Abstract
Background
The positive relationship between alcohol use, gender and violence-related injury is well established. However, less is known about injuries when alcohol is used in combination with other drugs.
Method
Self-report information was collected on alcohol and illicit drug use in the six hours prior to a violence-related injury in probability samples of patients presenting to emergency departments (n=9686).
Results
Patients with violence-related injuries reported the highest rates of alcohol use (49% of men; 23% of women) and alcohol use combined with illicit drugs (8% of men; 4% of women) prior to the injury event while non-violent injury patients reported lower rates of alcohol use (17% of men; 8% of women) and alcohol use combined with drugs (2% for men; 1% for women). Marijuana/hashish was the most commonly reported drug. The odds of a violent injury were increased when alcohol was used (men: odds ratio [OR]=5.4, 95% confidence interval [CI] 4.6–6.3; women: OR=4.0, 95% CI 3.0–5.5) or when alcohol was combined with illicit drug use prior to the injury (men: OR=6.6, 95% CI 4.7–9.3; women: OR=5.7, 95% CI=2.7–12.2) compared to non-users. No significant change in the odds of a violent injury was observed for men or women when alcohol users were compared with alcohol and drug users.
Conclusion
The positive association between alcohol and violent injury does not appear to be altered by the added use of drugs. Additional work is needed to understand the interpersonal, contextual and cultural factors related to substance use to identify best prevention practices and develop appropriate policies.
Keywords: emergency department, alcohol and illicit drug use, violence-related injury, gender differences
Introduction
Alcohol and illicit drug use are a major cause of harms to individuals and society. Each are substantial contributors to the international burden of mortality and morbidity[1] and, while these substances are typically indicated as separate categorisations to the global burden of disease, there is long standing evidence that the combined use of alcohol and drugs is not an uncommon practice. With few exceptions, large-scale survey data have identified significant and positive associations between the incidence of alcohol use in combination with drug use [2–5]. Moreover, emergency department (ED) studies have found that patients consuming alcohol prior to an injury event were more likely to have used illicit drugs in the recent past [6,7] and that self-reported use was generally reliable [8]. Similarly, general population studies show that individuals using the ED in the past year report higher rates of coexisting alcohol and drug use, spend more days using drugs and are more likely to have an alcohol or drug use disorder compared to non-ED users [9]. This is not surprising given that the physiological effects of alcohol can include impaired coordination, delayed response time and dis-inhibition believed to increase the risk for injury and admission to the ED [10].
The effects of alcohol when combined with illicit drugs can vary depending on the type of drug used [11]. Alcohol used in conjunction with opiates or marijuana can potentially exacerbate the sedative effects of these substances while alcohol may counteract the increased arousal experienced by stimulant use (e.g. cocaine, amphetamines). These acute effects can vary considerably depending on the amount and combinations consumed as well as by gender [12,13]. Furthermore, the acute effects of alcohol combined with other substances and a co-occurring injury are not fully understood.
Whereas evidence of the harm associated with alcohol use, particularly for a violence-related physical injury, is extensive [14–17] comparatively less attention has been given to the combined use of alcohol and drugs prior to a violence-related injury [6,18]. Although prior studies have found a significant relationship between drug use and violence-related injury [6,19,20] others have not observed such a clear distinction [21,22]. Recent ED studies suggest that the combined effect of alcohol and drug use may increase the risk of a violent injury [23] but that the type of drug used can play a significant role. While cocaine combined with alcohol has been found to increase the incidence of a violent injury [24,25] substances such as cannabis and opiates may not [26]. Additionally, while there are clear differences between men’s and women’s drinking patterns [27,28] there is less evidence that alcohol use and the risk of injury differs by gender [16]. However, gender specific data on the combined use of alcohol and illicit drugs and violence-related injury are lacking [29,30].
The present study will examine alcohol use and alcohol use in combination with illicit drugs in probability samples of injured ED patients. We seek to understand if use of alcohol combined with illicit drugs changes the odds of an injury event due to violence when compared with patients using alcohol alone or patients not using any substances prior to the injury event. We will also explore whether there are dose response associations when heavier alcohol consumption is present. Moreover, this work proposes to add to the literature on substance use and violence-related injury by considering potential gender differences in these associations.
