Abstract
Cervical cancer is the most common female genital tract malignancy in Korean women. Although age-standardized cancer incidence rate of cervical cancer has decreased from 18.6 per 100,000 women in 1999 to 12.3 per 100,000 women in 2010 in Korea with widespread routine screening, several epidemiologic characteristics are still present. Incidence of cervical cancer still varies according to geographic area, and a significant portion of cases are detected at a locoregionally advanced stage, without significant improvement of five-year survival rate.2014-01-15 Cervical screening techniques such as the Pap smear should be the gold standard strategy to decrease incidence and to improve the survival outcomes of patients with cervical cancer. In addition, screening programs for cervical cancer should be designed, organized and directed within the context of a nationwide program for cancer control.
Keywords: Cervical cancer, Incidence, Korea, Screening programs, Survival outcomes
INTRODUCTION
Cervical cancer is the third most common malignant disease of women worldwide and the most common malignant disease afflicting women in many developing countries [1,2]. Even though the incidence of cervical cancer has been reduced in developed countries in recent decades as a result of widespread, routine screening tests for premalignant lesions, the cancer burden (as related to incidence and mortality) has been reported to be disproportionately high in many developing countries [3]. The reported epidemiologic characteristics may be inaccurate in many low-resource countries due to the deficiency of well-organized reporting systems. The Korea Central Cancer Registry (KCCR), a nationwide and hospital-based cancer registry, has been operating since 1980. The statistical portal system containing data for cancer diseases constructed by KCCR is available and open to public via the Statistics Korea and National Cancer Center website [4,5]. This paper aims to review the epidemiologic characteristics of cervical cancer in Korean women based on these data and to emphasize the significance of screening test in decreasing the incidence of cervical cancer.
DATA SOURCES
We obtained the data for cervical cancer constructed by KCCR from the Statistics Korea and National Cancer Center website [4,5]. The history, objectives and activities of KCCR have been reported elsewhere [6]. The details for data processing were described previously in reports from Korean researchers [7-9]. Briefly, the collected data included the number of patients with cervical cancer, incidence rate calculated per 100,000 women for age-groups, rate of cervical cancer screening, International Federation of Gynecology and Obstetrics (FIGO) stage distribution, age-standardized mortality rate and 5-year survival rates. The number of women diagnosed with cervical cancer and age-standardized incidence rate (ASR) is reported annually. ASRs for cervical cancer according to geographic areas in 2002 and 2010 are compared. Age-standardized prevalence rate is reported from 2007 to 2010. The rate of cervical cancer screenings reported annually from 2002 to 2010. Age-standardized mortality rate is reported annually from 2000 to 2011. Five-year survival rate of women with cervical cancer is reported with every 5-year group from 1993 to 2010. Age-specific incidence rates for cervical cancer are reported in 5-year age group every year from 1999 to 2010. The stage distribution from 1999 to 2004 is reported based on FIGO clinical staging system revised in 1995. The data for stage distribution is available from the annual reports of the Gynecologic Oncology Committee of Korean Society of Obstetrics and Gynecology [10-15].
INCIDENCE, SCREENING RATE, STAGE DISTRIBUTION, AND SURVIVAL
A total of 49,503 women were diagnosed with cervical cancer from 1999 to 2010. Since the peak of 4,572 cases in 2001, the annual number of cervical cancer cases has been steadily declining, and reached 3,857 in 2010. The ASR of cervical cancer also decreased from 18.6 per 100,000 women in 1999 to 12.3 per 100,000 women in 2010 (Fig. 1) [4]. Table 1 shows the change of the age-specific incidence rate per 100,000 women from 1999 to 2010 [4]. Generally, the incidence rate decreased in all age groups except the 20-29 years and greater than 85 years groups. Compared with the ASR of 2002, all areas showed a reduced ASR in 2010. However, the ASRs of other areas were higher than that of Seoul (Fig. 2) [4]. In addition, age-standardized prevalence rate of cervical cancer decreased from 56.8 per 100,000 women in 2007 to 51.2 per 100,000 women in 2010 (Fig. 3) [4].
