Abstract
Background
Q fever is a zoonosis caused by Coxiella burnetii, a Gram negative bacterium present worldwide. Small ruminants are considered the main reservoirs for infection of humans. This study aimed to estimate the extent of C. burnetii infection among sheep and goats in part of The Gambia.
Methodology/Principal Findings
This survey was carried out from March to May 2012 at two areas in The Gambia. The first area comprised a cluster of seven rural villages situated 5–15 km west of Farafenni as well as the local abattoir. A second sampling was done at the central abattoir in Abuko (30 km from the capital, Banjul) in the Western Region. Serum samples were obtained from 490 goats and 398 sheep. In addition, 67 milk samples were obtained from lactating dams. Sera were tested with a Q fever ELISA kit. C. burnetii DNA was extracted from milk samples and then detected using a specific quantitative multiplex PCR assay, targeting the IS1111a element. A multivariable mixed logistic regression model was used to examine the relationship between seropositivity and explanatory variables. An overall seroprevalence of 21.6% was found. Goats had a significantly higher seroprevalence than sheep, respectively 24.2% and 18.5%. Seropositive animals were significantly older than seronegative animals. Animals from the villages had a significantly lower seroprevalence than animals from the central abattoir (15.1% versus 29.1%). C. burnetii DNA was detected in 2 out of 67 milk samples, whereas 8 samples gave a doubtful result.
Conclusion/Significance
A substantial C. burnetii seroprevalence in sheep and goats in The Gambia was demonstrated. People living in close proximity to small ruminants are exposed to C. burnetii. Q fever should be considered as a possible cause of acute febrile illness in humans in The Gambia. Future studies should include a simultaneous assessment of veterinary and human serology, and include aetiology of febrile illness in local clinics.
Introduction
Malaria has long been presumed to be the overwhelming cause of febrile illness in humans in sub-Saharan Africa. However, during the last decade a substantial decline in malaria prevalence and incidence has been observed in African countries [1]–[3]. For example, in The Gambia, during the 2008 malaria season, only 11% (24/224) of febrile episodes detected during 22 weeks follow up of a cohort of 800 children in Farafenni area were due to malaria [4]. Consequently, miss-diagnosis of presumed clinical malaria might now be present, which threatens the sustainability of currently effective antimalarial treatment, while treatable bacterial diseases that cause febrile illness are likely to be missed [2], [5]. The few studies that have been done show that these treatable bacterial diseases are often emerging or neglected zoonoses, such as Q fever [5], brucellosis [6], African tick-bite fever [7] and leptospirosis [8]. It is therefore important to get better insight into the extent of the problem of these zoonoses in the human and animal populations of sub Saharan Africa.
Q fever is a zoonosis caused by Coxiella burnetii, a Gram negative bacterium present worldwide [9]. In humans an infection with C. burnetii either goes by unnoticed or presents itself as a flu-like illness, as pneumonia, or as hepatitis. However, in 1 to 5% of cases, the disease progresses to a chronic stage characterized mainly by endocarditis or vascular infection [10], [11].
A recent study in Tanzania among hospitalized febrile patients showed that 13.5% had acute Q fever or Rickettsial infection [5]. Considering Q fever alone, the seroprevalence in apparently healthy people varies between 1% to 37% in different sub-Saharan countries [12]–[15]. In The Gambia, baseline sera from the cohort of 800 children mentioned above, were tested for antibodies against C. burnetii by ELISA, resulting in a seroprevalence of 8.3% [19].
Reservoirs of C. burnetii include many wild and domesticated mammals, birds and ticks [10]. C. burnetii is transmitted between domesticated animals such as sheep, goats, cattle, cats, and dogs, either by tick bite or through contact with infected excreta [9]. In animals, C. burnetii infection does not usually provoke severe symptoms. However, in cattle it has been associated with infertility and in small ruminants (goats and sheep) the infection can result in late abortions [16]. The massive shedding of C. burnetii during such abortions makes sheep and goats the main reservoirs responsible for infection of humans [9], [16]. Analysis of recent human Q fever outbreaks showed that these outbreaks are associated with small ruminants rather than cattle [18]. Infection of humans is primarily via inhalation of contaminated aerosols [10]. The association between high seroprevalence in humans and the prominent role of livestock breeding in many parts of sub-Saharan Africa has been suggested in several studies [13]–[14], [17]. However, as far as the authors have been able to establish, no data are available to prove this suggestion.
