Abstract
Objective
Many patients dropout of treatments for Post-traumatic stress disorder (PTSD) and some clinicians believe that ‘trauma focused’ treatments increase dropout.
Method
We conducted a meta-analysis of dropout among active treatments in clinical trials for PTSD (42 studies; 17 direct comparisons).
Results
The average dropout rate was 18%, but it varied significantly across studies. Group modality and greater number of sessions, but not trauma focus, predicted increased dropout. When the meta-analysis was restricted to direct comparisons of active treatments, there were no differences in dropout. Differences in trauma focus between treatments in the same study did not predict dropout. However, trauma focused treatments resulted in higher dropout as compared to Present Centered Therapy (PCT) – a treatment originally designed as a control, but now listed as a research supported intervention for PTSD.
Conclusion
Dropout varies between active interventions for PTSD across studies, but differences are primarily driven by differences between studies. There do not appear to be systematic differences across active interventions when they are directly compared in the same study. The degree of clinical attention placed on the traumatic event does not appear to be a primary cause of dropout from active treatments. However comparisons of PCT may be an exception to this general pattern, perhaps due to a restriction of variability in trauma focus among comparisons of active treatments. More research is needed comparing trauma focused interventions to trauma avoidant treatments such as PCT.
There are a number of effective psychotherapies available for the treatment of PTSD (SCP, 2012). Approaches include treatments that focus on the traumatic event such as Prolonged Exposure (PE), Cognitive Processing Therapy (CPT), and Eye Movement Desensitization and Reprocessing (EMDR) and a variety of other interventions that do not place a primary focus on discussion of the trauma (see Foa, Keane, & Friedman, 2010 for examples). However, the average dropout rate across treatments in PTSD clinical trials is approximately 20% (Bradley et al. 2005; Hembree et al., 2003).
There are likely many factors that contribute to poor retention, but it is important to determine if psychotherapies differ in the extent to which they are tolerated. Patients may begin a treatment and find some aspect of it distressing or impractical, resulting in discontinuation. As discussed in several papers, there is ongoing debate regarding the belief that exposure based treatments, which require the patient to retell traumatic events in detail to their therapist, are especially unacceptable or poorly tolerated by patients (e.g., Foa, Zoellner, Feeny, Hembree, & Alvarez-Conrad, 2002; Hembree et al., 2003; Speckens, Ehlers, Hackmann, & Clark, 2006; Tarrier et al., 1999). It remains important to determine if trauma focused treatments result in higher dropout rates.
Dropout rates in clinical trials - the proportion of patients who begin but do not complete the full course of recommended treatment - are a common metric used to determine the tolerability of psychotherapies. A recent meta-analysis of dropout in treatments across psychological disorders found the average dropout rate was 19.7%, but this rate varied widely across studies (Swift & Greenberg, 2012). Similarly, dropout rates in PTSD clinical trials are notable for their variability. For example, the dropout rate for exposure based treatments ranges from 0% (Neuner et al., 2008) to 41% (McDonagh et al., 2005), and the dropout rate for treatments that do not focus directly on the trauma memory is similarly wide-ranging from 0% (Schaal, Elbert, & Neuner, 2009) to 48% (Cottraux et al., 2008). Clearly, evidence in regard to differential dropout rates across psychotherapies for PTSD is mixed. As estimates of dropout rates from these individual clinical trials have limitations (e.g., could be due to sampling error, characteristics of the study or research team, number of sessions, etc.), meta-analyses can provide a more robust estimate of differential dropout rates across interventions.
Three meta-analyses that have compared the dropout rates of treatment categories in PTSD (e.g., Trauma Focused Cognitive Behavioral Therapy; EMDR, etc.; Bradley, Greene, Russ, Dutra, & Westen, 2005; Bisson et al. 2007; Hembree et al. 2003). There was some evidence in the Bradley et al. meta-analysis that exposure-based treatments had higher dropout rates (e.g., Exposure + Cognitive Therapy, 33%; CBT – no exposure; 17%), but no formal statistical tests were conducted. Generally, the authors of each meta-analysis concluded that the dropout rates of active treatment categories were comparable (active treatments being those that include specific ingredients purported to decrease PTSD symptoms; Powers et al., 2010). However, there are two primary confounds that may limit this conclusion such that the relative dropout rate of active treatments is unclear. These limitations include: 1) comparing dropout rates across studies rather than direct comparisons within the same study, introducing the possibility that it is differences between studies that are captured rather than differences between treatments, and 2) the appropriate classification of active vs. control and trauma focused treatments.
Direct Comparisons
A limitation of both the Bradley et al. (2005) and Hembree et al. (2003) meta-analyses is that the comparison of treatment categories was not restricted to treatments that were directly compared in the same study (i.e., effect sizes were not obtained from the direct comparison of two treatments in the same study). Studies vary with regard to participant demographics and clinical profiles (e.g., type of trauma, chronicity of PTSD), treatment standardization, study protocol and resources, treatment length, how dropout is defined, and other unmeasured variables (Shadish & Sweeney, 1991). These differences could influence estimates of dropout when specific treatments are compared to one another across studies. For example, the number of sessions involved in a similar treatment might vary across trials with higher dropout in longer treatments (see Swift & Greenberg, 2012 for exploration of study level covariates that influence dropout rates across disorders). In addition, a trauma focused treatment might be offered in a group modality, wherein patients have less individual attention and may dropout at a higher frequency (see Schnurr et al., 2003). These differences could create the appearance of differences between approaches or obscure an actual effect.
To address the problems that may result from the comparison of dropout rates across studies, it is necessary to restrict analyses of dropout rate to the direct comparison of treatments in the same study. This eliminates the effect of between study differences on estimates of relative dropout rates across treatment approaches – essentially the number of sessions and/or group vs. individual modality are typically controlled in the same study. Bisson et al. (2007) conducted several meta-analyses of dropout in clinical trials that directly compared at least two of several treatment categories (k=38). The authors reported that there were generally no differences in dropout between comparisons of active treatments, but concerns regarding the appropriate classification of treatments limit the conclusions of this and previous meta-analyses.
Categorization
There are a variety of psychotherapies available for PTSD. As differences between approaches can be subtle, categorizing treatments entails difficult decisions about how treatments should be organized. Placing each treatment in a distinct category can introduce a variety of classification problems that may help explain why the relative tolerability of active treatments remains unclear. Three primary issues related to categorization include: 1) analyzing treatments within the same category, 2) the use of ‘catchall’ categories to classify control conditions and ‘other’ treatments, and 3) determining a treatment’s focus on the trauma memory.
First, the general process of grouping treatments allows for tests of differences between categories, but it prevents an examination of differences in dropout within treatment categories (e.g., a CBT vs. a different CBT). Many published PTSD clinical trials are comparisons of treatments within a particular category (e.g., Arntz, Tiesema, & Kindt, 2007). However, all of the published meta-analyses are comparisons of different treatment categories, and thus are not sensitive to potential differences between treatments within a category.
Second, it is difficult to categorize treatments that are not commonly tested in clinical trials (e.g., if there are few psychodynamic treatments, how should they be categorized?). This often forces researchers to use catchall categories (e.g., ‘other therapies’; Bisson et al. 2007; Bradley et al., 2005) for treatments that do not fit in primary categories. The treatments included in the catchall categories often differ in important ways from more commonly tested treatments (e.g., they are less trauma focused or non-CBT), thus an adequate test of the relative dropout rate of treatments should accommodate these treatments. However, in the Bradley et al. meta-analysis several treatments did not fit in the primary treatment categories (e.g., Psychodynamic, Hypnotherapy) and were excluded from comparisons of dropout.