Fig. 1.
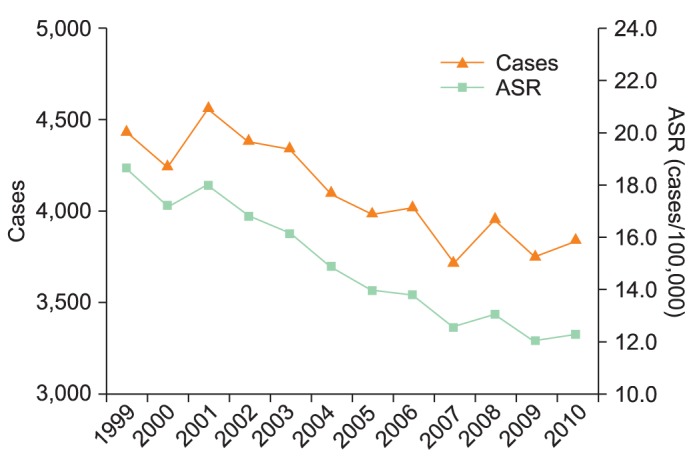
The number and age-standardized incidence rate (ASR) of women diagnosed with cervical cancer, 1999 to 2010.
Table 1.
Age-specific incidence rates for cervical cancer from 1999 to 2010
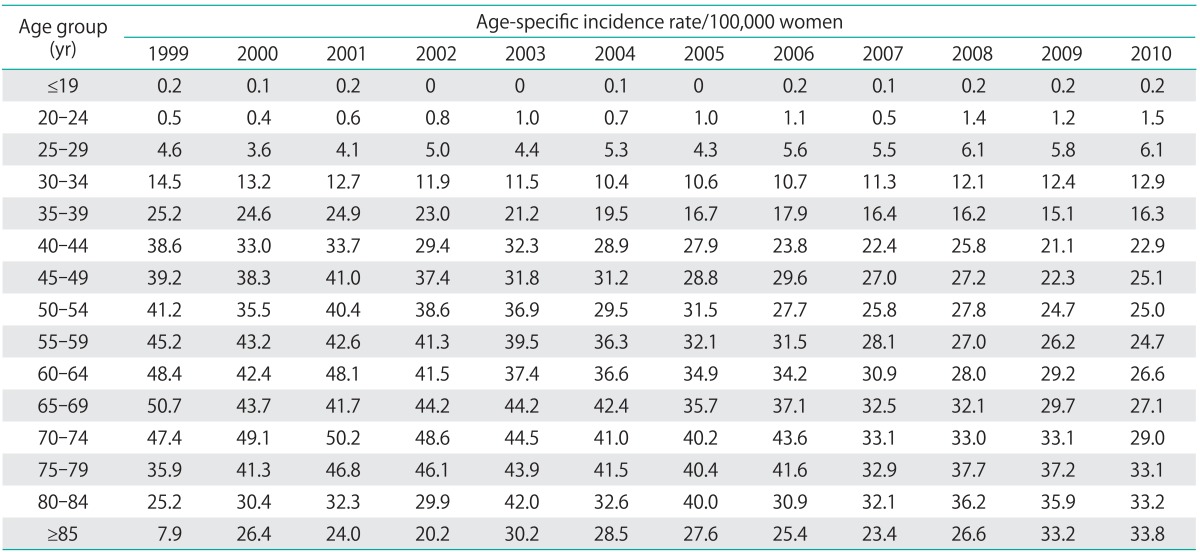
Fig. 2.
