Abstract
Background
This study aims to describe trends in the rate of acute myocardial infarction (AMI) and use of percutaneous coronary interventions (PCI) in patients with and without type 2 diabetes in Spain, 2001–2010.
Methods
We selected all patients with a discharge of AMI using national hospital discharge data. Discharges were grouped by diabetes status: type 2 diabetes and no diabetes. In both groups PCIs were identified. The cumulative incidence of discharges attributed to AMI were calculated overall and stratified by diabetes status and year. We calculated length of stay and in-hospital mortality (IHM). Use of PCI was calculated stratified by diabetes status. Multivariate analysis was adjusted by age, sex, year and comorbidity. Results: From 2001 to 2010, 513,517 discharges with AMI were identified (30.3% with type 2 diabetes). The cumulative incidence of discharges due to AMI in diabetics patients increased (56.3 in 2001 to 71 cases per 100,000 in 2004), then decreased to 61.9 in 2010. Diabetic patients had significantly higher IHM (OR, 1.14; 95%CI, 1.05–1.17). The proportion of diabetic patients that underwent PCI increased from 11.9% in 2001 to 41.6% in 2010. Adjusted incidence of discharge in patients with diabetes who underwent PCI increased significantly (IRR, 3.49; 95%CI, 3.30–3.69). The IHM among diabetics patients who underwent a PCI did not change significantly over time.
Conclusions
AMI hospitalization rates increased initially but declining slowly. From 2001 to 2010 the proportion of diabetic patients who undergo a PCI increased almost four-fold. Older age and more comorbidity may explain why IHM did not improve after a PCI.
Introduction
Diabetes is a major risk factor for atherosclerosis, which predisposes patients to occlusive coronary artery disease (CAD), acute myocardial infarction (AMI), and death [1]. It is well established that the long-term prognosis of AMI is worse in patients with diabetes than in those without diabetes [2], [3]. In fact, the mortality rate for AMI is approximately double in patients with diabetes [3].
Patients with diabetes are prone to a diffuse and rapidly progressive form of CAD, which increases their likelihood of undergoing revascularization procedures [4]. Approximately one-third of all percutaneous coronary interventions (PCI) performed each year in the US are in patients with diabetes [5]. As the prevalence of diabetes increases, the number of patients with diabetes requiring revascularization for advanced CAD will escalate [6]. Although management of patients with CAD has improved considerably, coronary event rates remain very frequent, and mortality is greater among patients with diabetes [7].
Secular trends in the use of PCI in patients with diabetes have been examined [8], [9]. In the UK, Vamos et al. [9] found that PCI rates increased significantly (IRR, 1.01, 95%CI, 1.005–1.03) in people with diabetes during 2004–2009. However, no studies have investigated national trends in the use and outcomes of PCI after AMI in diabetic patients in Spain.
In this study, we used national hospital discharge data to describe trends in the rate of AMI and use of PCI in patients with and without type 2 diabetes between 2001 and 2010 in Spain. In particular, we analyzed patient comorbidities and in-hospital outcomes such as length of stay and in-hospital mortality (IHM). Finally we analyzed the association between the use of PCI and IHM.
Materials and Methods
Ethics Statement
The Spanish National Hospital Database (CMBD) is hosted by the Ministry of Health Social Services and Equality (MSSSI). Researchers working in public and private institutions can request the databases by filling, signing and sending the questionnaire available the MSSSI web [10]. In the questionnaire the following information is required: 1. Researchers information. 2. Variables (years, diagnosis, procedures, outcomes and socio-demographic variables). 3. Objectives. 4. Analysis of patient records. 5. Proposed results dissemination. 6. Confidentiality Commitment.
All data used in this investigation was anonymized and de-identified by the MSSSI before it was provided to us.
Our investigation was presented and approved by the Institutional Review Board of the Rey Juan Carlos University.
According to the Confidentiality Commitment signed with the MSSSI we cannot provide anonymized or de-identified data to other researchers upon request. These researchers must request the data directly to the MSSSI.
Design
We performed a retrospective, descriptive, epidemiology study using the CMBD, which compiles all public and private hospital data and therefore covers more than 95% of hospital discharges [11]. The CMBD is managed by the MSSSI and includes patient variables (sex, date of birth), date of admission, date of discharge, up to 14 discharge diagnoses, and up to 20 procedures performed during the admission. The MSSSI sets standards for registration and performs periodic audits [11].
We selected discharges for AMI in patients whose main medical diagnosis was classified according to the International Classification of Diseases-Ninth Revision, Clinical Modification (ICD-9-CM), codes 410.0–419.0. Discharge grouped by diabetes status as follows: no diabetes and type 2 diabetes (ICD-9-CM codes 250.x0 and 250.x2). Patients with type 1 diabetes were excluded (ICD-9-CM codes: 250.x1; 250.x3). PCIs were identified using the ICD-9-CM codes 00.66, 36.06, and 36.07.
We calculated the cumulative incidence of discharge rates after AMI for patients with type 2 diabetic and non-diabetes patients per 100,000 inhabitants. We also calculated the yearly age- and sex-specific cumulative incidence rates for diabetic and non-diabetic patients by dividing the number of cases by year, sex, and age group by the corresponding number of people in that population group according to data from the Spanish National Institute of Statistics, as reported at December 31 of each year [12].
The outcomes of interest included the proportion of patients who died during admission (IHM) and the mean length of hospital stay (LOS).