Catchall categories can also result in the grouping of active treatments with interventions designed to be controls for active interventions (e.g., supportive therapy). Active interventions are typically defined as treatments that include therapeutic ingredients derived from a specific approach to psychotherapy purported to decrease PTSD symptoms (see Power et al., 2010, p.3), while control interventions (sometimes called non-specific controls) are defined as those that are designed or altered to test some aspect of a comparison treatment (Mohr et al., 2009; Wampold et al., 1997). In the Hembree et al. (2003) meta-analysis, the control category had approximately half the dropout rate of most active treatment categories (e.g., 11.4% vs. 21%), but it included active treatments, interventions designed as controls, and waitlists. In the Bisson et al. (2007) meta-analysis, the ‘other’ treatment category had a higher dropout rate than some active treatments. However, the other category included both active treatments (hypnotherapy, psychodynamic) and controls (e.g., supportive therapies).
Alternatively, some treatments designed as controls have also been erroneously categorized. Specifically, Bisson et al. (2007) noted that the category of Trauma Focused Cognitive Behavioral Therapy had a higher dropout rate than a treatment categorized as non-trauma focused CBT. However, this treatment (Present Centered Therapy [PCT] - Group; Schnurr et al. 2001; 2003) was designed as a non-specific control and excluded formal CBT components. As a further complication, PCT is now listed as an empirically supported treatment for PTSD with “strong research support” along with other primary treatments for PTSD (e.g., PE; Chambless et al., 1998; SCP, 2012). In sum, the use of catchall categories prevents a full test of the relative dropout rate of active treatments and creates ambiguity in how the results of meta-analytic comparisons should be interpreted.
Finally, previous meta-analyses estimating the relative tolerability of PTSD treatments have classified treatments into dichotomous categories based on the presence (trauma focused) or absence of a focus (non-trauma focused) on the traumatic event. A common definition used to classify treatments is based on the United Kingdom’s National Institute for Clinical Excellence Guidelines, which state, “the relevant consideration for the classification [of trauma focus] was whether or not the treatment mainly focused on the trauma memory and its meaning” (NCCMH, 2005, p.54). However, there may be important differences between the treatments included in trauma-focused and non-trauma focused categories. In the Bisson et al. (2007) meta-analysis, some treatments were classified as trauma focused despite explicit provisions prohibiting the therapist from focusing on the trauma memory itself (e.g., Marks, Lovell, Noshirvani, Livanou, & Thrasher, 1998; Tarrier et al., 1999). Other treatments that may include direct discussion of traumatic events, such as psychodynamic treatment (Brom et al., 1989) have been categorized in meta-analyses as non-trauma focused (Bisson et al., 2007; Hembree et al., 2003). A categorization scheme that allows for more variability in how the therapist deals with direct discussion of the trauma memory may provide a more sensitive test of dropout in clinical trials.
Purpose and hypotheses of the present meta-analysis
There is evidence that active interventions are similar in terms of dropout, but this evidence is limited both by the comparison of treatments across studies and various classification problems common in the meta-analysis of psychotherapies. Addressing these limitations may help resolve ongoing debates regarding the tolerability of PTSD treatments, and provide clinicians and administrators with useful information when selecting among treatment options.
The purpose of the present meta-analysis is to provide a test of differences in dropout across all direct comparisons of active treatments for PTSD, while addressing several limitations of previous categorization strategies. First, we statistically quantified the impact of between study differences on dropout by examining variability in the proportion of dropout in each active intervention across studies. Second, we restricted the meta-analysis to direct comparisons of active treatment interventions and conducted an omnibus test that avoided any classification of treatments into specific categories – allowing comparisons of treatments both within and between categories. The omnibus test avoids confounds related to categorization noted above and tests whether there are any differences in dropout between active treatments that were directly compared in the same study.
Finally, we coded each intervention according to a more graded level of trauma focus. Potential levels of trauma focus included: 1) treatments that primarily focus on retelling the traumatic event, 2) treatments that do not focus on retelling but allowed discussion of the trauma, and 3) those that refrain from any discussion of trauma. This categorization strategy provides a direct test of whether active treatments differ in the odds of dropout and allows for a more graded test of how trauma focus contributes to the tolerability of active treatments.
We expected that there would be differences in dropout rates in active treatment interventions across studies (Hypothesis 1). However, we expected there would be no differences between direct comparisons of active treatments (e.g., no differences between treatment interventions when controls were excluded; Hypothesis 2). Finally, we did not expect that differences in trauma focus between active treatments would predict dropout (Hypothesis 3).
Method
Study selection
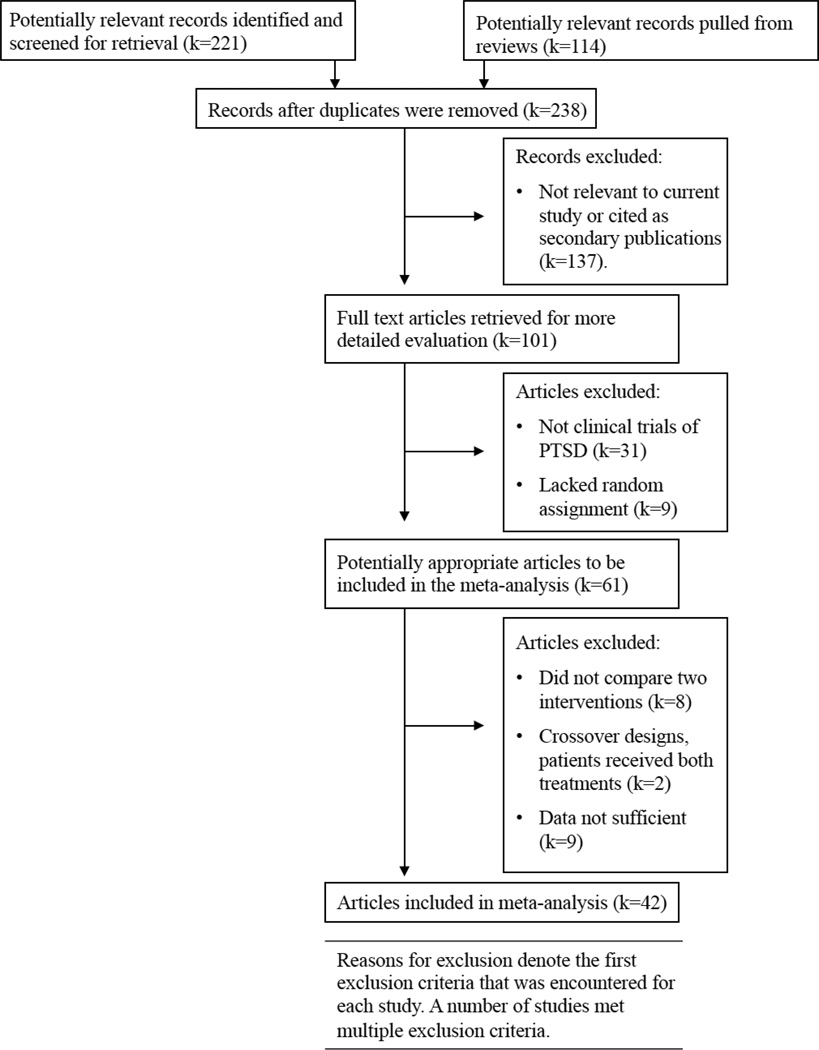
The literature search was conducted according to PRISMA guidelines for meta-analysis (Moher, Liberati, Tetzlaff, & Altman, 2009) (see Figure 1). To identify head-to-head comparisons of PTSD treatments, we performed a literature search including major databases: Pubmed, PsycInfo, using the keywords “PTSD,” “post-traumatic stress disorder,” “psychotherapy,” and “treatment.” In addition, we searched reference sections of previous meta-analyses of PTSD treatment and dropout, controlled studies of psychotherapy outcomes for PTSD, and literature reviews of PTSD treatment. The retrieval process was conducted between 10/2009 and 12/2010. To be included, the study must have included at least two psychological interventions to treat PTSD and an experimental design in which patients were randomly assigned. The experimental condition a patient was randomized to was considered an ‘intervention’ if a patient received some treatment in the study context beyond a wait list (e.g., referrals to usual care were excluded). Interventions paired with biological agents were excluded. Additionally, patients must have either met diagnostic criteria for PTSD using DSM-III or DSM-IV criteria or scored above traditional clinical cut-offs on standard measures of PTSD symptoms. However, there was not sufficient information across studies to code more specific diagnostic indicators (e.g., chronicity, number of traumatic events). Studies must have contained sufficient statistics to compute dropout rates. We utilized the authors’ definition of dropout, which was typically their report of the number of individuals randomized to a treatment condition that did not complete the full course (regardless of reason). In recent trials, numbers sufficient for dropout rates were reported in Figure 1 (e.g., Schnurr et al., 2007, p.822). However, in older trials it was often not possible to verify how rates were calculated. The first and second authors conducted the literature search, identifying study titles studies that potentially compared two interventions for PTSD. The results of the literature searches were merged in PubMed and the abstracts of studies were obtained and reviewed independently by the first and second authors. The first, second, and third authors independently evaluated full-text articles that appeared relevant to the current meta-analysis to determine if the study was a randomized clinical trial that compared at least two interventions for PTSD.
