Abstract
Objective:
Individuals with attention-deficit/hyperactivity disorder (ADHD) are at increased risk for experiencing alcohol-related problems. However, previous research has not examined alcohol expectancies, a widely studied risk factor for alcohol use, in this population. The current study examined mean differences in alcohol expectancies for adolescents with and without a history of childhood ADHD. The differential association between alcohol expectancies and alcohol use 1 year later as a function of ADHD status was also examined.
Method:
Two hundred and eighty-six adolescents ages 11–17 (ADHD: n = 165; non-ADHD: n = 121) reported their alcohol expectancies and alcohol use over a 1-year period as part of the Pittsburgh ADHD Longitudinal Study.
Results:
Individuals with a history of ADHD had lower mean levels of alcohol expectancies compared with individuals without ADHD. Specifically, at Time 1, individuals with ADHD reported lower levels of sociability, cognitive and behavioral impairment, and liquid courage expectancies than individuals without ADHD. Further, the association between negative alcohol expectancies at Time 1 and alcohol use at Time 2 differed for individuals with and without a history of ADHD.
Conclusions:
These findings highlight the possibility that individuals with a history of ADHD may rely less on explicit cognitions, such as alcohol expectancies, when making decisions to drink alcohol. This is consistent with the dual process model of alcohol cognitions that has posited that individuals with decreased executive control may rely more on implicit cognitions about alcohol.
Adolescent alcohol use is a significant health concern and is related to a variety of negative outcomes in adulthood. For example, higher levels of adolescent alcohol use are related to alcohol-related problems, aggression, theft, and suicidal ideation in young adulthood (Duncan et al., 1997). National data also highlight that alcohol use increases over the course of adolescence. Approximately 27% of 8th graders, 50% of 10th graders, and 64% of high school seniors report alcohol use in the past year. Further, a significant portion of adolescents also report drinking to the point of being drunk in the past year, and this increases with age (11% of 8th graders, 29% of 10th graders, and 42% of 12th graders; Johnston et al., 2012). Studying predictors of early alcohol use is important, given the riskiness of this behavior for both short- and long-term outcomes. In addition, examining predictors of alcohol use at a young age, when alcohol use is nascent, helps identify variables that may play an important role in drinking escalation in adolescence.
Attention-deficit/hyperactivity disorder and adolescent alcohol use
Adolescents with attention-deficit/hyperactivity disorder (ADHD) may be at increased risk for experiencing alcohol-related problems compared with individuals without ADHD. A recent meta-analytic study showed that, although childhood ADHD is not associated with higher rates of alcohol use in adolescence, it is associated with increased risk of alcohol use disorder by adulthood (Lee et al., 2011). Thus, aspects of alcohol use in this population are clearly building through adolescence to heighten the risk of problem drinking by adulthood. For example, when frequency measures of drinking are considered in adolescence (beyond just use/nonuse as reflected in the studies considered by Lee et al., 2011), group differences emerge by late adolescence (Molina et al., 2003, 2007). Similarly, in a large multisite sample of children with ADHD, repeated drinking or drunkenness in adolescence was elevated for the ADHD compared with the non-ADHD group (Molina et al., 2013). Thus, beginning in adolescence, there is an emerging vulnerability to later problematic alcohol use that warrants further research.
Despite this increase in risk, very few studies have examined potential differential associations between predictors of alcohol use and drinking behavior for individuals with ADHD compared with individuals without ADHD. However, there is some evidence for certain environmental predictors, such as parenting factors (Walther et al., 2012) and peer use (Marshal et al., 2003), to be more strongly associated with alcohol use for individuals with ADHD compared with individuals without ADHD. Although environmental factors may be more strongly related to alcohol use for individuals with ADHD, the reverse may be true for certain individual factors. Although not yet directly studied, it may be that certain individual differences, particularly ones that rely on higher order cognitive processes such as planful decision making, may be less associated with drinking for individuals with ADHD given the high levels of impulsivity and inattention that characterize this population. To consider this possibility, the current study focused on one widely studied individual cognitive risk factor for alcohol use: alcohol expectancies.
Alcohol expectancies
Alcohol expectancies are widely studied predictors of alcohol use. They develop before the onset of drinking (Dunn and Goldman, 2000; Miller et al., 1990) and predict drinking onset and escalation of use in adolescents (e.g., Goldman, 1994). Alcohol expectancies have been found to be positive or negative, with positive alcohol expectancies increasing and negative expectancies decreasing across adolescence (Dunn and Goldman, 1998, 2000). Recent work has also highlighted the possibility that, compared with younger children, older children hold more expectancies about alcohol: positive and negative (Bekman et al., 2011). Very limited research has examined if there are mean level differences in alcohol expectancies for individuals with ADHD or how expectancies relate to drinking behavior for this population. A recent study (Dattilo et al., 2013) examined the association between ADHD symptoms and positive alcohol expectancies in young adults. Dattilo and colleagues found that ADHD symptoms were related to higher levels of positive expectancies, and these expectancies were more related to alcohol problems for individuals with more ADHD symptoms. However, this research was conducted within a college sample with low levels of ADHD symptoms (3.3% of the sample met the diagnostic criteria for ADHD), and assessments were conducted in adulthood as opposed to childhood. Therefore, individual differences in the sample may actually represent a moderate range of adult impulsivity levels as opposed to clinically significant symptom levels. Research with samples in which more individuals meet diagnostic ADHD thresholds and who were assessed in childhood through multiple informant reporters is needed to further increase our understanding of the association between ADHD and alcohol expectancies.
