NA = not applicable; PRO = protein; REI = relative energy intake; MET = Metabolic equivalent of task; kcal = kilocalories; KJ = kilojoules; hrs = hours; min = minutes; wk = week.
Cross-Sectional Studies: Study Characteristics
Sample size
Median (range) sample size for studies that included both men and women was 447 (14–921) for men and 428 (10–1483) for women. In studies that included only men or women the median sample size for men was 137 (one study) and women was 60 (21–38,876).
Comparisons
Seven studies compared 2 groups (active vs. sedentary) [14], [35]–[40]. Six studies compared 3 groups [41]–[46] while 3 studies compared physical activity over 4 or more groups [47]–[49]. One study reported the correlation between physical activity level and energy intake [50].
Physical activity assessment
Seven studies (∼41%) employed a physical activity questionnaire [14], [35], [37], [41], [42], [44], [45], 5 studies (∼29%) used a single item self-report or self-report physical activity rating scale [36], [38], [39], [47], [49], and one study used a physical activity diary[46]. Two studies used objective assessments of physical activity (accelerometers/pedometers) [43], [50] while 2 studies recruited participants based on their self-reported participation in recreational aerobic sports [40], [48].
Energy/Macronutrient intake assessment
Food frequency questionnaires were used in 6 studies [35]–[37], [44], [45], [49] while 4 studies used non-weighed 3-day food records [38], [41]–[43]. One [48], 4 [39], [40] and 7-day [47] non-weighed food records, 3 [46] and 7-day weigh and measure food records [14] and repeated 24-hour recalls were also employed in 2 studies [47], [50].
Cross-Sectional Studies: Participant Characteristics
Age
The median (range) age across the 15 studies that reported age was 42 (18–60) years.
Gender
Nine studies included both men and women [35]–[39], [42], [47], [49], 8 studies included women only [14], [41], [43]–[46], [48], [50] while one study included only men [40].
BMI
The median (range) BMI across 13 studies that reported BMI was 24.8 (21.3–30.9) kg/m2.
Minority representation
In the 3 of 17 studies (18%) that provided data, minority representation ranged from 5% [44] to 24% [49] of the total sample.
Cross-Sectional Studies: Results
Energy intake
Seven of 17 (41%) cross-sectional studies indicated significantly higher absolute (kcal/day) [35], [39]–[41], [49] or relative (kcal/kg/day) energy intake [38], [50] in active compared with less active groups. There were no apparent differences in either basic study design parameters including sample size, assessment methods for both energy intake and physical activity, the number and type of comparison groups, or participant characteristics such as age, gender or BMI between studies that did and did not report a significant association between physical activity and energy intake.
Macronutrient intake
Thirteen of 17 studies presented data on the intake of one or more macronutrients (fat, carbohydrate, protein). All 13 studies included data on fat intake. Six studies (46%) reported either lower absolute (grams) [36], [42] or relative fat intake (% total energy intake) [14], [36], [37], [39], [42], [49] in groups with higher levels of physical activity while 7 studies (54%) that reported fat intake by activity level failed to find a significant association [35], [38], [40], [44], [45], [47], [50]. Eleven studies provided data on both carbohydrate and protein intake. Two studies (18%) reported higher carbohydrate intake in active groups [36], [39], while 9 studies (82%) found no association between the level of physical activity and carbohydrate intake [14], [35], [37], [38], [40], [42], [47], [49], [50]. Relative protein intake was higher (2 studies) [36], [37], lower (one study) [35] or not different (8 studies) [14], [38]–[40], [42], [47], [49], [50] between groups reporting higher vs. lower levels of physical activity.
Acute Studies
The 40 acute studies comprised ∼40% of the total studies identified for this review (Table 2). All acute studies employed cross-over designs, which compared energy intake assessed over a time frame of 24 hours or less following an acute exercise bout.
Table 2. Acute and Short-Term Studies.
| Study | Participants | Intervention | Meals | Results: Exercise | Results: Diet |
| Balaguera-Cortez et al. (2011) [77] | 10 men: Age = 21.3 (1.4); BMI = 23.7 (2); VO2 max = 58.1 (7.3) ml/kg/min | 45 min aerobic: Treadmill at 70% of VO2 peak; 45 min RT: 3 sets of 12 reps of 8 different exercises; Control: 45 min rest; experiment started at 7 AM, 45 min exercise, 30 min rest, followed by assessment of EI. | Buffet-type breakfast, foods and drinks for 30 min and instructed to eat ad libitum and to satiation. | Total weight lifted = 14,432 (3,551) kg. Aerobic exercise was at 71 (7%) VO2 peak, and EEEx was 2818 (418) kJ for the 45 min. Estimated EEEX from the RT trial was 1,350 kJ for 45 min. Control EE was 256 kJ for 45 min. | No significant effect of trial on total EI, or CHO, fat, or protein both in grams and as a percent of total EI. Also no differences between trials in solid food or drink consumption as a % of total EI. |
| Deighton et al. (2012) [81] | 12 men: Age = 23.0 (3.0); BMI = 22.9 (2.1); VO2 max = 57.9 (9.7) ml/kg/min | Control: 60 min rest; Exercise: 60 min treadmill run at 70% max VO2 performed either in a fasted (8 AM) or fed (12 PM) state. | Standardized breakfast served at 9:30 AM. Buffet meal offered at 1:30 and 5:30 PM. | Net EEEx fasted trial = 3247 (423 kJ); Net EEEx fed trial = 3234 (435) kJ | No significant differences in EI between trials resulting in a negative energy balance in the exercise trials relative to control after accounting for differences in EEEx. |
| Erdman et al. (2007) [64] Intensity trial | 5 women, 2 men: Age = 24.4 (0.6); BMI = 21.4 (0.8); Activity level/fitness = NR | Low intensity exercise: 30 min at 50 W (60 rpm). Higher intensity exercise: 30 min at 100 W (60 rpm). Control: 45 min rest. | Sandwiches consisting of bread, butter and ham (2.73 kcal/g, energy percent: 44.4% carbohydrate, 16.2% protein and 39.4% fat). Test meal offered 15 min post exercise | EEEX low intensity = 85.6 Kcal; EEEx higher intensity = 171.2 Kcal | Food (g) and EI (kcal) were not different after either intensity compared to the control. |
| Erdman et al. (2007) [64] Duration trial | 3 women, 4 men: Age = 24.8 (0.7); BMI = 22.1 (NR); Activity level/fitness = NR | Cycle ergometer exercise (60 rpm) for 30, 60, 120 min at 50 W. | Same as above | EEEx 30 min = 85.6 Kcal; EEEx 60 min = 171.2 Kcal; EEEx 120 min = 342.4 Kcal | EI and food intake after the 30 and 60 min exercise bouts was not different from controls. EI and food intake following the 120 min bout were significantly greater than control. |
| Farah et al. (2010) [96] | 10 men: Age = 35 (6); BMI = 28.2 (2.4); VO2 max = 43.0(6.4) ml/kg/min | 3–4 day trials: Control: No exercise on days 1–3. EX-1: One exercise session on day 3; treadmill walking, 50% VO2 max. EX-3: exercise sessions on each day 1–3 at 50% VO2max. | Reported to metabolic suite on the morning of day 4. Presented with ad lib buffet style breakfast and lunch. | Net EEEx = 2.98 (0.11) MJ in EX-1 and 8.92 (0.30) MJ in EX-3. | There were no differences between trials in energy, fat, carbohydrate, or protein intakes at breakfast, but energy, carbohydrate, and protein intakes at lunch were significantly higher in EX-3 than in both CON and EX-1 |
| Finlayson et al. (2009) [69] | 24 women: Age = 24.0 (6.1); BMI = 22.3 (2.9); Activity level/fitness = NR | Control: 50 min sitting. Exercise: 50 min cycle ergometer at 70% of maximum HR. | Test meal offered 40 min post trial. | Estimated EEEx = 189.3 (13) kcal. | EI was not different between exercise and control conditions. |
| George & Morganstein (2003) [73] | 24 sedentary women (12 normal and 12 overweight): Age = 35 (8); BMI = 22 (1) Normal weight; 28(1) overweight | Exercise = walking on a treadmill at 60% of max HR for 60 min. Non-exercise = sedentary activities for 60 min. | Ad libitum lunch at the university cafeteria. Test meal offered approximately 30 min post trial | Estimated EEEx = 150–200 kcal depending on body weight. | EI was not different between exercise and control in either normal or overweight women. |
| Harris et al. (2008) [61] | 80 sedentary men: Age = 30 (8); BMI = range 22–29; 5 groups: 1) normal weight, low-restraint, non-dieting; 2) normal weight, high-restraint, non-dieting; 3) overweight, low-restraint, non-dieting; 4) overweight, high-restraint, non-dieting; and 5) overweight, high-restraint, dieting. | Control: 60 min rest. Exercise: 60 min treadmill exercise at 60–65% age-predicted max HR. | Ad libitum lunch at the university cafeteria. Other EI over 12 hrs post exercise was assessed by diet recall conducted by phone. Test meal offered approximately 15 min post trial. | EEEx = NR | Exercise had no significant impact on post exercise EI in any study group. |
| Imbeault et al. (1997) [51] | 11 men: Age = 24.4 (3.3); BMI = 23.3 (2.3); VO2 max = 56.7(5.0) ml/kg/min | Control: seated for the same duration as the low intensity exercise condition. Low intensity exercise: Treadmill walking at 35% VO2 max, duration to reach EEEx of ∼2050 kJ. High intensity exercise: Treadmill running at 75% VO2 max to reach EEEx of ∼2050 kJ. | Buffet meal 15 min post trial. | EEEx low intensity = 2054 (45) kJ. EEEx high intensity = 2022 (38) kJ. | There were no significant between group differences for absolute EI. Relative EI (EI minus net EEEx) was significantly lower for high intensity exercise than both control and low intensity exercise. |
| Jokisch et al. (2012) [78] | 20 men; 10 active (exercise ≥150 min/wk); 10 inactive (exercise≤60 min/wk): Age = 21.2 (1.9); BMI = 23.4 (1.7) | Control: 45-min reading. Exercise; 45 min cycle ergometer at 65–75% of age predicted max HR to elicit EEEx of approximately 450 Kcal. | Ad libitum buffet lunch. Test meal offered 60 min post trial. | EEEx active = 456 (9) kcal/45 min. EEEx inactive = 451 (12) kcal/45 min both estimate using American College of Sports Medicine equations for energy expenditure during leg cycling. | EI was significantly lower at the ad libitum meal following exercise as compared to control in the inactive group. There was no effect of exercise on EI in the active group. No difference in meal macronutrient intake was found. |
| Keim et al. (1990) [90] | 12 sedentary to moderately active women: Age = 30 (1); BMI = 27.7 (NR) | 4 days acclimatization to exercise and 14 days at the specified exercise level. 3 conditions: No exercise (NO-EX): subjects maintained usual daily activity. Moderate duration exercise (M-EX): achieve an energy expenditure 12.5% above baseline. Long duration exercise (L-EX): achieve an energy expenditure 25% above baseline. | Participants were free-living. Required to report to a metabolic kitchen daily to consume breakfast and dinner, to pick up lunch and snacks, and to perform prescribed exercise programs. | EEEx goals for 12.5% and 25% above baseline were achieved with exercise at 72 (1)% of predicted VO2 max for both exercise groups. Duration of exercise ranged from 31–49 min in the M-Ex group and 51–88 min in the L-EX group. | There were non-significant increases in EI in both the M-EX (5%) and L-EX (8%) groups. Daily intake of carbohydrates, protein or fat averaged over the study period was not affected by exercise. |
| Keim et al. (1996) [91] | 15 weight reduced obese women, Aerobic exercise (n = 8): Age = 31 (2 SEM); BMI = 28.1 (1.6 SEM); Resistance exercise (n = 7):Age = 31 (3 SEM); BMI = 29.3 (2.0 SEM); Activity level/fitness = NR | 14 days Aerobic exercise: Supervised treadmill exercise 5 days/wk, 75% VO2 max, EEEx at 29% of RMR. Resistance exercise: Supervised, 1 set of 8 reps at 50–60% 1-RM. | All meals provided in a metabolic ward. | EEEx aerobic exercise = 354 kcal/session. EEEx resistance exercise = 96 kcal/session. | EI during the intervention was not significantly different from a 3 wk. control period in either the aerobic or resistance training groups. EI for both the aerobic and resistance training groups were not significantly different during the intervention period despite the higher levels of EEEx in the aerobic exercise group. |
| Kelly et al. (2012) [79] Normal hydration condition | 10 men: Age = 21.4 (1.3); BMI = 23.9 (2.1) Active | Control: 45 min rest. Exercise: 45 min treadmill running at 70% VO2 peak. | Buffet breakfast offered 30 min post trial. | EEEx = 2949 (207) kJ. | There was no significant difference in EI or macronutrient composition between trials. Relative EI (post-exercise EI minus (EEEx+EPOC) was significantly higher in control vs. the exercise trial. |
| King JA et al. (2010) [58] | 14 men: Age = 21.9 (0.5 SEM); BMI = 23.4 (0.6 SEM); VO2 max = 55.9 (1.8) ml/kg/min | Control: 7 hrs rest. Exercise: 60 min subjectively paced walk on a level motorized treadmill. | Ad libitum buffet foods that were identical for each meal. Test meal offered 30 min and 4 hrs post trial. | Walks were completed at a mean of 42.5(2)% of VO2 max and generated a net EEEx (exercise minus rest) of 2008 (134) kJ. | EI was not significantly different between the control and brisk walking trials. After adjusting for the energy expenditure of walking, there was an energy deficit of 1836 (130) kJ in the brisk walking trial compared with the control trial. No significant between trial differences absolute energy intake from fat, CHO or PRO. |
| King JA et al. (2010) [57] | 9 men: Age = 22.2 (0.8); BMI = 23.6 (0.4); VO2 max = 60.5 (1.5) ml/kg/min | Control: 8.5 hrs rest. Exercise: 90 min treadmill run at 68.8 (0.8)% of max VO2 followed by 8.5 hrs rest. | Ad libitum cold buffet offered at 2.5 and 9 hrs. Hot meal at 5.5 hrs. | Net energy expenditure (exercise minus rest) was EEEx = 5324 (186) kJ or 1273 (45) kcal. | No effect of trial on EI or macronutrient intake. After accounting for EEEx participants remained in energy deficit in the exercise as compared to the control trial. |
| King JA et al. (2011) [82] | 12 men: Age = 23.4 (1); BMI = 22.8 (0.4); VO2 max = 57.3 (1.2) ml/kg/min | Control: 7.5 hrs rest. Exercise: 90 min treadmill run at 70% VO2 max. | Test meal at 2 and 4.75 hrs. Buffet meal at 8 hrs. | Net EEEx (exercise minus rest) = 4715 (113) kJ. | No significant difference in EI or macronutrient intake between exercise and control. |
| King JA et al. (2011) [56] | 14 active men: Age = 22 (0.5); BMI = 23.2 (0.6) | Control: 7.5 hrs rest. Exercise: Swimming – 6 ten min blocks at a moderate intensity (perceived exertion between 12 and 14). | Ad libitum buffet meal offered at 3 hrs (∼12:00) and 7.5 hrs (∼16:30) into the trial. | Net estimated EEEx (exercise minus resting)+1921 (83) kJ. | No significant difference in EI or macronutrient intake between swimming and control trials. |
| King NA et al. (1997) [94] | 8 active men: Age = 26.0 (5.2); BMI = 22.4 (1.8) | Each condition was performed over 2 consecutive days. Control: No exercise (R1 and R2). Exercise (Ex1 and Ex 2): 2 session in one day of treadmill running at ∼70% max HR for 50 min (100 min at 70% max HR) | Food and drink intake were monitored using a set of digital weighing scales and a self-record diary. | The combined EEEx for both Ex sessions was 1200 kcal. | No significant differences in EI were noted between R1 and R2, Ex1 and Ex2 or Ex1 and R1 or Ex2 and R2. Also no differences between trials for PRO, FAT or CHO as a % of kcal intake. |
| King NA et al. (1996) [74] | 13 women: Age = 22.6 (2.3); BMI = 21.9 (1.6); VO2 max = 37.0 (3.0) ml/kg/min | Control: 50 min rest. Exercise: cycle ergometer, 50 min at 70% VO2 max. | Ad libitum lunch containing either 7 high-fat foods or 7 low-fat foods. Test meal offered 15 min post trial. | EEEx was approximately 350 kcal at 73% VO2 max. | EI after exercise increased slightly (9%), however was not significant when compared to the rest condition. EI was increased when participants consumed the high-fat lunch as compared to the low-fat lunch for both the rest and exercise conditions. |
| King NA et al. (1995) [59] | 24 men; assigned to either a treadmill running (n = 12) or cycle ergometer (n = 12) study. Age = Run: 21.4 (3.4); Cycle: 24.4 (5.3); BMI = Run: 22.9 (NR); Cycle: 22.8 (NR); VO2 max Cycle = 49.3 (2.2) ml/kg/min; VO2 max Run = 47.9 (8.2) | 4 test conditions for both the run and cycle groups. Control, high fat/low carb lunch options. Control, low fat/high carb lunch options. Exercise (70% VO2 max), high fat/low carb lunch options. Exercise (70% VO2 max), low fat/high carb lunch options. | Ad libitum test lunch. Ad libitum food provided for consumption on the rest of the day assessed by records. Test meal offered immediately post trial. | EEEx for both cycling and running was approximately 600 kcal over 45 min. | No significant main effect of exercise on EI; however, EI was higher when high fat/low carb food options were available. There was a significant main effect of exercise on relative energy intake (REI: test meal intake minus EEEX). REI was significantly suppressed in the low fat/high carb treatment but not the high fat/low carb treatment vs. control. |
| King NA et al. (1994) [60] Intensity trial | 11 active men: Age = (range 21–27); BMI = 24.2 (NR) | Control: Seated rest for ∼45 min. High intensity exercise: Cycle at 70% VO2 max ∼30 min (mean = 27 min). Low Intensity Exercise: Cycle at 30% of VO2max for ∼60 min (mean = 63 min). | Ad libitum test meal offered 15 min following completion of the trial. EI over the rest of the experimental day was assessed by food records. | EEEx high intensity = 340 (27.6) Kcals. EEEx low intensity = 359 (41.5) Kcals. | No significant difference in absolute EI or macronutrient intake at the test meal between the 3 treatments. Food diary data showed no significant difference between the 3 treatments for the remainder of the day. |