Figure 1.
Flow chart depicting the identification, retrieval, and selection of studies for the meta-analysis.
Coding of Treatment Descriptions
Control vs. ‘Active’ Treatment
We determined whether a treatment was intended to be an ‘active’ or experimental psychological intervention by asking coders to use the treatment description to determine if the treatment was likely altered or designed as a control to test some aspect of a comparison treatment. Note that coding for control vs. active treatment is problematic in component, parametric, or dismantling studies wherein the amount or presence of a specific treatment component is added or removed and then compared to the original (e.g., PE vs. PE + CR; Foa et al., 2005) – typically in order to test a specific component of the reference treatment. Here an active intervention (e.g., PE) effectively serves as a control for another experimental condition. We excluded studies from control vs. active treatment coding that were purely component, parametric, or dismantling studies (e.g., Cognitive Processing Therapy vs. Cognitive Processing Therapy – Cognitive only vs. Writing Assignment; Resick et al., 2008). Accordingly, treatments tested that exclusively used this design were not included in primary analyses.
Trauma Focus
We divided treatments into 3 categories, including: 1) trauma specific, 2) trauma inclusive/neutral, and 3) trauma avoidant categories. Trauma ‘Specific’ treatments included explicit retellings of the trauma memory (e.g., PE; Foa et al., 1999). Trauma inclusive/neutral treatments did not specify retellings of the trauma memory, but may have allowed discussion of the meaning or memory of the trauma (e.g., Psychodynamic; Brom et al., 1989). Finally, trauma avoidant treatments did not include retelling or focus on the trauma memory or its meaning (e.g., Supportive Counseling; Foa, Rothbaum, Riggs, & Murdock, 1991). Scores ranged from 1 to 3 with higher scores indicating more trauma focus.
Coding Process
Each author coded an initial set of 10 treatment descriptions. We then discussed disagreements and arrived at a consensus for each condition. Second, we trained two doctoral students to serve as blind raters. The blind raters independently evaluated the same 10 treatment descriptions (note that all other details of the study had been removed). In order to establish 100% agreement with the initial coding decisions made by authors, the first author then met with the coders to address errors and to discuss and resolve any disagreements among the raters. Raters then independently coded each treatment condition for degree of trauma focus and active vs. control treatment. Inter-rater agreement was high for the rating of trauma focus (intra class correlation [ICC] = .91, but somewhat lower for coding of control condition ICC=.73. The first author then discussed each disagreement with the raters. All disagreements were resolved after discussion. Note that one additional study was identified after the conclusion of the retrieval and initial coding process (Gilboa-Schechtman et al., 2010) and thus was not included in reliability analyses. The first and second author coded the treatment descriptions. We agreed on both trauma focus and control ratings.
Statistical Analysis
To test Hypothesis 1 in regards to the effect of between study differences in dropout from active treatments, we determined the proportion of patients that dropped out across active interventions in each study. This analysis provided an estimate of the overall dropout rate and its variability across active interventions. We also examined trauma focus, group vs. individual modality, and number of sessions as predictors of differences in dropout (b) across treatments.
As a test of Hypotheses 2, we examined differences in dropout between active treatments that were directly compared in the same study. Instead of deriving a proportional estimate of dropout for each treatment, differences in dropout for each active treatment comparison were calculated as a log odds ratio (LOR) with numbers greater than zero indicating greater odds of a patient dropping out of the reference treatment. Because this analysis contained a variety of treatment types (e.g., EMDR, SIT, Hypnosis, Psychodynamic, Cognitive Restructuring, etc.), the reference treatment is arbitrary. To provide an omnibus test of within study differences in dropout across treatments that were directly compared, we utilized an approach wherein the direction of the effect size was randomly assigned (see Wampold et al., 1997). Randomization forces the average LOR to be close to zero (as necessarily half of the effect sizes will be above zero and half below) and so the test of differences in dropout among active treatments is provided by the test of heterogeneity. A large heterogeneity estimate (I2) would be inconsistent with Hypothesis 2, suggesting there are some active treatments that result in larger dropout rates compared to others. A non-significant heterogeneity estimate would be consistent with Hypothesis 2, suggesting that direct comparisons of treatments consistently result in little difference in dropout. We also included a sensitivity analysis to determine if excluding component studies biased the meta-analysis of active treatments. Specifically, the excluded comparisons were integrated with comparisons of active treatments and we examined heterogeneity in a similar manner.
To determine the effect of differences in trauma focus on dropout from active treatments (Hypothesis 3), we calculated the imbalance in trauma focus among active treatments that were directly compared and entered it as a predictor of the LOR of dropout in a meta-regression. The indicator of imbalance of trauma focus ranged from −2 to 2, wherein a positive score indicated that the first treatment was more trauma focused and a negative score indicated that the second treatment was more trauma focused. A positive relationship between this variable and the odds of dropout would indicate that as the relative trauma focus of the first treatment increased, the odds of dropping out of the first treatment as compared to the second increased. Note that restricting analyses to direct comparisons eliminated most variability in number of sessions and group vs. individual treatment (e.g., most treatments directly compared were of the same length). Accordingly, these variables were not examined as predictors of dropout. Finally, we conducted several additional sensitivity analyses to determine if the omnibus test of trauma focus was missing more subtle differences in dropout. These included direct comparisons of: 1) PE to other treatments, 2) treatments rated as trauma specific to treatments rated as trauma neutral or avoidant, and 3) trauma specific treatments and Present Centered Therapy (PCT) – a treatment originally designed as a control that recently was listed as research supported psychological treatment for PTSD that has ‘strong research support’ (SCP, 2012). PCT was found to be equivalent to established treatments in at least two between group trials (Chambless et. al., 1998). For ease of interpretation we converted certain LOR effect sizes to standard odds-ratios.
We utilized random effects meta-analytic procedures that assume the k comparisons included in the meta-analysis are a random selection of comparisons drawn from the population. Consequently, results from random effects models can be generalized to this hypothetical population rather than limited to the observed studies in the meta-analysis (Cooper, Hedges, & Valentine, 2009). Primary analyses were conducted in ‘R’ (R Core Development Team, 2011) with the meta-analysis package ‘metafor’ (Viechtbauer, 2010).
Note that in small samples it is not uncommon for zero patients to drop out of a given treatment. Accordingly, odds ratios cannot be directly calculated and will have non-positive sampling variances. This is problematic for meta-analytic aggregation procedures as the weight of a study with a non-positive sampling variance is 1/0 (Viechtbauer, 2010). The solution we utilized was to add .5 to all cells in the effect size calculation (Cooper et al., 2009).