Dual process model of alcohol cognitions
Stacy and Wiers (2010) proposed a dual process model of alcohol use that identifies two cognitive systems that process information: a rational, explicit process and one that relies on automatic, implicit processes. This model highlights the possibility that explicit or implicit alcohol cognitions may be more or less related to drinking behavior for certain individuals. As such, individuals demonstrating relatively high levels of executive functioning (planning, organization, response inhibition, sustained attention, set shifting, working memory, and reasoning) would rely more on the controlled explicit process, whereas individuals low in executive functioning would rely more on the automatic, implicit process. In line with this, explicit expectancies have been shown to be less related to alcohol use for adolescents with low working memory capacity compared to adolescents with high working memory capacity. In addition, implicit cognitions were found to be more related to alcohol for the individuals with low working memory (Thush et al., 2008). Individuals high in positive and negative urgency, facets of impulsivity, have also been found to act more in line with their implicit alcohol cognitions than individuals with lower levels of these traits (Burton et al., 2012). Research has shown that explicit expectancies and alcohol use reciprocally influence one another (e.g., Smith et al., 1995). However, because this association is potentially reduced for individuals with lower executive control, expectancy development may be attenuated in ADHD and result in lower mean levels of explicit alcohol expectancies. Deficits in executive functions have been demonstrated in a number of studies examining individuals with ADHD (for review, see Seidman, 2006). Such deficits, in combination with the high levels of impulsivity characteristic of individuals with ADHD, suggest that explicit expectancies may be less related to alcohol use for this population than for individuals without ADHD. Further, these deficits combined with attentional difficulties may also result in slower development of alcohol expectancies in adolescence. The current study examined this possibility in a sample of adolescents with and without a childhood diagnosis of ADHD.
Study aims
Previous research has not examined if alcohol expectancies differ in mean level or in association with alcohol use for individuals with and without a diagnosis of childhood ADHD. The current study used data from the Pittsburgh ADHD Longitudinal Study (PALS; Molina et al., 2007), a follow-up study of children with ADHD and demographically similar individuals without ADHD, to examine if individuals with and without ADHD histories had different mean levels of positive and negative expectancies in adolescence. First, we hypothesized that individuals with a history of ADHD would hold lower levels of positive and negative expectancies compared with individuals without ADHD. Second, we examined if the association between alcohol expectancies (Time 1) and alcohol use 1 year later (Time 2) differed as a function of ADHD status. Based on the dual-cognitions model of alcohol use, we hypothesized that alcohol expectancies would be more strongly related to prospective alcohol use for individuals without ADHD compared to individuals with ADHD.
Method
Participants
ADHD group.
Participants with childhood ADHD were diagnosed with ADHD (according to the criteria in the Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised [DSM-III-R; American Psychiatric Association, 1987] or the DSM-IV [American Psychiatric Association, 1994]) at the ADD Clinic, Western Psychiatric Institute and Clinic, in Pittsburgh, PA, between 1987 and 1996. Average age at initial evaluation was 9.40 years old (SD = 2.27 years, range: 5.0–16.92). Ninety percent of children were diagnosed in their elementary school years (ages 5–12). The individuals with ADHD were selected for longitudinal follow-up with annual interviews because of their diagnosis of ADHD and participation in a summer treatment program for children with ADHD, an 8-week intervention that included behavioral modification, parent training, and psychoactive medication trials where indicated (Pelham and Hoza, 1996).
Diagnostic information for the participants with ADHD was collected in childhood using standardized parental and teacher DSM-III-R and DSM-IV symptom rating scales (Disruptive Behavior Disorders Rating Scale; Pelham et al., 1992) and a standardized semi-structured diagnostic interview administered to parents by a doctoral-level clinician. The information also included queries about other comorbidities to determine whether additional assessment was needed (instrument available through co-author W.E.P.). Two doctoral-level clinicians independently reviewed all ratings and interviews to confirm DSM diagnoses and when disagreement occurred, a third clinician reviewed the file and the majority decision was used. Exclusion criteria for follow-up were assessed in childhood and included a full-scale IQ score of less than 80; a history of seizures or other neurological problems; and/or a history of pervasive developmental disorder, schizophrenia, or other psychotic or organic mental disorders.
Of those eligible for follow-up in the PALS (n = 516), 70.5% participated (n = 364; M = 8.35 years after childhood diagnosis, SD = 2.79). A small percentage could not be located (n = 23), and 129 refused or failed to participate. Participants with childhood ADHD were compared with nonparticipating individuals with ADHD on demographic (e.g., age at first treatment, race, parental education level, and marital status) and diagnostic (e.g., parental and teacher ratings of ADHD symptoms and related symptomatology) variables collected in childhood. Only 1 of 14 comparisons was statistically significant at the p < .05 significance level. At the first PALS follow-up interview, which occurred on a rolling basis between 1999 and 2003, the mean age was 17.75 years (SD = 3.39 years, range: 11–25; three subjects were 26–28 years old). An age-relevant subsample was used for the current study (see section below on Subsample for the current study).
Non-ADHD group.