Clinical characteristics included information on overall comorbidity at the time of surgery, which was assessed by computing the Charlson comorbidity index (CCI). The index applies to 17 disease categories whose scores are totaled to obtain an overall score for each patient [13]. The index is subsequently categorized into three levels: 0, no disease; 1, one or two diseases; and 3, more than three diseases. To calculate the CCI we used 15 disease categories, excluding diabetes and AMI, as described by Thomsen RW et al. [14].
The percentage of use of PCI was calculated during the study period in patients with and without type 2 diabetes. We calculated LOS and IHM after PCI by diabetes status.
Statistical Analysis
A descriptive statistical analysis was performed. Statistical significance was set at p<0.05 (2-tailed). In order to test the time trend in the use of PCI, we fitted separate Poisson regression models for patients with and without type 2 diabetes, using year of discharge, sex, age, and CCI as independent variables. For IHM, logistic regression analyses were performed with mortality as a binary outcome using the same variables for the group with and without diabetes and for the entire population. Statistical analyses were performed using Stata version 10.1 (Stata, College Station, Texas, USA).
Results
During the 10-year study period, 513,517 discharges with AMI were identified. Patients with type 2 diabetes accounted for 30.3% of the total (155,676). Mean age was 67.26±13.95 years, and 60.5% were men. In patients without diabetes, the mean age was 71.38±11.18 years, and 73.2% were men (p<0.05).
Table 1 shows the annual hospital discharges rates for patients with and without type 2 diabetes. The cumulative incidence of discharges due to AMI in patients with diabetes increased from 56.3 cases per 100,000 inhabitants in 2001 to 71 cases per 100,000 inhabitants in 2004 and then decreased to 61.9 cases per 100,000 inhabitants in 2010. Cumulative incidence was significantly higher for men in both groups and in all the years studied.
Table 1. Hospital discharges due to acute myocardial infarction among patients with and without type 2 diabetes in Spain, 2001–2010.
| With Type 2 Diabetes | Without Diabetes | |||||||
| Year | Total | Incidence | LOS (SD) | %IHM | Total | Incidence | LOS (SD) | % IHM |
| 2001 | 12235 | 56.3 | 10.4(8.5) | 13.2 | 34131 | 156.9 | 9.9(9.4) | 11.2 |
| 2002 | 13864 | 62.9 | 10.6(9.1) | 13.8 | 36904 | 167.5 | 9.8(9.6) | 10.5 |
| 2003 | 15955 | 70.7 | 10.4(9.1) | 12.9 | 36870 | 163.5 | 9.3(8.6) | 10.3 |
| 2004 | 16396 | 71 | 10(8.3) | 11.8 | 36550 | 158.3 | 9.1(10.3) | 9.7 |
| 2005 | 16608 | 70.4 | 9.8(8.4) | 12.1 | 36187 | 153.4 | 8.8(8.8) | 9.2 |
| 2006 | 15754 | 65.4 | 9.6(8.7) | 11.2 | 35566 | 147.5 | 8.5(8.4) | 8.5 |
| 2007 | 16082 | 65.3 | 9.2(8.6) | 11.0 | 35537 | 144.4 | 8.3(8.9) | 8.5 |
| 2008 | 16221 | 64.6 | 9.2(8.3) | 10.6 | 35799 | 142.5 | 8.1(8.7) | 8.3 |
| 2009 | 16390 | 63.9 | 8.9(9.6) | 9.8 | 35309 | 137.7 | 7.8(8.3) | 7.9 |
| 2010 | 16171 | 61.9 | 8.6(9) | 9.8 | 34988 | 133.8 | 7.7(9.5) | 7.7 |
| Total Men | 94199 | 83.1 | 9.5(8.9) | 9.4 | 262013 | 231.1 | 8.6(9.1) | 7.4 |
| Total Female | 61477 | 50.1 | 9.9(8.6) | 14.9 | 95828 | 78.1 | 9(9.1) | 14.1 |
| Total | 155676 | 65.2 | 9.6(8.8) | 11.5 | 357841 | 149.9 | 8.7(9.1) | 9.2 |
Cumulative Incidence per100,000. Cumulative Incidence was calculated using the Spanish National Statistics Institute census projections [11]. LOS (SD): Mean length of stay (standard deviation). %IHM: In-Hospital Mortality.
The mean length of stay fell from 10.4 days in 2001 to 8.6 days in 2010 for patients with type 2 diabetes (p<0.05) and from 9.9 days in 2001 to 7.7 days in 2010 for patients without diabetes (p<0.05). LOS was significantly higher among men and women with than without diabetes in all the years analyzed (p<0.05).
Patients with type 2 diabetes had significantly higher IHM than patients without diabetes (11.5% vs. 9.2%). IHM decreased significantly from 13.2% in 2001 to 9.8% in 2010 among diabetic adults and from 11.2% to 7.7% among non-diabetic adults.
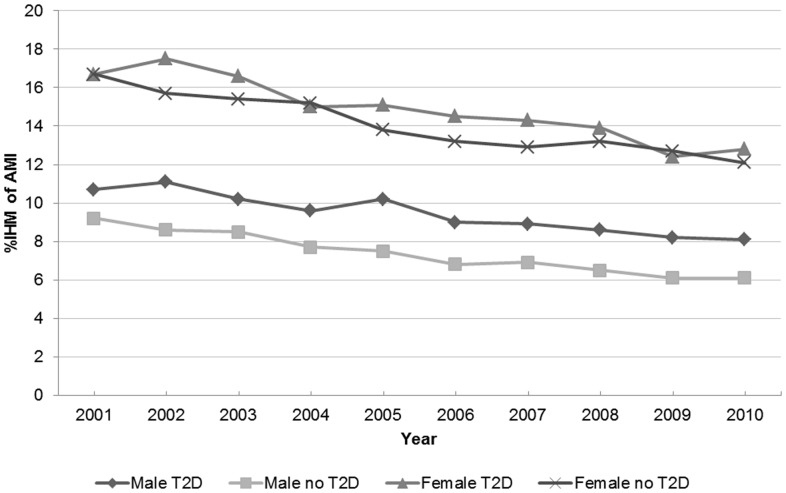
IHM decreased for both sexes, although it was always greater in women with type 2 diabetes than in men with type 2 diabetes (Figure 1).