Methods
This study includes probability samples of patients from studies represented by 15 localities and 30 EDs from eight countries. Data from Argentina, Mexico, Poland, Spain and the United States are from the Emergency Room Collaborative Alcohol Analysis Project (ERCAAP), which used similar methodologies and protocols across these countries [31–33]. Data from Australia, Canada and Switzerland recruited patients with methodologies and protocols akin to the ERCAAP studies but only injury patients were recruited [30,34,35]. Data were collected from 1984 to 2006 with each ED site using all arriving patients (or all arriving injury patients) and giving equal representation to each ED shift each day of the week during the study period. Patients who presented to the ED were approached with an informed consent to participate in the study and those who were too severely injured upon arrival to the ED were approached in the hospital once they were stabilised. Completion rates ranged from 65% in Warsaw, Poland to 93% in Pachuca, Mexico. Reasons for non-study participation were refusal, incapacitation from injury, leaving the ED, language barriers, or police custody
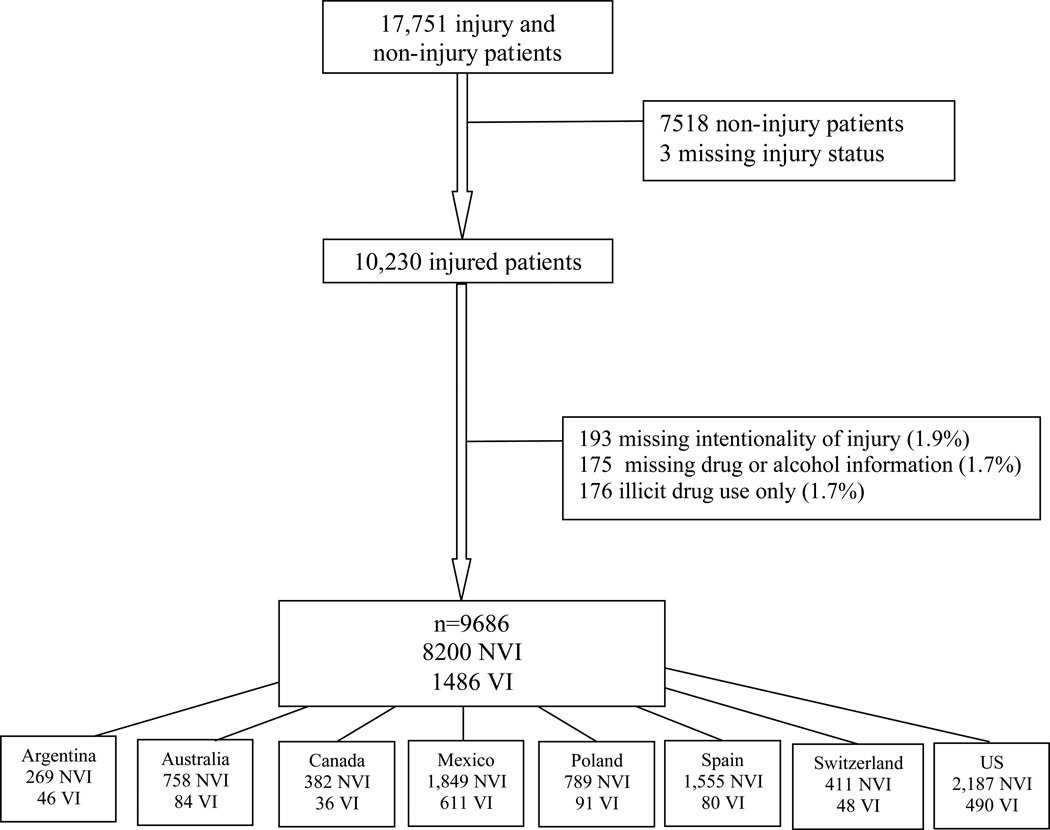
Patients agreeing to participate were administered an interview regarding, among other items, the reason for the ED visit, alcohol and drug use within six hours prior to the injury event, the number of drinks consumed and demographic information including age, gender and education. Only patients reporting an injury are used for the present study. The type and cause of injury was obtained using patient self-report. Violence-related injury was defined as injury initiated by either the patient’s actions or that of other person(s), including circumstances such as getting into a fight, being beaten, raped or attacked. Patients were grouped by either presenting with a violence-related injury vs. non-violence-related injury. Figure 1 displays the study sample selection.
Figure 1.
Flow chart of patient sample.
NVI, non-violent injury; VI, violent injury.
Data on drug use in the six hours prior to the injury event were obtained from a series of questions on marijuana/hashish, stimulants, sedatives, opiates and other non-prescription drugs. The studies varied in the types of drugs queried and employed terms that were inclusive of generic, brand and street names. For example, stimulants were inclusive of cocaine, crack, amphetamines, methamphetamine and ‘speed’, while sedatives included quaaludes, barbiturates, tranquilizers, benzodiazepines, Librium and Valium. Opiates included, heroin, codeine, Percodan, Demerol and opium and an ‘other’ non-prescription drug category included inhalants, LSD, PCP, mescaline, psilocybin and ‘angel dust’. Only illegal substances or substances that had the potential for abuse were included in the analysis, with over the counter medications excluded from consideration. Because this paper sought to understand the additive effect of illicit drug use with alcohol use, patients that reported using only illicit drugs prior to the injury event were excluded from the analysis (n=176; Figure 1). However, four study sites did not collect information on drug use if a patient did not consume alcohol in the six hours to the injury event and therefore illicit drug use could not be determined for those patients. These study sites were included in the analysis as not having used either alcohol or drugs in the six hours prior to the injury event. Patients were grouped into three categories of substance use, ‘no alcohol or drug use’, ‘alcohol only’ or ‘alcohol and illicit drug use’.