Individuals without ADHD were recruited into the PALS when individuals with ADHD were recruited for follow-up. Non-ADHD comparison participants were recruited on a rolling basis to ensure demographic similarity to the ADHD group (age within 1 year, sex, race, and highest parental education). They were recruited from the greater Pittsburgh area from several sources, including pediatric practices serving patients from diverse socioeconomic backgrounds (40.8%), advertisements in local newspapers and the university hospital staff newsletter (27.5%), local universities and colleges (20.8%), and other methods (10.9%) such as Pittsburgh Public Schools and word of mouth. A telephone screening interview administered to parents gathered basic demographic characteristics, history of diagnosis and treatment for ADHD and other behavior problems, presence of exclusionary criteria as previously listed for the ADHD participants, and a checklist of ADHD symptoms. Young adults ( ≥18 years) also provided self-report of the same information. Individuals who met DSM-III-R criteria for ADHD (presence of eight or more symptoms reported by either the parent or the young adult), currently or historically, were excluded. Non-ADHD comparison participants with subthreshold ADHD symptomatology, or with other psychiatric disorders, were retained. There were no statistically significant differences between the 364 individuals with childhood ADHD and the 240 non-ADHD comparison participants on age, sex, racial minority status, and highest parental education. As with the ADHD group, the non-ADHD comparison participants were interviewed on an annual basis once recruited into the PALS.
Subsample for the current study.
For the current study, data were selected for all participants ages 11–17 (M = 14.65, SD = 1.75) at recruitment into the follow-up study (Time 1: N = 286; ADHD: n = 165; non-ADHD: n = 121). Two hundred and seventy-seven participants completed the assessment the following year (Time 2). No statistically significant differences between ADHD and non-ADHD participants for this subsample were found on age, sex, or ethnicity/racial minority. Highest parental education, χ2(6) = 15.74, p < .05, and reported yearly household income, t(257) = 4.20, p < .01, were lower in the ADHD group than in the non-ADHD group. Individuals 18 years of age and older were excluded because of the educational and residential transitions for some at that transitional age that have implications for alcohol consumption.
Procedure
Interviews in adolescence were conducted by postbaccalaureate research staff. Informed consent was obtained from parents and children ages 14 years and older (children ages 11–13 provided assent), and all participants were assured confidentiality of all disclosed material, except in cases of impending danger or harm to self or others (reinforced with a Department of Health and Human Services Certificate of Confidentiality). In cases where distance prevented participant travel, information was collected through a combination of mailed and telephone correspondences; home visits were offered as need dictated. Self-report questionnaires were completed with either pencil-and-paper or computerized versions.
Measures
Alcohol consumption.
Alcohol use was assessed at each annual interview with a structured paper-and-pencil substance use questionnaire (Molina and Pelham, 2003; Molina et al., 2007) that is an adaptation of existing measures, including the Health Behavior Questionnaire (Jessor et al., 1989) and the National Household Survey of Drug Abuse interview (Substance Abuse and Mental Health Services Administration, 1992). The substance use questionnaire includes both lifetime exposure questions (e.g., have you ever had a drink, age at first drink) and quantity/frequency questions for alcohol and other substances. We created a factor score at each of the two time points using four substance use questionnaire items that assessed different facets of drinking behavior over the past 12 months: frequency of drinking, quantity consumed when drinking, frequency of five or more drinks, and frequency of drunkenness. The factor score at Time 1 (α = .94; skewness = 2.36; kurtosis = 4.91) was included as a covariate in regression analyses, whereas the factor score of drinking behavior at Time 2 (α = .95; skewness = 1.76; kurtosis = 2.13) was the outcome variable.
Explicit alcohol expectancies.
The Comprehensive Effects of Alcohol (CEOA) questionnaire (Fromme et al., 1993) is a widely used measure of explicit alcohol expectancies. The CEOA has 38 expectancy items, which have been found to load on two higher order factors of global positive and negative expectancies with seven distinct subscales (Fromme et al., 1993). Positive expectancies are sociability (eight items, α = .88), tension reduction (three items, α = .75), liquid courage (five items, α = .87), and sexuality (four items, α = .74). Negative expectancies are cognitive and behavioral impairments (nine items, α = .89), risk and aggression (five items, α = .73), and negative self-perception (four items, α = .64). The CEOA has demonstrated good test-retest and internal consistency reliability, and it has been found to be associated with alcohol use in adolescent and college student populations (Fromme and D’Amico, 2000; Fromme et al., 1993). The CEOA begins with the stem, “If I were under the influence from drinking alcohol” followed by 38 concluding phrases (e.g., I would be outgoing, I would have difficulty thinking, I would be clumsy). Ratings were obtained on a 4-point scale (1 = disagree, 2 = slightly disagree, 3 = slightly agree, and 4 = agree).
Data analytic plan
To test the hypothesis that individuals with a history of ADHD would have lower mean levels of alcohol expectancies compared with individuals without ADHD, t tests were conducted. Next, to examine the association between ADHD status, alcohol expectancies, and alcohol use, hierarchical regression analyses were conducted. All variables were mean centered, and separate hierarchical regressions were conducted for positive and negative alcohol expectancies predicting the Time 2 alcohol use factor score. For both regression equations, gender, age, ethnicity, and Time 1 alcohol use were entered in the first step as covariates. The main effects for positive or negative alcohol expectancies and ADHD status were entered in the second step. The interaction term between positive or negative expectancies and ADHD was entered in the last step.