Results
Forty-two studies included the direct comparison of at least two interventions. There were 17 comparisons that were coded as comparisons of at least two active treatments – pulled from a total of 54 treatments coded as active interventions. Seventeen treatments were component conditions - e.g. CPT-Cognitive Only vs. CPT and thus were not coded as either active or control. The range of trauma focus was restricted among active interventions; 41 (76%) were coded as trauma specific, 10 (19%) trauma neutral, and only 3 (6%) as trauma ‘avoidant.’ Of the control interventions that were excluded, 0 (0%) were coded as trauma specific, 4 (16%) as trauma neutral, and 21 (84%) as trauma avoidant. The correlation between being rated as a control intervention and greater trauma focus was extremely large (r = 0.81). Across active treatments, the number of sessions ranged from 4 (Neuner et al., 2004) to 30 (Schnurr et al., 2003), M=10.96, SD=5.26. An online appendix provides additional detail on all studies.
The aggregate proportion of dropout across all 54 active treatment arms (1850 patients; M=34.26, median =23.5) was 18.28% (95% CI: 14.84 to 21.75%). Consistent with Hypothesis 1, heterogeneity between active interventions across studies was very large, I2=78.40%, Q(53)= 310.29, p < .0001, suggesting that dropout rates varied quite dramatically across studies. As an additional exploratory test, we eliminated within study variability and then re-examined variability in dropout rates across studies (i.e., the number of completions and dropouts was summed across each active intervention in a study, resulting in a study level dropout rate). There was no reduction in the previous variability estimate, I2=89.40%, Q(35)= 311.76, p < .0001, suggesting that variability in dropout rate across studies is large and within study variability did not contribute to variability estimates. An increase in trauma focus did not predict an increase the dropout rate, b = −0.003 (95% CI: −0.31 to 0.40). However, group treatment was associated with a 12% increase in dropout rate, b = .12, p = .009 (95% CI: 3% to 21%). Number of sessions was also associated with an increase in the dropout rate, b = .01, p = .009 (95% CI: 0.3% to 1.5%), meaning that 1 additional session was associated with an addition of 1 percentage point to the predicted dropout rate.
The rank correlation test (Begg & Mazumdar, 1994) indicated a significant correlation between the proportion of dropout and sampling variance, r = 0.28, p < .003, indicating that smaller studies tended to have a higher proportion of patients dropout of active treatment.
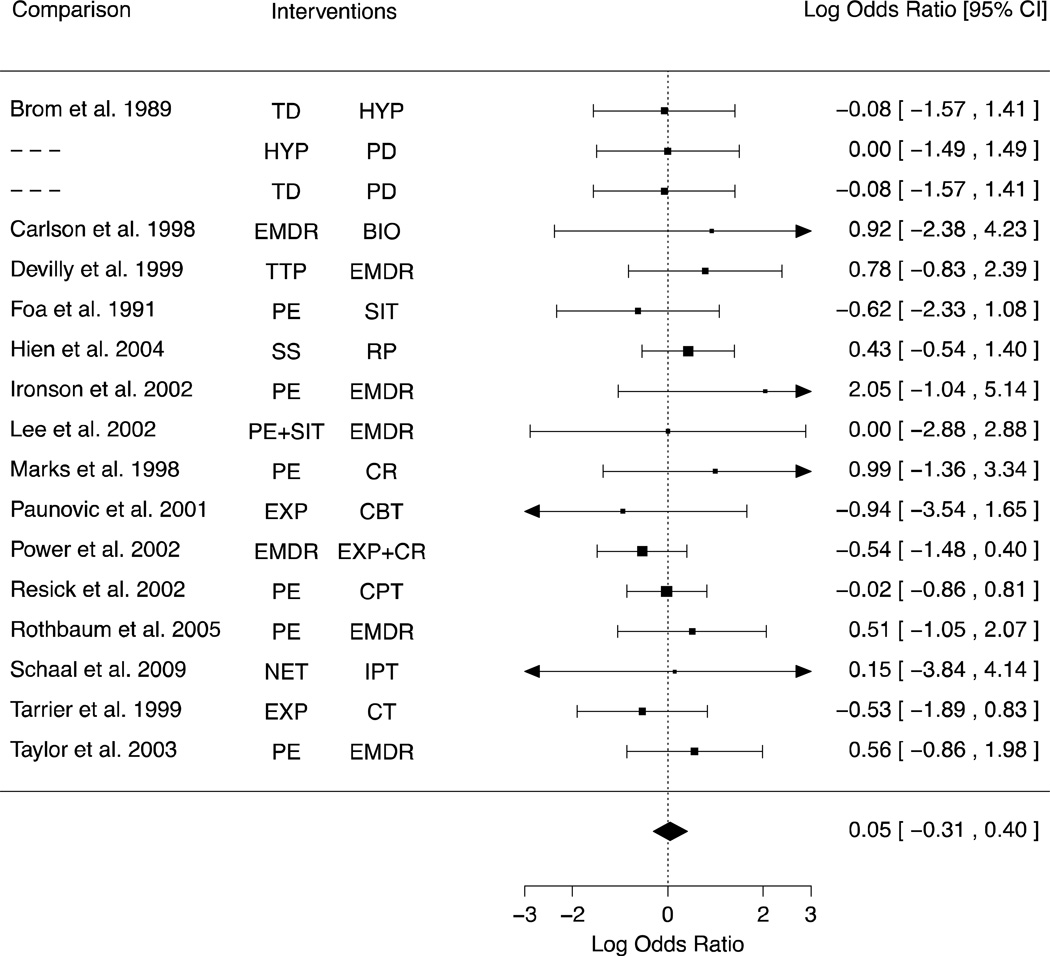
Next we examined the LOR of dropout in the 17 comparisons of active treatments (i.e., a comparison in which neither treatment was coded as a control). We randomly assigned +/- signs to the effect size for each comparison, thus the aggregate odds of dropout across comparisons was close to zero, LOR = .05 (95% CI: −0.31 to 0.40). Consistent with Hypothesis 2, among direct comparisons of active treatments, there was no evidence of variability in the LOR of dropout across studies, I2=0.00%, Q(16)= 8.17, p >.50 (see Figure 2). We also conducted a sensitivity analysis wherein the above model was fit repeatedly with a different effect size removed. This test involved 17 meta-analyses, each one with a different comparison left out of the model (Viechtbauer & Cheung, 2010). Results were consistent with the primary analysis.
Figure 2.
A forest plot depicting variability in the log odds of dropout among comparisons of active treatments. Note that the direction of the LOR is randomly assigned, thus the direction of any given effect size is arbitrary. Note: TD; Trauma Desentiziation, HYP; Hypnotherapy, PD; Brief Psychodynamic Therapy, PE; Prolonged Exposure, CR; Cognitive Restructuring, EMDR; Eye Movement Desensitization and Reprocessing, BIO; Biofeedback, TTP; Cognitive Behavior Trauma Treatment Protocol, SIT; Stress Inoculation Therapy, SS; Seeking Safety, RP; Relapse Prevention, PE+SIT; Prolonged Exposure plus Stress Inoculation Therapy, EXP; Exposure, CBT; Cognitive Behavioral Therapy, EXP+CR; Exposure+Cognitive Restructuring, CPT; Cognitive Processing Therapy, NET; Narrative Exposure Therapy, IPT; Interpersonal Therapy, CT; Cognitive Therapy
We tested the possibility that excluding comparisons of component/dismantling treatments (21 comparisons) from the analysis of active comparisons was responsible for the lack of differences between active treatments. To do so, we combined the component/dismantling comparisons with the set of active treatment comparisons (total of 38 comparisons). The homogeneity estimate was unchanged, I2=0.00%, Q(37)= 36.97, p =.47, indicating that dropout among active treatments was not biased by the exclusion of component/dismantling studies.