| King NA et al. (1994) [60] Duration trial | 12 active men: Age = range (22–31); BMI = 23.2 (2.2) | Control: Seated rest for ∼45 min. Short duration exercise: 26 min at 70% VO2 max. Long duration exercise: 52 min at 70% VO2 max. | Same as above | EEx short duration = 296 (38.4) kcal. EEEx long duration = 541 (52.2) kcal. | No significant difference in absolute EI or macronutrient intake at the test meal between the 3 treatments. Food diary data showed no significant difference between the 3 treatments for the remainder of the day. |
| Kissileff et al. (1990) [75] Non-Obese Participants | 9 sedentary women: Age = 22.7 (4.9); BMI = 21.1 (1.8) | Control: 40 min rest. Strenuous exercise: 40 min at 90 watts on a cycle ergometer. Moderate exercise: 40 min at 30 watts on a cycle ergometer. | Test meal offered 15 min post trial. | EEEx strenuous exercise = 246.8 (24.3) Kcal. EEEx moderate exercise = 113.7 (36.7) kcal. | EI was significantly reduced compared to control following strenuous but not moderate exercise. |
| Kissileff et al. (1990) [75] Obese Participants | 9 sedentary women: Age = 24.3 (4.9); BMI = 27.7 (0.9) | Same as above | Same as above | EEEx strenuous exercise = 237.2 (25.1) kcal. EEEx moderate exercise = 143.2 (33.3) | EI was not significantly different across conditions. |
| Laan et al. (2010) [65] | 10 men, 9 women: Age = 22.3 (2.5); BMI = 22.5 (1.8); VO2 max = 60.1 (22.5) ml/kg/min | Control: 35 min rest. Aerobic exercise: 35 min cycling at 70% HRR. Resistance exercise: 5 exercises, 3 sets at 70% 1 RM, 2 sets of 10 repetitions and a 3rd set to voluntary fatigue or 12 repetitions. | Test meal (large bowl of pasta salad) offered 30 min post trial. | Estimated EEEx = 290 (7) kcal for aerobic and 80 (2) kcal for resistance exercise. | EI was higher in both aerobic and resistance exercise trials compared with control. Relative EI (EI – EEEx) was lower in aerobic exercise compared with the resistance and control trials. |
| Larson-Meyer et al. (2012) [76] Runner sample | 9 women: Age = 23.7 (2.4); BMI = 19.8 (1.0); VO2 max = 49.7 (3.0) ml/kg/min | Control: 3 hrs rest. Exercise: 60 min treadmill run at 70% VO2 max. | Test meal offered 2 hrs post trial. | EEEx = 483.1 (49.7) kcal. | EI and macronutrient intake were not significantly different between exercise and control trials. REI was significantly lower following exercise vs. control. |
| Larson-Meyer et al. (2012) [76] Walker sample | 10 women: Age = 24.6 (6.9); BMI = 21.1 (3.4); VO2 max = 33.9 (3.7) ml/kg/min | Control: 3 hrs rest. Exercise: 60 min treadmill walk at 70% VO2 max. | Same as above | EEEx = 324.6 (138.1) Kcal. | EI was not significantly different in exercise vs. control trials. PRO and fat intake was significantly higher following exercise vs. control. |
| Lluch et al. (1998) [71] | 12 women: Age = 21.7 (2.2); BMI = 22.6 (1.9); VO2 max = 41.0 (4.4) ml/kg/min | Rest- low fat: 50 min rest - low fat test meal. Rest-high fat: 50 min rest - high fat test meal. Exercise-low fat: 50 min cycle at 70% VO2 max-low fat test meal. Exercise-high fat: 50 min cycle at 70% VO2 max-low fat test meal. | Test meal (lunch) offered 20 min post trial. | EEEx exercise-low fat trial = 425 (60) kcal. EEEx exercise-high fat trial = 422 (59) kcal. | Neither EI at the test meal nor EI during the rest of the day were significantly different between the exercise and rest conditions for either diet. When controlling for EEEx, exercise decreased relative EI by 43%. Therefore there was no energy compensation in response to exercise during the following lunch test meal. |
| Lluch et al. (2000) [70] | 13 women (unrestrained eaters: URE): Age = 22.6 (2.3); BMI = 21.9 (1.6); VO2 max = 37.0 (3.3) ml/kg/min. 12 women (restrained eaters: RE): Age = 21.7 (2.2); BMI = 22.6 (1.9); VO2 max = 41.0 (4.4) ml/kg/min | Same as above | Test meal (lunch) was offered immediately post trial. | EEEx unrestrained eaters = 1455 (213) kJ. EEEx restrained eaters = 1772 (242) kJ. | There was a significant main effect of lunch type on EI with EI increased in both high fat conditions compared with low fat. The exercise by group interaction on EI was not significant: URE increased EI after exercise whereas in RE the EI tended to decrease. When exercise induced EE was controlled for, there was a significant effect of lunch type, exercise and exercise by group interaction on relative EI: exercise decreased relative EI when compared to rest and this difference was higher in restrained compared to unrestrained eaters. |
| Maraki et al. (2005) [63] | 12 sedentary women: Age = 28 (6.4); BMI = 21.3 (1.6) | Control: 60 min rest. Exercise: 60 min aerobic and muscle conditioning exercise classes. Each trial was done both in the morning (0815 to 0915) nd in the evening (1915 to 2015). | Diet was assessed on each trial day by 24-hr diet record. | Estimated EEEx exercise trial = 1233 (106.8) kJ. Estimated EEEx control trial = 234 (20.3) kJ. | No significant difference between the 4 trials in daily EI. |
| Martins et al. (2007) [68] | 6 sedentary to active women, 6 sedentary to active men: Age = 25.9 (4.6); BMI = 22.0 (3.2) | Control: 60 min rest. Exercise: 60 min intermittent cycle ergometer exercise at 65% of each subject's estimated max HR (2 min warming up+17 min exercise+3 min break+17 min exercise+3 min break+17 min exercise+2 min cooling down) | Buffet test meal offered 1-hr post trial. | Estimated EE control session = 197 (37) kcal. Estimated EEEx = 492 (92) kcal. | Absolute EI at the buffet meal was significantly higher in the exercise vs, the control trial. No significant differences were observed in the percentage of energy provided by either PRO, fat or CHO. REI was significantly lower following the exercise vs with control. |
| Melby et al. (2002) [54] Non-carbohydrate supplement group | 13 women: Age = 23 (0.8); BMI = 21.6 (0.2); VO2 max = 39.6 (0.9) ml/kg/min | Control: ∼76 min rest. Exercise: Cycle ergometer exercise at 65% VO2 peak to produce a net energy cost of ∼500 kcal. | Buffet meal offered 90 min post trial. | Net EEEx = 517 (6) kcal. | No significant differences between control and exercise trials in EI or macronutrient intake either at the test meal or food consumed over the remainder of the day. |
| O'Donoghue et al. (2010) [55] | 9 men: Age = 20.3; BMI = 22.4 (1.6); VO2 max = 58.8 (5.6) ml/kg/min | Control: 45 min rest. Exercise: 45 min treadmill running at 75% VO2 peak. Exercise was performed at 7 AM or 5 PM. | Buffet breakfast, lunch and dinner were offered on trial days. | EEEx AM exercise = 2,831 (519) kJ.EEEx PM exercise = 2898 (570) kJ. | No significant differences between trials in absolute EI or macronutrient intake. REI was significantly lower post exercise compared with control; i.e., REI during the breakfast was significantly lower after AM exercise than either PM exercise or control. REI during the evening period was significantly lower after PM exercise than for the control trial and tended to be lower than the AM exercise trial. However, over the total 26- hr period REI was similar between all trials. |
| Pomerleau et al. (2004) [52] | 13 women: Age = 22.2 (2); BMI = 22.2 (4); VO2 max = 44.0 (4.7) ml/kg/min | Control: rest 75 min. Low intensity exercise = treadmill walking at 40% VO2 peak. High intensity exercise = treadmill walking at 70% VO2 peak. Duration to achieve EEEx of ∼350 kcal at both exercise intensities. | Buffet lunch offered 1-hr post trial. Afternoon snacks were provided. Participants returned at 5:30 PM for a dinner buffet-type meal and left with a second bag of snacks for the evening. | EEEx low intensity exercise = 350.6 (11.1) kcal. EEEx high intensity exercise = 358.6 (10.3 kcal. | EI at lunchtime was significantly increased following high but not low intensity exercise compared to control. REI at lunchtime for both the high and low intensity exercise sessions was significantly lower than control. No significant between trial differences in total daily absolute or REI. |
| Stubbs et al. (2002) [89] | 6 men: Age = 31 (5); BMI = 23.3 (2.4); VO2 max = 39.5 (1.5 SEM) ml/kg/min | 9-day protocol with 3 conditions: Control: no additional exercise. Moderate exercise = 2×40 min sessions/day at 21.4 kJ/kg/day, cycle ergometer. High exercise = 3×40 min exercise session/day at 42.8 kJ/kg/day, cycle ergometer. Exercise performed on days 3–9. | On days 1–2 of the study subjects consumed a mandatory maintenance diet (estimated at 1.6×RMR). Throughout the subsequent 7 days they had ad libitum access to their normal daily diet. They weighed all food items and fluids on Portable Electronic Tape Recording Automated scales. | Total daily EE: Control = 11.7 MJ/day. Moderate exercise = 12.9 MJ/day. High exercise = 16.8 MJ/day. | There were no significant differences in total daily food, EI or macronutrient composition of the diet between treatments. |
| Stubbs et al. (2002) [87] | 6 women: Age = 23.0 (0.6); BMI = 21.4 (1.0); VO2 max = 33.4 (2.5) ml/kg/min | Same as above | Same as above | Total daily EE: EE control = 9.2 MJ/day. EEEx moderate exercise = 11.0 MJ/day. EEEx high exercise = 12.1 MJ/day. | EI was significantly higher in the high exercise treatment vs. control, but not different from the moderate exercise treatment. No significant between group differences for energy from protein; however, energy from both fat and CHO were significantly higher for the high exercise treatment vs. control. |
| Stubbs et al. (2004) [92] | 6 men: Age = 23 (2.3); BMI = 22.2 (2.4); Activity level/fitness = NR | 7-day whole room calorimeter protocol with 2 conditions: Sedentary: 2×40 min cycle ergometer sessions to increase daily energy expenditure to 1.4×RMR. Active: 3×40 min cycle ergometer sessions to increase daily energy expenditure to 1.8×RMR. | All meals provided. Food items were weighed before and after each meal. | Sedentary daily EE = 9.75 MJ. Active daily EE = 12.77 MJ. | No significant differences in EI or macronutrient intake between treatments. |
| Schneider et al. (2009) [66] | 43 sedentary women, 22 sedentary men: Age = 34.4 (10.8); BMI = 33.5 (5.5) | Control: 3 min sitting. Active: 3 min step test, up and down a 17.5 cm bench at 92 steps/min. | Participants were offered two 800 kcal portions of cookies and chips (1600 kcal total) 10 min following the trial. | EEEx = NR | No significant differences in EI between conditions. |
| Shorten et al. (2009) [84] Neutral temperature condition | 11 men: Age = 20.8 (2.1); BMI = 24.1 (2.3); VO2 max = 53.8 (8.9) ml/kg/min | Control: 40 min rest. Exercise: 40 min treadmill running at 70% VO2 peak. | Buffet breakfast offered ∼30 min post trial. | EEEx = 2375 (280) kJ | EI was significantly higher following exercise vs. control. No significant difference in REI between exercise and control. No significant difference for PRO, fat or CHO intake as percentage of total EI. |
| Staten et al. (1991) [93] | 10 men, 10 women: Age = NR; BMI = 22.1 (NR); VO2 max men = 47.3 (6.2) ml/kg/min; VO2 max women = 36.9 (6.0) ml/kg/min | 5 day protocol with 2 conditions: Sedentary: Usual daily activities. Active: 60 min of daily treadmill exercise at 70% VO2 max | All food obtained from a metabolic kitchen. | EEEx for men = 669 (126) kcal/day. EEEx for women = 441 (92) kcal/day. | Significant increase in EI for men, but not women, in the exercise vs. the sedentary condition. However, REI estimates indicated that both men and women were in negative caloric balance during the exercise period. |
| Tremblay et al. (1994) [95] | 9 men: Age = 28.3 (6.1); BMI = 23.9 (NR); VO2 max = 54.7 (6.6) ml/kg/min | Control: 60 min rest. Exercise: 60 min treadmill walk at 55–60% VO2 max. | EI over 48 hrs post trial was assessed when participants were offered low fat, high fat or mixed diet obtained from a metabolic kitchen. | EEEx = 2.8 (0.4) MJ | EI following exercise for both the low-fat and mixed-diet conditions were not different from control. However, when subjects ate the high-fat diet ad lib following exercise EI increased about 5.5 MJ/48 hr. |
| Tsofliou et al. (2003) [72] | 10 women: Age = 50.0 (8.5); BMI = 37.2 (6.5); Activity level/fitness = NR | Control: 30 min sitting. Exercise: 29 min brisk walk indoors, under supervision at ∼13 on the RPE scale. | Buffet dinner presented 1-hr post trial | EEEx = NR. Exercise HR was 123 (18) bests/min at an RPE of 14 (2). | No significant difference in EI or macronutrient intake between trials. |
| Ueda et al. (2009) [85] | 10 men: Age = 23.4 (4.3); BMI = 22.5 (1.0); VO2 max = 45.9 (8.5) ml/kg/min | Control: 30 min sitting. Exercise: 30 min recumbent cycle, moderate intensity (50% VO2 max). Exercise: 30 min recumbent cycle, high intensity (75% VO2 max). | Test meal offered 30 min post trial. | EEEx = NR | EI was significantly lower following both high and low intensity exercise vs. control. EI was not different between the moderate and high intensity trials. |
| Ueda et al. (2009) [86] | 14 men: 7 normal weight, 7 obese. Normal weight: Age = 22.4 (4.2); BMI = 22.4 (2.4); VO2 max = 46.6 (3.9) ml/kg/min. Obese: Age = 22.9 (3.4); BMI = 30.0 (3.1); VO2 max = 34.0 (6.3) ml/kg/min | Control: 60 min sitting. Exercise: 60 min cycle ergometer at 50% VO2 max. | Test meal offered 2 hrs post trial. | EEEx = NR | EI and REI was significantly lower following exercise vs control session. There were significant differences in EI and REI between normal weight and obese males, suggesting a greater energy deficit due to exercise in obese compared with normal weight men. |
| Unick et al. (2010) [53] | 19 sedentary women: Age = 28.5 (8.3 ); BMI = 32.5 (4.3) | Control: ∼40 min rest. Exercise: Treadmill walk at 70–75% of age-predicted max HR with a duration to elicit EEEx of 3 kcal/kg body weight. | Buffet of a variety of snack foods offered 60 min post trial. | EE rest = 44.3 (8.9) kcal. EEEx = 353.6 (71.9) kcal. | EI was not significantly different between control and exercise trials. REI was significantly lower following the exercise vs control. |
| Vatansever-Ozen et al. (2011) [80] | 10 men: Age = 20.1 (0.2); BMI = 23.0 (0.4); VO2 max = 62.7 (5.1) ml/kg/min | Control: 4- hrs rest. Exercise: 120 min total – 105 min at 50% max VO2 and 15 min at 70% max VO2. | Buffet meal offered 1-hr post trial. | EEEx = 230 (20) kcal. | EI was not significantly different between trials. |
| Verger et al. (1992) [67] | 5 active women: Age = Range 20–25; BMI = 19.5 (1.7). 8 active men: Age = Range 20–25; BMI = 23.4 (1.5) | Control: 3 hrs rest. Exercise: 2 hrs of non-stop athletic activities of similar intensity planned to be sub-maximal and aerobic. | Test meal offered immediately post trial or 30, 60 or 120 min post trial. | Estimated EEEx = 500 kcal. | EI for the meal consumed 60 min post exercise was significantly greater than control. EI increased as time post exercise increased. The increases from immediately post to 60 min post exercise and from immediately post to 120 min post exercise were statistically significant. Males and females responded similarly. |
| Verger et al. (1994) [83] | 58 active men: Age = Range 18–22; BMI = 21.3 (1.6) | Participants were randomly assigned to: Control (n = 30): 2 hrs rest. Exercise (n = 28): 2 hrs of non-stop, submaximal athletic activities. | Buffet meal offered 30 min post trial. | Estimated EE control = 100 kcal/hr. Estimated EEEx = 400 kcal/hr. | EI post exercise was significantly higher than control. |
| Visona et al. (2002) [62] | 36 sedentary women: Age = 26.0 (7.0); BMI = 27.0 (3.0). 3 groups of 12 representing dieting status and dietary restraint: 1. Dieter/High Restraint (D-HR) 2. Non-Dieter/High Restraint (ND-HR).3. Non-Dieter/Low Restraint (ND-LR). | Control: 60 min sitting. Exercise: 60 min treadmill walk at 60–70% max HR. | Cafeteria lunch offered 30 min post trial. 12 hr EI included the lunch plus all food consumed until bedtime on the experimental day assessed by food record. | EEEx = NR | There was a significant main effect of dieting/restraint status on lunch EI. The ND-LR group ate significantly more across the 2 trials than the D-HR group. There was a significant interaction of dieting/restraint status and condition (exercise vs. control) on 12-hr EI. The mean difference in 12-hr EI between the exercise and control day was significantly higher for the D-HR compared with the ND-HR group. |
| Whybrow et al. (2008) [88] | 6 sedentary to moderately active women: Age = 24.7 (5.9); BMI = 22.9 (1.6). 6 sedentary to moderately active men: Age = 29.7 (5.9); BMI = 24.2 (2.2) | Participants were resident in, but not confined to a human nutrition research facility for 16 days (2 days run in, 14 days active intervention). Control: Usual activity. Moderate exercise = 2×40 min sessions on a cycle ergometer to expend 28.6 kJ/kg body weight. High exercise = 3×40 min sessions on a cycle ergometer to expend 57.1 kJ/kg body weight. | All meals selected from a menu of foods prepared by the research facility. | Women: EEEx moderate trial = 2.0 MJ/day. EEEx high trial = 3.8 MJ/day. Men: EEEx moderate trial = 2.8 MJ/day. EEEx high trial = 4.9 MJ/day. | Women: No significant between trial differences in average daily EI or macronutrient composition. Men: Average daily EI and energy from carbohydrate, fat and protein increased significantly with increased EEEx. |
Note, Values are means (standard deviation) unless otherwise noted. Abbreviations: CHO = carbohydrate; EEEx = exercise energy expenditure; EI = energy intake; NR = not reported; PRO = protein; REI = relative energy intake; kcal = kilocalories; MJ = megajoules; KJ = kilojoules; hrs = hours; min = minutes; wk = week.