Data Analysis
Only injury patients 18 years and older who responded to the type of injury and the alcohol and drug use questions are included for the present paper with all analyses conducted for the overall sample and stratified by gender. Regression models predicting violence-related injury were conducted using the Statistical Package for the Social Sciences (SPSS) version 17.0. Weights were assigned to several studies to adjust for data that were not collected with equal representation of all shifts in a day across all days of the week.
Results
Demographics
Injury patients were predominantly male, representing 63.7% of the sample (Table 1). The majority of injury patients were current drinkers, reaching 90.6% among men with violence-related injuries. Less than a third of the injury patients had obtained a college education, which may be partially attributable to the high percentage of men and women under the age of 30 (47.5% of non-violent injuries and 61.2% of violence-related injuries). Among those with a non-violent injury, 15.4% reported any alcohol or drug use prior to the event compared to 48.8% of those with a violence-related injury. Alcohol was the most prevalently reported substance used, with higher rates among those with violence-related injuries (42.1%) compared to those with non-violence-related injuries (13.8%); alcohol and drug use followed a similar pattern, but rates were relatively small: 6.7% of those with violence-related injuries and 1.6% of those with non-violence-related injuries. Marijuana/hashish was the most commonly reported illicit drug (4.5% for violence-related injuries vs. 1.1% for non-violence-related injuries).
Table 1.
Demographic, drinking and drug use characteristics by intentionality and gender (n=9686).
| Non-violence related injury | Violence-related injury | |||||
|---|---|---|---|---|---|---|
| men (n=5075) |
women (n=3125) |
total (n=8200) |
men (n=1101) |
women (n=385) |
total (n=1486) |
|
| % | % | % | % | % | % | |
| Current drinkers | 84.6 | 67.9 | 78.2 | 90.6 | 71.1 | 85.6 |
| College education | 28.7 | 24.6 | 27.1 | 20.6 | 22.9 | 21.2 |
| Age LE 30 | 53.2 | 38.3 | 47.5 | 64.2 | 52.4 | 61.2 |
| Mean age (95% CI) | 33.5 (33.1, 33.9) | 40.9 (40.2, 41.58) | 36.3 (36.0, 36.7) | 29.8 (29.1, 30.5) | 33.7 (32.2, 35.1) | 30.8 (30.1, 31.4) |
| Alcohol and drug use 6 hours prior to injury | ||||||
| None | 80.5 | 91.3 | 84.6 | 43.5 | 73.4 | 51.2 |
| alcohol only | 17.3 | 8.1 | 13.8 | 48.9 | 22.5 | 42.1 |
| alcohol + illicit drug use | 2.2 | 0.6 | 1.6 | 7.6 | 4.1 | 6.7 |
| Drug use | ||||||
| Cannabis | 1.6 | 0.4 | 1.1 | 5.3 | 2.1 | 4.5 |
| Number of drinks in the 6 hours prior | ||||||
| None | 80.9 | 91.7 | 85.0 | 43.6 | 73.0 | 51.2 |
| 1–3 drinks | 8.5 | 5.2 | 7.2 | 16.9 | 11.8 | 15.6 |
| 4–7 drinks | 4.3 | 1.7 | 3.3 | 13.0 | 7.3 | 11.6 |
| 8+ drinks | 6.3 | 1.5 | 4.5 | 26.5 | 7.9 | 21.6 |
CI, confidence interval.
Nearly half (48.9%) of the men with violence-related injuries reported using alcohol in the six hours prior to the injury event. Comparatively, 17.3% of men with non-violence-related injuries reported using only alcohol. Men with violence-related injuries also reported significantly higher rates of combined alcohol and drug use compared to those with non-violence-related injuries (7.6% vs. 2.2%).
Though women reported lower rates of alcohol use in the six hours prior to injury than men, they exhibited similar patterns in relation to injury type. Female patients with a violence-related injury reported higher rates of alcohol and drug use compared to those with non-violent related injuries, and this was especially marked for those using only alcohol (22.5% with violence-related injury vs. 8.1% with non-violence-related injury). The rates of alcohol and combined drug use was particularly low for women with non-violence-related injury (0.6%) compared with women with violence-related injuries (4.1%).