Results
Alcohol use: Descriptive statistics
At Time 2, sufficient variability in alcohol use behavior was reported to test the study hypotheses (43% of participants indicated that they consumed at least one drink in the past 12 months compared with 36% at Time 1). Although the original scaled values for alcohol use were used in the main statistical analyses, the raw data were recoded for descriptive purposes here. Using the ordinal scale anchor points, we calculated the approximate number of times participants drank alcohol in the past 12 months and the average quantity of drinks consumed per drinking occasion. At Time 2, participants with a history of ADHD reported drinking approximately 12 different times in the past year (M = 12.15 days, SD = 40.18, range: 0–365 days) and consumed an average of a little more than two drinks per drinking occasion (M = 2.37, SD = 4.28, range: 0–26 drinks). At the same timepoint, participants without a history of ADHD reported drinking approximately 10 different times in the past year (M = 9.92 days, SD = 26.75, range: 0–130 days) and consumed an average of 1.5 drinks per drinking occasion (M = 1.55, SD = 2.48, range: 0–9.5 drinks). ADHD group differences in the four alcohol use variables were not statistically significant, frequency of drinking: t(272) = -.06, p = .95; quantity consumed when drinking: t(272) = -1.20, p = .23; frequency of five or more drinks: t(272) = -0.73, p = .47; and frequency of drunkenness: t(272) = -0.95, p = .34. However, previous work in the current sample has found ADHD-related differences in heavy drinking for the older adolescents ages 15–17 years (Molina et al., 2007).
Mean-level differences in alcohol expectancies
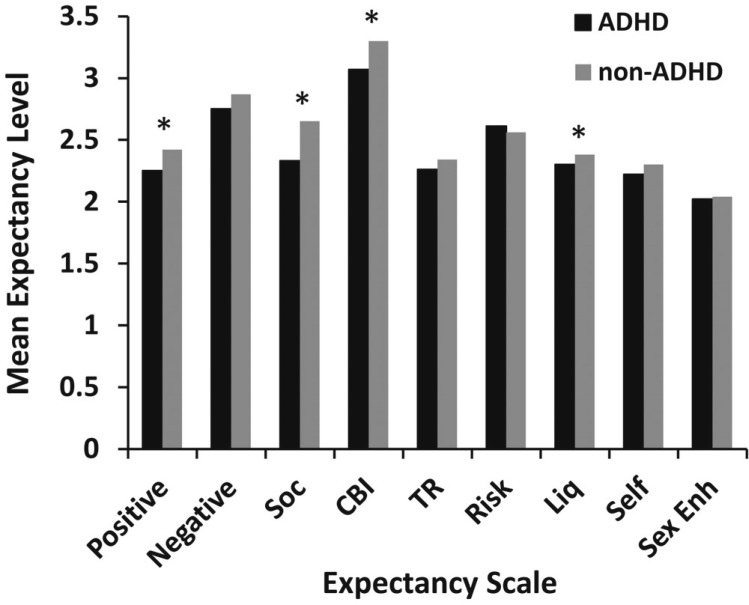
Mean levels of positive and negative alcohol expectancies were compared as a function of childhood ADHD status (Figure 1). At Time 1, individuals with ADHD had lower levels of global positive expectancies compared with individuals without ADHD, t(275) = 2.60, p < .01. Within this factor, individuals with ADHD had lower mean levels of sociability, t(275) = 2.92, p < .01, and liquid courage expectancies, t(275) = 2.54, p < .05, compared to those without ADHD. Individuals with and without ADHD did not differ in mean level for the global negative expectancies factor. However, individuals with childhood ADHD had significantly lower mean levels of cognitive and behavioral impairment expectancies, a facet of the global negative expectancies factor, t(270) = 2.15, p < .05. To further understand if these mean-level group differences were a result of differences in drinking experiences, supplemental analyses were conducted within the portion of the sample at Time 1 that did not have prior experience with alcohol (n = 170). The pattern of mean differences in expectancies was similar within the alcohol-naïve subsample: Individuals with ADHD had marginally lower levels of global positive expectancies, t(168) = 1.92, p = .06, and, within this factor, individuals with ADHD had lower mean levels of sociability, t(168) = 2.23, p < .05, and liquid courage expectancies, t(168) = 2.22, p < .05, compared to those without ADHD. Additionally, individuals with childhood ADHD held marginally lower levels of cognitive and behavioral impairment expectancies, which is a facet of the global negative expectancies factor, t(168) = 1.78, p = .08.
Figure 1.
Mean expectancy level as a function of attention-deficit/hyperactivity disorder (ADHD) status: Observed means of positive and negative alcohol expectancies and individual expectancy subscales separately for individuals with and without a history of ADHD. Notes: Positive = global positive expectancy subscale; negative = global negative expectancy subscale. Individual expectancy facets were abbreviated as follows: Soc = sociability; CBI = cognitive and behavioral impairment; TR = tension reduction; Risk = risk and aggression; Liq = liquid courage; Self = negative self-perception; Sex Enh = sexuality. *p < .05.
ADHD group differences in alcohol expectancies at Time 2 were then examined. Results were largely consistent with findings from Time 1: Individuals with a history of ADHD had lower levels of sociability, t(268) = 3.24, p < .001, and cognitive and behavioral impairment expectancies, t(268) = 2.53, p < .05. However, group differences in global positive expectancies were only marginally significant, t(268) = 1.91, p = .06, and the groups no longer differed in liquid courage expectancies, t(268) = 0.73, p = 47.