Consistent with Hypothesis 3, the effect of differences in trauma focus between comparisons of active treatments was not significant, LOR= 0.21, p = .43 (95% CI: −0.32 to 0.74), indicating that more trauma focused treatments were not associated with an increase in the odds of dropout in the context of comparisons with other active treatments. We conducted additional tests to rule out the potential that this general analysis of trauma focus across active treatments was missing more subtle differences in dropout. First, we examined if the prototypical trauma specific treatment, PE, had higher dropout rates than other active treatments (k=7). Also consistent with Hypothesis 3, there was no difference in LOR of dropout between PE and other active treatments, LOR = −0.05, p >.50 (95% CI: −0.52 to 0.62), I2=0.00%, Q(6)= 3.86, p >.50. A limitation of this finding is that many of the active treatments to which PE was compared were also rated as trauma specific (e.g. EMDR). We also compared active treatments that were rated as trauma specific to those treatments that were rated trauma neutral or avoidant (k=9). Similarly, there was no difference in dropout between trauma specific and trauma neutral or avoidant treatments, LOR = 0.27, p >.50 (95% CI: −0.34 to 0.81), I2=0.00%, Q(8)= 2.46, p >.50.
Finally, we tested the effect of including comparisons of trauma specific treatments and PCT - a trauma avoidant control that was recently labeled a psychological treatment with strong research support - in the original set of 17 active treatment comparisons. We combined the PCT comparisons with the original set of 17 active treatment comparisons (k=20) and examined variability in effects in a manner similar to Hypothesis 2 above. The estimate of between study variability increased, I2=32.34%, Q(19)= 26.81, p =.11, but was not significant. However, because this may indicate that including PCT comparisons (that were all comparisons of trauma specific vs. trauma avoidant treatments) increased variability in dropout among treatments comparisons, we then used meta-regression to examine the effect of differences in trauma focus among this set of 20 comparisons. Inconsistent with Hypothesis 3, the effect of trauma focus was significant, LOR= 0.33, p < .0001 (95% CI: 0.16 to 0.49), indicating that more trauma focused treatments were associated with an increase in the odds of dropout when PCT comparisons were included.
To further explore this finding, we examined the difference in the odds of dropout among the three comparisons of trauma specific interventions and PCT. There was a significant difference in the odds of dropout between trauma specific treatment and PCT, LOR = 0.70, p = .0009, (95% CI: 0.29 to 1.11), I2= 22.15%, Q(2)= 3.54, p = .17. The LOR converts to an odds ratio of 2.02, which suggests trauma specific treatment was associated with a 2-fold increase in the odds of dropout as compared to PCT. Specifically, 36% of patients dropped out of trauma specific treatment as compared to 22% of patients who received PCT – a difference of 14%.
Discussion
The current meta-analysis provides a rigorous test of the relative tendency of patients to dropout of PTSD treatments in clinical trials. There are several methodological contributions. We utilized a coding system that separated active and control treatments, while being sensitive to the range of variability in trauma focus across PTSD treatments (i.e., trauma specific, neutral, and avoidant). In addition, we quantified the amount of between study variability in dropout and then restricted the examination of treatment differences to direct comparisons of active PTSD treatments – removing any bias contributed by between study differences. Finally, in contrast to previous meta-analyses, our approach was sensitive to potential differences in dropout both within and between treatment categories.
There was a large amount of variability in dropout among active interventions across studies. In addition, several study level variables, including group modality and number of sessions were associated with dropout. However, restricting the analysis of dropout to direct comparisons of active interventions reduced variability between studies to zero. Consistent with general claims from previous meta-analyses (Bisson et al., 2007; Hembree et al., 2003; Swift & Greenberg, 2012), there was no evidence of differences in dropout between these active treatments.
Findings in regards to the effect of trauma focus were mixed. Differences in trauma focus did not predict dropout across studies or between direct comparisons. There were also no differences in dropout in direct comparisons of PE to other active interventions as well as the more general comparison of treatments that were rated as trauma specific to those that were not. However, there were only 3 ‘trauma avoidant’ treatments in the 17 comparisons of active interventions. It appears the de facto way to design a control intervention in PTSD intervention research is to remove discussion of the trauma memory. As many cognitive behavioral therapies focus on emotional processing through exposure to the trauma memory as a primary therapeutic ingredient, this is not surprising. However, one possibility is that the restriction of range in trauma focus among active treatments may obscure a real effect of trauma focus on dropout. Consistent with this idea, comparisons of PCT (a trauma avoidant control) and trauma specific treatments appear to be an exception to the pattern of no effect of trauma focus on dropout. There was evidence across 3 relatively large trials (795 patients) that dropout is lower in PCT compared to trauma specific treatments. This evidence stands in contrast to prior meta-analyses that provided little evidence of differences in dropout between trauma and non-trauma focused treatments (e.g., Bisson et al., 2007; Hembree et al. 2003).
Limitations
There are several limitations of this meta-analysis. First, while group modality and number of sessions predicted dropout across studies, a lack of within study comparisons that varied on these parameters (e.g., group vs. individual in the same study) mean these results could not be tested in the meta-analysis of direct comparisons. Second, the clinical meaning of ‘dropout’ in clinical trials is not clear. It is possible that some patients who do not complete treatment have outcomes that are comparable to those who do. There is evidence that much of the improvement in psychotherapy happens early in treatment. For example, patients who receive the fewest sessions of psychotherapy in community settings often improve the most (Baldwin, Berkeljon, Atkins, Olsen, & Nielsen, 2009). In this sense, some dropouts may actually be better characterized as early completers. Specific groups of PTSD patients (e.g., patients with one recent focal trauma vs. prolonged and repeated traumatic experiences) who ‘dropout’ of PTSD treatment may contain as many successes as failures. This apples and oranges problem may obscure potential differences between treatments. Outcome studies should consider reporting both the number of patients that did not complete the full course of treatment as well as their symptom severity at termination (Hembree et al., 2003).
Perhaps most important, conclusions regarding dropout among active interventions should be restricted to the types of interventions included in the meta-analysis (primarily trauma specific and neutral). There was some diversity among active interventions that were directly compared in this meta-analysis, but comparisons were primarily of trauma specific and neutral (repeated discussions of the trauma memory are not required, but may be allowed). Increasing the number of trials with emerging therapies for PTSD (Schnyder, 2005) that do not include a focus on the trauma memory such as IPT (Markowitz, 2010; Rafaeli & Markowitz, 2011), Behavioral Activation (Jakupcak et al., 2006), Acceptance and Commitment Therapy (ACT) and mindfulness based approaches (Walser & Westrup, 2007), and now PCT, may provide a more thorough test of whether treatments with varying degree of focus on trauma differ in their ability to retain patients.
A final factor that is germane to the issue of dropout that has not yet been incorporated into PTSD trials or meta-analytic work is the importance of the therapist providing the treatment. There is initial evidence that therapists differ in the rate that patients drop out of treatment (Owen, Imel, & Adelson, 2012). A failure to model potential therapist differences in dropout may bias traditional statistical tests used to make treatment comparisons and inflate the size of effects attributed to treatments (Kenny & Judd, 1986; Wampold & Serlin, 2000). As therapist differences were not modeled in any of the trials included in this (or any other) meta-analysis, it is possible that results represent an over-estimate of the true differences in dropout between treatments. A direction for future research would be to investigate therapists as a source of dropout and also the characteristics of those therapists who routinely retain patients in treatment.
Clinical Implications
Many have been concerned that exposure based therapies can lead to symptom exacerbation and result in dropout (Yehuda, 2000). Our findings suggest that dropout is not significantly different among ‘active’ treatments. Accordingly if administrators or clinicians are choosing among a menu of these treatment options, which primarily include trauma specific and neutral interventions, there is no compelling reason to expect any active treatment will enhance retention as compared to any other.