Use of alcohol alone or alcohol combined with drugs prior to the injury event were both positively predictive 0f a violence-related injury for men (Table 2). Men who reported using a combination of alcohol and drugs were over seven times more likely to report a violence-related injury and over five times more likely to do so when consuming alcohol alone, compared with those reporting no use of either alcohol or drugs prior to injury. When compared to those reporting alcohol use alone, use of alcohol combined with drugs was not predictive of a violence-related injury. Alcohol and drug use among women was also associated with incurring a violence-related injury. Women were four times more likely to report a violence-related injury when using only alcohol, and over six times more likely when using alcohol and drugs combined. Compared to those using only alcohol, drug use in combination with alcohol did not predict a violence-related injury.
Table 2.
Logistic regression models of alcohol and drug use in the 6 hours prior to injury predicting a violence-related injury~.
| Adjusted odds ratios (95% CI) | |||
|---|---|---|---|
| men+ | women+ | total ++ | |
| All patients | |||
| Model 1~ | |||
| ref=no alcohol or drug use | |||
| alcohol use only | 5.4 (4.6, 6.3)*** | 4.0 (3.0, 5.5)*** | 5.0 (4.4, 5.8)*** |
| alcohol + illicit drugs | 6.6 (4.7, 9.3)*** | 5.7 (2.7, 12.2)*** | 6.4 (4.7, 8.7)*** |
| Alcohol and any illicit drug use | |||
| Model 2 ~ | |||
| ref = alcohol use only | |||
| alcohol + illicit drugs | 1.3 (0.9, 1.8) | 1.6 (0.7, 3.6) | 1.3 (1.0, 1.9) |
| Alcohol and marijuana/hashish use | |||
| Model 3 &~ | |||
| ref = no alcohol or drug use | |||
| Alcohol use only | 5.4 (4.6, 6.4)*** | 4.1 (3.0, 5.7)*** | 5.1 (4.4, 5.9)*** |
| Alcohol + marijuana/hashish | 6.7 (4.5, 10.2)*** | 3.4 (1.1, 10.1)* | 6.1 (4.1, 8.9)*** |
| Alcohol and marijuana/hashish use | |||
| Model 4 &~ | |||
| Ref= Alcohol use only | |||
| Alcohol + marijuana/hashish | 1.3 (0.8, 2.0) | 0.9 (0.3, 2.8) | 1.3 (0.9, 1.9) |
Additional models with interactions terms for substance use and gender and substance use and age were non-significant.
Models control for age, education, and study country.
Models control for age, education, study country, and gender.
P<0.05 ;
P <0.001.
Comparisons using other illicit drugs (e.g., stimulants, opiates) were not possible due to small sample sizes.
CI, confidence interval.
Models using the most commonly reported drug of marijuana or hashish and excluding other illicit substance users, showed similar odds ratios to models 1 and 2.
Because men and women may differ in the use of substance and sustaining a violence-related injury, additional models (not tabled) tested the interaction between substance use and gender but none were significant. Also, because violence-related injury is more often reported among younger males additional interaction models were employed to examine substance use by age and all were non-significant (not tabled).
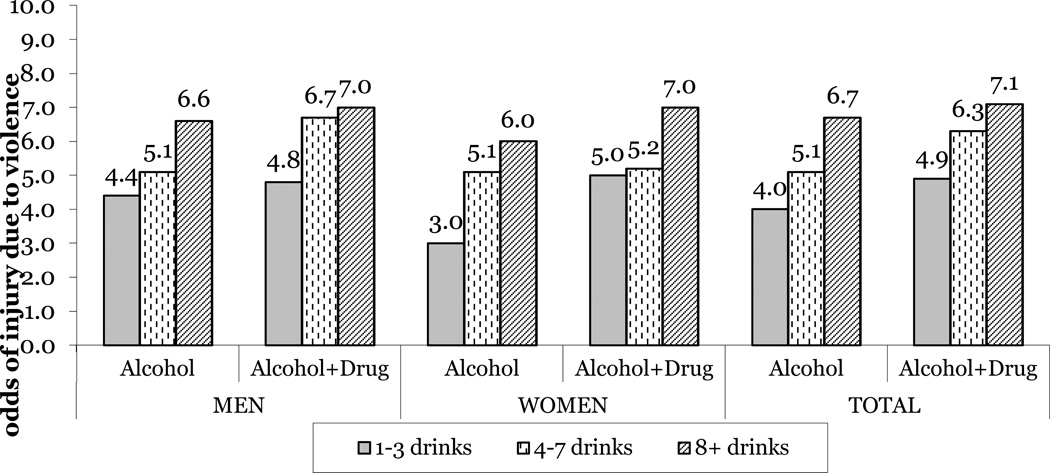
Models that include the amount of drinking prior to the injury (Figure 2) show that men consuming 1–3 drinks were over four times more likely to report a violence-related injury and odds ratios increased over six times more likely when consuming eight or more drinks, compared to those reporting no substance use. Men using alcohol combined with drugs prior to the injury were nearly five times more likely to report a violence-related injury when having 1–3 drinks and over six times more likely when consuming 4 or more drinks in combination with drug use. An interaction regression model showed that at each of the three levels of alcohol consumption, the risk of an injury due to violence did not differ for those that consumed only alcohol compared with those who drank and used illicit drugs.