Acute Studies: Study Characteristics
Sample size
The median (range) sample size across the 40 acute studies was 12 (7–65).
Exercise intensity/duration
The median (range) exercise intensity was 70% (60–75%) of HRMax, and 70% (30–75%) of maximal oxygen uptake. Five studies did not provide information on exercise intensity. The median (range) exercise duration was 50 min (3–90 min). Four acute studies dosed exercise by level of energy expenditure [51]–[54].
Energy intake assessment
Single ad-libitum test meals with energy intake assessed by the weigh and measure technique were utilized in the majority (25/40, 63%) of acute studies. Multiple ad-libitum meals [52], [55]–[58], a combination of ad-libitum meal plus energy intake over the rest of the day by recall [54], [59]–[62], diet recalls alone [63], and the consumption of specific food items, e.g. sandwiches [64], pasta salad [65] or cookies and chips [66] were also utilized.
Interval between end of exercise and energy intake assessment
Eleven acute trials assessed energy intake over the entire exercise day [52], [54]–[63]. In the remaining 29 acute studies, energy intake was assessed on one occasion with a median (range) of 30 minutes (immediate-330 min) post-exercise.
Acute Studies: Participant Characteristics
Age
The median (range) age across the 36 studies that reported age was 23 (20.1–50) years.
Gender
Six studies included both men and women [64]–[68], 15 included women only [52]–[54], [62], [63], [69]–[76] and 19 studies included only men [51], [55]–[61], [77]–[86].
BMI
The median (range) BMI across 39 studies that reported BMI was 22.9 (19.8–37.2) kg/m2. Five of 40 studies (∼13%) included overweight or obese participants [53], [66], [72], [73], [85], [86].
Minority status
No studies described the racial or ethnic composition of the study sample or reported post-exercise energy intake by race or ethnicity.
Participant activity level
Participants recruited for the majority of acute studies (24/40–60%) were physically active and/or aerobically fit [51], [52], [54]–[60], [65], [67], [70], [71], [74], [76], [77], [79]–[84]. Eleven studies (∼28%) recruited sedentary or moderately active participants [53], [62], [63], [66], [68], [69], [73], [75], [85], [86] while 5 studies (∼13% ) did not describe baseline participant physical activity [61], [64], [72], [78].
Acute Studies: Results
Energy intake
Nine of 40 acute studies (∼23%) [52], [62], [64], [65], [67], [68], [70], [83], [84] reported a significant increase in absolute energy intake (∼80 to 470 kcal/day) following exercise compared with non-exercise control while 27 studies (∼68%) found no difference in absolute energy intake between exercise and control conditions [51], [53]–[61], [63], [64], [66], [69], [72]–[77], [79]–[82]. Four studies (10%) reported a significant decrease in absolute energy intake (∼125 to 240 kcal/day) following exercise compared with non-exercise control [75], [78], [85], [86]. Fifteen studies (∼38%) reported a significant decrease in relative energy intake (energy intake - exercise energy expenditure) following exercise compared with control [51]–[53], [55], [57]–[59], [65], [68], [70], [71], [76], [79], [84]–[86]; 5 of those studies also reported significant increases in absolute energy intake [52], [65], [68], [70], [84] suggesting only partial compensation in energy intake following acute exercise.
Macronutrient intake
Sixteen of the 40 acute studies (40%) reported data on macronutrient intake [54]–[58], [60], [68], [72], [76]–[79], [82], [84]. Fifteen studies showed no effect, while one study indicated significantly higher fat and protein intake following exercise compared with non-exercise control [76].
Effect of Study Parameters on Energy Intake
Exercise mode
Three studies provided information relative to the effect of exercise mode on post-exercise energy intake. Balaguera-Cortes et al. [77] reported no effect of either aerobic (treadmill) or resistance exercise while King et al. [56] showed no effect of swimming on absolute post-exercise energy intake. These results are in contrast to those of Laan et al. [65] who showed an increase in absolute post-exercise energy intake following both aerobic (cycling) and resistance exercise; however, relative energy intake was lower following aerobic exercise compared to resistance exercise or control.
Exercise intensity
Six acute studies reported the effect of exercise intensity on post-exercise energy intake. Four studies found no effect of exercise intensity on absolute energy intake following exercise [51], [60], [64], [85]; however, Imbeault et al. [51] reported a lower relative energy intake following high intensity exercise (75% VO2 max) compared with low intensity exercise (35% VO2 max) or non-exercise control. One study [52] showed a significant increase in absolute energy intake for high (70% VO2 peak) but not low intensity exercise (40% VO2 peak); however relative energy intake was lower in both the high and low intensity exercise groups compared with non-exercise controls. One study reported a significant decrease in absolute energy intake following strenuous (40 min/90 W cycle ergometer) but not moderate exercise (40 min/30 W cycle ergometer) in non-obese but not in obese women [75].
Exercise duration
Two studies evaluated the role of exercise duration on post-exercise energy intake with divergent results. King et al. [60] reported no effect of exercise duration on post-exercise energy intake; however, Erdman et al. [64] reported that absolute energy intake was not significantly greater than control following cycle ergometer exercise bouts of 30 and 60 min, but was significantly greater than control following 120 minutes of exercise.
Exercise time of day
Two studies evaluated the effect of the time of day of aerobic exercise on post-exercise energy intake [55], [63]. Both studies found no significant difference in absolute post-exercise energy intake between exercise performed in the morning (7 and 8:15 AM) compared to the same exercise performed in the evening (5 and 7:15 PM). However, O'Donoghue et al. [55] showed that relative energy intake at breakfast was lower after morning exercise compared with afternoon exercise or control while relative energy intake at dinner was lower post afternoon exercise compared with control.
Composition of test meals
Four studies evaluated the effect of the macronutrient composition of the test meal on post-exercise energy intake. Three studies found no significant differences in absolute post-exercise energy intake compared to rest between low or high fat test meals [70], [71], [74]. King et al. [59] found no difference in absolute post-exercise energy intake when either high fat/low carbohydrate or low fat/high carbohydrate test meals were presented; however, relative energy intake was significantly lower in the low fat/high carbohydrate, but not the high fat/low carbohydrate condition compared with control.
Time between the end of exercise and the presentation of the test meal
In the one acute study that investigated the effect of time between exercise and presentation of the test meal on energy intake, Verger et al. [67] showed that absolute energy intake increased as the time post-exercise that the test meals were presented increased (immediate to 120 min).
Effect of Participant Characteristics on Energy Intake
Age
No studies evaluated the effect of age on post-exercise energy intake. Studies were generally conducted in young adults with a median age of 23 years.
Gender
Although 6 studies included both men and women [64]–[68] the data were presented separately in only one study. Verger et al. [67] showed significant increases in absolute EI following exercise (2 hours of non-stop submaximal aerobic athletic activities) in both men and women.
Weight status
Three studies provided data on the effect of weight status on post-exercise energy intake [73], [75], [86]. George et al. [73] found non-significant differences in absolute post-exercise energy intake between normal and overweight women. Kissileff et al. [75] reported significant decreases in post-exercise energy intake in non-obese, but not obese women, while Ueda et al. [86] found larger energy deficits (i.e. decreased energy intake) induced by exercise in obese compared with normal weight men.
Weight/Diet/Dietary restraint
Three studies evaluated the effect of combinations of weight, dieting status or level of eating restraint on post-exercise energy intake. Harris et al. [61] found no differences in post-exercise energy intake in a sample of men across 5 groups: 1) normal weight/low dietary restraint/non-dieting; 2) normal weight/high dietary restraint/non-dieting; 3) overweight/low dietary restraint/non-dieting; 4) overweight/high dietary restraint/non-dieting; and 5) overweight/high dietary restraint/dieting. In a sample of normal weight young women, Lluch et al. [70] found increased absolute post-exercise energy intake in women classified as unrestrained eaters and decreased energy intake in restrained eaters. Relative energy intake compared with rest was greater in restrained compared with unrestrained eaters. Visonia et al. [62] demonstrated a significant interaction between dieting/eating restraint status and study condition (exercise vs. control) on 12-hour energy intake in sample of women. The mean difference in 12-hour energy intake between the exercise and control day was significantly higher for the dieting-high restraint group compared with the non-dieting high restraint group.
Activity level
Two studies evaluated the effect of activity level on post-exercise energy intake. Jokisch et al. [78] showed a significant decrease in post-exercise energy intake compared with control in inactive but not in active men. Larson-Meyer et al. [76] found non-significant differences between post-exercise energy intake and control in a normal weight sample of both habitual walkers (≥3 days/wk for ≥60 min/day) and habitual runners (≥32 km/wk); however, relative post-exercise energy intake was significantly lower in runners compared with controls, but not in walkers vs. controls.
Short-Term Studies
The 10 short-term studies comprised ∼9% of the total studies identified for this review (Table 2). These studies employed cross-over designs that compared energy intake assessed over a time frame of 2–14 days during which participants engaged in exercise with energy intake during an equivalent period of no imposed exercise.
Short-Term Studies: Study Characteristics
Sample size
The median (range) sample size for the 10 short-term studies was 9.5 (6–20)
Trial length
The median (range) duration of short-term studies was 8 (2–14) days.
Exercise intensity/duration
One study prescribed exercise intensity at 70% of heart rate max (HRMax). Five studies prescribed intensity relative to VO2 max (median [range] 60% [44–75%]). Three studies did not report exercise intensity relative to VO2 or HRMax [19], [87], [88]. Eight of 10 short-term studies (80%) dosed exercise by energy expenditure; 3 relative to body weight [87]–[89], 3 relative to resting or baseline daily energy expenditure [90]–[92], and 2 to an absolute exercise energy expenditure goal [93], [94]. Two studies prescribed exercised by time that ranged from 60 [93] to 100 min/day [94]. Prescriptions ranged from 21.4 [89] to 57.1 kJ/kg body weight [88], 1.4 to 1.8 times RMR [92], 12.5% [90] to 29% above baseline total energy expenditure [91] and net exercise energy expenditure from 2.8 [95] to 2.98 MJ/day [96].
Energy intake assessment
Seven studies used weigh and measured meals provided by a metabolic kitchen [88], [90]–[93], [95], [96] 3 used weigh and measure food records [87], [89], [94].
Short-Term Studies: Participant Characteristics
Age
The median (range) for age across all short-term studies was 28.3 (23–35) years.
Gender
Two studies (20%) included both men and women [88], [93], 3 (30%) included women only [87], [90], [91] and 5 studies (50%) included only men [89], [92], [94]–[96].
BMI
The median (range) BMI was 23.5 (21.4–28.2) kg/m2. Three of 10 studies (30%) had a mean sample BMI in the overweight category (i.e. ≥25 kg/m2) [90], [91], [96].
Minority status
No studies describe the racial or ethnic composition of the study sample or reported an association between exercise level and energy intake by race or ethnicity.
Participant activity level
Participants recruited for the majority of short-term studies (7/10 - 70%) were sedentary or moderately active [87]–[90], [92], [93], [96]. Two studies (20%) recruited active participants [94], [95] while one study (10%) did not describe baseline participant physical activity [91].
Short-Term Studies: Results
Energy intake
Five of 10 short-term studies (50%) reported increased absolute energy intake (∼200–335 kcal/day) over periods of 2 to14 days when exercise was imposed compared with a non-exercise control period [87], [88], [93], [95], [96]. Three studies that reported increased absolute energy intake showed relative energy intake at a level to maintain a negative energy balance during the exercise period [87], [88], [93]; however, Tremblay et al [95] showed that participants achieved a positive energy balance when presented with a high fat diet.
Macronutrient intake
Seven of the 10 short-term studies (70%) reported macronutrient intake [87]–[90], [92], [94], [96]. Four of 7 studies (57%) showed no effect of exercise on macronutrient intake [89], [90], [92], [94]. Farah et al. [96] reported increased intake of carbohydrate and protein while Stubbs et al. [87] observed increased intake of carbohydrate and fat with exercise compared to control. Whybrow et al. [88] noted increased intake of carbohydrate, fat and protein with exercise vs. control in men but not in women.
Effect of Study Parameters on Energy Intake
Exercise mode
The one study that compared the effect of aerobic and resistance exercise reported no significant difference between exercise and control for short-term energy intake during either aerobic or resistance training [91].
Level of exercise energy expenditure
Four studies evaluated the effect of increased levels of exercise energy expenditure on short-term energy intake [87]–[90]. Levels of energy compared were 12.5% vs. 25% above baseline energy expenditure [90], 21.4 vs. 42.8 kJ/kg/day [87], [89] and 28.6 vs.57.1 kJ/kg/day [88]. Three studies observed no effect [87], [89], [90]. The study by Whybrow et al. [88] reported increased short-term energy intake associated with higher levels of exercise energy expenditure (57.1 vs. 28.6 kJ/kg/day) in men but not in women.
Exercise intensity
No studies evaluated the effect of exercise intensity on short-term energy intake.
Composition of test meals
The one study that compared the effect of the composition of test meals (mixed, high fat, low fat) on short-term energy intake noted increased energy intake when high fat, but not low or mixed fat meals were presented [95].
Effect of Participant Characteristics on Energy Intake
Age
No short-term studies evaluated the effect of age on post-exercise energy intake. Studies were generally conducted in young adults with a median age of 28.3 years.
Gender
Results from the two studies that evaluated gender differences in short-term energy intake with exercise reported that absolute energy intake increased in men but not in women [88], [93]. Results from 2 separate studies that used identical exercise and energy intake protocols in samples of men [89] and women [87] found increased energy intake with exercise in women, but not in men.
Other participant characteristics
No studies evaluated the effect of weight, physical activity or level of dietary restraint on short-term changes in energy intake induced by exercise.
Non-Randomized Trials
The 12 non-randomized trials comprised ∼12% of the total studies identified for this review (Table 3). Most trials (11/12) evaluated changes in energy intake in a single group (no control) assigned to complete a longitudinal exercise training program [18], [21], [97]–[105] while one study observed differences in energy intake between women who participated in an 8 week exercise program at a commercial exercise facility with a group of non-exercise volunteer controls [106].
Table 3. Non-Randomized Trials.