The implications of lower rates of dropout from PCT as compared to trauma specific active treatments are more complex. This finding could be dismissed because PCT was designed as a control treatment. The comparability of an active treatment that demands the commitment and involvement of the patient with a ‘sham’ that was designed to prevent overlap with a comparison is subject to numerous confounds. In addition, therapists would seem unlikely to offer a control intervention wherein they are prevented from ever asking about the traumatic event and re-direct the patient to other topics if the patient initiates such a discussion. Similarly, administrators would not likely be interested in the dissemination of a control treatment. However, PCT appears to differ from other psychological controls in important ways. Many psychological controls contain little beyond active listening and the proscription of specific therapist activities (Mohr et al., 2009). PCT is more developed, including a cogent rationale, training, treatments manuals, and explicit psychological bases of the treatment (e.g., McDonagh et al., 2005). Moreover, PCT was of comparable efficacy to established treatments in three clinical trials such that it was recently included in a list of empirically supported treatments for PTSD (SCP, 2012).
Despite the advantage of PCT, the effect is dwarfed by problems with retention in “real world” studies of treatment utilization. Only 56% of PTSD patients who received some treatment in the community received a minimally adequate dose of psychotherapy (defined as at least 8 sessions of 30 minutes in length; Wang, Lane, Olfson, Pincus, Wells, & Kessler, 2005). Accordingly, the dropout rate of 18% in clinical trials would represent a massive improvement. Thus, the most promising method for improving retention in the community is not likely tied to a specific treatment approach, but may involve systemic and logistical changes. Thus, retention might be improved by focusing on disseminating the ‘machinery’ of clinical trial management that can be replicated so that community settings can approach the ability of clinical trials to retain patients. This might include therapist training, support, and supervision, patient screening, regular assessment, and ongoing contact with assistants that may promote session attendance.
In conclusion, dropout rates varied widely across studies, suggesting that attempts to compare the dropout rates of active interventions across studies should be interpreted with caution. It is more appropriate to interpret a dropout rate as an indicator of something about the study itself rather than an indication of a given treatment’s tolerability. Meta-analytic conclusions about specific PTSD treatments should be restricted to treatments compared in the same study, which control for study level confounds. Here evidence regarding dropout among active treatments mirrors the comparative efficacy of active treatments (Benish et al., 2008; Powers et al., 2010) - there is little evidence that some active treatments result in higher dropout rates as compared to other treatments. However, PCT may be an exception to this general pattern of no differences among active treatments, perhaps due to a restriction of range in trauma focus among evaluated treatments. If future research replicates this pattern of comparative efficacy and a lower rate of dropout relative to other treatment modalities, it would seem appropriate to consider PCT as a first line treatment – especially for patients who do not prefer a trauma focused treatment.
Supplementary Material
Acknowledgements
Portions of the manuscript were supported by the University of Washington Institute of Translational Health Science funded by grant UL1RR025014 from the NIH National Center for Research Resources. We would also like to thank both the VA Puget Sound Health Care System for their generous support of the investigators. Writing of this manuscript was also partially supported by the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research, Education and Clinical Center (MIRECC), Department of Veterans Affairs.
References
- *.Arntz A, Tiesema M, Kindt M. Treatment of PTSD: A comparison of imaginal exposure with and without imagery rescripting. Journal of Behavior Therapy and Experimental Psychiatry. 2007;38(4):345–370. doi: 10.1016/j.jbtep.2007.10.006. [DOI] [PubMed] [Google Scholar]
- Baldwin SA, Berkeljon A, Atkins DC, Olsen JA, Nielsen SL. Rates of change in naturalistic psychotherapy: Contrasting dose–effect and good-enough level models of change. Journal of Consulting and Clinical Psychology. 2009;77(2):203–211. doi: 10.1037/a0015235. [DOI] [PubMed] [Google Scholar]
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101. [PubMed] [Google Scholar]
- Benish SG, Imel ZE, Wampold BE. The relative efficacy of bona fide psychotherapies for treating post-traumatic stress disorder: A meta-analysis of direct comparisons. Clinical Psychology Review. 2008;28(5):746–758. doi: 10.1016/j.cpr.2007.10.005. [DOI] [PubMed] [Google Scholar]
- *.Bichescu D, Neuner F, Schauer M, Elbert T. Narrative exposure therapy for political imprisonment-related chronic posttraumatic stress disorder and depression. Behaviour Research and Therapy. 2007;45(9):2212–2220. doi: 10.1016/j.brat.2006.12.006. [DOI] [PubMed] [Google Scholar]
- Bisson JI, Ehlers A, Matthews R, Pilling S, Richards D, Turner S. Psychological treatments for chronic post-traumatic stress disorder: Systematic review and meta-analysis. The British Journal of Psychiatry. 2007;190(2):97–104. doi: 10.1192/bjp.bp.106.021402. [DOI] [PubMed] [Google Scholar]
- *.Blanchard EB, Hickling EJ, Devineni T, Veazey CH, Galovski TE, Mundy E, Malta LS, et al. A controlled evaluation of cognitive behaviorial therapy for posttraumatic stress in motor vehicle accident survivors. Behaviour Research and Therapy. 2003;41:79–96. doi: 10.1016/s0005-7967(01)00131-0. [DOI] [PubMed] [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry. 2005;162(2):214–227. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- *.Brom D, Kleber RJ, Defares PB. Brief psychotherapy for posttraumatic stress disorders. Journal of Consulting and Clinical Psychology. 1989;57(5):607–612. doi: 10.1037//0022-006x.57.5.607. [DOI] [PubMed] [Google Scholar]
- *.Bryant RA, Moulds ML, Guthrie RM, Dang ST, Nixon RDV. Imaginal exposure alone and imaginal exposure with cognitive restructuring in treatment of posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2003;71:706–712. doi: 10.1037/0022-006x.71.4.706. [DOI] [PubMed] [Google Scholar]
- *.Bryant RA, Moulds ML, Guthrie RM, Dang ST, Mastrodomenico J, Nixon RDV, Felmingham KL, Hopwood S, et al. A randomized controlled trial of exposure therapy and cognitive restructuring for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2008;76(4):695–703. doi: 10.1037/a0012616. [DOI] [PubMed] [Google Scholar]
- *.Carlson JG, Chemtob CM, Rusnak K, Hedlund NL, Muraoka MY. Eye movement desensitization and reprocessing (EDMR) treatment for combat-related posttraumatic stress disorder. Journal of Traumatic Stress. 1998;11(1):3–24. doi: 10.1023/A:1024448814268. [DOI] [PubMed] [Google Scholar]
- *.Catani C, Kohiladevy M, Ruf M, Schauer E, Elbert T, Neuner F. Treating children traumatized by war and Tsunami: A comparison between exposure therapy and meditation-relaxation in North-East Sri Lanka. BMC Psychiatry. 2009;9(1):9–22. doi: 10.1186/1471-244X-9-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambless DL, Baker MJ, Baucom DH, Beutler LE, Calhoun KS, Crits-Christoph P, Woody SR. Update on empirically validated therapies, II. The Clinical Psychologist. 1998;51(1):3–16. [Google Scholar]