Figure 1. In-hospital mortality after AMI in patients with and without type 2 diabetes according to sex.
IHM of AMI: In-hospital mortality after acute myocardial infarction. Male T2D: Men with type 2 diabetes. Male no T2D: Men without type 2 diabetes. Female T2D: Women with type 2 diabetes. Female without T2D: Women without type 2 diabetes.
Table 2 presents the results of a multivariate analysis of the factors associated with cumulative incidence and IHM after AMI. When the year 2004 was used as the reference and after controlling for possible confounders, we observed that the cumulative incidence of discharges in patients with type 2 diabetes did not change significantly after this year (IRR, 0.98; 95%CI, 0.96–1.01).
Table 2. Multivariate analysis of the factors associated with cumulative incidence and in-hospital mortality after acute myocardial infarction in patients with and without type 2 diabetes in Spain, 2001–2010.
| With Type 2 Diabetes | Without Diabetes | ||||
| Incidence (IRR)* | IHM (OR)† | Incidence (IRR)* | IHM (OR)† | ||
| Age (years) | 35–60 years | 1 | 1 | 1 | 1 |
| 61–70 years | 1.32 (1.30–1.34) | 1.97 (1.82–2.13) | 1.58 (1.54–1.61) | 2.05 (1.95–2.16) | |
| 71–80 years | 2.11 (2.07–2.14) | 3.46 (3.23–3.71) | 1.23 (1.21–1.25) | 3.99 (3.82–4.17) | |
| >80 years | 1.21 (1.19–1.22) | 5.84 (5.45–6.30) | 1.72 (1.69–1.75) | 7.79 (7.46–8.15) | |
| Sex | Men | 1 | 1 | 1 | 1 |
| Female | 0.65 (0.64–0.66) | 1.28 (1.24–1.32) | 0.37 (0.36–0.38) | 1.28 (1.25–1.32) | |
| Charlson Index | 0 | 1 | 1 | 1 | 1 |
| 1–2 | 0.82 (0.81–0.83) | 1.88 (1.82–1.95) | 0.51 (0.50–0.53) | 1.88 (1.83–1.92) | |
| ≥3 | 0.20 (0.19–0.21) | 2.64 (2.52–2.78) | 0.09 (0.08–0.10) | 2.76 (2.64–2.87) | |
| Year | 2001 | 0.75 (0.73–0.76) | 1 | 0.93(0.92–0.95) | 1 |
| 2002 | 0.84(0.83–0.86) | 1.03 (0.95–1.10) | 1.01(0.99–1.02) | 0.89 (0.85–0.94) | |
| 2003 | 0.97(0.95–0.99) | 0.90 (0.84–0.97) | 1.00(0.99–1.02) | 0.86 (0.82–0.90) | |
| 2004 | 1 | 0.81 (0.76–0.87) | 1 | 0.80 (0.76–0.84) | |
| 2005 | 1.01(0.99–1.03) | 0.82 (0.77–0.89) | 0.99(0.97–1.00) | 0.73 (0.70–0.77) | |
| 2006 | 0.96(0.94–0.98) | 0.76 (0.71–0.82) | 0.97(0.96–0.98) | 0.68 (0.65–0.72) | |
| 2007 | 0.98(0.96–1.00) | 0.73 (0.68–0.79) | 0.97(0.96–0.98) | 0.67 (0.64–0.71) | |
| 2008 | 0.98(0.97–1.01) | 0.69 (0.64–0.74) | 0.98(0.96–0.99) | 0.65 (0.62–0.68) | |
| 2009 | 0.99(0.98–1.02) | 0.63 (0.58–0.68) | 0.97(0.95–0.98) | 0.61 (0.58–0.65) | |
| 2010 | 0.98 (0.96–1.01) | 0.63 (0.58–0.68) | 0.96(0.94–0.97) | 0.61 (0.58–0.64) | |
| PCI | Yes | 1 | 1 | ||
| No | 2,44 (2,32–2,56) | 2,56 (2,42–2,66) | |||
IHM: In-Hospital Mortality. PCI: Percutaneous Coronary Intervention.
Calculated using multivariate Poisson regression: Incidence Rate Ratios (IRR).
Calculate using logistic regression models: Odds Ratio (OR).
The logistic regression multivariate model and Poisson regression model were built using as dependent variables “death (yes/no)” and “Cumulative incidence of PCI” respectively, and as independent variables year, sex, Charlson comorbidity index, and age.
IHM was significantly greater in women with diabetes than in men with diabetes (OR, 1.28; 95%CI, 1.24–1.32) and in those with more diabetes-associated comorbidities (OR, 1.88; 95%CI, 1.82–1.95 [for those with 1 or 2 comorbidities] and OR, 2.64; 95%CI, 2.52–2.78 [for those with 3 or more comorbidities]). Those diabetic patients who did not receive a PCI had a 2.44-fold (95%CI, 2.32–256) higher probability of dying during their stay than those who underwent this procedure.