Figure 2.
Odds ratios of a violence-related injury by the number of drinks in the 6 hours prior to the injury+~
+ reference group = no drinking or drug use in the 6 hours prior to injury.
Models control for age and education. All odds ratios are significant at P <0.05.
~ Additional models with interactions terms for substance use and gender and substance use and age were non-significant.
The increase in the number of drinks consumed prior to injury also put women at a higher risk for a violence-related injury. When compared with women who did not use alcohol or drugs, women consuming 1–3 drinks in the six hours prior to injury were three times more likely to have a violence-related injury and six times more likely when eight or more drinks were consumed prior to the injury. When alcohol was combined with drug use there was also a higher risk of violence-related injury. Women having 1–3 drinks or 4–7 drinks were five times more likely to have a violence-related injury and nearly 10 times more likely when consuming eight or more drinks. An interaction model examining the dose response between the alcohol only using women with alcohol and drug using women was not significant. Models examining the interaction of substance use by gender and substance use by age were non-significant.
Models for Table 2 and Figure 2 were re-analysed excluding the four study sites that did not collect drug use information for patients not reporting alcohol use and the significance levels did not change.
Discussion
Findings support a greater likelihood of a violence-related injury when alcohol or alcohol combined with drugs were consumed prior to the injury event, compared to non-substance using injury patients, regardless of gender. No significant difference in the likelihood of violence-related injury was observed among either men or women who reported alcohol combined with drug use compared to those reporting alcohol use alone prior to injury, however. Similar odds of violence-related injury by substance use classification was observed for both the genders.
There is some indication that the type of drug used in the six hours prior to injury may have played a role in lack of significant findings between the patients using alcohol only and the alcohol and drug using patients. The majority of the men who used drugs reported marijuana/hashish use, a drug that has not demonstrated an association with incurring a violence-related injury [25,26]. Our models selecting only for marijuana/hashish users or marijuana/hashish and alcohol users, showed no significant differences between the groups. While stimulant use has been shown to increase the risk of a violence-related injury [29], our patients reported rates of stimulant use that were too low for reliable statistical comparisons to be conducted although the self-report rates are similar to other studies that collected information on drug use in the six hours prior to the injury [6].
An increase in the odds ratios of a violence-related injury was observed with heavier alcohol consumption for both alcohol use alone and in combination with drugs (Figure 2). Any amount of drinking increased the odds of a violence-related injury at least threefold for women and over fourfold for men. Interestingly, patients with violence-related injuries reported a greater average number of drinks prior to the injury event compared to the patients with a non-violence-related injury. This is somewhat reflected in the alcohol and drug using patient odds ratios for eight or more drinks but there was no significant interaction between alcohol use and alcohol and drug users and the number of drinks before the injury to a violence-related injury. Similarly, though odds ratios varied somewhat by gender, interaction models between substance use and gender were not significant.
Limitations
These data represent a rich source of probability-sampled injury patients from eight countries, yet some limitations should be noted. The present study only examined injured ED patients and no community controls were available to estimate the relative risk of violence-related injury. Similarly, measures of self-reported drug use is assumed to be underestimated due to the patients risk of stigma or social desirability and rates of use may vary due to the time of the study data collection and the locality. There was also potential for bias as collection of drug specific information varied among the study sites and may have contributed to variations in response. Though four of the 16 study sites used identical questions to obtain responses to specific drug use, some study sites asked very specific questions about drug use (e.g. “did you use powder cocaine?”, “did you use crack cocaine?”, “did you inject cocaine?”) whereas other sites were less specific (e.g. “did you take any speed, amphetamines or cocaine?”). Bias in reporting may have also occurred because any drug use reported in the six hours before injury was included and besides marijuana/hashish, we could not obtain odds ratios for any other drug classes. Though we controlled for study site in our models, identifying trends in drug use by time and region were beyond the scope of the present paper. Finally, the findings from this study cannot rule out the potential influence of unmeasured variables that may play an explanatory role in the association between substance use and violence-related injury such as within-patient characteristics of lifestyle choices and personality (i.e. impulsivity).