The objective of this study was to estimate the prevalence of C. burnetii infection among small ruminants in Farfenni area of The Gambia. This location was chosen because the Coxiella burnetii seroprevalence in children had been examined in this area in an earlier study [19].
Methods
Study Sites
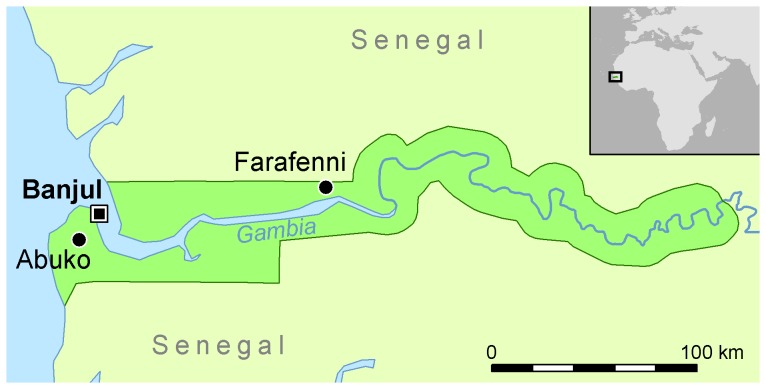
This survey was carried out from March to May 2012. In these months it is expected that the infection status of the small ruminants is stabilized, following the period of August to November during which most parturitions occur. The sampling was performed at two areas comprising different sites in The Gambia. The first area is located around Farafenni, a town situated on the Trans-Gambia Highway in the North Bank Region, just south of the border with Senegal (Figure 1). It is an important market town with a high number of travellers from Senegal. The area comprised a cluster of seven rural villages (Alkali Kunda, Jarjary, India, Yallal, Daru Yallal, Jumansareba and Conteh Kunda Nicci) situated 5–15 km west of Farafenni, as well as the local Farafenni abattoir. The villages are the same where human samples for a malaria cohort study were collected [4] and which were also used for the human Q fever survey [19].
Figure 1. Geographical location of Farafenni area, Abuko and Banjul (capital city) within The Gambia, Western Africa.
A second sampling was done at the central abattoir in Abuko (30 km from the capital, Banjul) in the Western Region. The Animal Health and Production Services (AHPS) of The Gambia estimated 1000 sheep and 1500 goats to be living in the Farafenni area. According to AHPS records, 10 to 15 small ruminants are slaughtered daily at the local abattoir in Farafenni, whereas the central abattoir in Abuko slaughters on average 50 small ruminants a day.
Study Population
The traditional and still widely practiced livestock system in The Gambia is agropastoralism, a low-input mixed crop-livestock system with extensive grazing and a low level of integration [20]. In this type of production system livestock are dependent on natural forage and leftovers of the cropping season [20]. During the dry season sheep and goats are left free for grazing whereas in the rainy season (cropping season) the sheep and goats are either tethered in the vicinity of the village or herded so as to avoid crop damage. Most of the rural households own a few small ruminants which serve as savings or emergency cash (e.g. to pay for funerals or school fees), provide protein (meat or milk) or non-food commodities (manure, hides) and are used in religious celebrations [21]. The indigenous small ruminant breeds are the Djallonké sheep and the West African Dwarf (WAD) goats. With a height range of 40–60 cm for sheep and 30–50 cm for goats, these breeds are classified as dwarf breeds [22]. Sahelian long-legged sheep and goats from Senegal and Bali Bali sheep from Mali are however more and more often imported specially at certain religious occasions such as Tobaski (Eid al-Adha) [21]–[22].
Study Design
Preceding the sampling, introductory meetings were held in the seven villages with the community elders and owners, and at both abattoirs with the health inspectors and slaughterers. All owners gave consent for their animals to be sampled for the study. In each of the seven villages 25 sheep and 25 goats were randomly selected for sampling. At both abattoirs 156 sheep and 156 goats offered for slaughtering were targeted for sampling. This sample size, calculated using WinEpiscope 2.0 [23], was expected to enable detection of a 30% difference in seropositivity between different subpopulations, for instance sheep versus goats or young versus old animals. Assuming a statistically worst-case scenario prevalence of 50% and a confidence interval of 95%, calculations with an absolute precision of 7,85% can be realized.
Ethics Statement
The study described in this manuscript was conducted in compliance with legislation on animal experimentation and practicing veterinary medicine of both The Netherlands and The Gambia. The study is not an animal experiment, but an epidemiological study in the field using common sampling methods for routine diagnostic purposes. According to Dutch legislation, such studies do not need approval from an animal ethics committee, but they need to be performed according to the Dutch Veterinary Practice Act.