| Study | Participants | Trial Length | Exercise Prescription/Intervention | Diet Assessment | Results: Exercise | Results: Diet |
| Andersson et al. (1991) [101] | 22 women: Age = 36 (1.4) years; BMI = 24.6 (0.3); VO2 max = 33.9 (NR) ml/kg/min. 9 men: Age = 37 (2.4) years; BMI = 25.7 (0.4); VO2 max = 42.0 (2.8) ml/kg/min | 12 wks | Supervised 60 min sessions of gym activity, 3 times/wk. Interval training - lighter intensity exercise (jogging, coordination, strength) with 3–5 min periods at 80% max work capacity. | Diet history at baseline, mid and end study. | EEEx or other data on exercise adherence were NR | No significant change in EI for lean women (n = 15, mean body fat 24.8 kg). EI was significantly decreased in obese women (n = 7, mean body fat 31.3 kg). No significant change in EI for men |
| Bryant et al. (2012) [103] | Total sample (39 women & 19 men): Age = 35.6 (9.8) years; BMI = 31.8 (4.5); VO2 max = 29.1 (5.7) ml/kg/min) | 12 wks | Supervised sessions of cycle ergometer exercise, 5 days/wk at 70% VO2 max for a duration designed to expend 500 kcal/session. | EI intake was measured during probe days every 4 weeks. EI was calculated by weighing food before and after consumption. | EEEx or other data on exercise adherence were NR | No significantly change in EI over the course of the intervention. |
| Caudwell et al. (2013) [104] | 72 women: Age = 40.6 (9.5); BMI = 31.8 (4.3); VO2 max = 28.9 (NR) ml/kg/min. 35 men: Age = 41.3 (8.6) years; BMI = 30.5 (8.6); VO2 max = 34.7 (NR) ml/kg/min | 12 wks | Supervised exercise 5 days/wk at 70% HR max with a duration designed to expend ∼10.5 MJ/wk. Mode: choice of treadmill, cross-trainer, rowing or cycle ergometers. | Test meals in the lab at baseline and 12 wks. After an individualized fixed-energy breakfast (ad libitum on the first visit), participants were provided with a fixed-energy lunch, an ad libitum dinner meal, and a snack box for the evening. | Total EEEx over 12 wks was 122.8 (20.9) MJ for men and 115.3 (15.1) MJ for women, NS. Average exercise session for men was 43 (8.7) min and 54 (10.2) min for women. | No significant change in EI for either women. No significant change in EI for either men |
| Di Blasio et al. (2012) [105] | 41 women (34 completed intervention). Completer data: Age = 55.9 (3.6); BMI = 26.9 (4.2); VO2 max = 27.0 (5.0) ml/kg/min | 13 wks | Group walks, 4 days/wk. Month 1: 40 min at RPE 11 on 15 point scale. Month 2: 50 min/RPE 11. Month 3: 50 min/RPE 13. 2 of 4 sessions/wk were supervised. | 3–day food records (2 weekdays and 1 weekend day) collected at baseline and 13 wks. | Attendance at exercise sessions was 85 (10.8)%. No significant increase in total or PA EE (SenseWear Armband) between baseline and 13 wks. | No significant change in EI or % of energy from fat, CHO or PRO. |
| Keytel et al. (2001) [106] | 19 women (non-randomized observation of 9 exerciser and 10 non-exercisers). Exercisers: Age = 58 (7) years; BMI = 25.1 (2.7); VO2 max = 1.87 (0.42) L/min. Non-exercisers: Age = 55 (5) years; BMI = 26.6 (4.3); VO2 max = 1.96 (0.42) L/min. | 8 wks | Exercise: New participants in a commercial walk/run exercise program; met 3 days/wk. Started walking 3 km and progressed to walk/jog between 3–6 km at 70–75% of age predicted max HR. Non-exercise: Volunteers recruited by media and investigator. Told no to make major lifestyle changes. | 1–24 hr recall at baseline and 2 at 8 wks. | No difference in total daily EE across 8 wks. in either the exercise or control group. Activity diary data indicated significantly greater levels of PA in exercise vs. control for sedentary, active and very active categories. | No significant change in EI or % of energy from fat, CHO or PRO. |
| King et al. (2008) [18] | 35 total (25 women &10 men): Age = 39.6 (11) years; BMI = 31.8 (4.1); VO2 max = 28.6 (5.7) ml/kg/min | 12 wks | Supervised exercise, 5 days/wk at 70% max HR, duration to expend ∼500 kcal/session. Mode: cycle ergometer, stepper, rowing ergometer or treadmill. | Test meals (lunch/dinner) on 1 day at baseline and 12 wks. | Attendance at exercise sessions was 82%. EEEx was 2333 kcal/wk. | No significant change in EI or % of energy from fat, CHO or PRO. |
| Koulouri et al. (2006) [97] | 12 total (7 women & 5 men) active participants enrolled.10 completers: Age = 28.3 (6.0) years; BMI = 22.3 (3.3). | 3 wks | 1 wk habitual activity followed by 2 wks of advice to increase walking by 2000 steps/day. | Daily food diaries over the 3 wk study period. | During the exercise period steps/day (pedometer) increased by 2, 677; EE (diary) increased 30 kJ/day, and EE (activPAL) increased 100 kJ/day. | No significant change in EI between baseline and the intervention period. |
| Manthou et al. (2010) [21] | 34 women: Age = 31.7 (8.1) years; BMI = 29.3 (4.3); VO2 max = 2.1 (0.38) L/min. | 8 wks | 150 min of supervised cycle ergometer exercise at 72–77% of age-predicted max HR in one of 2 patterns: 75 min 2 days/wk (n = 18) or 30 min 5 days/wk (n = 16) | 7-day weighed food record at baseline and 8 wks. | Compliance with exercise was 100%. EEEx = 30.2 (12.6 MJ) over the intervention. | EI increased significantly from baseline to 8 wks. No significant changes in energy from fat, CHO or PRO. Differences in EI or macronutrient intake between exercise patterns was not presented. |
| Martins et al. (2010) [98] | 22 total (Completer: 7 women & 8 men): Age = 36.9 (8.3) years; BMI = 31.3 (2.3); VO2 max = 32.9 (6.6) ml/kg/min | 12 wks | Supervised treadmill walking or running 5 days/wk at 75% max HR to induce and energy deficit of 500 kcal/session. | 3-day food record (at least 1 weekend day) at baseline and 12 wks. | Average attendance at exercise sessions = 89 (5.9)% | No significant change in EI or macronutrient intake. |
| Snyder et al (1997) [99] | 13 women (15 started): Age = 43 (11); BMI = 32.5 (8.0); VO2 max = 24.0 (4.6) ml/kg/min | 32 wks | Walking (in and outdoors) 10 min bouts, 3 times/day, 5 days/wk. at 50–67% HRR. 3 of 5 sessions/wk were supervised. | 3-day food record at baseline and 32 wks; 24- hr. recalls at 11 and 22 wks. | Adherence to exercise = 82.6 (10)%. Total estimated EEEx = 81843 (21014) kJ. | No significant change in EI or macronutrient intake. |
| Suzuki et al. (1998) [102] | 31 women: Age = 19.2 (0.2 SEM) years; BMI = 21.5 (1.2 SEM); VO2 max = 36.2 (1.1) ml/kg/min | 12 wks | Supervised cycle ergometer exercise, 30 min/day, 5 days/wk at 40% VO2 max. | Daily weighed food records analyzed weekly. | EEEx = 117.3 (3.1 SEM) kcal/session. | No significant change in EI or macronutrient intake between baseline and the training period. |
| Westerterp et al. (1992) [100] | 32 total (16 women &16 men) sedentary participants enrolled: Age range = 28–41 years; BMI range = 19.4–26.4. 5 women and 4 men did not complete the intervention. | 44 wks | Supervised training (running), 4 sessions/wk. With increasing running time to 10–30 min, 20–60 min and 30–90 min/session after 8, 20 and 40 weeks respectively. Goal of running a half marathon. | 7-day weighed food records at baseline, 8, 20 and 40 wks. | Median PA index (daily EE/sleep EE) increased over the intervention. | No significant changes in or nutrient composition of the diet were detected. |
Note, Values are means (standard deviation) unless otherwise noted. Abbreviations: CHO = carbohydrate; PA = physical activity; EE = energy expenditure; EI = energy intake; NR = not reported; PRO = protein; REI = relative energy intake; kcal = kilocalories; KJ = kilojoules; MET = Metabolic equivalent of task; hrs = hours; min = minutes; wk = week.
Non-Randomized Trials: Study Characteristics
Sample size/completion rate
The median (range) sample size across the 12 non-randomized trials was 31 (10–107). The median (range) rate of trial completion in the 5 trials that provided data on this parameter was 83% (68–87%) of participants who started the intervention [97]–[100], [105].
Trial length
The median (range) length of non-randomized trials was 12 (3–44) weeks.
Exercise mode
Six of 12 non-randomized trials involved laboratory based aerobic exercise conducted on cycle ergometers/rowers/steppers/treadmills [18], [21], [98], [102]–[104], 5 trials employed indoor or outdoor walking [97], [99], [100], [105], [106]while one trial required participants to complete a combination of gym activities (jogging/coordination/resistance) [101].
Exercise supervision
All exercise sessions were supervised in 8 trials [18], [21], [98], [100]–[104], partially supervised in 3 trials [99], [105], [106] and unsupervised in one trial [97].
Exercise prescription (frequency)
The median (range) exercise frequency was 5 (2–5) days/week.
Exercise prescription (intensity)
Three trials prescribed intensity as a percentage of maximal VO2 [101]–[103], 5 by percentage of HRMax [18], [21], [98], [104], [106], one by heart-rate-reserve [99] and one by ratings of perceived exertion [105]. The median (range) of intensity prescriptions were: 40% (40–80%) max VO2; 73% (70–75%) HRMax, 59–67% heart-rate-reserve; and perceived exertion 11–13 on a 15 point scale. Prescribed exercise intensity was not reported in 2 trials [97], [100].
Exercise prescription (duration)
Six trials prescribed exercise duration by time [21], [99]–[102], [105], 4 by level of exercise energy expenditure [18], [98], [103], [104], one by walking distance [106] and one by pedometer steps/day [97]. The median (range) duration for the 6 trials prescribing exercise by time was 40 (30–60) min/day. All 4 studies prescribing exercise by energy expenditure assigned 500 kcal/exercise session. Prescribed walking distance was 3–6 km/day, and pedometer steps were to increase steps by 2,000 per day above baseline over 2 weeks.
Compliance with the exercise protocol
Seven studies presented data relative to participant compliance with the exercise protocol [18], [21], [97]–[99], [104], [105]. Five trials reported the percentage of exercise sessions attended (range 82–100%) [18], [21], [98], [99], [105], 1 reported the level of exercise energy expenditure (prescribed 10.5 MJ/wk; achieved 9.9 MJ/wk) [104] and one trial reported pedometer steps/day (prescribed 2,000; achieved 2,677 steps/day) [97].
Energy and macronutrient assessment
Five trials used non-weighed food records [97], [98], [100], [101], [105], 2 used weighed food records [21], [102], 3 used test meals [18], [103], [104], 1 used 12 hour recall [106] and one used a combination of food records and 24-hour recalls [99]. Six studies assessed energy intake at baseline and end [18], [21], [98], [101], [104], [105], 3 studies completed energy intake assessments at 4 time points [99], [100], [103], one study at 3 time points [106] while 2 studies collected daily estimates of energy intake over the course of the intervention [97], [102].
Non-Randomized Trials: Participant Characteristics
Age
The median (range) age across all non-randomized trials was 36.9 (19.2–56) years.
Gender
Seven studies (58%) included both men and women [18], [97], [98], [100], [101], [103], [104] while 5 studies (42%) included women only [21], [99], [102], [105], [106].
BMI
The median (range) BMI was 29.3 (21.5–32.5) kg/m2. Five of 12 studies (42%) had a mean sample BMI in the overweight category (i.e. ≥25 kg/m2) [21], [100], [101], [105], [106], while the mean sample BMI was classified as obese (i.e. ≥30 kg/m2) in 5 trials [18], [98], [99], [103], [104] and normal weight (i.e. BMI<25 kg/m2) in 2 trials [97], [102].
Minority status
No non-randomized trials described the racial or ethnic composition of the study sample or reported an association between exercise level and energy intake by race or ethnicity.
Participant activity level
Eleven of 12 non-randomized trials described inclusion criteria for level of baseline physical activity or aerobic fitness. With the exception of the trial of Koulouri et al. [97] who recruited regularly active participants, non-randomized trials were conducted in participants categorized as sedentary [18], [21], [98], [100], [102], [103], [105], [106]or with low aerobic fitness [99], [104].
Non-Randomized Trials: Results
Energy intake
Eleven of 12 (92%) of non-randomized trials reported no change in energy intake in response to exercise training [18], [97]–[106]. One non-randomized trial reported a significant increase in energy intake (∼84 kcal/day) as a result of participating in an exercise training program [21].
Macronutrient intake
None of the 8 non-randomized trials that evaluated the effect of exercise training on macronutrient intake reported significant change in the intake of carbohydrate, fat or protein [18], [21], [98]–[100], [102], [105], [106].
Effect of Study Parameters on Energy Intake
Exercise mode
No studies evaluated the effect of exercise mode on changes in energy intake in response to exercise training.
Level of exercise energy expenditure/duration
No studies evaluated the effect of exercise energy expenditure/duration on energy intake in response to exercise training.
Exercise intensity
No studies evaluated the effect of exercise intensity on energy intake in response to exercise training.
Composition of test meals
Three non-randomized trials evaluated energy intake using test meals [18], [103], [104]; however, the effect of variations in the macronutrient composition of the test meals was not evaluated.
Effect of Participant Characteristics on Energy Intake
Age
No studies evaluated the effect of age on changes in energy intake in response to exercise training.
Gender
Three non-randomized trials provided data on gender differences [100], [101], [104]. Two trials reported no differences for change in energy intake between men and women in response to exercise training [100], [104], while one trial found no effect in men or lean women, and a significant decrease in energy intake with exercise training in obese women [101].
Other participant characteristics
No non-randomized trials were identified that specifically evaluated the effect of weight status, level of physical activity or level of dietary restraint on the energy intake response to exercise training.
Randomized Trials
The 24 randomized trials constituted ∼24% of the total number of studies identified for this review (Table 4). The majority of trials (16/24; ∼67%) evaluated the effect of exercise training on energy and macronutrient intake between participants randomized to exercise compared with non-exercise controls [107]–[122]. The effect of specific exercise training parameters on energy intake including mode (resistance/resistance plus aerobic/swim) [118]–[120], [123], [124], intensity [124]–[127], volume [116], [121], [122] and timing (intermittent vs. continuous) [128] were also reported. The majority of randomized trials employed an efficacy design; however, reports from Jakicic et al. [122] and Foster-Schubert et al. [110] employed an intent-to-treat design, and Rosenkilde et al. [121] reported both efficacy and intent-to-treat results.
Table 4. Randomized Trials.
| Study | Participants | Length | Intervention/Groups | Diet Assessment | Results: Exercise | Results: Diet |
| Bales et al. (2012) [123] | 117 sedentary men and women in 3 groups: Aerobic training (AT) 19 men/20 women: Age = 53 (NR); BMI = 30.1 (NR); Resistance training (RT) 18 men/20 women: Age = 48.5 (NR); BMI = 30.4 (NR). Aerobic+Resistance training (AT/RT) 18 men/22 women: Age = 47 (NR); BMI = 30.2 (NR) | 8 mos | AT: Calorically equivalent to approximately 12 miles/wk at 65%–80% VO2 peak) treadmill, elliptical and cycle ergometer. RT: 3 days/wk., 3 sets, 8–12 reps. RT program began with one set of each exercise during the first 2 wks., followed by two sets during weeks 3 and 4, and reaching the goal of 3 sets at week 5. AT/RT: Linear combination of both exercise prescriptions. | 2 EI assessment methods were used at baseline and end study: 1) Combination of 3-day food records (2 wk days/1 wk end day) and unannounced 24 hr. recall. (QDI). 2) Block Food Frequency Questionnaire (FFQ). | Adherence to exercise treatment: AT = 90.1%; RT = 82.9%; AT/RT = 83.3%/82.0% | FFQ results: Significant decreases in absolute EI, and the intake of CHO, fat and PRO for both the AT and AT/RT groups. QDI results: Changes were non-significant; except a significant decreased in absolute fat intake for RT. When EI was expressed relative to body mass, results were similar, i.e., significant decreases EI for AT and AT/RT (FFQ results), with no change in RT. |
| Brandon & Elliott-Lloyd (2006) [107] | 52 women: Exercise = 15 African American: Age = 34 (7.2); BMI = 34.4 (8.2); VO2 max = 31.4 (5.2) ml/kg/min; 13 White: Age = 40.5 (7.1); BMI = 29.5 (5.7); VO2 max = 32.3 (6.0) ml/kg/min. Control = 12 African American: Age = 36 (8.4); BMI = 33.0 (7.1); VO2 max = 30.8 (4.5) ml/kg/min. 12 White: Age = 42 (9.7); BMI = 32.8 ( 7.3); VO2 max = 32.3 (6.0) ml/kg/min | 2 wk run-in period, 16 wks at walking goal. Studied only women who were able to walk 3 miles/session after the 2 wk run-in period. | Control: No exercise. Exercise: Supervised brisk walking in groups, 3 days/wk., 3 miles/session, outdoors (indoor track or treadmill in bad weather). Self-paced intensity. Goal was to walk 3.5 mph pace. | 2-day food record (Sunday and Monday) at study wks. 1, 9 and 16. | Exercise Adherence: African American = 86%; White = 90%. Pace: African American = 3.54 mph; White = 3.61 mph. Retention rate was higher in Whites (74%) vs. African American (45%) based on performance in the run-in period. | African American: EI significantly increased from baseline to wk 16. CHO intake (g/day) increased, no change in fat or PRO intake. Whites: Reductions in EI below baseline at both wks 9 (12.7%) and wk. 16 (5.1%) were observed, statistically significant at wk. 8 only. CHO intake decreased significantly (wk. 9), no change in fat or PRO intake. |
| Broeder et al. (1992) [108] | 64 men randomized. Control, n = 20; Endurance, n = 22; Resistance, n = 22. 47 men completed the study. Control n = 19; Age = 18–35; BMI = 25.3 (1.0); VO2 max = 49.1 (2.2) ml/kg/min. Endurance, n = 15; Age = 18–35; BMI = 25.1 (1.1); VO2 max = 49.6 (2.2) ml/kg/min. Resistance, n = 13; Age = 18–35; BMI = 25.5 (1.1); VO2 max = 48.1 (1.5) ml/kg/min | 12 wks | Endurance training: Supervised walk/jog program, 4 days/wk progressed to 40 min at a minimum intensity of 70% VO2 max by wk 4. After wk 8, each person was exercising for 50 min at between 70% and 85% VO2 max. Resistance training: Supervised free weights/machines, 4 days/wk. (2 days upper and 2 days lower body), 3-sets, 11 exercises. | 3-day food records at baseline, and wks 6, 7 and 12. Recording days randomly assigned but always included 2 week days and 1 weekend day. | Exercise groups each subject completed ≥90% of scheduled workout sessions. | No significant change in EI for any study group. No significant between group differences between the mid and post-treatment periods for the percentage of kcal derived from CHO, fat or PRO. |