- *.Chard KM. An evaluation of cognitive processing therapy for the treatment of posttraumatic stress disorder related to childhood sexual abuse. Journal of Consulting and Clinical Psychology. 2005;73(5):965–971. doi: 10.1037/0022-006X.73.5.965. [DOI] [PubMed] [Google Scholar]
- *.Cloitre M, Stovall-McClough KC, Nooner K, Zorbas P, Cherry S, Jackson CL, Gan W, et al. Treatment for PTSD related to childhood abuse: A randomized controlled trial. American Journal of Psychiatry. 2010;167(8):915–924. doi: 10.1176/appi.ajp.2010.09081247. [DOI] [PubMed] [Google Scholar]
- *.Cook JM, Harb GC, Gehrman PR, Cary MS, Gamble GM, Forbes D, Ross RJ. Imagery rehearsal for posttraumatic nightmares: A randomized controlled trial. Journal of Traumatic Stress. 2010;23(5):553–563. doi: 10.1002/jts.20569. [DOI] [PubMed] [Google Scholar]
- Cooper H, Hedges LV, Valentine JC. The Handbook of Research Synthesis and Meta-Analysis. 2nd ed. New York: Russell Sage; 2009. [Google Scholar]
- *.Cottraux J, Note I, Yao SN, de Mey Guillard C, Bonasse FCO, Djamoussian D, Mollard E, et al. Randomized controlled comparison of cognitive behavior therapy with rogerian supportive therapy in chronic post-traumatic stress disorder: A 2-year follow-up. Psychotherapy and Psychosomatics. 2008;77(2):101–110. doi: 10.1159/000112887. [DOI] [PubMed] [Google Scholar]
- *.Devilly GJ, Spence SH. The relative efficacy and treatment distress of EMDR and a cognitive-behavior trauma treatment protocol in the amelioration of posttraumatic stress disorder. Journal of Anxiety Disorders. 1999;13(1–2):131–157. doi: 10.1016/s0887-6185(98)00044-9. [DOI] [PubMed] [Google Scholar]
- *.Dunn NJ, Rehm LP, Schillaci J, Souchek J, Mehta P, Ashton CM, Yanasak E, et al. A randomized trial of self-management and psychoeducational group therapies for comorbid chronic posttraumatic stress disorder and depressive disorder. Journal of Traumatic Stress. 2007;20(3):221–237. doi: 10.1002/jts.20214. [DOI] [PubMed] [Google Scholar]
- *.Echeburua E, De Corral P, Zubizarreta I, Sarasua B. Psychological treatment of chronic posttraumatic stress disorder in victims of sexual aggression. Behavior Modification. 1997;21(4):433–456. doi: 10.1177/01454455970214003. [DOI] [PubMed] [Google Scholar]
- *.Ehlers A, Clark DM, Hackmann A, McManus F, Fennell M, Herbert C, Mayou R. A randomized controlled trial of cognitive therapy, a self-help booklet, and repeated assessments as early interventions for posttraumatic stress disorder. Archives of General Psychiatry. 2003;60(10):1024–1032. doi: 10.1001/archpsyc.60.10.1024. [DOI] [PubMed] [Google Scholar]
- *.Feske U. Treating Low-Income and Minority Women With Posttraumatic Stress Disorder: A Pilot Study Comparing Prolonged Exposure and Treatment as Usual Conducted by Community Therapists. Journal of Interpersonal Violence. 2008;23(8):1027–1040. doi: 10.1177/0886260507313967. [DOI] [PubMed] [Google Scholar]
- *.Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, Street GP. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology. 1999;67(2):194–200. doi: 10.1037//0022-006x.67.2.194. [DOI] [PubMed] [Google Scholar]
- *.Foa EB, Hembree EA, Cahill SP, Rauch SAM, Riggs DS, Feeny NC, Yadin E. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005;73(5):953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- Foa EB, Keane TM, Friedman MJ. Effective Treatments for PTSD. New York: Guilford; 2010. Practice Guidelines from the International Society for Traumatic Stress Studies. [Google Scholar]
- *.Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology. 1991;59(5):715–723. doi: 10.1037//0022-006x.59.5.715. [DOI] [PubMed] [Google Scholar]
- Foa EB, Zoellner LA, Feeny NC, Hembree EA, Alvarez-Conrad J. Does imaginal exposure exacerbate PTSD symptoms? Journal of Consulting and Clinical Psychology. 2002;70(4):1022–1028. doi: 10.1037//0022-006x.70.4.1022. [DOI] [PubMed] [Google Scholar]
- *.Gilboa-Schechtman E, Foa EB, Shafran N, Aderka IM, Powers MB, Rachamim L, Rosenbach L, et al. Prolonged Exposure Versus Dynamic Therapy for Adolescent PTSD: A Pilot Randomized Controlled Trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(10):1034–1042. doi: 10.1016/j.jaac.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Glynn SM, Eth S, Randolph ET, Foy DW, Urbaitis M, Boxer L, Paz GG, et al. A test of behavioral family therapy to augment exposure for combat-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1999;67:243–251. doi: 10.1037//0022-006x.67.2.243. [DOI] [PubMed] [Google Scholar]
- *.Hien DA, Cohen LR, Miele GM, Litt LC, Capstick C. Promising treatments for women with comorbid PTSD and substance use disorders. American Journal of Psychiatry. 2004;161(8):1426–1432. doi: 10.1176/appi.ajp.161.8.1426. [DOI] [PubMed] [Google Scholar]
- *.Hien DA, Wells EA, Jiang H, Suarez-Morales L, Campbell ANC, Cohen LR, Miele GM, et al. Multisite randomized trial of behavioral interventions for women with co-occurring PTSD and substance use disorders. Journal of Consulting and Clinical Psychology. 2009;77(4):607–619. doi: 10.1037/a0016227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hembree EA, Foa EB, Dorfan NM, Street GP, Kowalski J, Tu X. Do patients drop out prematurely from exposure therapy for PTSD? Journal of Traumatic Stress. 2003;16(6):555–562. doi: 10.1023/B:JOTS.0000004078.93012.7d. [DOI] [PubMed] [Google Scholar]
- *.Ironson G, Freund B, Strauss J, Williams J. Comparison of two treatments for traumatic stress: A community-based study of EMDR and prolonged exposure. Journal of Clinical Psychology. 2002;58(1):113–128. doi: 10.1002/jclp.1132. [DOI] [PubMed] [Google Scholar]
- Jakupcak M, Roberts LJ, Martell C, Mulick P, Michael S, Reed R, Balsam KF, et al. A pilot study of behavioral activation for veterans with posttraumatic stress disorder. Journal of Traumatic Stress. 2006;19(3):387–391. doi: 10.1002/jts.20125. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Judd CM. Consequences of violating the independence assumption in analysis of variance. Psychological Bulletin. 1986;99:422–431. [Google Scholar]
- *.Lee C, Gavriel H, Drummond P, Richards J, Greenwald R. Treatment of PTSD: Stress inoculation training with prolonged exposure compared to EMDR. Journal of Clinical Psychology. 2002;58(9):1071–1089. doi: 10.1002/jclp.10039. [DOI] [PubMed] [Google Scholar]
- *.Litz B, Engel C, Bryant R, Papa A. A randomized, controlled proof-of-concept trial of an Internet-based, therapist-assisted self-management treatment for posttraumatic stress disorder. American Journal of Psychiatry. 2007;164(11):1676–1684. doi: 10.1176/appi.ajp.2007.06122057. [DOI] [PubMed] [Google Scholar]
- Markowitz JC. IPT and PTSD. Depression and Anxiety. 2010;27(10):879–881. doi: 10.1002/da.20752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Marks I, Lovell K, Noshirvani H, Livanou M, Thrasher S. Treatment of posttraumatic stress disorder by exposure and/or cognitive restructuring: a controlled study. Archives of General Psychiatry. 1998;55(4):317–325. doi: 10.1001/archpsyc.55.4.317. [DOI] [PubMed] [Google Scholar]
- *.McDonagh A, Friedman M, McHugo G, Ford J, Sengupta A, Mueser K, Demment CC, et al. Randomized Trial of Cognitive-Behavioral Therapy for Chronic Posttraumatic Stress Disorder in Adult Female Survivors of Childhood Sexual Abuse. Journal of Consulting and Clinical Psychology. 2005;73(3):515–524. doi: 10.1037/0022-006X.73.3.515. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Journal of Clinical Epidemiology. 2009;62(10):1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Spring B, Freedland KE, Beckner V, Arean P, Hollon SD, Ockene J, et al. The selection and design of control conditions for randomized controlled trials of psychological interventions. Psychotherapy and Psychosomatics. 2009;78(5):275–284. doi: 10.1159/000228248. [DOI] [PubMed] [Google Scholar]