Sampling
A structured questionnaire was used to record data including the name of the owner (villages) or trader (abattoirs), species, breed, sex, estimated age, lactating or not, and, if lactating, the suckling lamb(s) or kid(s) were also sampled and their relationships were documented. In the villages milk samples were taken from the lactating dams which were included in the serum sampling. Age was estimated by dentition as defined earlier [21].
Blood samples were collected from the jugular vein in evacuated blood collecting tubes of 8 ml (Greiner Bio-One, Kremsmünster, Austria), using 20 G×1.5 Multi-Sample Blood Collection needles (Greiner Bio-One, Kremsmünster, Austria). The tubes were left at ambient temperature for circa 1 hour and then stored in a cool box on ice and/or in a refrigerator. Samples were centrifuged within 18 hours (2500 g,10 min) and serum samples were then stored frozen.
After cleaning the teats with disinfectant wipes and forestripping, milk samples were collected in 15 ml polystyrene milk tubes (Greiner Bio-One, Kremsmünster, Austria). Milk samples were preserved with Broad Spectrum Microtabs II (D&F Control Systems, Norwoord, USA), containing bronopol and natamycin. The milk samples were stored frozen until testing.
Diagnostic Tests
Sera were tested with the Q fever LSI ELISA kit (LSI, Lissieu, France) [24], according to manufacturer’s instructions. In addition to the negative and positive control samples supplied by the ELISA kit, an extra positive control sample was added to every plate. This extra control was adjusted to a titer just above the cut off value of the test. The results were expressed as optical density Sample/Positive control (S/P) ratio, corrected for the negative control. A serum sample was considered to be positive when the S/P ratio of the serum was >40 and seronegative ≤40.
DNA was extracted from the milk using the NucliSens easyMag extractor (bioMérieux, Marcy l’Etoile, France) according to the manufacturer’s recommendations. In case of repeated errors, DNA extraction was performed using a DNA tissue kit (DNeasy Blood and Tissue kit; QIAGEN, Hilden, Germany) according to the manufacturer’s guidelines. C. burnetii DNA was detected using a specific quantitative multiplex PCR assay, targeting the IS1111a element. Positive, negative and inhibition controls were included, as described earlier [25]. A milk sample was considered positive when the cycle threshold (Ct) value was ≤36, negative when the Ct was ≥40 and doubtful when the Ct was between >36 and <40. The source for the thresholds is the repeatability in goat milk: below the lower threshold (positive result) the repeatability is 100%; above the threshold and the negative result (doubtful result) the repeatability is decreasing towards zero.
Statistical Analyses
A multivariable mixed logistic regression model was used to examine the relationship between seropositivity and explanatory variables ‘species’, ‘breed’, ‘sex’, ‘age’ and ‘location’. The latter included as a random effect [26], as animals from the same study site might not be independent of each other. Most variables, including the dependent variable, were dichotomous. Age was classified in three groups: <1 year, 1–3 years and ≥4 years. Location was categorized based on the three study sites: villages Farafenni area, Farafenni abattoir and Abuko abattoir.
A backward stepwise selection on the full model was performed to find the best fitting model to describe the dataset. Selection of the best fitting model was based on the value of Akaike’s Information Criterion (AIC). The model with the lowest AIC value was considered the best fitting model, with the AIC being the –2 * loglikelihood +2 * the number of parameters in the model. The odds ratio and 95% confidence interval for the explanatory variables were calculated. The analyses were performed using R software, version 2.12.2 [27] and package lme4, version 0.999375–42 [28] for generalized linear mixed-effects models using the Laplace approximation method.
Results
Descriptive Statistics
Serum samples were obtained from 490 goats and 398 sheep (Table 1). During the four weeks of sampling at Farafenni abattoir, the number of sheep offered for slaughter was limited to 66 sheep.