When we analyzed the entire database, patients with type 2 diabetes had significantly higher mortality than patients without diabetes after adjusting for age, gender, CCI, and year (OR, 1.14; 95%CI, 1.05–1.17).
Coronary revascularization
Between 2001 and 2010, the overall number of PCIs in Spain was 168,537 (44,331 among patients with type 2 diabetes [26.3%]). There was a considerable male predominance in both patients with and patients without diabetes (70.0% and 81.2%, respectively). The mean age at the time of the PCI was significantly higher in patients with type 2 diabetes (67.2±0.05 years vs. 62.5±0.04 years).
Among those who underwent PCI, the mean LOS was significantly higher in patients with diabetes than in those without diabetes (9.31±0.04 days vs. 8.23±0.02 days). In addition, IHM was significantly higher in patients with diabetes (4.4% vs. 3.1%).
Patients with type 2 diabetes undergoing PCIs had a higher CCI than those without diabetes (39.2% vs. 28.5% with ≥1, respectively).
Table 3 shows the time trend for annual PCIs in patients with and without type 2 diabetes in Spain during 2001–2010. We found that use of PCI increased significantly in patients with and without diabetes. In 2001, 11.9% of patients with type 2 diabetes and 16.7% of patients without type 2 diabetes underwent PCI; in 2010, the corresponding figures were and 41.6% and 50.4%. The proportion of patients who had AMI and underwent PCI was significantly higher among those without diabetes in all the years studied.
Table 3. Characteristics and outcomes of hospital discharges after percutaneous coronary intervention among patients with and without type 2 diabetes in Spain, 2001–2010.
| 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | |
| Diabetes | ||||||||||
| N* | 1,467 | 2,206 | 2,885 | 3,640 | 4,439 | 4,781 | 5,474 | 6,067 | 6,645 | 6,727 |
| %PCI* | 11.9 | 15.9 | 18.1 | 22.2 | 26.7 | 30.3 | 34.1 | 37.4 | 40.5 | 41.6 |
| Age, mean (SD)* | 65.7 | 66.2 | 66.3 | 66.6 | 66.7 | 67.2 | 67.6 | 67.9 | 67.6 | 67.8 |
| (10.2) | (10.3) | (10.5) | (10.4) | (10.6) | (10.7) | (10.7) | (10.8) | (11.1) | (11.1) | |
| Female, n (%) | 457 | 702 | 861 | 1101 | 1304 | 1435 | 1691 | 1850 | 1980 | 1925 |
| (31.1) | (31.8) | (29.8) | (30.2) | (29.3) | (30.0) | (30.8) | (30.4) | (29.8) | (28.6) | |
| CCI 0, n (%) | 965 | 1420 | 1750 | 2226 | 2758 | 3086 | 3344 | 3524 | 3897 | 3994 |
| (65.7) | (64.3) | (60.6) | (61.1) | (62.1) | (64.5) | (61.1) | (58.1) | (58.6) | (59.3) | |
| CCI 1–2, n (%)* | 456 | 709 | 1004 | 1246 | 1442 | 1482 | 1846 | 2141 | 2265 | 2247 |
| (31.1) | (32.1) | (34.8) | (34.2) | (32.5) | (31.0) | (33.7) | (35.2) | (34.1) | (33.4) | |
| CCI≥3, n (%)* | 46 | 77 | 131 | 168 | 239 | 213 | 284 | 402 | 483 | 486 |
| (3.1) | (3.5) | (4.5) | (4.6) | (5.4) | (4.5) | (5.2) | (6.6) | (7.2) | (7.2) | |
| LOS, mean (SE)* | 11.3 | 10.9 | 10.5 | 9.8 | 9.7 | 9.3 | 9.1 | 9.0 | 8.6 | 8.2 |
| (0.23) | (0.21) | (0.18) | (0.13) | (0.12) | (0.12) | (0.11) | (0.1) | (0.1) | (0.1) | |
| IHM, n (%)* | 58 | 114 | 126 | 130 | 207 | 221 | 253 | 291 | 276 | 291 |
| (3.9) | (5.1) | (4.3) | (3.6) | (4.7) | (4.6) | (4.6) | (4.8) | (4.1) | (4.3) | |
| No diabetes | ||||||||||
| N* | 5,715 | 7,624 | 8,882 | 10,252 | 12,249 | 13,216 | 14,807 | 16,325 | 17,499 | 17,637 |
| %PCI* | 16.7 | 20.6 | 24.1 | 28.1 | 33.8 | 37.1 | 41.6 | 45.6 | 49.5 | 50.4 |
| Age, mean (SD)* | 61.6 | 61.8 | 61.5 | 61.9 | 62.4 | 62.5 | 62.6 | 62.9 | 63.1 | 62.8 |
| (12.0) | (12.2) | (12.3) | (12.3) | (12.5) | (12.6) | (12.7) | (12.9) | (12.9) | (12.9) | |
| Female, n (%) | 1034 | 1363 | 1567 | 1808 | 2286 | 2526 | 2799 | 3115 | 3434 | 3473 |
| (18.0) | (17.8) | (17.6) | (17.6) | (18.6) | (19.1) | (18.9) | (19.0) | (19.6) | (19.6) | |
| CCI 0, n (%)* | 4188 | 5508 | 6367 | 7296 | 8675 | 9599 | 10548 | 11543 | 12438 | 12634 |
| (73.3) | (72.2) | (71.7) | (71.1) | (70.8) | (72.6) | (71.2) | (70.7) | (71.1) | (71.6) | |
| CCI 1–2, n (%)* | 1427 | 1968 | 2300 | 2688 | 3243 | 3262 | 3798 | 4208 | 4410 | 4339 |
| (24.9) | (25.8) | (25.9) | (26.2) | (26.4) | (24.6) | (25.6) | (25.7) | (25.2) | (24.6) | |
| CCI≥3, n (%)* | 100 | 148 | 215 | 268 | 331 | 355 | 461 | 574 | 651 | 664 |
| (1.7) | (1.9) | (2.4) | (2.6) | (2.7) | (2.6) | (3.1) | (3.5) | (3.7) | (3.7) | |
| LOS, mean (SE)* | 10.0 | 9.6 | 8.9 | 8.7 | 8.6 | 8.1 | 7.8 | 7.8 | 7.6 | 7.4 |
| (0.16) | (0.11) | (0.08) | (0.09) | (0.08) | (0.07) | (0.06) | (0.06) | (0.06) | (0.06) | |
| IHM, n (%)* | 227 | 238 | 297 | 324 | 379 | 367 | 422 | 497 | 566 | 531 |
| (3.9) | (3.1) | (3.3) | (3.1) | (3.0) | (2.7) | (2.8) | (3.0) | (3.2) | (3.0) | |
N:number of procedure; PCI:Percutaneous Coronary Intervention; SE:Standard Error;LOS:Length of stay; IHM:In-hospital mortality; CCI:Charlson comorbidity index;
p<0.05 Statistically significant differences were observed during 2001–2010.