Alcohol expectancies and ADHD predicting prospective alcohol use
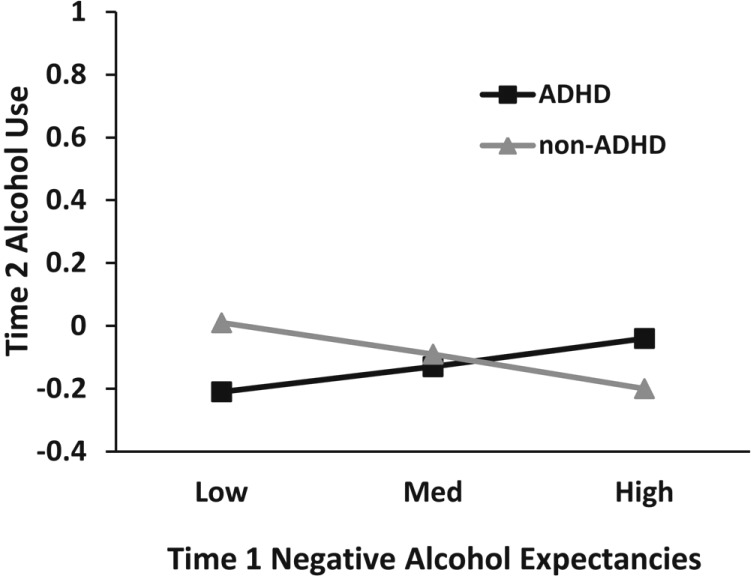
Separate regression equations for childhood ADHD and positive and negative alcohol expectancies predicting alcohol use 1 year later were conducted (see Table 1 for the equation for negative expectancies). When examining positive expectancies, a significant main effect was found (β = .16, p < .001): Higher levels of positive alcohol expectancies at Time 1 predicted increased alcohol use at Time 2. Additionally, age (β = .17, p < .001) and alcohol use at Time 1 (β = .61, p < .001) were related to alcohol use at Time 2. The interaction between positive alcohol expectancies and ADHD was not significant. The main effect of Time 1 negative expectancies on Time 2 alcohol use was not significant (β = .02, p = .72). However, there was a significant interaction between Time 1 negative expectancies and ADHD (β = .15, p < .05; Figure 2). Simple slopes for this interaction were analyzed according to the procedure recommended by Aiken and West (1991). These follow-up tests showed that the significant group difference in association between negative expectancy and alcohol use was attributable to contrasting directionality in the associations. Although each of the simple slopes were not significantly different from zero, the simple slope for the ADHD group was slightly positive in direction, β = .07, t(147) = 1.04, p =.30, and the simple slope for the non-ADHD group was slightly negative in direction, β = -.06, t(115) = -0.97, p = .33. When the covariates (gender, age, ethnicity, and Time 1 alcohol use)—which absorbed much of the variance in Time 2 alcohol use—were removed, the contrasting simple slopes were clearer. For the non-ADHD group, higher Time 1 negative expectancies predicted less Time 2 alcohol use, β = –.18, t(115) = –1.99, p < .05, but for the ADHD group, the association was not significant, β = −.04, t(147) = −0.48, p = .63.
Table 1.
Negative expectancies and ADHD predicting alcohol use 1 year later
| Variables entered on step | b | SE b | β |
| Equation for negative expectancies, R2 = .51, F(7, 258) = 37.56, p < .001 | |||
| Step 1 | |||
| Constant | -.15 | .16 | |
| Covariates (R2 change = .497, p < .001) | |||
| Gender | .20 | .17 | .05 |
| Ethnicity | -.05 | .04 | -.06 |
| Alcohol use Time 1 | .60 | .05 | .61*** |
| Age | .10 | .03 | 17*** |
| Step 2 | |||
| Main effects (R2 change = .001, p = .898) | |||
| Negative expectancies | .02 | .07 | .02 |
| ADHD | -.02 | .09 | -.01 |
| Step 3 | |||
| Interaction (R2 change = .008, p < .05) | |||
| Negative Expectancies × ADHD | .27 | .14 | .15* |
Notes: ADHD = attention-deficit/hyperactivity disorder; gender was coded 0 = male, 1 = female; ADHD group was coded 0 = non-ADHD, 1 = ADHD. b = unstandardized regression coefficient; SE b = unstandardized standard error; β = beta or standardized regression coefficient.
p < .05
p < .001
Figure 2.
ADHD Status Predicting Alcohol Use × Negative Expectancies: Graph of the two-way interaction between attention-deficit/hyperactivity disorder (ADHD) status and negative alcohol expectancies predicting alcohol use 1 year later. Age, gender, ethnicity, and Time 1 alcohol use were included as covariates. Med = medium.
Discussion
Despite research showing that individuals with a history of ADHD may be at increased risk for experiencing alcohol use problems in adulthood, little research has examined how widely studied predictors of early alcohol use relate to drinking behavior for this population. The current study is the first to examine the functioning of alcohol expectancies, a widely studied cognitive risk factor for alcohol use, for adolescents with and without a history of ADHD. We found that adolescents with ADHD histories reported lower mean levels of both positive and negative alcohol expectancies. Specifically, compared to adolescents without a history of ADHD, they had lower expectations that alcohol would have effects on them, either positively (social, courageous) or negatively (mentally and physically impaired). Importantly, there were ADHD group differences in the association between negative expectancies and alcohol use 1 year later, tentatively suggesting that negative expectancies are protective for individuals without, but not for individuals with, an ADHD history.