Table 1. Number of serum samples at the different study sites.
| Goats | Sheep | |
| Villages Farafenni area | 175 | 175 |
| Farafenni abattoir | 156 | 66 |
| Abuko abattoir | 159 | 157 |
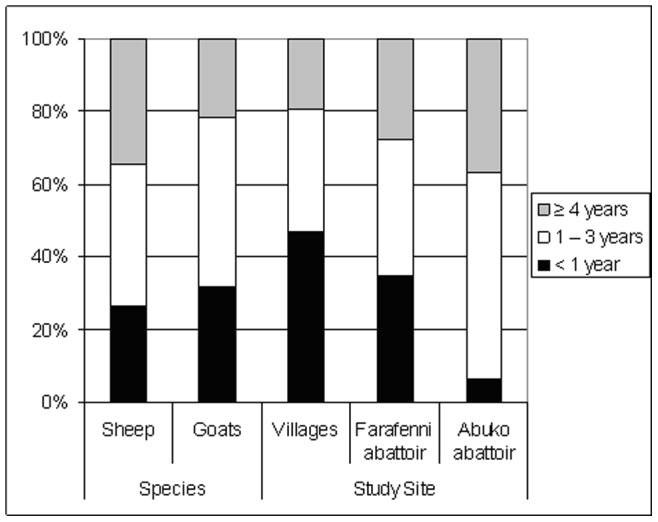
As to the sex distribution: 68.6% of the goats and 80.4% of the sheep were female. Practically all animals sampled in the villages belonged to the indigenous WAD goats and Djallonké sheep, whereas at Abuko abattoir 81.1% of the animals were exotic breeds. At Farafenni abattoir the proportion indigenous to imported breeds was 55.7% to 44.3%. Of the animals sampled in the villages 47% was younger than 1 year of age. At Abuko abattoir the middle and the oldest age groups were most prominent (Figure 2).
Figure 2. Proportion of sampled animals per age group, related to species and study site.
Milk samples were collected from lactating dams in the villages only. In total 67 milk samples from lactating dams (33 goats and 34 sheep) were collected, in conjunction with serum sampling. In each of the seven villages between 9 to 12 milk samples were collected, except for Jarjary, where only 3 milk samples could be obtained.
Seroprevalence and Associated Factors
The general linear model was performed based on 879 complete records, as 9 records contained missing values. Based on the AIC, the best fitting model included explanatory variables location, age and species. The degree of clustering within the 9 different locations (two abattoirs and seven villages) was very small in the general mixed model with a variance of 2.3927e-14. In the best fitting model the correlation was negligible (σ2 = 0). The best fitting model showed no significant difference in the odds of seropositivity in animals being offered for slaughtering at Farafenni abattoir or at Abuko abattoir (OR 0.78, p = 0.26) (Table 2).
Table 2. Risk of being anti-Coxiella burnetii antibody seropositive associated with animal characteristics and demographics, multivariable mixed logistic regression.
| Variable | Number of animals | Seroprevalence (%) | ||||
| OR | 95% CI | p-value | ||||
| Total | 879 | 21.6 | ||||
| Location | Abuko abattoir | 313 | 29.1 | 1.0 (ref.) | ||
| Farafenni abattoir | 221 | 21.3 | 0.78 | 0.51–1.20 | 0.26 | |
| Villages | 345 | 15.1 | 0.61 | 0.40–0.91 | 0.02 | |
| Estimated age group | <1 year | 256 | 9.8 | 1.0 (ref.) | ||
| 1–3 years | 379 | 26.1 | 2.78 | 1.69–4.56 | 5.46e-05 | |
| ≥4 years | 244 | 27.0 | 3.10 | 1.83–5.25 | 2.67e-05 | |
| Species | Goat | 484 | 24.2 | 1.0 (ref.) | ||
| Sheep | 395 | 18.5 | 0.65 | 0.46–0.92 | 0.02 | |
OR, Odds ratio; CI, confidence interval.
Animals located in the villages on the other hand had a significantlylower seroprevalence than animals offered for slaughtering at Abuko abattoir (OR 0.61, p = 0.02). Seropositive animals were significantly older than seronegative animals (Table 2). Sheep had a significantly lower risk of being seropositive as compared to goats (OR 0.65, p = 0.02).
Milk Samples; PCR Analysis and Relation to Seroprevalence Results
C. burnetii DNA was detected in 2 out of 67 milk samples, whereas 8 samples gave a doubtful (i.e. Ct values >36 and ≤40) result. In 57 samples no Coxiella DNA was found. One of the dams with a positive milk sample was seropositive; three dams with a doubtful PCR result also were seropositive.
Of the 67 lactating dams, 19 (28.4%) were seropositive and 48 (71.6%) were seronegative. The serum of 14 kids of the seropositive lactating dams and 39 kids of the lactating seronegative dams were included in the sampling. These kids were all less than 12 months of age, with a minimum of one week of age. From the seropositive lactating dams two kids (14.3%) were seropositive and of the seronegative lactating dams no kids were seropositive. This difference is not significant (Fisher’s exact test, p = 0.081).