As can be seen in Table 3, the mean age of a person with diabetes who underwent PCI was 65.7±10.2 years in 2001 and 67.8±11.1 years in 2010. The proportion of men varied from 68.9% in 2001 to 71.4% in 2010, and the prevalence of those with a CCI of ≥1 increased from 34.2% to 40.6% (p<0.05).
LOS after PCI decreased significantly during the study period in both groups of patients, showing higher values among those with diabetes in all the years analyzed (Table 3). IHM among those who underwent PCI decreased for patients without diabetes (3.9% to 3.0; p<0.05) but remained stable for those with diabetes (3.9% to 4.3%; p>0.05)
Multivariate analysis revealed that the cumulative incidence of discharge in patients with diabetes who underwent PCI increased significantly during the study period (IRR 3.49; 95%CI, 3.30–3.69) (Table 4).
Table 4. Multivariate analysis of the factors associated with cumulative incidence and mortality after percutaneous coronary intervention in patients with type 2 diabetes in Spain, 2001–2010.
| Incidence (IRR)* | In-hospital mortality (OR)† | ||
| Age (years) | 35–60 years | 1 | 1 |
| 61–70 years | 0.87 (0.85–0.89) | 1.37 (1.16–1.61) | |
| 71–80 years | 0.70 (0.68–0.71) | 2.56 (2.21–2.98) | |
| >80 years | 0.33 (0.32–0.35) | 3.31 (2.78–3.94) | |
| Sex | Men | 1 | 1 |
| Female | 0.80 (0.79–0.82) | 1.32 (1.20–1.46) | |
| Charlson Index | 0 | 1 | 1 |
| 1–2 | 0.74 (0.73–0.76) | 2.39(2.17–2.64) | |
| ≥3 | 0.51 (0.49–0.53) | 3.19 (2.73–3.73) | |
| Year | 2001 | 1 | 1 |
| 2002 | 1.32 (1.24–1.41) | 1.27 (0.92–1.76) | |
| 2003 | 1.53 (1.43–1.62) | 1.04 (0.76–1.43) | |
| 2004 | 1.86 (1.75–1.98) | 0.83 (0.60–1.14) | |
| 2005 | 2.25 (2.12–2.39) | 1.08 (0.80–1.46) | |
| 2006 | 2.52 (2.38–2.67) | 1.07 (0.80–1.45) | |
| 2007 | 2.86 (2.70–3.03) | 1.03 (0.77–1.38) | |
| 2008 | 3.16 (2.98–3.34) | 1.02 (0.75–1.36) | |
| 2009 | 3.40 (3.21–3.60) | 0.89 (0.66–1.19) | |
| 2010 | 3.49 (3.30–3.69) | 0.92 (0.69–1.23) | |
IRR: Incidence Rate Ratios calculated using multivariate Poisson regression.
OR: Odds Ratio calculated using logistic regression models.
The logistic regression multivariate model and Poisson regression model were built using as dependent variables “death (yes/no)” and “Cumulative incidence of PCI” respectively, and as independent variables year, sex, Charlson comorbidity index, and age.
After an adjusted multivariate analysis, the IHM among persons with diabetes who underwent a PCI did not change significantly over time. IHM was significantly greater in women than in men (OR 1.32; 95%CI, 1.20–1.46) and was higher in those with 1 or 2 diabetes-associated conditions (OR 2.39; 95%CI, 2.17–2.64) and ≥3 conditions (OR 3.19; 95%CI 2.73–3.73) than in those who had no associated comorbidities.
Discussion
Our results reveal that more than 30% of Spanish adults who experience AMI have an associated diagnosis of diabetes. These results are consistent with those of Gore et al. (2012) [15], who showed that 29% of patients admitted to hospital for AMI in the US had diabetes.