| Bryner et al. (1997) [125] | 25 women randomized, 15 women completed study. Low intensity = 7 women: Age = 24.9 (4.6); BMI = 23.6 (NR); VO2 max = 36.2 (4.7) ml/kg/min. High intensity = 8 women: Age = 24.2 (6.0); BMI = 23.2 (NR); VO2 max = 29.2 (5.7) ml/kg/min | 16 wk trial, 12 wk active intervention. | Supervised walk/jog, 40–45 min/day, 4 days/wk at either low or high intensity. Low intensity: 60–70% max HR. High intensity: 80–90% max HR | 7-day food records, monthly. | Low intensity group: Exercise day/wk = 4.2 (0.47). Min/day = 46 (10.2); HR = 131.6 (7.6). High intensity group: Exercise day/wk = 3.9 (0.3); Min/day = 43 (9.3); HR = 162.8 (9.5) | No significant change in EI or CHO, fat or PRO intake for either group. |
| Cox et al. (2010) [124] | 116 women. Walk group (60 women): Age = 55.2 (4.8); BMI = 26.4 (3.5); VO2 max = 27.5 (4.1) ml/kg/min. Swim group (56 women): Age = 55.8 (4.5); BMI = 26.3 (3.0); VO2 max = 27.5 (4.2) ml/kg/min. 42 walk and 44 swim group completed 12 mos. assessments for a retention rate of 74%. | 12 mos | 6 mos. supervised and 6 mos. unsupervised exercise. Walk: 30 min/session, 3 days/wk. at 60–70% HRR, on a track or around a park. Swimming: 30 min/session, 3 days/wk. at 60–70% HRR. Unsupervised exercise at a venue of choice. Half of women received a behavioral intervention package to encourage adoption and adherence to exercise, the other half received standard exercise information of “usual care” | FFQ at baseline, 6 and 12 mos which assessed nutrient intake for the previous 3 mos. | Exercise min/wk. at 6 mos. Walk = 122 min/wk. Swim = 126 min/wk. Exercise min/wk at 12 mos. Walk = 116 min/wk.Swim = 117 min/wk. | EI was unchanged, with no significant between-group differences after 6 or 12 mos. |
| Cox et al. (2003) [129] Normal Diet Arm | Light exercise (17 men): Age = NR; BMI = 29.7 (3.4); VO2 max = 2.4(range 2.2–2.6) L/min. Vigorous exercise (13 men): Age = NR; BMI = 30.5 (3.9); VO2 max = 2.6 (range 2.4–2.8) L/min. Mean age total sample = 42.4 (5.0). | 16 wks | Supervised exercise 30 min/session, 3 days/wk. Light exercise: Slow flexibility exercises 1 day/wk. and stationary cycling (zero resistance) 2 days/wk. Vigorous exercise: Stationary cycling at 60%–70% HRR. | 3-day food records completed every 2 wks. | Exercise intensity: Light exercise = 18% HRR. Vigorous intensity = 76% HRR. EEEx ranged from 1,507 to 1,758 kJ/session. | No significant change in EI or % of energy from CHO, fat or PRO in either the light or vigorous exercise groups. |
| Church et al. (2009) [16] | 411 women. Control (94 women): Age = 57.2 (5.9); BMI = 32.2 (3.9); VO2 max = 15.7 (2.0) ml/kg/min. Exercise 4 kcal/kg/wk (KKW):139 women: Age = 57.9 (6.5); BMI = 31.4 (3.7); VO2 max = 15.5 (2.9) ml/kg/min. Exercise 8 KKW (85 women): Age = 56.7 (6.4); BMI = 32.2 (4.1); VO2 max = 15.1 (2.2) ml/kg/min. Exercise 12 KKW (93 women): Age = 56.4 (6.3); BMI = 31.1 (3.6); VO2 max = 16.1 (2.8) ml/kg/min | 6 mos | Control: no exercise. Exercise groups: 3–4 sessions/wk. at 50% VO2 max designed to achieve EEEx of 4, 8 and 12 KKW. Exercise alternated between semi-recumbent cycle ergometers and treadmills. | EI at baseline and end study was assessed using the Food Intake and Analysis System semi-quantitative food frequency questionnaire. | Exercise adherence: 4 KKW = 99.5%; 8 KKW = 99.3%; 12 KKS = 99.2%. Exercise min/wk.: 4 KKW = 72.2 (12.4); 8 KKW = 136.3 (19.4); 12 KKW = 193 (31). Total EEEx completed (kcal): 4 KKW = 7932; 8 KKW = 15197; 12 KKW = 20560 | No significant between group differences in mean EI at either baseline or end study. For all groups the mean EI was significantly lower at end study compared to baseline. There were no between groups difference in baseline or follow-up in dietary PRO, fat and CHO intake. |
| Donnelly et al. (2003) [9] | 131 men/women randomized; 74 men/women completed the study (56.5%). Control = 15 men: BMI = 29.0 (3.0); VO2 max = 39.5 (5.7) ml/kg/min.18 women: BMI = 29.3 (2.3); VO2 max = 32.4 (3.1) ml/kg/min. Exercise = 16 men: BMI = 29.7 (2.9); VO2 max = 39.2 (5.2) ml/kg/min.25 women: BMI = 28.7 (3.2); VO2 max = 32.8 (4.2) ml/kg/min. Sample age NR: recruited age range 17–35. | 16 mos | Control: no exercise. Exercise: supervised treadmill exercise, 5 days/wk. progressed from 20 min/session at baseline to 45 min/session at 6 mos. and intensity progressed from 60% HRR at baseline to 75% HRR at 6 mos. | Weight and measure over 2 wk periods at baseline, 3, 6, 9, 12 and 16 mos. of ad libitum eating at a university cafeteria. Food consumption outside the cafeteria (i.e. snacks) was assessed by multiple-pass 24-hr recalls. | Exercise adherence: Men = 90.3%; Women = 89.6%. EEEx: Men = 667 (116) kcal/session. Women = 439 (88) kcal/session | Men: No significant between group differences at baseline or at 16 mos. for EI, fat (g), or CHO (g) intake. PRO intake (g) increased significantly in men in the exercise group vs control. No significant between group differences were observed for fat, CHO or PRO intake as a percentage of total EI. Women: No significant between group differences at baseline or 16 mos for EI or either absolute (g) or relative (% EI) intake of fat, CHO, or PRO. |
| Donnelly et al. (2000) [128] | 22 women. Continuous exercise (CON) = 11 women: Age = 54 (9); BMI = 30.1 (2.5); VO2 max = 23.6 (2.8) ml/kg/min. Intermittent exercise (INT) = 11 women: Age = 49 (8); BMI = 32.2 (5.1); VO2 max = 22.9 (4.1) ml/kg/min | 18 mos | Supervised exercise. CON = 30 min/day, 3 days/wk., at 60–70% max VO2. INT = Brisk walk at approximately 50–60% HRR, 2 times/day, 15 min/session, 5 days/wk. at their home or worksite. | EI and macronutrient intake measured with 3-day food records (2 wk days, 1 wk end day) at baseline, 9, and 18 mos. 24-hr recalls were collected at 3, 6, 12, and 15 mos. | Exercise adherence: CON = 90.1 (2.3)%; INT = 90.3 (9.1)%; Supervision: CON = 100%; INT = 17.9 (4.8)%. Weekly EEEx (kJ): CON = 2235 (614); INT = 3235 (872) | Total EI did not change significantly during the duration of the study. Macronutrient composition was unchanged with the exception of fat intake for INT which significantly lower at 9 and 18 mos compared to baseline. Results for the 24-hr recalls were similar to the 3-day food records. |
| Foster-Schubert et al. (2012) [110] Exercise vs. Control Arms | Control = 87 women: Age = 57.4 (4.4); BMI = 30.7 (3.9); Non-Hispanic white = 85.1%; VO2 max = 23.1 (4.1) ml/kg/min. Exercise = 117 women: Age = 58.1 (6.0); BMI = 30.7 (3.7); Non-Hispanic white = 83.3%; VO2 max = 22.5 (4.1) ml/kg/min. Completion rates: Control = 80/87 (92%); Exercise = 106/117 (91%) | 12 mos | Control: no exercise. Exercise: Progressed from 15 min/session, 60–70% max HR, 5 days/wk to a target of 45 min/session, 70–85% max HR, 5 days/wk. at week 7. Supervised at exercise facility 3 days, at home 5 days. | Women's Health Initiative 120-item self-administered. FFQ administered at baseline and 12 mos. | Exercise adherence: Achieved on average 80% of the target 225 min/wk aerobic exercise over the 12 mo trial. | EI and fat intake (%EI) decreased in both control and exercise groups, with no significant between group differences. |
| Grediagan et al. (1995) [126] | High Intensity Exercise = 6 women: Age = 30 (5); BMI = 23.8 (2.3); White = 50%; VO2 max = 31.5 (3.8) ml/kg/min. Low Intensity Exercise = 6 women: Age = 31 (6); BMI = 26.2 (1.4); White = 0%; VO2 max = 31.3 (3.3) ml/kg/min. Completion rate: High = 67%;Low = 67% | 12 wks | Supervised treadmill exercise, 4 days/wk at either low (50% VO2 max) or high (80% VO2 max) intensity. Duration was adjusted to elicit EEEx of 300 kcal/session | 4-day food records at baseline, 6 and 12 wks. | Exercise adherence: All subjects completed the 48 prescribed exercise sessions at the prescribed work rate. | No significant changes in EI or macronutrient composition in either group. |
| Jakicic et al. (2011) [122] | Control (n = 89): 92.1% female; 78.6% white; Age = 44.7 (7.9); BMI = 27.1 (1.7). Moderate dose (n = 82): 90.2% female; 78.9% white; Age = 43.5 (8.8); BMI = 27.1 (1.7). High dose (n = 98): 91.8% female; 81.1% white; Age = 45.0 (8.4); BMI = 27.0 (1.6). Completion rate: ITT analysis, Control = 94%; Moderate dose = 93%; High dose = 90%. All subjects sedentary. | 18 mos | Control: no PA intervention. Moderate dose PA: Progressed to 150 min/wk., 55–85% age-predicted max HR, structured, non-supervised PA at wk. 12. High dose PA: Progressed from 100 to 300 min/wk. | Block FFQ | Estimated EEEx (kcal/wk.): Control 6 mos = 1529; 12 mos = 1439; 18 mos = 1460. Moderate dose: 6 mos = 1504;12 mos = 1324; 18 mos = 1147. High dose: 6 mos = 2008; 12 mos = 1685; 18 mos = 1527 | No significant group-by-time interaction for changes in EI or percent of energy from fat, CHO or PRO. |
| Kirkwood et al. (2007) [111] Exercise vs. Control arms | Control = 18 women: BMI = 32.5 (4.5). Exercise = 19 women: BMI = 31.6 (3.8). Mean age for total sample = 41(NR). Total sample completion rate = 63.3%. Activity/fitness level = NR | 12 wks | Control: no exercise. Exercise: Specific advice to achieve 60 min brisk walking/day. | 4-day unweighed food record (3 wk and 1 wk end day) at baseline, 6 and 12 wks. | EEEx estimated by accelerometer increased 150 kcal/day and 203 kcal/day over baseline at wks 6 and 12, respectively. | Control: EI decreased at wks. 6 and 12 vs. baseline. No change in macronutrient intake as a % of EI over 12 wks. Exercise: EI significantly lower than baseline at wk 6. % energy from fat increased from baseline at wk 12. No change in % energy from CHO or PRO. |
| Miyashita et al. (2010) [127] | Walking group = 8 men: Age = 49.1 (3.4); BMI = 29.7 (2.0); VO2 max = 27.4 (1.7) ml/kg/min. Jogging group = 7 men: Age = 46.7 (3.2); BMI = 29.6 (0.7); VO2 max = 30.7 (2.0) ml/kg/min. | 12 wks | Supervised brisk walking or jogging – 30–60 min/day, 3 days/wk., outdoors. Walking = 65–70% age predicted max HR. Jogging = 75–80% age predicted max HR. | 3 day weighed food record at baseline and 10 wks. | Exercise adherence: Walking = 75(8)%; Jogging = 74 (11)%. Exercise intensity: Walking = 69 (4)% max HR. Jogging = 78 (1)% max HR. | No significant differences for total EI or macronutrient intake between or within groups at baseline or at 10 wks. |
| Nieman et al. (1990) [112] | Control group = 18 sedentary women: Age = 32.8 (1.4); BMI = 27.8 (0.9). Exercise group = 18 sedentary women: Age = 36 (1.6); BMI = 28.3 (0.7). | 15 wks | Brisk walking, 45 min/session, 5 days/wk at 62% VO2 max. | 7-day food records at baseline, 6 and 15 wks. | 90% of sessions were supervised. Intensity = 62 (2)% VO2 max. | EI decreased significantly over 15 wks in the exercise group and showed a non- significant increase in the control group. The between group differences were non-significant. No significant group by time interactions for CHO, fat or PRO intake as a % of EI. |
| Nordby et al. (2012) [113] Exercise vs. control groups | Control = 15 men: Age = 31 (2); BMI = 28.0 (0.4); VO2 max = 35.7 (1.7) ml/kg/min. Exercise = 17 men: Age = 28 (1); BMI = 28.3 (0.3); VO2 max = 38.2 (1.7) ml/kg/min. Completion rate = Control = 75%; Exercise = 85%. | 12 wks | Control: no exercise. Exercise: Supervised endurance training, 3–4 sessions/wk., moderate intensity ∼65% HRR and 3–4 sessions/wk. of continuous exercise with intermittent high intensity training intervals at ∼85% HRR, until the 600 kcal were utilized. | Weighed 3-day food records at baseline, 2, 6 and 12 wks. | EEEx = 576.3 (10.9) Kcal/day. Exercise duration = 51.4 (4.3) min/day | No significant between group differences for change in EI, or % of energy from fat, CHO or PRO. |
| Prichard et al. (1997) [114] Control vs. Exercise Arms | Control = 19 men: Age = 42.3 (4.5); BMI = 28.6 (2.8). Exercise = 21 men: Age = 44.9 (6.5); BMI = 29.2 (2.8). Completion rate = 62% of those that started the intervention. Activity/fitness level = NR. | 12 mos | Control: no exercise. Exercise: Self-selected to be completed in leisure time; minimum 3–30 min sessions/wk at a recommended intensity of 65–75% of max HR. | 3-day food records at 6 and 12 mos. and monthly 24-hr recalls. | Exercise modes: Of the 21 exercisers, 11 walked, 4 jogged (2 alternated jogging with swimming) 3 attended a gym (45 min of aerobic, 15 min RT and anaerobic exercise), and 3 rode an exercise bike. Exercise participation: 3 and 7 sessions/wk. | No significant changes in EI or % energy from fat in either the control or exercise groups. |
| Reseland et al. (2001) [117] Control vs. exercise arms | Control = 37 men. Exercise = 48 men. Mean age (complete sample) = 44.9 (2.5). Mean BMI (complete sample) = 28.6 (3.4). No data or data from which to calculate completion rate are presented. Activity/fitness level = NR | 12 mos | Control: no exercise. Exercise: Supervised, 3 day/wk., 60 min/session at 60–80% of peak HR. Sessions were 60% aerobics, 25% circuit training and 15% jogging/fast walking. | FFQ completed at baseline and 12 mos. | NR | Fat intake as a % of EI was significantly lower at 12 mos. vs. baseline in the exercise group; intakes of other macronutrient was unchanged in both exercise and control groups over the 1-year intervention period. |
| Ready et al. (1995) [115] | Control = 10 women: BMI = 32.1 (4.1); VO2 max = 24.2 (2.8) ml/kg/min. Walk group = 15 women: BMI = 29.4 (6.1); VO2 max = 28.5 (4.9) ml/kg/min. Average age of total sample = 60.9 (4.6). Completion rate: Control = 63%, Walk = 67%. | 6 mos | Control: no exercise. Walk: 60 min/day, 5 days/wk at 60% HRR. | 3-day food record at baseline and 6 mos. | Estimated EEEx = 6367 (1890) kJ/wk. Duration = 54.3 (7.7) min/session. Intensity = 54% HRR. | No significant change in EI or diet composition. |
| Ready et al. (1996) [116] | Control = 20 women: BMI = 26.6 (3.8); VO2 max = 21.8 (2.8) ml/kg/min. 3-day group = 19 women: BMI = 26.8 (4.3); VO2 max = 23.2 (4.3) ml/kg/min. 5 day group = 17 women: BMI = 26.2 (2.5); VO2 max = 22.3 (4.3) ml/kg/min. Mean age complete sample = 61.3 (5.8). Completion rate = 71% overall. Control group = 80%; 3-day group = 70%; 5-day group = 63% | 24 wks | Control: no exercise. Exercise: Walk (outdoor track), 60 min/session at 60% VO2 peak either 3 or 5 days/wk. Successful completion required 150 min/wk. and 240 min/wk. for the 3 and 5 day/wk. groups, respectively. | 3-day food records (2 wk days and 1 wk end day). | Exercise frequency: 3 day = 2.9 (0.1) days/wk. 5 day = 4.9 (0.4) days/wk. Exercise duration: 3 day = 171(8) min/wk. 5 day = 279 (20) min/wk. Estimated EEEx: 3 day = 4380 kJ/wk. 5 day = 7150 kJ/wk. Supervision: 3 day = 1.1 (0.4) sessions/wk. 5 day = 0.9 (0.3) days/wk. | No significant change in EI, or % energy from fat, CHO or PRO in any group over the 24 wk trial. |
| Rosenkilde et al. (2012) [121] | Control = 17 men: Age = 31 (6); BMI = 28.0 (2.3); VO2 max = 35.9 (4.8) ml/kg/min. Moderate dose exercise (MOD) = 18 men: Age = 30 (7); BMI = 28.6 (1.8); VO2 max = 34.6 (4.1) ml/kg/min. High dose exercise (HIGH) = 18 men: Age = 28 (5); BMI = 27.6 (1.4); VO2 max = 36.2 (5.3) ml/kg/min. Completion rates: Control = 17/18 = 94%; MOD = 18/21 = 86%; HIGH = 18/22 = 82% | 13 wks | Control: no exercise. MOD dose: running/cycling 300 kcal/day. Intense sessions (>70% VO2 max) 3 days/wk. HIGH dose: running/cycling 600 kcal/day. Intense sessions (>70% VO2 max) 3 days/wk. | 3-day weighed food records at baseline and wk. 11.Diets for ad libitum consumption were presented over 8 days at baseline and wk 13. Diets were provided in a randomized double-blinded order and consisted of 4 consecutive days of either high-CHO or low-CHO diet, respectively. | Exercise adherence: MOD = 99%, HIGH = 96%. Training EEEx: MOD = 335 (8) kcal/day. HIGH = 653 (10) kcal/day. Exercise duration: MOD = 29.9 (8.2) min/session. HIGH = 55.2(6.6) min/session. | No difference in EI in response to the intervention between or within groups. The intervention did not change the relative contribution of dietary macronutrients between or within the groups. No changes between or within groups were observed when ad libitum EI was expressed as total EI or relative to body weight during a high-CHO or low-CHO diets, |
| Shaw et al. (2010) [118] | Control = 12 sedentary men: Age = 25.0 (2.4); BMI = 24.7 (2.7). Endurance training (ET) = 12 sedentary men: Age = 25 (5.6); BMI = 23.9 (2.3). Concurrent endurance+Resistance training (CT) = 13 sedentary men: Age = 26 (3.1); BMI = 26.8 (5.0) | 16 wks | Control: no exercise. ET: Rowing, stepping, cycling and walking on treadmill for 45 min at 60% age predicted max HR, 3 days/wk. CT: 22 min of endurance training as described for the ET group+3 sets/15 reps at 60% 1-RM for 8 exercises. All exercise was supervised. | 7-day food records at baseline and 16 wks. | Exercise adherence or EEEx were NR | No association between EI and treatment group. However there was a significant decrease in total EI and in absolute intake (g/day) of CHO, fat and PRO in the CT group. |
| Van Etten et al. (1997) [119] | Control = 8 sedentary men: Age = 35 (6); BMI = 23.6 (NR). Exercise = 18 sedentary men: Age = 33 (6); BMI = 23.8 (NR) | 18 wks | Control: no exercise. Exercise: Supervised resistance training, 2 non-consecutive days/wk., 3 sets, 15 reps, 10 exercises. | 3-day food record (including 1 wk end day) at baseline 8, and 18 wks. | Exercise compliance = 95 (7)% | EI and macronutrient intake did not differ between baseline, 8 and 18 wks in either control or exercise groups. |
| Washburn et al. (2012) [120] | Control = 13 sedentary men; Age = 20.8 (3.5); BMI = 27.7 (2.5).10 sedentary women: Age = 21.6 (2.5); BMI = 26.4 (3.3). Exercise = 17 sedentary men: Age = 21.1 (2.6); BMI = 27.6 (2.3); 15 sedentary women: Age = 19.1 (1.3); BMI = 27.3 (3.5) | 6 mos | Control: no exercise. Exercise: Supervised resistance training, 3 days/wk, 1 set, 9 exercises, 3–6 repetition max. | Monthly–randomly selected period (2 wk days, 1 wk end day) using 24-hr recalls. | Exercise adherence = 96% of scheduled training sessions. | No significant between group differences at baseline or during the intervention for EI or macronutrient intake as a % of EI in the total sample or for men or women. |
Note, Values are means (standard deviation) unless otherwise noted. Abbreviations: CHO = carbohydrate; PA = physical activity; EEEx = exercise energy expenditure; EI = energy intake; FFQ = food frequency questionnaire; HRR = Heart Rate Reserve; NR = not reported; PRO = protein; REI = relative energy intake; kcal = kilocalories; KJ = kilojoules; MET = Metabolic equivalent of task; hrs = hours; min = minutes; wk = week.