Discussion
In this study in The Gambia, 18.5% of sheep and 24.2% of goats had antibodies to C. burnetii. To our knowledge, this is the first seroprevalence study of C. burnetii in sheep and goats in West Africa. A recent literature review on the prevalence of C. burnetii infection in domestic ruminants in different countries worldwide, revealed a wide variation in reported prevalence and study quality [17]. The overall mean prevalences on animal level were 15% and 27% for sheep and goats respectively [17]. Out of the 69 publications reviewed, only four studies on small ruminants were performed in African countries [17]. In a well-designed study in Chad, Central Africa, seroprevalences of 11% and 13% were found in sheep and goats respectively [29]. Results of our study showed a higher seroprevalence among small ruminants, which suggests that Q fever is of considerable importance in the small ruminant population in The Gambia.
The age of the animals appeared to be the most significant risk factor for seropositivity. The older the animals are, the higher the risk of being seropositive. This difference was especially notable between animals younger than 1 year of age versus older animals. Animals between 1 to 3 years of age and animals of 4 years or older were shown to be respectively 2.8 and 3.1 times more likely to be seropositive as compared to animals younger than 1 year of age. These findings are indicative of horizontal rather than vertical transmission. C. burnetii infections usually induce an immune response which provides long-lasting protection against further disease [9]. However, the risk of being seropositive seems to reach a plateau, after which seroprevalence decreases slightly with age.
Taking into account all other variables in the model, the odds of being seropositive for animals located at the villages was 0.6 (lower risk) as compared to animals being offered for slaughtering at Abuko abattoir. At Abuko abattoir animals from all over the country and abroad are assembled [21]. As such, these animals might originate from entirely different populations with different prevalence figures. In contrast with Farafenni abattoir, where animals are slaughtered directly, most animals arriving at Abuko are kept at the adjoining marketplace preceding slaughtering. Animals at Abuko are sometimes kept several months before being slaughtered [21]. In addition, to what extent these animals are a random selection of these populations is unknown, as selection criteria used by livestock keepers to sell a specific animal are not identified. However, the majority of animals offered for slaughtering appeared to be clinically healthy, which matches with earlier observations [21]. As such, a difference in origin, (extensive) travelling and assembling, and a prolonged stay at the adjoining marketplace, are possible risk factors for the higher C. burnetii seroprevalence found in sheep and goats offered for slaughtering at Abuko abattoir.
Furthermore, in the present study sheep appeared to have a significantly lower risk of being seropositive as compared to goats. Differences in intrinsic susceptibility to C. burnetii between sheep and goats have not been described in the literature. Some studies found higher seroprevalences in sheep [30]–[32], whereas others found higher seroprevalences in goats [29]. Although the LSI ELISA kit uses antigen of an ovine strain, due to the use of a monoclonal anti-protein G HRP labeled conjugate, the test is equally suitable for bovine, ovine and caprine species. An in-house validation of the test by the Central Veterinary Institute (The Netherlands) found similar results in known positive and negative sera from both sheep and goats (unpublished results). As such, transmission within the Gambian sheep population seems to be different from that in the goat population, and there probably is no random mixing between the species.
Most small ruminants in The Gambia are kept in free-roaming village-based flocks with only limited management or capital inputs [33]. During the dry seasons, most of the animals roam freely, but sheep stay closer to the villages than goats [34]. In addition, village-based sheep in The Gambia are more often tethered at night as compared to village-based goats [34]. On the other hand, in case goats are tethered at night, their night shelters are more often provided with a roof and wall as compared to the shelters of sheep [34]. In terms of exchange for cash or kind, goats are considered the cheapest form of trade followed by sheep, donkeys, cattle and finally, horses [33]. In addition, sheep are preferred for slaughter when celebrating religious festivities or ceremonies, whereas goats are preferred for commercial slaughter and the preparation of afra (grilled meat) [21]. This explains the limited number of sheep offered for slaughtering at the local abattoir in Farafenni during the sampling period. In addition, the differences in trade value and accompanying management practices might explain the difference in seropositivity between the two species.
In a small proportion of lactating dams C. burnetii DNA was found in the milk, while a larger proportion of milk samples gave a doubtful result. This indicates that only low Coxiella DNA loads were detected. Shedding prevalence is an indicator of current infection and can be used as a measure to estimate the risk of transmission between ruminants and from ruminants to humans [17]. However, shedding of C. burnetii through milk may be continuous or intermittent [9]. Additionally, some animals seroconvert without detectable shedding, whereas other shedding animals may never seroconvert [35], although this has been questioned and might be explained by cross contamination for the environment [36].