From 2004 to 2010, rates of hospitalization for AMI in patients with type 2 diabetes decreased, but not significantly. The results of a study in the UK showed a considerable decline in hospital discharge for AMI in patients with diabetes between 2004–2005 and 2009–2010 (OR, 0.95; 95%CI, 0.93–0.97) [9]. Our results are consistent with this finding: rates of hospitalization for AMI increased initially before leveling off in 2004 and finally declining slowly from 71 cases per 100,000 inhabitants in 2004 to 61.9 cases per 100,000 inhabitants in 2010, thus revealing the same tendency as in the UK. The changes in these rates can be attributed to favorable trends in physical activity levels and cigarette smoking and increased use of effective treatments (eg, antihypertensive agents, ACE inhibitors, and lipid-lowering drugs) [9]. We think that the lack in improvement of lifestyles among diabetic patients [16], [17] and the absence of national prevention and treatment program throughout the study period may explain the different behavior in the reduction of hospitalizations for AMI between our data and those reported by Vamos et al [9].
IHM as a consequence of AMI decreased both in patients with and in patients without type 2 diabetes. Recent studies showed that patients with and without diabetes who have experienced AMI have lower mortality rates over time, suggesting that management of AMI patients has improved in recent years [9], [18]–[20]. More frequent and effective use of PCI, which reduced IHM in our study, has been observed by other investigators [18], [20]. We found that IHM for patients who did not receive a PCI was very similar in 2001 and 2010 for both those with diabetes (14.4% to 13.6%) and those without diabetes (12.6% to 12.4%).
Consistent with the results of other studies, and after adjusting for age and gender, we found that IHM for patients with AMI was significantly greater for patients with type 2 diabetes than for those without diabetes (11.5% vs. 9.2%) [21]–[23], possibly because these patients have a worse clinical status or are at a greater risk of complications [9], [18]. In our population, the proportion of patients with diabetes and a CCI≥3 was 10.0%, whereas the proportion for those without diabetes was 5.8% (p<0.05).
Our results are similar to those of studies reporting that women have a lower cumulative incidence of AMI than men [24], [25]. However, after controlling for possible confounders, we found that women with diabetes had significantly higher IHM rates than men with diabetes. These results are consistent with those of other studies that analyze differences in diabetes between the sexes [3], [24], [25]. A recent study indicated that women with diabetes have a greater risk of mortality than men (3.44; 95%CI, 2.47–4.79), especially when diagnosed at a later stage [26]. These data suggest that factors such as the extent of treatment and monitoring, underuse of medications recommended by clinical guidelines, and reduced efficacy of active agents may be more common in women with diabetes than in men with diabetes [27], [28].
Coronary revascularization
During the study period, the number of PCIs performed in patients with type 2 diabetes increased considerably from 11.9% in 2001 to 41.6% in 2010. This result is consistent with those of other studies [9], [20], [29], in which PCI rates increased significantly owing to marked advances in stent technology and adjunctive pharmacology. One report documented the rapid progress in PCI treatment options for patients with diabetes and indicated that PCI devices (drug-eluting stents) were used more often in patients with severe comorbidities and multivessel disease and were associated with more frequent prescription of recommended cardiac medications at discharge [30].
Successful PCI has probably improved in-hospital survival rates. Therefore, IHM was more likely to be associated with patient clinical status and medical treatment strategy. Vamos et al. [9] found significant increases in IHM rates for PCI, despite technological advances in interventional techniques and improvements in periprocedural care. The authors explained their findings by referring to the increasing complexity of cases referred for PCI.
We found that IHM remained stable among diabetic patients with PCI. The higher comorbidity and older age can partially explain this lack of improvement.
In patients with AMI who had undergone PCI, women with type 2 diabetes had worse outcomes than men with diabetes. Our results are consistent with those of other studies, which suggest that the worse effect of diabetes on outcomes in women might be related to the onset mechanism of AMI, the success of the PCI procedure, and the higher burden of cardiovascular risk factors [20], [24], [31], [32].
The strength of our investigation lies in its large sample size and standardized methodology, which has previously been used to investigate diabetes in Spain and elsewhere [33], [34]. Nevertheless, our study is subject to a series of limitations. Our data source was the CMBD, an administrative database that contains discharge data for Spanish hospitalizations and uses information the physician has included in the discharge report; therefore, it does not include all the variables in the clinical history. Another limitation of this database is its anonymity (no identifying items such as number of the clinical history or the name of the hospital), which makes it impossible to detect whether the same patient was admitted more than once during the same year. In addition, patients who moved from one hospital to another would appear twice.
Nevertheless, this dataset, which was introduced in Spain in 1982, is a mandatory register, and its coverage is estimated to be more than 95% [10].
Unfortunately in Spain a validation study to assess the rate of unreported diagnosis of diabetes in administrative databases has not been conducted so far. However, a recent review and meta-analysis conducted by Leong A et al (2013) concluded that a commonly-used administrative database definition for diabetes had a pooled sensitivity of 82.3% (95%CI 75.8, 87.4) and specificity of 97.9% (95%CI 96.5, 98.8%), based on the findings of 6 studies with complete data available. While this definition appears to miss approximately one fifth of diabetes cases and wrongly classifies 2.1% of non-cases in the population as diabetes cases, it is likely sufficiently sensitive for monitoring prevalence trends in the general population if its accuracy remains reasonably stable over time [35].
We were unable to calculate diabetes-specific cumulative incidence rates, because no studies in Spain cover blood glucose measurements for the entire population; consequently, no precise estimation of the prevalence of diabetes is available [36]. Concerns have been raised about the accuracy of routinely collected datasets; however, these datasets are periodically audited. Consequently, the quality and validity of our dataset has been assessed and shown to be useful for health research [37].