The dual process model of alcohol cognitions presented by Stacy and Wiers (Stacy and Wiers, 2010; Wiers and Stacy, 2006) postulates that certain individuals rely more on explicit and controlled processes (cool processing system), whereas other individuals rely more on implicit and automatic processes (hot processing system). However, this work has predominantly been conducted in student or normative adolescent populations. We extended this work to a population characterized by deficiencies in higher order cognitive processes needed to guide planful behavior—individuals with childhood ADHD. Our findings are consistent with the idea that individuals with ADHD may be less likely to access this “cool” processing system when making decisions to drink alcohol, particularly for the expected negative effects of drinking. Instead, individuals with ADHD may rely more on the “hot” processing system to decide when to drink alcohol.
Studies conducted in nonclinical populations have shown that, for individuals low in response inhibition (Houben and Wiers, 2009) or high in positive and negative urgency (Burton et al., 2012), automatic or implicit cognitions about alcohol use were more strongly related to drinking behavior than for individuals with lower levels of disinhibition. A similar process may be occurring for individuals with ADHD: Implicit alcohol-related cognitions may be more strongly driving drinking behavior compared to explicit cognitions measured with paper-and-pencil questionnaires that require insightful access to cognitive schemas that guide behavior. Future work testing the idea that implicit alcohol cognitions are more related to alcohol use for individuals with ADHD compared to their non-ADHD counterparts is needed. Additional work is also needed to understand why we found these effects for negative but not positive alcohol expectancies. One potential explanation could be that adolescents with a history of ADHD actually viewed some of the expected negative outcomes as “good.” Research has highlighted that integrating these subjective evaluations of the outcomes of alcohol use is important (Fromme and D’Amico, 2000), and it could be especially important in an ADHD population that is known to have increased reward sensitivity (e.g., Luman et al., 2010).
We also found tentative support for the possibility that expectancies may develop differently for individuals with, than without, ADHD. Lower mean levels of several facets of alcohol expectancies, despite similar levels of alcohol use, were found for the adolescents with, versus without, ADHD histories. Interestingly, based on the acquired preparedness model (e.g., Smith and Anderson, 2001), which has found that individuals high in impulsivity traits have higher mean levels of positive expectancies, we could have expected the opposite mean-level pattern of differences. Individuals with ADHD have higher levels of disinhibited personality traits, which could lead to the development of higher positive alcohol expectancies. However, in the current study, the ADHD portion of the sample had lower mean levels of expectancies at both time points. Additionally, individuals with a history of ADHD also had lower levels of certain facets of expectancies before the onset of drinking. Therefore, it might not be the impulsivity aspect of ADHD that is driving this effect. Rather, the attentional deficits of ADHD may influence the encoding and retrieval of these alcohol cognitions. Another possibility is that in clinical populations with more extreme levels of impulsivity, the acquired preparedness model becomes less applicable. Up to a certain point, higher levels of impulsivity may be related to increases in positive expectancies, but above a given threshold, impulsivity may have a different association with alcohol expectancy development. This possibility may also explain the seemingly inconsistent findings between the current study and a recent study that found a positive association between positive expectancies and number of ADHD symptoms in a college sample (Dattilo et al., 2013). Laboratory paradigms that study the formation and use of alcohol-related cognitions in children as a function of attentional capacity and impulsivity would be useful to understand the early determinants of drinking in this population. Additionally, integrating a more complete assessment of impulsivity facets (e.g., urgency, lack of planning) with the current findings would allow for a direct test of the acquired preparedness model in a population with elevated levels of impulsivity.
The current study provided an initial examination of alcohol expectancies in an adolescent sample with and without a history of ADHD. However, several limitations of this work are noted. First, given our focus on adolescents, the range of alcohol use was restricted, which may have limited our ability to detect effects and prevented us from examining how expectancies relate to more problematic or heavy drinking behavior. Further work examining alcohol expectancies in young adults with ADHD histories—when alcohol consumption is more frequent, heavier, and sometimes problematic—would allow testing of this possibility and build off the findings of Dattilo and colleagues (2013), as well as those of the current study. Second, the participants with a history of ADHD in the current study had elevated levels of both inattention and impulsivity symptoms, which restricted our ability to examine which specific subtype of ADHD (predominantly inattentive, predominantly hyperactive/impulsive, and combined type) was related to alcohol expectancy differences. Additionally, we were unable to examine ADHD symptoms dimensionally because of limited variability in these symptoms within the non-ADHD comparison group. However, our focus was to examine between-group differences instead of associations within the ADHD group. Future work examining ADHD symptoms dimensionally, with consideration of longitudinal patterns in symptoms, would facilitate a deeper understanding of the development of alcohol expectancies in this population. In line with this, future research designed to understand alcohol expectancies and related cognitive factors for individuals with ADHD and conduct problems may help to understand the additional alcohol-related risk for this subgroup shown in many studies (e.g., Flory and Lynam, 2003). Finally, recruitment of the non-ADHD group included reliance on imperfect parental recall of ADHD symptoms in childhood, and ADHD diagnosis may have been missed in a small proportion of our comparison sample. We recently reported a statistically significant correlation of .50 between ratings of ADHD symptoms provided by parents in childhood and later recalled when their children were adolescents (Sibley et al., 2012). However, our study is strengthened by the inclusion of parental report above and beyond reliance on self-report, which is well established in the ADHD field as biased (Barkley et al., 2002; Sibley et al., 2012).