C. burnetii can survive in the open for weeks and is highly infectious [10]. A clear relationship between dry weather, strong wind, and the spread of infection in dust from a variety of animal sources has been reported [9]. In addition, areas with low vegetation densities and low groundwater levels are more prone to transmission over large areas [37]. The climate in The Gambia is semi-arid with distinct dry (December to June) and wet (July to November) seasons [21]. In an earlier study it was found that the number of parturitions in sheep and goats in The Gambia was higher between August and November as compared to other months [34]. As ruminants have been reported to shed large amounts of bacteria during parturition [9], [16] and as the bacterium is highly resistant [10], the onset of the dry season, which is accompanied by strong winds, can be considered as a high risk period. Hence, an incident resulting in shedding of large numbers of bacteria may quickly impact a large area.
In the human survey, based on sera collected for a malaria study in 2008, the average seroprevalence in the same seven villages found was 8.8%, ranging from 5.1 to 14.3% [19]. Both the veterinary and human data show significant differences in seroprevalence between the villages. Comparing the human and veterinary seroprevalence data, the results show a poor correlation. Direct relationships between the seroprevalence in the children and the small ruminants in the Farafenni villages could not be demonstrated, because demographic information was lacking and because of the four-year time difference between the collection of the human and the veterinary data. However, given the fact that antibodies to C. burnetii are present in significant numbers in both humans and animals, possible linkage should be investigated further. In order to determine to what extent C. burnetii prevalence rates in humans and animals interact, more data will have to be collected simultaneously on both humans and animals in different geographical locations. Furthermore, more research could be carried out in villages with both high and low prevalence rates in humans and animals, in order to determine what types of human behavior or interaction with animals might cause higher incidence levels.
This serological survey of C. burnetii seroprevalence in small ruminants in The Gambia demonstrates a considerable prevalence of current or past infection in the sheep and goat population. The species and age of the animals as well as their location and origin are of influence on the seropositivity of C. burnetii. Although a direct link between the human and veterinary data could not be demonstrated, there are clear zoonotic implications. C. burnetii is highly contagious and very resistant in the environment. People living in a Q fever endemic area are at risk of getting infected. To avoid incorrect diagnoses of febrile illnesses as being malaria, resulting in an overuse of anti-malarial drugs, it is important that other prevalent (treatable) causes are considered and can be diagnosed. As such, Q fever is one of the diseases that should be taken into account. While malaria rapid diagnostic tests are now widely available, there is a need for low-cost point-of-care diagnostics for non-malarial febrile illness. Simultaneous assessments of veterinary and human serology with aetiologic studies of febrile illness in local clinics would provide important information of the importance of zoonotic pathogens such as C. burnetii.
Acknowledgments
We wish to thank the villagers of Farafenni, and the health inspectors and slaughterers of both Farafenni and Abuko abattoir for their collaboration. The General Hospital and adjacent Public Health Office of the North Bank, East Farafenni are greatly acknowledged for the use of their centrifuging and storing facilities. The authors are also grateful to the National Public Health Laboratories in Kotu, part of the Ministry of Health and Social Welfare, for their hospitality concerning the usage of their laboratory facilities. We thank Betty van Gelderen for her assistance in the laboratory activities and Hans Vernooij for his assistance in the statistical analyses. We thank Marianne van der Sande (National Institute for Public Health and the Environment) for critically reviewing an earlier version of the manuscript.