- National Collaborating Centre for Mental Health. Post-traumatic stress disorder (PTSD): The management of PTSD in adults and children in primary and secondary care. National Institute for Clinical Excellence. 2005:1–176. [Google Scholar]
- *.Neuner F, Onyut PL, Ertl V, Odenwald M, Schauer E, Elbert T. Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2008;76(4):686–694. doi: 10.1037/0022-006X.76.4.686. [DOI] [PubMed] [Google Scholar]
- *.Neuner F, Schauer M, Klaschik C, Karunakara U, Elbert T. A comparison of narrative exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress disorder in an African refugee settlement. Journal of Consulting and Clinical Psychology. 2004;72(4):579–587. doi: 10.1037/0022-006X.72.4.579. [DOI] [PubMed] [Google Scholar]
- Owen J, Imel Z, Adelson J. “No-Show”: Therapist Racial/Ethnic Disparities in Client Unilateral Termination. Journal of Counseling Psychology. 2012;59:314–320. doi: 10.1037/a0027091. [DOI] [PubMed] [Google Scholar]
- *.Paunovic N, Öst LG. Cognitive-behavior therapy vs exposure therapy in the treatment of PTSD in refugees. Behaviour Research and Therapy. 2001;39(10):1183–1197. doi: 10.1016/s0005-7967(00)00093-0. [DOI] [PubMed] [Google Scholar]
- *.Power K, McGoldrick T, Brown K, Buchanan R, Sharp D, Swanson V, Karatzias A. A controlled comparison of eye movement desensitization and reprocessing versus exposure plus cognitive restructuring versus waiting list in the treatment of post-traumatic stress disorder. Clinical Psychology & Psychotherapy. 2002;9(5):299–318. [Google Scholar]
- Powers MB, Halpern JM, Ferenschak MP, Gillihan SJ, Foa EB. A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review. 2010;30(6):635–641. doi: 10.1016/j.cpr.2010.04.007. [DOI] [PubMed] [Google Scholar]
- Rafaeli AK, Markowitz JC. Interpersonal Psychotherapy (IPT) for PTSD: A case study. American Journal of Psychotherapy. 2011;65(3):205–223. doi: 10.1176/appi.psychotherapy.2011.65.3.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Resick PA, Galovski TE, Uhlmansiek MO, Scher CD, Clum GA, Young-Xu Y. A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting and Clinical Psychology. 2008;76(2):243–258. doi: 10.1037/0022-006X.76.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen CS, Chow HC, Finney JF, Greenbaum MA, Moos RH, Sheikh JI, Yesavage JA. VA practice patterns and practice guidelines for treating posttraumatic stress disorder. Journal of Traumatic Stress. 2004;17(3):213–222. doi: 10.1023/B:JOTS.0000029264.23878.53. [DOI] [PubMed] [Google Scholar]
- *.Rothbaum BO, Astin MC, Marsteller F. Prolonged exposure versus eye movement desensitization and reprocessing (EMDR) for PTSD rape victims. Journal of Traumatic Stress. 2005;18(6):607–616. doi: 10.1002/jts.20069. [DOI] [PubMed] [Google Scholar]
- *.Schaal S, Elbert T, Neuner F. Narrative exposure therapy versus interpersonal psychotherapy. Psychotherapy and Psychosomatics. 2009;78(5):298–306. doi: 10.1159/000229768. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Lavori PW, Hsieh FY. Design of VA Cooperative Study #420: Group treatment of PTSD. Controlled Clinical Trials. 2001;22:74–88. doi: 10.1016/s0197-2456(00)00118-5. [DOI] [PubMed] [Google Scholar]
- *.Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, Resick PA, et al. Cognitive behavioral therapy for posttraumatic stress disorder in women. Journal of the American Medical Association. 2007;297(8):820–830. doi: 10.1001/jama.297.8.820. [DOI] [PubMed] [Google Scholar]
- *.Schnurr PP, Friedman MJ, Foy DW, Shea MT, Hsieh FY, Lavori PW, Glynn SM, et al. Randomized trial of trauma-focused group therapy for posttraumatic stress disorder: Results from a Department of Veterans Affairs cooperative study. Archives of general psychiatry. 2003;60(5):481–489. doi: 10.1001/archpsyc.60.5.481. [DOI] [PubMed] [Google Scholar]
- Schnyder U. Why New Psychotherapies for Posttraumatic Stress Disorder? Psychotherapy and Psychosomatics. 2005;74(4):199–201. doi: 10.1159/000085142. [DOI] [PubMed] [Google Scholar]
- Shadish WR, Sweeney RB. Mediators and moderators in meta-analysis: There’s a reason we don’t let dodo birds tell us which psychotherapies should have prizes. Journal of Consulting and Clinical Psychology. 1991;59(6):883–893. doi: 10.1037//0022-006x.59.6.883. [DOI] [PubMed] [Google Scholar]
- Society of Clinical Psychology (SCP): American Psychological Association, Division 12. Present-Centered Therapy for Post-Traumatic Stress Disorder. 2012 Retrieved from http://www.div12.org/PsychologicalTreatments/treatments/ptsd_present.html.
- Speckens AEM, Ehlers A, Hackmann A, Clark DM. Changes in intrusive memories associated with imaginal reliving in posttraumatic stress disorder. Journal of Anxiety Disorders. 2006;20(3):328–341. doi: 10.1016/j.janxdis.2005.02.004. [DOI] [PubMed] [Google Scholar]
- Swift JK, Greenberg RP. Premature discontinuation in adult psychotherapy: A Meta-Analysis. Journal of Consulting and Clinical Psychology. 2012;80:547–559. doi: 10.1037/a0028226. [DOI] [PubMed] [Google Scholar]
- *.Tarrier N, Pilgrim H, Sommerfield C, Faragher B, Reynolds M, Graham E, Barrowclough C. A randomized trial of cognitive therapy and imaginal exposure in the treatment of chronic posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1999;67(1):13–18. doi: 10.1037//0022-006x.67.1.13. [DOI] [PubMed] [Google Scholar]
- *.Taylor S, Thordarson DS, Maxfield L, Fedoroff IC, Lovell K, Ogrodniczuk J. Comparative efficacy, speed, and adverse effects of three PTSD treatments: Exposure therapy, EMDR, and relaxation training. Journal of Consulting and Clinical Psychology. 2003;71(2):330–338. doi: 10.1037/0022-006x.71.2.330. [DOI] [PubMed] [Google Scholar]
- R Core Development Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2011. ISBN 3-900051-07-0. [Google Scholar]
- Viechtbauer W. Conducting meta-analyses in R with the metafor package. Journal of Statistical Software. 2010;36(3):1–49. [Google Scholar]
- Viechtbauer W, Cheung MWL. Outlier and influence diagnostics for meta-analysis. Research Synthesis Methods. 2010;1(2):112–125. doi: 10.1002/jrsm.11. [DOI] [PubMed] [Google Scholar]
- Walser RD, Westrup D. Acceptance and Commitment Therapy for the Treatment of Post-Traumatic Stress Disorder and Trauma-Related Problems. New Harbinger Incorporated; 2007. A Practitioner's Guide to Using Mindfulness and Acceptance Strategies; p. 272. [Google Scholar]
- Wampold BE, Mondin GW, Moody M, Stich F, Benson K, Ahn H. A meta-analysis of outcome studies comparing bona fide psychotherapies: Empiricially, “all must have prizes.”. Psychological Bulletin. 1997;122(3):203–215. [Google Scholar]
- Wampold BE, Serlin RC. The consequence of ignoring a nested factor on measures of effect size in analysis of variance. Psychological Methods. 2000;5:425–433. doi: 10.1037/1082-989x.5.4.425. [DOI] [PubMed] [Google Scholar]
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Archives of general psychiatry. 2005;62(6):629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- Yehuda R. Clinical treatment of posttraumatic stress disorder: Conceptual challenges raised by recent research. Australian and New Zealand Journal of Psychiatry. 2000;34:940–953. doi: 10.1080/000486700268. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.