In conclusion, we provide national data on changes in the burden of AMI events in Spain. Our results show that AMI hospitalization rates increased initially, before leveling off in 2004 and finally declining slowly in people with and without diabetes. Outcomes such as LOS and IHM are worse among persons with diabetes than without diabetes, although they improved over time for both groups. Higher comorbidity and female sex are associated with higher IHM.
The proportion of diabetic patients who undergo a PCI increased almost four-fold from 2001 to 2010. Older age and more comorbidity may explain why IHM among diabetic persons did not improve after a PCI during the study period.
Furthermore, given the rapid increase in prevalence of diabetes and the aging population, these findings emphasize the need for further improvement in the control of cardiovascular risk factors in people with diabetes.
Funding Statement
This study forms part of research funded by the FIS (Fondo de Investigaciones Sanitarias—Health Research Fund, grant no. PI10/00360, Instituto de Salud Carlos III). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Lüscher TF, Creager MA, Beckman JA, Cosentino F (2003) Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: Part II. Circulation 108: 1655–1661. [DOI] [PubMed] [Google Scholar]
- 2. American Diabetes Association (2008) Economic costs of diabetes in the U.S. in 2007. Diabetes Care 31: 596–615. [DOI] [PubMed] [Google Scholar]
- 3. Svensson AM, Dellborg M, Abrahamsson P, Karlsson T, Herlitz J, et al. (2007) The influence of a history of diabetes on treatment and outcome in acute myocardial infarction, during two time periods and in two different countries. Int J Cardiol 119: 319–325. [DOI] [PubMed] [Google Scholar]
- 4. Ryden L, Standl E, Bartnik M, Van den Berghe G, Betteridge J, et al. (2007) Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: executive summary. The Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD). Eur Heart J 28: 88–136. [DOI] [PubMed] [Google Scholar]
- 5. Flahert JD, Davidson CJ (2005) Diabetes and coronary revascularization. JAMA 293: 1501–1508. [DOI] [PubMed] [Google Scholar]
- 6. Aronson D, Edelman ER (2010) Revascularization for coronary artery disease in diabetes mellitus: angioplasty, stents and coronary artery bypass grafting. Rev Endocr Metab Disord 11: 75–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Action to Control Cardiovascular Risk in Diabetes Study Group (2008) Gerstein HC, Miller ME, Byington RP, Goff DC Jr, et al. (2008) Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 358: 2545–2559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Singh M, Holmes DR Jr, Gersh BJ, Frye RL, Lennon RJ, et al. (2013) Thirty-year trends in outcomes of percutaneous coronary interventions in diabetic patients. Mayo Clin Proc 88: 22–30. [DOI] [PubMed] [Google Scholar]
- 9. Vamos EP, Millett C, Parsons C, Aylin P, Majeed A, et al. (2012) Nationwide study on trends in hospital admissions for major cardiovascular events and procedures among people with and without diabetes in England, 2004–2009. Diabetes Care 35: 265–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ministry of Health Social Services and Equality. Conjunto Mínimo Básico de Datos. Available:http://www.msssi.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SolicitudCMBDdocs/Formulario_Peticion_Datos_CMBD.pdf. Accessed 23 Sep 2013.
- 11.Instituto Nacional de Gestión Sanitaria, Ministerio de Sanidad y Consumo. Conjunto Mínimo Básico de Datos, Hospitales del INSALUD. 2001; Available: http://www.ingesa.msc.es/estadEstudios/documPublica/CMBD- 2001.htm. Accessed 15 May 2013.
- 12.Instituto Nacional de Estadística (INE) Population estimates. 2010.Available: www.ine.es. Accessed 15 May 2013.
- 13. Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40: 373–383. [DOI] [PubMed] [Google Scholar]
- 14. Thomsen RW, Nielsen JS, Ulrichsen SP, Pedersen L, Hansen AM, et al. (2012) The Danish Centre for Strategic Research in Type 2 Diabetes (DD2) study: Collection of baseline data from the first 580 patients. Clin Epidemiol 4: 43–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gore MO, Patel MJ, Kosiborod M, Parsons LS, Khera A, et al. (2012) Diabetes mellitus and trends in hospital survival after myocardial infarction, 1994 to 2006: data from the national registry of myocardial infarction. Circ Cardiovasc Qual Outcomes 5: 791–797. [DOI] [PubMed] [Google Scholar]
- 16. Jiménez-García R, Hernández-Barrera V, Jiménez-Trujillo I, Garrido PC, López de Andrés A, et al. (2009) Trends in cardiovascular risk factors and lifestyle behaviors among Spanish adults with diabetes (1993–2003). J Diabetes Complications 23: 394–400. [DOI] [PubMed] [Google Scholar]
- 17. Jiménez Trujillo I, Jiménez García R, Vazquez-Fernandez del Pozo S, Hernández Barrera V, Carrasco Garrido P, et al. (2010) Trends from 1995 to 2006 in the prevalence of self-reported cardiovascular risk factors among elderly Spanish diabetics. Diabetes Metab 36: 29–35. [DOI] [PubMed] [Google Scholar]
- 18. Booth GL, Kapral MK, Fung K, Tu JV (2006) Recent trends in cardiovascular complications among men and women with and without diabetes. Diabetes Care 29: 32–37. [DOI] [PubMed] [Google Scholar]