Randomized Trials: Study Characteristics
Sample size/completion rate
The median (range) sample size across the 24 randomized trials was 43.5 (12–411). The median (range) proportion of randomized participants who completed the intervention and provided data for energy intake for the 23 trials that provided data on this parameter was 74% (21–100%).
Trial length
The median (range) length of the 24 randomized trials was 21 (12–72) wks.
Exercise mode
Eight of 24 randomized trials involved laboratory based aerobic exercise where participants used a variety of modalities including cycle ergometers, rowers, recumbent cycles, steppers and treadmills [16], [110], [113], [114], [117], [118], [123], 8 evaluated indoor/outdoor walk/jog [107], [111], [112], [115], [116], [122], [124], [127], 5 trials employed primarily laboratory based treadmill walking/jogging [108], [109], [125], [126], [128], 4 trials involved resistance training only [108], [119], [120], [123], 2 trials used a combination of resistance and aerobic training [118], [123] and one trial each involved swimming [124] and laboratory cycle ergometer exercise [129].
Exercise supervision
All exercise sessions were supervised in 15/24 (63%) of randomized trials [16], [107]–[109], [112], [113], [117]–[120], [123], [125]–[127], [129], partially supervised in 6 trials (25%) [110], [115], [116], [121], [124], [128] and unsupervised in 3 trials (∼13%) [111], [114], [122].
Exercise prescription (frequency)
The median (range) exercise frequency was 4 (2–7) days/wk in trials/groups randomized to aerobic exercise and 3 (2–4) days/wk for participants randomized to resistance training.
Exercise prescription (intensity)
Seven randomized trials prescribed intensity as a percentage of maximal VO2 [16], [108], [112], [116], [121], [123], [128], 8 trials used a percentage of HRMax [110], [114], [117], [118], [122], [125]–[127], 6 used a percentage of heart-rate-reserve [109], [113], [115], [124], [128], [129] and in 2 trials intensity was “self-paced” [107], [111]. The median (range) of intensity prescriptions were: 65% (50–85%) maximal VO2; 70% (50–90%) HRMax, and 65% (50–75%) heart-rate-reserve.
Exercise prescription (duration)
Sixteen randomized trials prescribed exercise duration by time [108]–[112], [114]–[118], [122], [124], [125], [127]–[129], 3 by level of exercise energy expenditure [113], [121], [126], and one each by energy expenditure/kg body weight [16], caloric equivalent of walking 12 miles/wk [123] and walking distance [107]. The median (range) duration for the 16 trials prescribing exercise by time was 42 (30–60) min/day. Exercise prescriptions by level of energy expenditure were 300 kcal/day [126], 600 kcal/day [113] and both 300 and 600 kcal/day [121]. Church et al. [16] randomized participants to energy expenditure groups of 4, 8 and 12 kcal/kg/wk, while Bales et al. [123] assigned participants to a combination of aerobic exercise modes (treadmill, elliptical, cycle ergometer) at a caloric equivalent of 12 miles/wk and Brandon et al. [107] prescribed walking 3 miles/session.
Compliance with the exercise protocol
Eighteen studies presented data relative to participant compliance with the exercise training protocol [16], [107]–[110], [112], [115], [116], [119]–[121], [123]–[128]. Fifteen trials reported the percentage of exercise sessions attended [(median(range) 95% (74–100%)] [16], [107]–[110], [112], [115], [116], [119]–[121], [123], [126]–[128], while 3 trials compared the prescribed with actual minutes of actual exercise completed. Bryner et al. [125] prescribed 40–45 min/day, 4 days/wk and observed 45 min/day, 4.1 days/wk. Cox et al. [124] prescribed 90 and achieved 124 min/wk while Nordby et al. [113] prescribed 600 kcal/session and achieved 576 kcal/session.
Energy and macronutrient assessment
Twelve trials used non-weighed food records over 2 to 7 days [107], [108], [111], [112], [115], [116], [118], [119], [121], [125], [126], [129], 2 used weighed 3-day food records [113], [127], 5 used food frequency questionnaires [16], [110], [117], [122], [124], 3 used a combination of food records and 24 hour recalls [114], [123], [128], and one study each employed repeated 24 hour recalls [120], one study used weigh and measure ad libitum eating over 2 weeks [109], and one study used test meals offered over 8 days [121]. Nine studies assessed energy intake only at baseline and end [16], [110], [115]–[118], [121], [123], [127], 7 studies completed energy intake assessments at 3 time points [111]–[114], [119], [124], [126], and 4 studies at 4 time points [107], [108], [122], [125] and 4 at more than 4 time points [109], [120], [128], [129].
Randomized Trials: Participant Characteristics
Age
The median (range) for age across all randomized trials 43 (25–61) years.
Gender
Eleven trials (∼46%) included only women [16], [107], [110]–[112], [115], [116], [124]–[126], [128], 9 men only [108], [113], [114], [117]–[119], [121], [127], [129] and four studies (∼17%) included both men and women [109], [120], [122], [123]; however, only 2 of these studies provided separate result data by gender [109], [120].
BMI
The median (range) BMI for participants over the 24 randomized trials was 28.3 (25.0–32.4) kg/m2. Thirteen of the 24 randomized trials (∼54%) evaluated overweight participants (i.e. BMI>25 to ≤30 kg/m2) [108], [109], [112]–[114], [116], [117], [120]–[122], [124], [126], [127], while the mean sample BMI was classified as obese (i.e. ≥30 kg/m2) in 8 trials [16], [107], [110], [111], [115], [123], [128], [129] and normal weight (i.e. BMI≤25 kg/m2) in 3 trials [118], [119], [125].
Minority status
The median (range) percentage of non-white participants was 19% (0–60%) for the 9 randomized that provided information relative to the racial or ethnic composition of the study sample [16], [107]–[110], [122], [123], [126], [129].
Participant activity level
With the exception of the trial by Broeder et al. [108], who studied active but untrained participants; all randomized trials were conducted in participants who were sedentary or minimally active at baseline.
Randomized Trials: Results
Energy intake
Eighteen of 24 randomized trials (75%) found no significant change in energy intake in response to exercise training [108]–[110], [113]–[117], [119]–[122], [124]–[129]. Five randomized trials reported significant decreases (∼200–500 kcal/day) in energy intake in response to exercise training [16], [111], [112], [118], [123]. One randomized trial reported a significant increase in energy intake (Brandon 06). However, energy intake increased only in African American, but not white women, where energy intake decreased [107].
Macronutrient intake
Eighteen of the 23 randomized trials (∼78%) that provided data on macronutrient intake found no change as a result of exercise training [16], [108], [109], [112]–[120], [122], [124]–[127], [129]. Results from the 5 randomized trials that reported significant changes in macronutrient intake as a result of exercise training were mixed [107], [110], [111], [123], [128]. For example, Brandon et al. [107] reported a significant increase in absolute carbohydrate intake in white, but not African American women, while Kirkwood et al. [111] reported a significant increase in the intake of fat as a percentage of total energy intake, with no change in the percentage of energy intake from carbohydrate or protein. Studies reported significant decreases in the absolute intake of carbohydrate [107], [118], [123], fat [118], [123], [128] and protein [118], [123] as well as decreases in the intake of fat as a percentage of total energy intake [117].
Effect of Study Parameters on Energy Intake
Exercise mode
Two randomized trials compared change in energy intake in response to aerobic and resistance training. Broeder et al. [108] reported no change in energy intake in either the aerobic or resistance training groups while Bales et al. [123] reported a significant decrease in energy intake induced by aerobic, but not resistance training. A combination of aerobic plus resistance training was compared with aerobic training alone in 2 trials. Bales et al. [123] reported no between group differences for the change in energy intake with significant decreases in energy intake in both groups. Shaw et al. [118] reported significant decreases in energy intake in the aerobic plus resistance training group but not the aerobic training group. No significant changes in energy intake were reported in the 2 trials that evaluated energy intake in response to resistance training compared with non-exercise controls [119], [120] or between participants who completed swim vs. walking training programs [124].
Level of exercise energy expenditure/duration
No between group differences for change in energy intake in response to aerobic exercise training at difference levels of exercise energy expenditure were reported in the 4 trials that evaluated this parameter [16], [116], [121], [122].
Exercise intensity
Four randomized trials compared changes in energy intake in response to aerobic exercise training at low or high intensity [125]–[127], [129]. No significant between group differences for change in energy intake were reported in any of the 4 trials.
Intermittent vs. continuous exercise
The one randomized trial that compared changes in energy intake in response to continuous (one-30 minute sessions/day) vs. intermittent exercise (2–15 minute sessions/day) reported no between or within group differences [128].
Composition of test meals
Rosenkilde et al. [121] found no differences in energy intake with exercise training when low or high carbohydrate test meals were offered.
Effect of Participant Characteristics on Energy Intake
Age
No randomized trials evaluated the effect of age on changes in energy intake in response to exercise training.
Gender
Two randomized trials provided data on gender differences for changes in energy intake in response to exercise training [109], [120]. Donnelly et al. [109] reported no between group (exercise vs. control) for change in energy intake in response to 16 months of supervised exercise in either men or women. Similarly, Washburn et al. [120] found no between group differences (exercise vs. control) for change in energy intake in response to 6 months of supervised resistance training in either men or women.
Other participant characteristics
No randomized trials were identified that specifically evaluated the effect of weight status, level of physical activity or level of dietary restraint on the energy intake response to exercise training.
Risk of bias
The risk of bias for all randomized trials is presented in Table 5. The description of the procedures for random sequence generation were unclear in the majority of trials (16/24 - ∼67%). Six trials adequately described randomization procedures and were considered low risk of bias [109], [110], [113], [121], [123], [124], while 2 trials were considered high risk for randomization bias based on failure to provide any description of the randomization process [119] or randomization based on level of occupational and lifestyle physical activity [127]. With the exception of the trial reported by Cox et al. [124], which adequately described procedures for allocation concealment (low bias) all other randomized trials (96%) provided no description of procedures for allocation concealment. Blinding participants and personnel is not feasible in an exercise trial. Blinding of personnel performing outcome assessments is feasible in exercise trials; however, this was described in only 2 trials [110], [121]. Twenty one trials provided no information relative to blinding of outcome assessments, while one trial directly stated that outcome assessments were not blinded [113]. Based on an effectiveness study paradigm the risk of attrition bias is high in the majority of the 24 randomized trials included in this review. Fifty-four percent of trials reported completion rates of less than 80%; however, 22 of 24 of these studies were conducted as efficacy trials where data from participants who were non-adherence to the exercise intervention or outcome assessment protocols were not included in the analysis.
Table 5. Study Risk of Bias.
| Study | Random Sequence Generation (selection bias) | Allocation concealment (selection bias) | Blinding participants and personnel (performance bias) | Blinding of outcome assessment (detection bias) | Incomplete outcome data (attrition bias) | Selective reporting (reporting bias) | Other bias |
| Bales et al. (2012) [123] | Low risk | NR | High risk | NR | High risk | Low risk | High risk |
| Brandon & Elliott-Lloyd (2006) [107] | Unclear | NR | High risk | NR | High risk | Low risk | High risk |
| Broeder et al. (1992) [108] | Unclear | NR | High risk | NR | High risk | Low risk | High risk |
| Bryner et al. (1997) [125] | Unclear | NR | High risk | NR | High risk | Low risk | High risk |
| Church et al. (2009) [16] | Unclear | NR | High risk | NR | High risk | Low risk | High risk |
| Cox et al. (2010) [124] | Low risk | NR | High risk | NR | High risk | Low risk | High risk |
| Cox et al.(2003) [129] | Unclear | NR | High risk | NR | Low risk | Low risk | High risk |
| Donnelly et al. (2003) [9] | Low risk | NR | High risk | NR | High risk. | Low risk | High risk |
| Donnelly et al. (2000) [128] | Unclear | NR | High risk | NR | Low risk | Low risk | High risk |
| Foster-Schubert et al. (2012) [110] | Low risk | NR | High risk | Low risk | Low risk | Low risk | High risk |
| Grediagin et al. (1995) [126] | Unclear | NR | High risk | NR | High risk | Low risk | High risk |
| Jakicic et al. (2011) [122] | Unclear | NR | High risk | NR | Low risk | Low risk | High risk |
| Kirkwood et al. (2007) [111] | Unclear | NR | High risk | NR | High risk | Low risk | High risk |
| Miyashita et al. (2010) [127] | High risk | NR | High risk | NR | Low risk | Low risk | High risk |
| Nieman et al. (1990) [112] | Unclear | NR | High risk | NR | Low risk | Low risk | High risk |
| Nordby et al. (2012) [113] | Low risk | NR | High risk | High risk | Low risk | Low risk | High risk |
| Pritchard et al. (1997) [114] | Unclear | NR | High risk | NR | High risk | Low risk | High risk |
| Ready et al. (1995) [115] | Unclear | NR | High risk | NR | High risk | Low risk | High risk |
| Ready et al. (1996) [116] | Unclear | NR | High risk | NR | High risk | Low risk | High risk |
| Reseland et al. (2001) [117] | Unclear | NR | High risk | NR | NR | Low risk | High risk |
| Rosenkilde et al. (2012) [121] | Low risk | NR | Low risk | Low risk | Low risk | Low risk | High risk |
| Shaw et al. (2010) [118] | Unclear | NR | High risk | NR | Low risk | Low risk | High risk |
| Van Etten et al. (1997) [119] | High risk | NR | High risk | NR | Low risk | Low risk | High risk |
| Washburn et al. (2012) [120] | Unclear | NR | High risk | NR | Low risk | Low risk | High risk |
Note. NR = Not Reported.
Discussion
Summary of Evidence
In this paper we systematically reviewed 99 studies that employed a variety of study designs including cross-sectional, acute/short-term, non-randomized and randomized trials to address the question: Does increased exercise or physical activity alter ad-libitum daily energy intake or macronutrient composition in healthy adults? Our results can be summarized as follows.
Energy intake
It is commonly believed that individuals increase energy intake in response to increased physical activity or exercise training. However overall, we found no consistent, compelling evidence that any level of increased physical activity or exercise has any impact on energy intake. Forty-one percent of cross-sectional studies reported higher energy intake among active compared with inactive individuals. However, cross-sectional data precludes determination of cause and effect. Likewise, it is not possible to determine if the higher energy intake observed among inactive individuals meets or exceeds their level of daily energy expenditure or how between group differences in body weight may impact the results of cross-sectional studies. In agreement with the results of the recent meta-analysis by Schubert et al. [30] on acute exercise and subsequent energy intake, our results from both acute and short-term trials suggest that any observed increase in post-exercise energy intake only partially compensates for the energy expended during exercise. Thus, in the short-term, exercise results in a negative energy balance. Results from both non-randomized and randomized trials are in agreement with the results from acute and short-term trials. Only 2 of 36 (∼6%) non-randomized and randomized trials, ranging in duration from 3 to 72 weeks, report an increase in absolute energy intake in response to exercise training, thus implying that exercise does not result in a compensatory increase in energy intake. A limited number of studies across all study designs have evaluated the effect of exercise parameters and participant characteristics on energy intake. Our results suggest no effect of either exercise parameters including mode (aerobic, resistance), intensity, duration/energy expenditure or participant characteristics including age, gender, weight or physical activity level on energy intake. These results are in contrast to those of Schubert et al. [30] from their meta-analysis on the acute effect of exercise on absolute post-exercise energy intake where they noted individuals with low to moderate levels of physical activity were more likely to reduce energy intake in response to exercise compared to their more active counterparts.
Macronutrient intake
Data on macronutrient intake was reported in 67 of the 99 studies (68%) included in this review. Irrespective of study design we found no consistent evidence for an effect of exercise on macronutrient intake. Forty-four of 54 acute/short-term, non-randomized and randomized trials (81%) reported no effect of exercise on macronutrient intake, while results of the 10 trials reporting an association were mixed. Thus, it appears individuals do not spontaneously alter the composition of their diets in response to physical activity or exercise.
Limitations in the Available Literature
There are several important limitations in the literature available for this systemic review. The most critical limitation in the available literature is the lack of studies that have been specifically designed and adequately powered to detect significant between or within group differences in energy intake in response to exercise training. With the exception of 2 acute studies [56], [61] no studies included in this review were statistically powered to detect between or within group differences in energy or macronutrient intake. Only 5 of 12 non-randomized trials (∼42%) [97], [100], [102]–[104] and 3 of 24 randomized trials (∼13%) were conducted specifically to evaluate the effect of exercise training on energy and macronutrient intake [112], [121], [125]. The sample size in each of these 3 trials was <20 participants/group. Inadequate statistical power may explain the disconnect between the results of our review, which found no effect of exercise training on energy intake and other trials that have evaluated the effect of exercise on body weight. For example, studies have reported high individual variability in weight loss in response to the same level of exercise energy expenditure [18] and no significant increase in weight loss in response to increased level of exercise energy expenditure [11], [121]. Both of these observations suggest compensatory increases in energy intake in response to exercise training; however, changes in resting metabolic rate and non-exercise physical activity may also play a role.