Funding Statement
This project was funded by a grant of the Dutch Ministry of Economic Affairs. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Rodrigues A, Schellenberg JA, Kofoed PE, Aaby P, Greenwood B (2008) Changing pattern of malaria in Bissau, Guinea Bissau. Trop Med Int Health 13: 410–417. [DOI] [PubMed] [Google Scholar]
- 2.Reyburn H, Mbakilwa H, Mwangi R, Mwerinde O, Olomi R, et al. (2007) Rapid diagnostic tests compared with malaria microscopy for guiding outpatient treatment of febrile illness in Tanzania: randomised trial. BMJ, doi: 10.1136/bmj.39073.496829.AE. [DOI] [PMC free article] [PubMed]
- 3. Gething PW, Kirui VC, Alegana VA, Okiro EA, Noor AM, et al. (2010) Estimating the number of paediatric fevers associated with malaria infection presenting to Africa’s public health sector in 2007. PLoS Med 7(7): e1000301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ceesay SJ, Casals-Pascual C, Nwakanma DC, Walther M, Gomez-Escobar N, et al. (2010) Continued decline of malaria in The Gambia with implications for elimination. PLoS ONE 5(8): e12242 10.1371/journal.pone.0012242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Prabhu M, Nicholson WL, Roche AJ, Kersh GJ, Fitzpatrick KA, et al. (2011) Q fever, spotted fever group, and typhus group rickettsioses among hospitalized febrile patients in northern Tanzania. Clin Infect Dis 53(4): e8–e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Maichomo MW, McDermott JJ, Arimi SM, Gathura PB, Mugambi TJ, et al. (2000) Study of brucellosis in a pastoral community and evaluation of the usefulness of clinical signs and symptoms in differentiating it from other flu-like diseases. Afr J Health Sci 7: 114–119. [PubMed] [Google Scholar]
- 7. Ndip LM, Bouyer DH, Travassos Da Rosa AP, Titanji VP, Tesh RB, et al. (2004) Acute spotted fever rickettsiosis among febrile patients, Cameroon. Emerg Infect Dis 10: 432–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Biggs HM, Bui DM, Galloway RL, Stoddard RA, Shadomy SV, et al. (2011) Leptospirosis among hospitalized febrile patients in northern Tanzania. Am J Trop Med Hyg 85: 275–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Aitken ID, Bögel K, Cračea E, Edlinger E, Houwers D, et al. (1987) Q fever in Europe: current aspects of aetiology, epidemiology, human infection, diagnosis and therapy. Infection 15(5): 323–327. [DOI] [PubMed] [Google Scholar]
- 10. Raoult D, Marrie TJ, Mege JL (2005) Natural history and pathophysiology of Q fever. Lancet Infect Dis 5: 219–226. [DOI] [PubMed] [Google Scholar]
- 11. Kampschreur LM, Dekker S, Hagenaars JC, Lestrade PJ, Renders NH, et al. (2012) Identification of risk factors for chronic Q fever, the Netherlands. Emerg Infect Dis 18(4): 563–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kobbe R, Kramme S, Kreuels B, Adjei S, Kreuzberg C, et al. (2008) Q fever in young children, Ghana. Emerg Infect Dis 14(2): 344–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tissot Dupont H, Brouqui P, Faugere B, Raoult D (1995) Prevalence of antibodies to Coxiella burnetii, Rickettsia conorii, and Rickettsia typhi in seven African countries. Clin Infect Dis 21: 1126–1133. [DOI] [PubMed] [Google Scholar]
- 14. Mediannikov O, Fenollar F, Socolovschi C, Diatta G, Bassene H, et al. (2010) Coxiella burnetii in humans and ticks in rural Senegal. PLoS Negl Trop Dis 4(4): e654 10.1371/journal.pntd.0000654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kelly PJ, Matthewman LA, Mason PR, Raoult D (1993) Q fever in Zimbabwe. A review of the disease and the results of a serosurvey of humans, cattle, goats and dogs. S Afr Med J 83(1): 21–5. [PubMed] [Google Scholar]
- 16. Maurin M, Raoult D (1999) Q fever. Clin Microbiol Rev 12: 518–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guatteo R, Seegers H, Taurel A-F, Joly A, Beaudeau F (2011) Prevalence of Coxiella burnetii infection in domestic ruminants: a critical review. Vet Microbiol 149: 1–16. [DOI] [PubMed] [Google Scholar]
- 18.Georgiev M, Afonso A, Neubauer H, Needham H, Thiéry R, et al. (2013) Q fever in humans and farm animals in four European countries, 1982 to 2010. Euro Surveill 18(8): pii = 20407. [PubMed]
- 19. van der Hoek W, Sarge-Njie R, Herremans T, Chisnall T, Okebe J, et al. (2013) Prevalence of antibodies against Coxiella burnetii (Q fever) in children in The Gambia, West Africa. Tropical Medicine and International Health 18: 850–853. [DOI] [PubMed] [Google Scholar]
- 20.Devendra C, Morton J, Rischkowsky B, Thomas D (2005) Livestock systems. In: Owen E, Kitalyi A, Jayasuriya N, Smith T, editors. Livestock and wealth creation; improving the husbandry of animals kept by resource-poor people in developing countries. Nottingham: National Resources International Limited. 29–52.