Conclusion and future directions
It is well documented that self-reported rates of substance use are considerably lower than that of toxicology screens, although this method of data collection is beneficial in establishing a causal relationship between substance use and injury [8]. Yet, self-report measures generally produce rates of drug positives that are too small to allow for thorough examination of the relationship between injury and substance use. Future research on injury in ED settings should attempt to incorporate creative methodologies that combine self-report, biomedical screening and contextual factors (e.g. others’ drug use, attribution of injury, clinical assessment), with detailed drug specific information in an attempt to establish authentic rates of substance use and the role of substance use to injury.
As defined, violence-related injury was the result of the patient’s or another’s actions, and thus the occurrence of a violence-related injury may differ considerably for men and women. For example, women are less likely to report being victim to intimate partner violence if they are not actively screened for intimate partner violence [37] thereby resulting in underestimation of violence-related injuries among women. Studies that focus on the context of substance use are needed to better understand the use of alcohol and drugs prior to a violence-related injury.
Ideally, routinised screening of injury patients in the ED for substance use would maximise identification of those who may benefit from screening and brief intervention but special consideration should be given to populations vulnerable to violence. Inclusion of assessment that identifies the typology of drug user (e.g. casual vs. frequent user) would also aid in identifying patients with recurring substance use problems or those who are episodic users [38], and enable clinicians to guide patients to appropriate intervention or treatment services. Additionally, comparative amounts of illicit substances consumed between men and women may also help to inform clinicians, as thresholds for abuse and dependence of alcohol differ by gender, yet thresholds for illicit drug use, especially in combination with alcohol use, are not well established.
While the majority of substance-using ED injury patients do not present with a violence-related injury it is interesting that large percentages of patients with a violence-related injury report or test positive for alcohol and/or drugs [39]. This suggests that contextual and cultural attributes of alcohol and illicit drug use need further examination to implement effective community strategies to prevent the antecedents that lead to violence and injury. Community prevention measures should be used in conjunction with individual level policies designed to limit access or exposure to alcohol and drugs [39].
Acknowledgements
Analysis supported by a grant from the US National Institute on Alcohol Abuse and Alcoholism (RO1 AA013750). The paper is based, in part, on data collected by the following collaborators participating in the Emergency Room Collaborative Alcohol Analysis Project (ERCAAP): S. Bazargan (USA), P. Bendtsen (Sweden), G. Borges (Mexico), C. J. Cherpitel (USA), W. Cook (USA), M. Cremonte (Argentina), J.Moskalewicz (Poland), J. Rhodes (Spain), T. Stockwell (Canada) and G. Swiathiewicz (Poland). This paper is also based, in part, on the data and experience obtained during the participation of the authors in the World Health Organization (WHO) Collaborative Study on Alcohol and Injuries, sponsored by the WHO and implemented by the WHO Collaborative Study Group on Alcohol and Injuries that includes: G. Borges (Mexico); C. Cherpitel (USA); M. Cremonte (Argentina); S. Macdonald (Canada); M. Peden (WHO, Switzerland); V. Poznyak (WHO, Switzerland); J. Rehm (Switzerland); A list of other staff contributing to the project can be found in the Main Report of the Collaborative Study on Alcohol and Injuries, WHO, Geneva. The authors alone are responsible for views expressed in this paper, which do not necessarily represent those of the other investigators participating in the ERCAAP or WHO Collaborative Studies on Alcohol and Injuries, nor the views or policy of the World Health Organization, or the US National Institute on Alcohol and Alcoholism.