Because most exercise training studies did not prescribe exercise by level of energy expenditure, assess exercise energy expenditure, or employ adequate methods for the assessment of energy intake, it is not possible to determine the level of exercise induced energy imbalance actually achieved. Only 7 of the 36 non-randomized and randomized trials included in this review (∼19%) prescribed exercise by level of energy expenditure [18], [98], [103], [104], [113], [121], [126] while only 3 of those trials included assessments of the actual level of exercise energy expenditure by indirect calorimetry [18], [104], [126]. Furthermore, the heterogeneity of exercise/physical activity prescriptions prohibits the identification of a specific level that may elicit compensatory changes in energy intake. Only 5 of 36 non-randomized and randomized trials employed more precise estimates of dietary intake such as weigh and measure test meals [18], [103], [104], [121] or observed weigh and measure ad-libitum eating [109]. Two of the 3 trials that measured exercise energy expenditure used only 1 day assessments of energy intake using test meals at baseline and end study [18], [104], while one trial employed 4 day food records at baseline, mid and end study [126]. Thus, reported estimates of energy balance should be cautiously interpreted. The available literature is also limited by a preponderance of data from acute/short-term studies as compared to non-randomized and randomized longitudinal trials. For example, approximately 50% of studies reviewed evaluated the acute or short-term (2–14 days) effect of exercise on energy and macronutrient intake. While acute/short-term studies have employed precise methods for the assessment of energy intake (weigh and measure test meals), the short time frame over which energy intake was assessed may be insufficient to demonstrate significant adaptations in energy intake that may be induced by changes in parameters such as aerobic fitness, body weight or hormonal status etc. associated with longer term exercise training. For example, in overweight men and women Kirk et al. [130] have shown that changes in aerobic fitness and weight takes 4 months and does not level off until 9 months in an exercise program with a typical progressive exercise protocol
Approximately 60% of acute studies reviewed recruited participants who were relatively young (median age = 23 years), normal weight, and physically active or aerobically fit. Thus, results from acute trials do not generalize to the older, sedentary overweight population in need of weight management. The available literature is also limited by an insufficient number of studies that have evaluated the impact of exercise parameters (e.g. mode, frequency, intensity, duration, time of day, time course) or participant characteristics (e.g. age, gender, ethnicity, weight, activity level) on energy and/or macronutrient intake.
Limitations of this Review
Our conclusions should be cautiously interpreted as they are based on both data from sub-optimal study designs (e.g. cross-sectional, acute/short-term, non-randomized trials) and from randomized trials with a high risk of one or more forms of bias. In addition, we did not contact authors to obtain missing data or for clarification of any information presented in the published reports; therefore missing information may reflect reporting bias as opposed to any limitations in the conduct of the study.
Conclusions
The present systematic review found limited evidence to suggest that acute exercise or exercise training has a significant effect on energy or macronutrient intake. However, as previously discussed the available literature on this topic suffers numerous methodological shortcomings. Therefore, we recommend additional randomized trials to specifically evaluate the impact of exercise training on energy and macronutrient intake that: 1) are powered specifically to detect clinically significant differences in energy and/or macronutrient intake; 2) utilize state-of-the-art techniques for the assessment of energy intake such as direct observation weigh and measure or picture-plate-waste and provide multiple measures across the duration of the study; 3) include assessments of exercise energy expenditure across the duration of the study; 4) evaluate and compare levels of exercise for weight management currently recommended by governmental agencies or professional organizations such as the International Association for the Study of Obesity, the Institute of Medicine, and the American College of Sports Medicine (i.e. 60–90 min/day, moderate intensity) to determine differential effects on energy and macronutrient intake; 5) include overweight and obese, sedentary middle-age or older adults; and 6) evaluate both the effect of exercise parameters (e.g. mode, frequency, intensity duration, time course) and participant characteristics (e.g. age, gender, body weight, activity level, ethnicity) on the association between exercise and energy and macronutrient intake.
Supporting Information
PubMed complete search strategy.
(DOC)
Funding Statement
This review was funded by the International Life Sciences Institute. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Flegal KM, Carroll MD, Kit BK, Ogden CL (2012) Prevalence of Obesity and Trends in the Distribution of Body Mass Index Among US Adults, 1999–2010. Journal of the American Medical Association 307: 491–497. [DOI] [PubMed] [Google Scholar]
- 2. Finkelstein EA, Trogdon JG, Cohen JW, Dietz W (2009) Annual Medical Spending Attributable To Obesity: Payer-And Service-Specific Estimates. Health Affairs 28: w822–w831. [DOI] [PubMed] [Google Scholar]
- 3. Yaemsiri S, M SM, K AS (2011) Perceived weight status, overweight diagnosis, and weight control among US adults: the NHANES 2003–2008 Study. International Journal of Obesity 35: 1063–1070. [DOI] [PubMed] [Google Scholar]
- 4. Saris WH, Blair SN, van Baak MA, Eaton SB, Davies PS, et al. (2003) How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st Stock Conference and consensus statement. Obes Rev 4: 101–114. [DOI] [PubMed] [Google Scholar]
- 5. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Natl Academy Pr [DOI] [PubMed] [Google Scholar]
- 6.(2008) 2008 Physical Activity Guidelines for Americans. Available: http://www.health.gov/paguidelines: Office of Disease Prevention & Health Promotion.
- 7.Healthy People 2020. Office of Disease Prevention and Health Promotion. Washington, DC. Available: http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=29. Accessed 2012 Mar 16.
- 8. Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, et al. (2009) American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc 41: 459–471. [DOI] [PubMed] [Google Scholar]
- 9. Donnelly JE, Hill JO, Jacobsen DJ, Potteiger J, Sullivan DK, et al. (2003) Effects of a 16-month randomized controlled exercise trial on body weight and composition in young, overweight men and women: the Midwest Exercise Trial. Arch Intern Med 163: 1343–1350. [DOI] [PubMed] [Google Scholar]
- 10. Slentz CA, Duscha BD, Johnson JL, Ketchum K, Aiken LB, et al. (2004) Effects of the amount of exercise on body weight, body composition, and measures of central obesity - STRRIDE - A randomized controlled study. Archives of Internal Medicine 164: 31–39. [DOI] [PubMed] [Google Scholar]
- 11. Donnelly JE, Honas JJ, Smith BK, Mayo MS, Gibson CA, et al. (2013) Aerobic exercise alone results in clinically significant weight loss for men and women: midwest exercise trial 2. Obesity (Silver Spring) 21: E219–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wilmore JH, Stanforth PR, Hudspeth LA, Gagnon J, Daw EW, et al. (1998) Alterations in resting metabolic rate as a consequence of 20 wk of endurance training: the HERITAGE Family Study. Am J Clin Nutr 68: 66–71. [DOI] [PubMed] [Google Scholar]
- 13. Stiegler P, Cunliffe A (2006) The role of diet and exercise for the maintenance of fat-free mass and resting metabolic rate during weight loss. Sports Med 36: 239–262. [DOI] [PubMed] [Google Scholar]
- 14. Gilliat-Wimberly M, Manore MM, Woolf K, Swan PD, Carroll SS (2001) Effects of habitual physical activity on the resting metabolic rates and body compositions of women aged 35 to 50 years. J Am Diet Assoc 101: 1181–1188. [DOI] [PubMed] [Google Scholar]
- 15. Potteiger JA, Kirk EP, Jacobsen DJ, Donnelly JE (2008) Changes in resting metabolic rate and substrate oxidation after 16 months of exercise training in overweight adults. Int J Sport Nutr Exerc Metab 18: 79–95. [DOI] [PubMed] [Google Scholar]
- 16. Church TS, Martin CK, Thompson AM, Earnest CP, Mikus CR, et al. (2009) Changes in weight, waist circumference and compensatory responses with different doses of exercise among sedentary, overweight postmenopausal women. PLoS One 4: e4515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. King NA, Caudwell P, Hopkins M, Byrne NM, Colley R, et al. (2007) Metabolic and behavioral compensatory responses to exercise interventions: barriers to weight loss. Obesity (Silver Spring) 15: 1373–1383. [DOI] [PubMed] [Google Scholar]
- 18. King NA, Hopkins M, Caudwell P, Stubbs RJ, Blundell JE (2008) Individual variability following 12 weeks of supervised exercise: identification and characterization of compensation for exercise-induced weight loss. Int J Obes (Lond) 32: 177–184. [DOI] [PubMed] [Google Scholar]
- 19. Stubbs RJ, Hughes DA, Johnstone AM, Whybrow S, Horgan GW, et al. (2004) Rate and extent of compensatory changes in energy intake and expenditure in response to altered exercise and diet composition in humans. Am J Physiol Regul Integr Comp Physiol 286: R350–358. [DOI] [PubMed] [Google Scholar]
- 20. Westerterp K (2001) Pattern and intensity of physical activity. Nature 410: 539. [DOI] [PubMed] [Google Scholar]
- 21. Manthou E, Gill JMR, Wright A, Malkova D (2010) Behavioral compensatory adjustments to exercise training in overweight women. Med Sci Sports Exerc 42: 1221–1228. [DOI] [PubMed] [Google Scholar]
- 22. Blundell JE, Stubbs RJ, Hughes DA, Whybrow S, King NA (2003) Cross talk between physical activity and appetite control: does physical activity stimulate appetite? Proceedings of the Nutrition Society 62: 651–661. [DOI] [PubMed] [Google Scholar]
- 23. Martins C, Robertson MD, Morgan LM (2008) Effects of exercise and restrained eating behaviour on appetite control. Proceedings of the Nutrition Society 67: 28–41. [DOI] [PubMed] [Google Scholar]
- 24. Martins C, Morgan L, Truby H (2008) A review of the effects of exercise on appetite regulation: an obesity perspective. International Journal of Obesity 32: 1337–1347. [DOI] [PubMed] [Google Scholar]
- 25. King NA, Horner K, Hills AP, Byrne NM, Wood RE, et al. (2012) Exercise, appetite and weight management: understanding the compensatory responses in eating behaviour and how they contribute to variability in exercise-induced weight loss. British Journal of Sports Medicine 46: 315–322. [DOI] [PubMed] [Google Scholar]
- 26. Hopkins M, King NA, Blundell JE (2010) Acute and long-term effects of exercise on appetite control: is there any benefit for weight control? Current Opinion in Clinical Nutrition and Metabolic Care 13: 635–640. [DOI] [PubMed] [Google Scholar]
- 27. Stensel D (2010) Exercise, appetite and appetite-regulating hormones: implications for food intake and weight control. Annals of Nutrition and Metabolism 57: 36–42. [DOI] [PubMed] [Google Scholar]
- 28. Melzer K, Kayser B, Saris WHM, Pichard C (2005) Effects of physical activity on food intake. Clinical Nutrition 24: 885–895. [DOI] [PubMed] [Google Scholar]
- 29. Prentice A, Jebb SA (2004) Energy Intake/Physical Activity Interactions in the Homeostasis of Body Weight Regulation. Nutrition Reviews 62: S98–S104. [DOI] [PubMed] [Google Scholar]
- 30. Schubert MM, Desbrow B, Sabapathy S, Leveritt M (2013) Acute exercise and subsequent energy intake. A meta-analysis. Appetite 63: 92–104. [DOI] [PubMed] [Google Scholar]
- 31. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzce PC, et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of Clinical Epidemiology 62: e1–e34. [DOI] [PubMed] [Google Scholar]
- 32. Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche PC, et al. (2010) CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol 63: e1–37. [DOI] [PubMed] [Google Scholar]
- 33. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, et al. (2009) Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42: 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Higgins JP, Green S, Collaboration C (2008) Cochrane handbook for systematic reviews of interventions: Wiley Online Library.
- 35. Camoes M, Lopes C (2008) Dietary intake and different types of physical activity: Full-day energy expenditure, occupational and leisure-time. Public Health Nutrition 11: 841–848. [DOI] [PubMed] [Google Scholar]
- 36. Eaton CB, McPhillips JB, Gans KM, Garber CE, Assaf AR, et al. (1995) Cross-sectional relationship between diet and physical activity in two southeastern New England communities. American Journal of Preventive Medicine 11: 238–244. [PubMed] [Google Scholar]
- 37. Lake AA, Townshend T, Alvanides S, Stamp E, Adamson AJ (2009) Diet, physical activity, sedentary behaviour and perceptions of the environment in young adults. Journal of Human Nutrition and Dietetics 22: 444–454. [DOI] [PubMed] [Google Scholar]
- 38. Rintala M, Lyytikainen A, Leskinen T, Alen M, Pietilainen KH, et al. (2011) Leisure-time physical activity and nutrition: a twin study. Public Health Nutr 14: 846–852. [DOI] [PubMed] [Google Scholar]
- 39. Van Walleghen EL, Orr JS, Gentile CL, Davy KP, Davy BM (2007) Habitual physical activity differentially affects acute and short-term energy intake regulation in young and older adults. International Journal of Obesity 31: 1277–1285. [DOI] [PubMed] [Google Scholar]
- 40. Van Pelt RE, Dinneno FA, Seals DR, Jones PP (2001) Age-related decline in RMR in physically active men: Relation to exercise volume and energy intake. American Journal of Physiology - Endocrinology and Metabolism 281: E633–E639. [DOI] [PubMed] [Google Scholar]
- 41. D'Angelo E, Di Blasio A, Di Donato F, Di Gregorio S, Di Renzo D, et al. (2010) Relationships between physical exercise practice, dietary behaviour and body composition in female university students. J Sports Med Phys Fitness 50: 311–317. [PubMed] [Google Scholar]
- 42. Duvigneaud N, Wijndaele K, Matton L, Philippaerts R, Lefevre J, et al. (2007) Dietary factors associated with obesity indicators and level of sports participation in Flemish adults: A cross-sectional study. Nutrition Journal 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hornbuckle LM, Bassett DR Jr, Thompson DL (2005) Pedometer-determined walking and body composition variables in African-American women. Medicine and Science in Sports and Exercise 37: 1069–1074. [PubMed] [Google Scholar]
- 44. Lee IM, Djousse L, Sesso HD, Wang L, Buring JE (2010) Physical activity and weight gain prevention. JAMA - Journal of the American Medical Association 303: 1173–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lissner L, Heitmann BL, Bengtsson C (1997) Low-fat diets may prevent weight gain in sedentary women: prospective observations from the population study of women in Gothenburg, Sweden. Obes Res 5: 43–48. [DOI] [PubMed] [Google Scholar]
- 46. Mulligan K, Butterfield GE (1990) Discrepancies between energy intake and expenditure in physically active women. British Journal of Nutrition 64: 23–36. [DOI] [PubMed] [Google Scholar]
- 47. Matthews CE, Hebert JR, Ockene IS, Saperia G, Merriam PA (1997) Relationship between leisure-time physical activity and selected dietary variables in the worcester area trial for counseling in hyperlipidemia. Medicine and Science in Sports and Exercise 29: 1199–1207. [DOI] [PubMed] [Google Scholar]
- 48. Perry AC, Shaw MH, Hsia L, Nash MS, Kaplan T, et al. (1992) Plasma lipid levels in active and sedentary premenopausal females. International Journal of Sports Medicine 13: 210–215. [DOI] [PubMed] [Google Scholar]
- 49. Jago R, Nicklas T, Yang SJ, Baranowski T, Zakeri I, et al. (2005) Physical activity and health enhancing dietary behaviors in young adults: Bogalusa Heart Study. Preventive Medicine 41: 194–202. [DOI] [PubMed] [Google Scholar]
- 50. Butterworth DE, Nieman DC, Underwood BC, Lindsted KD (1994) The relationship between cardiorespiratory fitness, physical activity, and dietary quality. Int J Sport Nutr 4: 289–298. [DOI] [PubMed] [Google Scholar]
- 51. Imbeault P, Saint-Pierre S, Almeras N, Tremblay A (1997) Acute effects of exercise on energy intake and feeding behaviour. British Journal of Nutrition 77: 511–521. [DOI] [PubMed] [Google Scholar]
- 52. Pomerleau M, Imbeault P, Parker T, Doucet E (2004) Effects of exercise intensity on food intake and appetite in women. American Journal of Clinical Nutrition 80: 1230–1236. [DOI] [PubMed] [Google Scholar]
- 53. Unick JL, Otto AD, Goodpaster BH, Helsel DL, Pellegrini CA, et al. (2010) Acute effect of walking on energy intake in overweight/obese women. Appetite 55: 413–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Melby CL, Osterberg KL, Resch A, Davy B, Johnson S, et al. (2002) Effect of carbohydrate ingestion during exercise on post-exercise substrate oxidation and energy intake. Int J Sport Nutr Exerc Metab 12: 294–309. [DOI] [PubMed] [Google Scholar]
- 55. O'Donoghue KJM, Fournier PA, Guelfi KJ (2010) Lack of effect of exercise time of day on acute energy intake in healthy men. International Journal of Sport Nutrition and Exercise Metabolism 20: 350–356. [DOI] [PubMed] [Google Scholar]