- 19. Degano IR, Elosua R, Marrugat J (2013) Epidemiology of acute coronary syndromes in Spain: Estimation of the number of cases and trends from 2005 to 2049. Rev Esp Cardiol 66: 472–481. [DOI] [PubMed] [Google Scholar]
- 20. Ouhoummane N, Abdous B, Louchini R, Rochette L, Poirier P (2010) Trends in postacute myocardial infarction managmenent and mortality in patients with diabetes. A population-based study from 1995 to 2001. Can J Cardiol 26 (10) 523–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Whiteley L, Padmanabhan S, Hole D, Isles C (2005) Should diabetes be considered a coronary heart disease risk equivalent? Results from 25 years of follow-up in the Renfrew and Paisley survey. Diabetes Care 28: 1588–1593. [DOI] [PubMed] [Google Scholar]
- 22. Vaccaro O, Eberly LE, Neaton JD, Yang L, Riccardi G, et al. (2004) Impact of diabetes and previous myocardial infarction on long-term survival: 25-year mortality follow-up of primary screenees of the Multiple Risk Factor Intervention Trial. Arch Intern Med 164: 1438–1443. [DOI] [PubMed] [Google Scholar]
- 23. Hirakawa Y, Masuda Y, Kuzuya M, Iguchi A, Kimata T, et al. (2007) Influence of diabetes mellitus on in-hospital mortality in patients with acute myocardial infarction in Japan: a report from TAMIS-II. Diabetes Res Clin Pract 75: 59–64. [DOI] [PubMed] [Google Scholar]
- 24. Norhammar A, Stenestrand U, Lindbäck J, Wallentin L (2008) Register of Information and Knowledge about Swedish Heart Intensive Care Admission (RIKS-HIA) (2008) Women younger than 65 years with diabetes mellitus are a high-risk group after myocardial infarction: a report from the Swedish Register of Information and Knowledge about Swedish Heart Intensive Care Admission (RIKS-HIA). Heart 94: 1565–1570. [DOI] [PubMed] [Google Scholar]
- 25. Maier B, Thimme W, Kallischnigg G, Graf-Bothe C, Rohnisch JU, et al. (2006) Does diabetes mellitus explain the higher hospital mortality of women with acute myocardial infarction? Results from the Berlin Myocardial Infarction Registry. J Investig Med 54: 143–151. [DOI] [PubMed] [Google Scholar]
- 26. Roche MM, Wang PP (2013) Sex differences in all-cause and cardiovascular mortality, hospitalizations for individuals with and without diabetes, and patients with diabetes diagnosed early and late. Diabetes Care 36: 2582–2590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gouni-Berthold I, Berthold HK, Mantzoros CS, Böhm M, Krone W (2008) Sex disparities in the treatment and control of cardiovascular risk factors in type 2 diabetes. Diabetes Care 31: 1389–1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ferrara A, Mangione CM, Kim C, Marrero DG, Curb D, et al. (2008) Sex disparities in control and treatment of modifiable cardiovascular disease risk factors among patients with diabetes: Translating Research Into Action for Diabetes (TRIAD) Study. Diabetes Care 31: 69–74. [DOI] [PubMed] [Google Scholar]
- 29. Bottle A, Millett C, Khunti K, Majeed A (2009) Trends in cardiovascular admissions and procedures for people with and without diabetes in England, 1996–2005. Diabetologia 52: 74–80. [DOI] [PubMed] [Google Scholar]
- 30. Rana JS, Venkitachalam L, Selzer F, Mulukutla SR, Marroquin OC, et al. (2010) Evolution of percutaneous coronary intervention in patients with diabetes. A report from the National Heart, Lung, and Blood Institute-sponsored PTCA (1985–1986) and Dynamic (1997–2006) Registries. Diabetes Care 33: 1976–1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Champney KP, Veledar E, Klein M, Samady H, Anderson D, et al. (2007) Sex-specific effects of diabetes on adverse outcomes after percutaneous coronary intervention: trends over time. Am Heart J 153: 970–978. [DOI] [PubMed] [Google Scholar]
- 32. Blöndal M, Ainla T, Marandi T, Baburin A, Eha J (2012) Sex-specific outcomes of diabetic patients with acute myocardial infarction who have undergone percutaneous coronary intervention: a register linkage study. Cardiovasc Diabetol 11: 96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. López-de-Andrés A, Martínez-Huedo MA, Carrasco-Garrido P, Hernández-Barrera V, Gil-de-Miguel A, et al. (2011) Trends in lower-extremity amputations in people with and without diabetes in Spain, 2001–2008. Diabetes Care 34: 1570–1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. López –de-Andrés A, Jiménez-García R, Hernández-Barrera V, Gil-de-Miguel A, Jiménez-Trujillo MI, et al. (2013) Trends in utilization and outcomes of bariatric surgery in obese people with and without type 2 diabetes in Spain (2001–2010). Diabetes Res Clin Pract 99: 300–306. [DOI] [PubMed] [Google Scholar]
- 35. Leong A, Dasgupta K, Bernatsky S, Lacaille D, Avina-Zubieta A, et al. (2013) Systematic review and meta-analysis of validation studies on a diabetes case definition from health administrative records. PLoS ONE 8 (10) e75256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ruiz-Ramos M, Escolar-Pujolar A, Mayoral-Sánchez E, Corral-San Laureano F, Fernández-Fernández I (2006) Diabetes mellitus in Spain: death rates, prevalence, impact, costs and inequalities. Gac Sanit 20: 15–24. [DOI] [PubMed] [Google Scholar]
- 37. Ferreira-González I, Cascant P, Pons JM, Mitjavila F, Salas T, et al. (2008) Predicting in-hospital mortality with coronary bypass surgery using hospital discharge data: comparison with a prospective observational study. Rev Esp Cardiol 61: 843–852. [PubMed] [Google Scholar]