References
- 1.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–1360. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 2.Degenhardt L, Chiu W-T, Sampson N, et al. Toward a Global View of Alcohol, Tobacco, Cannabis, and Cocaine Use: Findings from the WHO World Mental Health Surveys. PLoS Med. 2008;5:e141. doi: 10.1371/journal.pmed.0050141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hall W, Teesson M, Lynskey M, Degenhardt L. The 12-month prevalence of substance use and ICD-10 substance use disorders in Australian adults: findings from the National Survey of Mental Health and Well-Being. Addiction. 1999;94:1541–1550. [PubMed] [Google Scholar]
- 4.Stinson FS, Grant BF, Dawson DA, Ruan WJ, Boji H, Saha T. Comorbidity Between DSM – IV Alcohol and Specific Drug Use Disorders in the United States. Alcohol Research & Health. [Article] 2006;29:94–106. [Google Scholar]
- 5.Hedden SL, Martins SS, Malcolm RJ, Floyd L, Cavanaugh CE, Latimer WW. Patterns of illegal drug use among an adult alcohol dependent population: Results from the National Survey on Drug Use and Health. Drug Alcohol Depend [Article] 2010;106:119–125. doi: 10.1016/j.drugalcdep.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vitale S, Mheen Dvd. Illicit drug use and injuries: A review of emergency room studies. Drug Alcohol Depend. 2006;82:1–9. doi: 10.1016/j.drugalcdep.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 7.Cowperthwaite MC, Burnett MG. Treatment course and outcomes following drug and alcohol-related traumatic injuries. J Trauma Manag Outcomes. 2011;5:1–9. doi: 10.1186/1752-2897-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vitale SG, van de Mheen H, van de Wiel A, Garretsen HF. Substance use among emergency room patients: Is self-report preferable to biochemical markers? Addict Behav. 2006;31:1661–1669. doi: 10.1016/j.addbeh.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 9.Wu LT, Swartz MS, Wu Z, Mannelli P, Yang C, Blazer DG. Alcohol and drug use disorders among adults in emergency department settings in the United States. Ann Emerg Med. 2012;60:172–180. e5. doi: 10.1016/j.annemergmed.2012.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Normand J, Lempert RO, O'Brien CP. Under the influence?: Drugs and the American work force. National Academies Press; 1994. [PubMed] [Google Scholar]
- 11.Marr JN. Washington, DC: Office of Justice Programs Drug Court Clearinghouse and Technical Assistance Project at American University; 1999. Aug, [Accessed: 2013-08-06]. The Interrelationship Between the Use of Alcohol and Other Drugs: Overview for drug court practitioners. Archived by WebCite® at http://www.webcitation.org/6IfpiafsS. [Google Scholar]
- 12.Anderson BM, Rizzo M, Block RI, Pearlson GD, O'Leary DS. Sex, drugs, and cognition: effects of marijuana. J Psychoactive Drugs. 2010;42:413–424. doi: 10.1080/02791072.2010.10400704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wiren KM, Hashimoto JG, Alele PE, et al. Impact of sex: determination of alcohol neuroadaptation and reinforcement. Alcohol Clin Exp Res. 2006;30:233–242. doi: 10.1111/j.1530-0277.2006.00032.x. [DOI] [PubMed] [Google Scholar]
- 14.Cherpitel CJ, Borges G, Giesbrecht N, et al., editors. Alcohol and Injuries: Emergency department studies in an international perspective. Geneva, Switzerland: World Health Organization; 2009. [Google Scholar]
- 15.Vinson DC, Maclure M, Reidinger C, Smith GS. A population-based case-crossover and case-control study of alcohol and the risk of injury. J Stud Alcohol. 2003;64:358–366. doi: 10.15288/jsa.2003.64.358. [DOI] [PubMed] [Google Scholar]
- 16.Borges G, Cherpitel CJ, Orozco R, et al. Multicentre study of acute alcohol use and non-fatal injuries: data from the WHO collaborative study on alcohol and injuries. Bulletin of the World Health Organization. 2006;84:453–460. doi: 10.2471/blt.05.027466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Norton RN, Morgan MY. The role of alcohol in mortality and morbidity from interpersonal violence. Alcohol Alcohol. 1989;24:565–576. doi: 10.1093/oxfordjournals.alcalc.a044960. [DOI] [PubMed] [Google Scholar]
- 18.el-Guebaly N, Armstrong SJ, Hodgins DC. Substance abuse and the emergency room: programmatic implications. J Addict Dis. 1998;17:21–40. doi: 10.1300/J069v17n02_03. [DOI] [PubMed] [Google Scholar]
- 19.Macdonald S, Wells S, Giesbrecht N, Cherpitel C. Demographic and substance use factors related to violent and accidental injuries: results from an emergency room study. Drug Alcohol Depend. 1999;55:53–61. doi: 10.1016/s0376-8716(98)00184-7. [DOI] [PubMed] [Google Scholar]
- 20.Cunningham R, Walton MA, Maio RF, Blow FC, Weber JE, Mirel L. Violence and substance use among an injured emergency department population. Acad Emerg Med. 2003;10:764–775. doi: 10.1111/j.1553-2712.2003.tb00071.x. [DOI] [PubMed] [Google Scholar]