Our study provides initial evidence that a widely studied predictor of alcohol use may function differently for individuals with ADHD. If negative expectancies are not relating to decisions to limit or abstain from alcohol, this may increase the risk for heavy alcohol use over time for this population. This is consistent with a growing body of literature showing that risk for alcohol-related problems increases in adulthood for individuals with a history of ADHD (Lee et al., 2011) and underscores the importance of conducting research to further understand why individuals with ADHD drink. Based on previous findings (e.g., Marshal et al., 2003), they may be affected more by direct environmental influences, such as social modeling or peer selection, and guided more by impulsive choices than by planful decisions to drink or abstain. Automatic associations about alcohol (e.g., implicit alcohol cognitions) may instead drive drinking behavior in these contexts, particularly in light of poor behavioral regulation that is characteristic of ADHD and the limited insight in this population (Hoza et al., 2002) that may affect both the development of expectancies and their connection to behavior. Research that integrates implicit cognitions about alcohol into this framework is needed, because if future interventions to reduce alcohol use assume that cognitions about alcohol operate similarly for individuals with and without ADHD, and they do not, then efforts to decrease alcohol use will be hampered. Instead, consistent with the dual process model tentatively supported by our findings, targeting implicit associations about alcohol (Wiers et al., 2011) may be particularly effective for people with ADHD.
Footnotes
This research was supported by National Institute on Alcohol Abuse and Alcoholism Grants AA011873, AA021135, AA007453, and AA00202. Additional support was provided by Grants DA12414, MH50467, MH12010, ESO5015, AA12342, DA016631, MH065899, KAI-118-S1, DA85553, MH077676, MH069614, MH62946, MH065899, MH53554, MH069434, IES LO3000665A, IESR324B060045, and NS39087.
References
- Aiken LS, West SG. Thousand Oaks, CA: Sage; 1991. Multiple regression: Testing and interpreting interactions. [Google Scholar]
- American Psychiatric Association. 3rd ed., rev. Washington, DC: Author; 1987. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- American Psychiatric Association. 4th ed. Washington, DC: Author; 1994. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- Barkley RA, Fischer M, Smallish L, Fletcher K. The persistence of attention-deficit/hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. Journal of Abnormal Psychology. 2002;111:279–289. [PubMed] [Google Scholar]
- Bekman NM, Goldman MS, Worley MJ, Anderson KG. Pre-adolescent alcohol expectancies: Critical shifts and associated maturational processes. Experimental and Clinical Psychopharmacology. 2011;19:420–432. doi: 10.1037/a0025373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton CM, Pedersen SL, McCarthy DM. Impulsivity moderates the relationship between implicit associations about alcohol and alcohol use. Psychology of Addictive Behaviors. 2012;26:766–772. doi: 10.1037/a0028742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dattilo L, Murphy KG, Van Eck K, Flory K. Do ADHD symptoms moderate the relation between positive alcohol expectancies and alcohol-related outcomes? ADHD Attention Deficit and Hyperactivity Disorders. 2013;5:93–104. doi: 10.1007/s12402-012-0098-y. [DOI] [PubMed] [Google Scholar]
- Duncan SC, Alpert A, Duncan TE, Hops H. Adolescent alcohol use development and young adult outcomes. Drug and Alcohol Dependence. 1997;49:39–48. doi: 10.1016/s0376-8716(97)00137-3. [DOI] [PubMed] [Google Scholar]
- Dunn ME, Goldman MS. Age and drinking-related differences in the memory organization of alcohol expectancies in 3rd-, 6th-, 9th-, and 12th-grade children. Journal of Consulting and Clinical Psychology. 1998;66:579–585. doi: 10.1037//0022-006x.66.3.579. [DOI] [PubMed] [Google Scholar]
- Dunn ME, Goldman MS. Validation of multidimensional scaling-based modeling of alcohol expectancies in memory: Age and drinking-related differences in expectancies of children assessed as first associates. Alcoholism: Clinical and Experimental Research. 2000;24:1639–1646. [PubMed] [Google Scholar]
- Flory K, Lynam DR. The relation between attention deficit hyperactivity disorder and substance abuse: What role does conduct disorder play? Clinical Child and Family Psychology Review. 2003;6:1–16. doi: 10.1023/a:1022260221570. [DOI] [PubMed] [Google Scholar]
- Fromme K, D’Amico EJ. Measuring adolescent alcohol outcome expectancies. Psychology of Addictive Behaviors. 2000;14:206–212. doi: 10.1037//0893-164x.14.2.206. [DOI] [PubMed] [Google Scholar]
- Fromme K, Stroot EA, Kaplan D. Comprehensive effects of alcohol: Development and psychometric assessment of a new expectancy questionnaire. Psychological Assessment. 1993;5:19–26. [Google Scholar]
- Goldman MS. The alcohol expectancy concept: Applications to assessment, prevention, and treatment of alcohol abuse. Applied and Preventive Psychology. 1994;3:131–144. [Google Scholar]
- Houben K, Wiers RW. Response inhibition moderates the relationship between implicit associations and drinking behavior. Alcoholism: Clinical and Experimental Research. 2009;33:626–633. doi: 10.1111/j.1530-0277.2008.00877.x. [DOI] [PubMed] [Google Scholar]