- 21. Goossens B, Osaer S, Kora KJ, Chandler L, Petrie JA, et al. (1998) Abattoir survey of sheep and goats in The Gambia. Vet Rec 142: 277–281. [DOI] [PubMed] [Google Scholar]
- 22. Geerts S, Osaer S, Goossens B, Faye D (2008) Trypanotolerance in small ruminants of sub-Saharan Africa. Trends Parasitol 25(3): 132–138. [DOI] [PubMed] [Google Scholar]
- 23. Thrusfield M, Ortega C, De Blas I, Noordhuizen P, Frankena K (2001) WIN EPISCOPE 2.0: improved epidemiological software for veterinary medicine. Vet Rec 148: 567–572. [DOI] [PubMed] [Google Scholar]
- 24. Horigan MW, Bell MM, Pollard TR, Sayers AR, Pritchard GC (2011) Q fever diagnosis in domestic ruminants: comparison between complement fixation and commercial enzyme-linked immunosorbent assays. J Vet Diagn Invest 23(5): 924–931. [DOI] [PubMed] [Google Scholar]
- 25. Roest HIJ, Ruuls RC, Tilburg JJHC, Nabuurs-Franssen MH, Klaassen CHW, et al. (2011) Molecular epidemiology of Coxiella burnetii from ruminants in Q fever outbreak, the Netherlands. Emerg Infect Dis 17(4): 668–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dohoo I, Martin W, Stryhn H (2009) Logistic regression with random effects. In: Dohoo I, Martin W, Stryhn H, editors. Veterinary Epidemiologic Research, second edition. Charlottetown, Prince Edward Island, Canada: VER Inc. 580–584.
- 27.R Development Core Team (2011) R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. ISBN 3-900051-07-0. Available: http://www.R-project.org/.
- 28.Bates D, Maechler M, Bolker B (2011) lme4: Linear mixed-effects models using S4 classes. R package version 0.999375-42. Available: http://CRAN.R-project.org/package=lme4.
- 29. Schelling E, Diguimbaye C, Daoud S, Nicolet J, Boerlin P, et al. (2003) Brucellosis and Q-fever seroprevalences of nomadic pastoralists and their livestock in Chad. Prev Vet Med 61: 279–293. [DOI] [PubMed] [Google Scholar]
- 30. Ruiz-Fons F, Astobiza I, Barandika JF, Hurtado A, Atxaerandio R, et al. (2010) Seroepidemiological study of Q fever in domestic ruminants in semi-extensive grazing systems. BMC Vet Res 6: 3 10.1186/1746-6148-6-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ryan E, Kirby M, Clegg T, Collins DM (2011) Seroprevalence of Coxiella burnetii antibodies in sheep and goats in the Republic of Ireland. Vet Rec 169(11): 280 10.1136/vr.d5208 [DOI] [PubMed] [Google Scholar]
- 32. Vaidya VM, Malik SVS, Bhilegaonkar KN, Rathore RS, Kaur S, et al. (2010) Prevalence of Q fever in domestic animals with reproductive disorders. Comp Immunol Microb 33: 307–321. [DOI] [PubMed] [Google Scholar]
- 33.Osaer S, Goossens B (1999) Trypanotolerance in Djallonké sheep and West African Dwarf goats in The Gambia: importance of trypanosomosis, nutrition, helminth infections and management factors. PhD thesis. Utrecht: Utrecht University, 300. [Google Scholar]
- 34. Osaer S, Goossens B, Kora S, Gaye M, Darboe L (1999) Health and productivity of traditionally managed Djallonké sheep and West African Dwarf goats under high and moderate trypanosomosis risk. Vet Parasitol 82: 101–119. [DOI] [PubMed] [Google Scholar]
- 35. McQuiston JH, Childs JE, Thompson HA (2002) Q fever. J Am Vet Med Assoc 221: 796–799. [DOI] [PubMed] [Google Scholar]
- 36. Roest HJ, van Gelderen B, Dinkla A, Frangoulidis D, van Zijderveld F, et al. (2012) Q Fever in pregnant goats: pathogenesis and excretion of Coxiella burnetii . PLoS ONE 7(11): e48949 10.1371/journal.pone.0048949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Van der Hoek W, Hunink J, Vellema P, Droogers P (2011) Q fever in The Netherlands: the role of local environmental conditions. Int J Environ Health Res 21(6): 441–451. [DOI] [PubMed] [Google Scholar]