- 21.Borges G, Cherpitel CJ, Rosovsky H. Male drinking and violence-related injury in the emergency room. Addiction. 1998;93:103–112. doi: 10.1046/j.1360-0443.1998.93110310.x. [DOI] [PubMed] [Google Scholar]
- 22.Watt K, Purdie DM, Roche AM, McClure RJ. Risk of injury from acute alcohol consumption and the influence of confounders. Addiction. 2004;99:1262–1273. doi: 10.1111/j.1360-0443.2004.00823.x. [DOI] [PubMed] [Google Scholar]
- 23.Blondell RD, Dodds HN, Looney SW, et al. Toxicology screening results: injury associations among hospitalized trauma patients. J Trauma. 2005;58:561–570. doi: 10.1097/01.ta.0000152638.54978.53. [DOI] [PubMed] [Google Scholar]
- 24.Macdonald S, Erickson P, Wells S, Hathaway A, Pakula B. Predicting violence among cocaine, cannabis, and alcohol treatment clients. Addict Behav. 2008;33:201–205. doi: 10.1016/j.addbeh.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 25.Lindenbaum GA, Carroll SF, Daskal I, Kapusnick R. Patterns of alcohol and drug abuse in an urban trauma center: The increasing role of cocaine abuse. J Trauma. 1989;29:1654–1658. doi: 10.1097/00005373-198912000-00012. [DOI] [PubMed] [Google Scholar]
- 26.Macdonald S, Anglin-Bodrug K, Mann RE, et al. Injury risk associated with cannabis and cocaine use. Drug Alcohol Depend. 2003;72:99–115. doi: 10.1016/s0376-8716(03)00202-3. [DOI] [PubMed] [Google Scholar]
- 27.Wilsnack RW, Wilsnack SC, Kristjanson AF, Vogeltanz-Holm ND, Gmel G. Gender and alcohol consumption: patterns from the multinational GENACIS project. Addiction. 2009;104:1487–1500. doi: 10.1111/j.1360-0443.2009.02696.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wells S, Thompson JM, Cherpitel C, MacDonald S, Marais S, Borges G. Gender differences in the relationship between alcohol and violent injury: An analysis of cross-national emergency department data. J Stud Alcohol Drugs. 2007;68:824–833. doi: 10.15288/jsad.2007.68.824. [DOI] [PubMed] [Google Scholar]
- 29.Schnitzer S, Bellis MA, Anderson Z, et al. Nightlife Violence: A gender-specific view on risk factors for violence in nightlife settings: A cross-sectional study in nine European countries. J Interpers Violence. 2010;25:1094–1112. doi: 10.1177/0886260509340549. [DOI] [PubMed] [Google Scholar]
- 30.Stockwell T, McLeod R, Stevens M, Phillips M, Webb M, Jelinek G. Alcohol consumption, setting, gender and activity as predictors of injury: a population-based case-control study. J Stud Alcohol. 2002;63:372–379. doi: 10.15288/jsa.2002.63.372. [DOI] [PubMed] [Google Scholar]
- 31.Cherpitel CJ. A study of alcohol use and injuries among emergency room patients. In: Giesbrecht N, Gonzales R, Grant M, et al., editors. Drinking and Casualties: Accidents, poisonings and violence in an international perspective. London; New York: Tavistock/Routledge; 1989. pp. 288–299. [Google Scholar]
- 32.Cherpitel CJ, Bond J, Ye Y, Borges G, Macdonald S, Giesbrecht NA. A cross-national meta-analysis of alcohol and injury: data from the Emergency Room Collaborative Alcohol Analysis Project (ERCAAP) Addiction. 2003;98:1277–1286. doi: 10.1046/j.1360-0443.2003.00459.x. [DOI] [PubMed] [Google Scholar]
- 33.Bazargan-Hejazi S, Gaines T, Duan N, Cherpitel CJ. Correlates of injury among ED visits: effects of alcohol, risk perception, impulsivity, and sensation seeking behaviors. Am J Drug Alcohol Abuse. 2007;33:101–108. doi: 10.1080/00952990601087455. [DOI] [PubMed] [Google Scholar]
- 34.Cherpitel CJ, Martin G, Macdonald S, Brubacher JR, Stenstrom R. Alcohol and drug use as predictors of intentional injuries in two emergency departments in British Columbia. Am J Addict. 2013;22:87–92. doi: 10.1111/j.1521-0391.2013.00316.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gmel G, Kuendig H, Rehm J, Schreyer N, Daeppen JB. Alcohol and cannabis use as risk factors for injury – a case-crossover analysis in a Swiss hospital emergency department. BMC Public Health. 2009;9:40. doi: 10.1186/1471-2458-9-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McDonald A, Duncan ND, Mitchell DI. Alcohol, cannabis and cocaine usage in patients with trauma injuries. West Indian Med J. 1999;48:200–202. [PubMed] [Google Scholar]
- 37.Ernst AA, Weiss SJ. Intimate partner violence from the emergency medicine perspective. Women Health. 2002;35:71–81. doi: 10.1300/J013v35n02_05. [DOI] [PubMed] [Google Scholar]
- 38.French MT, Fang H, Balsa AI. Longitudinal analysis of changes in illicit drug use and health services utilization. Health Serv Res. 2011;46:877–899. doi: 10.1111/j.1475-6773.2010.01218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fagan J. Interactions among drugs, alcohol, and violence. Health Affairs. 1993;12:65–79. doi: 10.1377/hlthaff.12.4.65. [DOI] [PubMed] [Google Scholar]