- Hoza B, Pelham WE, Jr, Dobbs J, Owens JS, Pillow DR. Do boys with attention-deficit/hyperactivity disorder have positive illusory self-concepts? Journal of Abnormal Psychology. 2002;111:268–278. doi: 10.1037//0021-843x.111.2.268. [DOI] [PubMed] [Google Scholar]
- Jessor R, Donovan JE, Costa FM. Boulder, CO: University of Colorado, Institute of Behavioral Science; 1989. Health Behavior Questionnaire. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2012. Monitoring the Future national survey results on drug use, 1975–2011: Volume I, Secondary school students. [Google Scholar]
- Lee SS, Humphreys KL, Flory K, Liu R, Glass K. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: A meta-analytic review. Clinical Psychology Review. 2011;31:328–341. doi: 10.1016/j.cpr.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luman M, Tripp G, Scheres A. Identifying the neurobiology of altered reinforcement sensitivity in ADHD: A review and research agenda. Neuroscience and Biobehavioral Reviews. 2010;34:744–754. doi: 10.1016/j.neubiorev.2009.11.021. [DOI] [PubMed] [Google Scholar]
- Marshal MP, Molina BSG, Pelham WE., Jr Childhood ADHD and adolescent substance use: An examination of deviant peer group affiliation as a risk factor. Psychology of Addictive Behaviors. 2003;17:293–302. doi: 10.1037/0893-164X.17.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller PM, Smith GT, Goldman MS. Emergence of alcohol expectancies in childhood: A possible critical period. Journal of Studies on Alcohol. 1990;51:343–349. doi: 10.15288/jsa.1990.51.343. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Hinshaw SP, Arnold LE, Swanson JM, Pelham WE, Hechtman L, Hoza B. the MTA Cooperative Group. Adolescent substance use in the multimodal treatment study of attention-deficit/hyperactivity disorder (ADHD) (MTA) as a function of childhood ADHD, random assignment to childhood treatments, and subsequent medication. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52:250–263. doi: 10.1016/j.jaac.2012.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina B. S. G, Pelham W. E., Jr Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. Journal of Abnormal Psychology. 2003;112:497–507. doi: 10.1037/0021-843x.112.3.497. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Pelham WE, Gnagy EM, Thompson AL, Marshal MP. Attention-deficit/hyperactivity disorder risk for heavy drinking and alcohol use disorder is age specific. Alcoholism: Clinical and Experimental Research. 2007;31:643–654. doi: 10.1111/j.1530-0277.2007.00349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelham WE, Jr, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Hoza B. Intensive treatment: A summer treatment program for children with ADHD. In: Hibbs ED, Jensen PS, editors. Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice. New York: American Psychological Association Press; 1996. pp. 311–340. [Google Scholar]
- Seidman LJ. Neuropsychological functioning in people with ADHD across the lifespan. Clinical Psychology Review. 2006;26:466–485. doi: 10.1016/j.cpr.2006.01.004. [DOI] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE, Jr, Molina BSG, Gnagy EM, Waschbusch DA, Garefino AC, Karch KM. Diagnosing ADHD in adolescence. Journal of Consulting and Clinical Psychology. 2012;80:139–150. doi: 10.1037/a0026577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith GT, Anderson KG. Adolescent risk for alcohol problems as acquired preparedness: A model and suggestions for intervention. In: Monti PM, Colby SM, O’Leary TA, editors. Adolescents, alcohol, and substance abuse: Reaching teens through brief interventions. New York, NY: Guilford Press; 2001. pp. 109–141. [Google Scholar]
- Smith GT, Goldman MS, Greenbaum PE, Christiansen BA. Expectancy for social facilitation from drinking: The divergent paths of high-expectancy and low-expectancy adolescents. Journal of Abnormal Psychology. 1995;104:32–40. doi: 10.1037//0021-843x.104.1.32. [DOI] [PubMed] [Google Scholar]
- Stacy AW, Wiers RW. Implicit cognition and addiction: A tool for explaining paradoxical behavior. Annual Review of Clinical Psychology. 2010;6:551–575. doi: 10.1146/annurev.clinpsy.121208.131444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Rockville, MD: 1992. National Household Survey on Drug Abuse. Author. Retrieved from http://www.icpsr.umich.edu/icpsrweb/SAMHDA/studies/6887. [Google Scholar]
- Thush C, Wiers RW, Ames SL, Grenard JL, Sussman S, Stacy AW. Interactions between implicit and explicit cognition and working memory capacity in the prediction of alcohol use in at-risk adolescents. Drug and Alcohol Dependence. 2008;94:116–124. doi: 10.1016/j.drugalcdep.2007.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walther CAP, Cheong J, Molina BSG, Pelham WE, Jr, Wymbs BT, Belendiuk KA, Pedersen SL. Substance use and delinquency among adolescents with childhood ADHD: The protective role of parenting. Psychology of Addictive Behaviors. 2012;26:585–598. doi: 10.1037/a0026818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiers RW, Eberl C, Rinck M, Becker ES, Lindenmeyer J. Retraining automatic action tendencies changes alcoholic patients’ approach bias for alcohol and improves treatment outcome. Psychological Science. 2011;22:490–497. doi: 10.1177/0956797611400615. [DOI] [PubMed] [Google Scholar]
- Wiers RW, Stacy AW. Implicit cognition and addiction. Current Directions in Psychological Science. 2006;15:292–296. [Google Scholar]