- 56. King JA, Wasse LK, Stensel DJ (2011) The acute effects of swimming on appetite, food intake, and plasma acylated ghrelin. J Obes 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. King JA, Miyashita M, Wasse LK, Stensel DJ (2010) Influence of prolonged treadmill running on appetite, energy intake and circulating concentrations of acylated ghrelin. Appetite 54: 492–498. [DOI] [PubMed] [Google Scholar]
- 58. King JA, Wasse LK, Broom DR, Stensel DJ (2010) Influence of brisk walking on appetite, energy intake, and plasma acylated ghrelin. Med Sci Sports Exerc 42: 485–492. [DOI] [PubMed] [Google Scholar]
- 59. King NA, Blundell JE (1995) High-fat foods overcome the energy expenditure induced by high-intensity cycling or running. European Journal of Clinical Nutrition 49: 114–123. [PubMed] [Google Scholar]
- 60. King NA, Burley VJ, Blundell JE (1994) Exercise-induced suppression of appetite: Effects on food intake and implications for energy balance. European Journal of Clinical Nutrition 48: 715–724. [PubMed] [Google Scholar]
- 61. Harris CL, George VA (2008) The impact of dietary restraint and moderate-intensity exercise on post-exercise energy intake in sedentary males. Eating Behaviors 9: 415–422. [DOI] [PubMed] [Google Scholar]
- 62. Visona C, George VA (2002) Impact of dieting status and dietary restraint on postexercise energy intake in overweight women. Obes Res 10: 1251–1258. [DOI] [PubMed] [Google Scholar]
- 63. Maraki M, Tsofliou F, Pitsiladis YP, Malkova D, Mutrie N, et al. (2005) Acute effects of a single exercise class on appetite, energy intake and mood. Is there a time of day effect? Appetite 45: 272–278. [DOI] [PubMed] [Google Scholar]
- 64. Erdmann J, Tahbaz R, Lippl F, Wagenpfeil S, Schusdziarra V (2007) Plasma ghrelin levels during exercise - Effects of intensity and duration. Regulatory Peptides 143: 127–135. [DOI] [PubMed] [Google Scholar]
- 65. Laan DJ, Leidy HJ, Lim E, Campbell WW (2010) Effects and reproducibility of aerobic and resistance exercise on appetite and energy intake in young, physically active adults. Appl Physiol Nutr Metab 35: 842–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Schneider KL, Spring B, Pagoto SL (2009) Exercise and energy intake in overweight, sedentary individuals. Eating Behaviors 10: 29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Verger P, Lanteaume MT, Louis-Sylvestre J (1992) Human intake and choice of foods at intervals after exercise. Appetite 18: 93–99. [DOI] [PubMed] [Google Scholar]
- 68. Martins C, Morgan LM, Bloom SR, Robertson MD (2007) Effects of exercise on gut peptides, energy intake and appetite. J Endocrinol 193: 251–258. [DOI] [PubMed] [Google Scholar]
- 69. Finlayson G, Bryant E, Blundell JE, King NA (2009) Acute compensatory eating following exercise is associated with implicit hedonic wanting for food. Physiology and Behavior 97: 62–67. [DOI] [PubMed] [Google Scholar]
- 70. Lluch A, King NA, Blundell JE (2000) No energy compensation at the meal following exercise in dietary restrained and unrestrained women. Br J Nutr 84: 219–225. [PubMed] [Google Scholar]
- 71. Lluch A, King NA, Blundell JE (1998) Exercise in dietary restrained women: no effect on energy intake but change in hedonic ratings. Eur J Clin Nutr 52: 300–307. [DOI] [PubMed] [Google Scholar]
- 72. Tsofliou F, Pitsiladis YP, Malkova D, Wallace AM, Lean ME (2003) Moderate physical activity permits acute coupling between serum leptin and appetite-satiety measures in obese women. Int J Obes Relat Metab Disord 27: 1332–1339. [DOI] [PubMed] [Google Scholar]
- 73. George VA, Morganstein A (2003) Effect of moderate intensity exercise on acute energy intake in normal and overweight females. Appetite 40: 43–46. [DOI] [PubMed] [Google Scholar]
- 74. King NA, Snell L, Smith RD, Blundell JE (1996) Effects of short-term exercise on appetite responses in unrestrained females. European Journal of Clinical Nutrition 50: 663–667. [PubMed] [Google Scholar]
- 75. Kissileff HR, Pi-Sunyer FX, Segal K, Meltzer S, Foelsch PA (1990) Acute effects of exercise on food intake in obese and nonobese women. Am J Clin Nutr 52: 240–245. [DOI] [PubMed] [Google Scholar]
- 76. Larson-Meyer DE, Palm S, Bansal A, Austin KJ, Hart AM, et al. (2012) Influence of running and walking on hormonal regulators of appetite in women. Journal of Obesity 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Balaguera-Cortes L, Wallman KE, Fairchild TJ, Guelfi KJ (2011) Energy intake and appetite-related hormones following acute aerobic and resistance exercise. Appl Physiol Nutr Metab 36: 958–966. [DOI] [PubMed] [Google Scholar]
- 78. Jokisch E, Coletta A, Raynor HA (2012) Acute energy compensation and macronutrient intake following exercise in active and inactive males who are normal weight. Appetite 58: 722–729. [DOI] [PubMed] [Google Scholar]
- 79. Kelly PJ, Guelfi KJ, Wallman KE, Fairchild TJ (2012) Mild dehydration does not reduce postexercise appetite or energy intake. Med Sci Sports Exerc 44: 516–524. [DOI] [PubMed] [Google Scholar]
- 80. Vatansever-Ozen S, Tiryaki-Sonmez G, Bugdayci G, Ozen G (2011) The effects of exercise on food intake and hunger: Relationship with acylated ghrelin and leptin. Journal of Sports Science and Medicine 10: 283–291. [PMC free article] [PubMed] [Google Scholar]
- 81. Deighton K, Zahra JC, Stensel DJ (2012) Appetite, energy intake and resting metabolic responses to 60 min treadmill running performed in a fasted versus a postprandial state. Appetite 58: 946–954. [DOI] [PubMed] [Google Scholar]
- 82. King JA, Wasse LK, Ewens J, Crystallis K, Emmanuel J, et al. (2011) Differential acylated ghrelin, peptide YY3-36, appetite, and food intake responses to equivalent energy deficits created by exercise and food restriction. Journal of Clinical Endocrinology and Metabolism 96: 1114–1121. [DOI] [PubMed] [Google Scholar]
- 83. Verger P, Lanteaume MT, Louis-Sylvestre J (1994) Free food choice after acute exercise in men. Appetite 22: 159–164. [DOI] [PubMed] [Google Scholar]
- 84. Shorten AL, Wallman KE, Guelfi KJ (2009) Acute effect of environmental temperature during exercise on subsequent energy intake in active men. Am J Clin Nutr 90: 1215–1221. [DOI] [PubMed] [Google Scholar]
- 85. Ueda SY, Yoshikawa T, Katsura Y, Usui T, Fujimoto S (2009) Comparable effects of moderate intensity exercise on changes in anorectic gut hormone levels and energy intake to high intensity exercise. Journal of Endocrinology 203: 357–364. [DOI] [PubMed] [Google Scholar]
- 86. Ueda SY, Yoshikawa T, Katsura Y, Usui T, Nakao H, et al. (2009) Changes in gut hormone levels and negative energy balance during aerobic exercise in obese young males. J Endocrinol 201: 151–159. [DOI] [PubMed] [Google Scholar]
- 87. Stubbs RJ, Sepp A, Hughes DA, Johnstone AM, King N, et al. (2002) The effect of graded levels of exercise on energy intake and balance in free-living women. International Journal of Obesity 26: 866–869. [DOI] [PubMed] [Google Scholar]
- 88. Whybrow S, Hughes DA, Ritz P, Johnstone AM, Horgan GW, et al. (2008) The effect of an incremental increase in exercise on appetite, eating behaviour and energy balance in lean men and women feeding. British Journal of Nutrition 100: 1109–1115. [DOI] [PubMed] [Google Scholar]
- 89. Stubbs RJ, Sepp A, Hughes DA, Johnstone AM, Horgan GW, et al. (2002) The effect of graded levels of exercise on energy intake and balance in free-living men, consuming their normal diet. European Journal of Clinical Nutrition 56: 129–140. [DOI] [PubMed] [Google Scholar]
- 90. Keim NL, Barbieri TF, Belko AZ (1990) The effect of exercise on energy intake and body composition in overweight women. Int J Obes 14: 335–346. [PubMed] [Google Scholar]
- 91. Keim NL, Canty DJ, Barbieri TF, Wu MM (1996) Effect of exercise and dietary restraint on energy intake of reduced-obese women. Appetite 26: 55–70. [DOI] [PubMed] [Google Scholar]
- 92. Stubbs RJ, Hughes DA, Johnstone AM, Horgan GW, King N, et al. (2004) A decrease in physical activity affects appetite, energy, and nutrient balance in lean men feeding ad libitum. American Journal of Clinical Nutrition 79: 62–69. [DOI] [PubMed] [Google Scholar]
- 93. Staten MA (1991) The effect of exercise on food intake in men and women. American Journal of Clinical Nutrition 53: 27–31. [DOI] [PubMed] [Google Scholar]
- 94. King NA, Lluch A, Stubbs RJ, Blundell JE (1997) High dose exercise does not increase hunger or energy intake in free living males. European Journal of Clinical Nutrition 51: 478–483. [DOI] [PubMed] [Google Scholar]
- 95. Tremblay A, Almeras N, Boer J, Kranenbarg EK, Despres JP (1994) Diet composition and postexercise energy balance. American Journal of Clinical Nutrition 59: 975–979. [DOI] [PubMed] [Google Scholar]
- 96. Farah NM, Malkova D, Gill JM (2010) Effects of exercise on postprandial responses to ad libitum feeding in overweight men. Med Sci Sports Exerc 42: 2015–2022. [DOI] [PubMed] [Google Scholar]
- 97. Koulouri AA, Tigbe WW, Lean MEJ (2006) The effect of advice to walk 2000 extra steps daily on food intake. Journal of Human Nutrition and Dietetics 19: 263–266. [DOI] [PubMed] [Google Scholar]
- 98. Martins C, Kulseng B, King NA, Holst JJ, Blundell JE (2010) The effects of exercise-induced weight loss on appetite-related peptides and motivation to eat. Journal of Clinical Endocrinology and Metabolism 95: 1609–1616. [DOI] [PubMed] [Google Scholar]
- 99. Snyder KA, Donnelly JE, Jabobsen DJ, Hertner G, Jakicic JM (1997) The effects of long-term, moderate intensity, intermittent exercise on aerobic capacity, body composition, blood lipids, insulin and glucose in overweight females. International Journal of Obesity 21: 1180–1189. [DOI] [PubMed] [Google Scholar]
- 100. Westerterp KR, Meijer GA, Janssen EM, Saris WH, Ten Hoor F (1992) Long-term effect of physical activity on energy balance and body composition. Br J Nutr 68: 21–30. [DOI] [PubMed] [Google Scholar]
- 101. Andersson B, Xu X, Rebuffe-Scrive M, Terning K, Krotkiewski M, et al. (1991) The effects of exercise training on body composition and metabolism in men and women. International Journal of Obesity 15: 75–81. [PubMed] [Google Scholar]
- 102. Suzuki S, Urata G, Ishida Y, Kanehisa H, Yamamura M (1998) Influences of low intensity exercise on body composition, food intake and aerobic power of sedentary young females. Appl Human Sci 17: 259–266. [DOI] [PubMed] [Google Scholar]
- 103. Bryant EJ, Caudwell P, Hopkins ME, King NA, Blundell JE (2012) Psycho-markers of weight loss. The roles of TFEQ Disinhibition and Restraint in exercise-induced weight management. Appetite 58: 234–241. [DOI] [PubMed] [Google Scholar]
- 104. Caudwell P, Gibbons C, Hopkins M, King N, Finlayson G, et al. (2013) No Sex Difference in Body Fat in Response to Supervised and Measured Exercise. Medicine and Science in Sports and Exercise 45: 351–358. [DOI] [PubMed] [Google Scholar]
- 105. Di Blasio A, Ripari P, Bucci I, Di Donato F, Izzicupo P, et al. (2012) Walking training in postmenopause: effects on both spontaneous physical activity and training-induced body adaptations. Menopause-the Journal of the North American Menopause Society 19: 23–32. [DOI] [PubMed] [Google Scholar]
- 106. Keytel LR, Lambert MI, Johnson J, Noakes TD, Lambert EV (2001) Free living energy expenditure in post menopausal women before and after exercise training. International Journal of Sport Nutrition 11: 226–237. [DOI] [PubMed] [Google Scholar]
- 107. Brandon LJ, Elliott-Lloyd MB (2006) Walking, body composition, and blood pressure dose-response in African American and White women. Ethnicity and Disease 16: 675–681. [PubMed] [Google Scholar]
- 108. Broeder CE, Burrhus KA, Svanevik LS, Wilmore JH (1992) The effects of either high-intensity resistance or endurance training on resting metabolic rate. American Journal of Clinical Nutrition 55: 802–810. [DOI] [PubMed] [Google Scholar]
- 109. Donnelly JE, Kirk EP, Jacobsen DJ, Hill JO, Sullivan DK, et al. (2003) Effects of 16 mo of verified, supervised aerobic exercise on macronutrient intake in overweight men and women: the Midwest Exercise Trial. Am J Clin Nutr 78: 950–956. [DOI] [PubMed] [Google Scholar]
- 110. Foster-Schubert KE, Alfano CM, Duggan CR, Xiao L, Campbell KL, et al. (2012) Effect of Diet and Exercise, Alone or Combined, on Weight and Body Composition in Overweight-to-Obese Postmenopausal Women. Obesity 20: 1628–1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Kirkwood L, Aldujaili E, Drummond S (2007) Effects of advice on dietary intake and/or physical activity on body composition, blood lipids and insulin resistance following a low-fat, sucrose-containing, high-carbohydrate, energy-restricted diet. International Journal of Food Sciences and Nutrition 58: 383–397. [DOI] [PubMed] [Google Scholar]
- 112. Nieman DC, Haig JL, Fairchild KS, De Guia ED, Dizon GP, et al. (1990) Reducing-diet and exercise-training effects on serum lipids and lipoproteins in mildly obese women. American Journal of Clinical Nutrition 52: 640–645. [DOI] [PubMed] [Google Scholar]
- 113. Nordby P, Auerbach PL, Rosenkilde M, Kristiansen L, Thomasen JR, et al. (2012) Endurance training per se increases metabolic health in young, moderately overweight men. Obesity 20: 2202–2212. [DOI] [PubMed] [Google Scholar]
- 114. Pritchard JE, Nowson CA, Wark JD (1997) A worksite program for overweight middle-aged men achieves lesser weight loss with exercise than with dietary change. J Am Diet Assoc 97: 37–42. [DOI] [PubMed] [Google Scholar]
- 115. Ready AE, Drinkwater DT, Ducas J, Fitzpatrick D, Brereton DG, et al. (1995) Walking program reduces elevated cholesterol in women postmenopause. Canadian Journal of Cardiology 11: 905–912. [PubMed] [Google Scholar]
- 116. Ready AE, Naimark B, Ducas J, Sawatzky JAV, Boreskie SL, et al. (1996) Influence of walking volume on health benefits in women post-menopause. Medicine and Science in Sports and Exercise 28: 1097–1105. [DOI] [PubMed] [Google Scholar]
- 117. Reseland JE, Anderssen SA, Solvoll K, Hjermann I, Urdal F, et al. (2001) Effect of long-term changes in diet and exercise on plasma leptin concentrations. American Journal of Clinical Nutrition 73: 240–245. [DOI] [PubMed] [Google Scholar]
- 118. Shaw BS, Shaw I, Mamen A (2010) Contrasting effects in anthropometric measures of total fatness and abdominal fat mass following endurance and concurrent endurance and resistance training. J Sports Med Phys Fitness 50: 207–213. [PubMed] [Google Scholar]
- 119. Van Etten LM, Westerterp KR, Verstappen FT, Boon BJ, Saris WH (1997) Effect of an 18-wk weight-training program on energy expenditure and physical activity. J Appl Physiol 82: 298–304. [DOI] [PubMed] [Google Scholar]
- 120. Washburn RA, Kirk EP, Smith BK, Honas JJ, Lecheminant JD, et al. (2012) One set resistance training: effect on body composition in overweight young adults. J Sports Med Phys Fitness 52: 273–279. [PubMed] [Google Scholar]
- 121. Rosenkilde M, Auerbach P, Reichkendler MH, Ploug T, Stallknecht BM, et al. (2012) Body fat loss and compensatory mechanisms in response to different doses of aerobic exercise-a randomized controlled trial in overweight sedentary males. American Journal of Physiology - Regulatory Integrative and Comparative Physiology 303: R571–R579. [DOI] [PubMed] [Google Scholar]
- 122. Jakicic JM, Otto AD, Lang W, Semler L, Winters C, et al. (2011) The Effect of Physical Activity on 18-Month Weight Change in Overweight Adults. Obesity 19: 100–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Bales CW, Hawk VH, Granville EO, Rose SB, Shields T, et al. (2012) Aerobic and resistance training effects on energy intake: the STRRIDE-AT/RT study. Med Sci Sports Exerc 44: 2033–2039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Cox KL, Burke V, Beilin LJ, Puddey IB (2010) A comparison of the effects of swimming and walking on body weight, fat distribution, lipids, glucose, and insulin in older women–the Sedentary Women Exercise Adherence Trial 2. Metabolism 59: 1562–1573. [DOI] [PubMed] [Google Scholar]
- 125. Bryner RW, Toffle RC, Ullrich IH, Yeater RA (1997) The effects of exercise intensity on body composition, weight loss, and dietary composition in women. Journal of the American College of Nutrition 16: 68–73. [DOI] [PubMed] [Google Scholar]
- 126. Grediagin A, Cody M, Rupp J, Benardot D, Shern R (1995) Exercise intensity does not effect body composition change in untrained, moderately overfat women. J Am Diet Assoc 95: 661–665. [DOI] [PubMed] [Google Scholar]
- 127. Miyashita M, Eto M, Sasai H, Tsujimoto T, Nomata Y, et al. (2010) Twelve-week jogging training increases pre-heparin serum lipoprotein lipase concentrations in overweight/obese middle-aged men. Journal of Atherosclerosis and Thrombosis 17: 21–29. [DOI] [PubMed] [Google Scholar]
- 128. Donnelly JE, Jacobsen DJ, Heelan KS, Seip R, Smith S (2000) The effects of 18 months of intermittent vs continuous exercise on aerobic capacity, body weight and composition, and metabolic fitness in previously sedentary, moderately obese females. International Journal of Obesity 24: 566–572. [DOI] [PubMed] [Google Scholar]
- 129. Cox KL, Burke V, Morton AR, Beilin LJ, Puddey IB (2003) The independent and combined effects of 16 weeks of vigorous exercise and energy restriction on body mass and composition in free-living overweight men–a randomized controlled trial. Metabolism 52: 107–115. [DOI] [PubMed] [Google Scholar]
- 130. Kirk EP, Jacobsen DJ, Gibson C, Hill JO, Donnelly JE (2003) Time course for changes in aerobic capacity and body composition in overweight men and women in response to long-term exercise: the Midwest Exercise Trial (MET). Int J Obes Relat Metab Disord 27: 912–919. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PubMed complete search strategy.
(DOC)