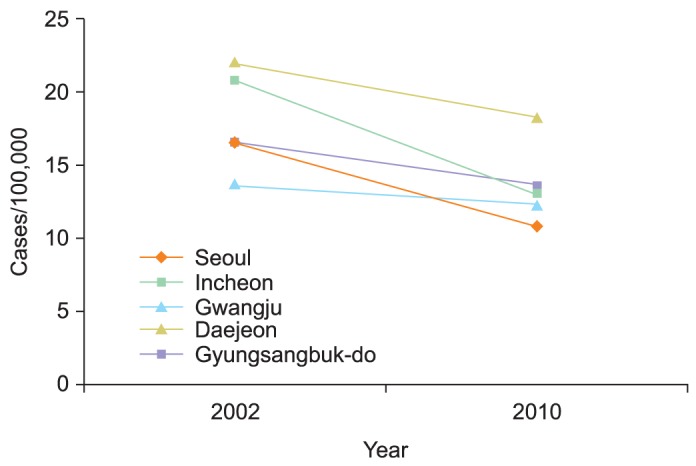
Age-standardized incidence rates for cervical cancer according to geographic areas in 2002 and 2010.
Fig. 3.
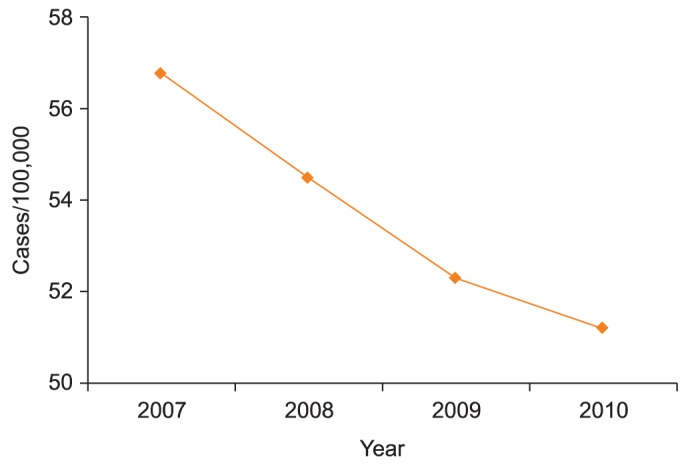
Age-standardized prevalence rate of cervical cancer, 2007-2010.
To review the relationship between the rate of cervical cancer screening and the incidence rate of cervical cancer, we examined the overall rate of participation in the cervical cancer screening arm of the National Cancer Screening Program, whose target population includes Medical Aid Program recipients and the lower income bracket of National Health Insurance beneficiaries, and the screening rate of cervical cancer based on recommendation, proportion of females aged 30 and above who received a Pap smear in the latest two years, including individual screening as well as organized screening. Although the former has been increasing steadily since 2004, it does not reach 20% even in 2010. The latter has also increased from 58.3% in 2004 to 62.4% in 2011 (Fig. 4) [5].
Fig. 4.
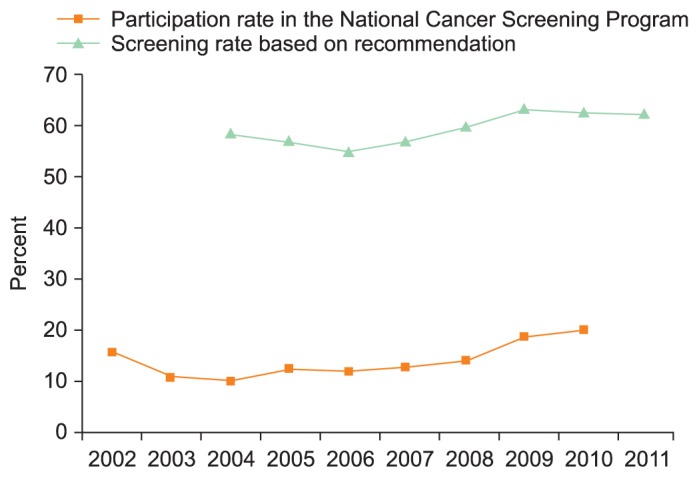
Participation rate in the National Cancer Screening Program and screening rate based on recommendation for cervical cancer.
Table 2 shows the stage distribution from 1999 to 2004. Stage IB1 was the most common stage at 26.6%, followed by stage IA1 at 20.8%. However, about 50% of patients were diagnosed at a loco-regionally advanced stage ≥ IB2 [10-15].
Table 2.
FIGO stage distribution of cervical cancer in Korea from 1999 to 2004
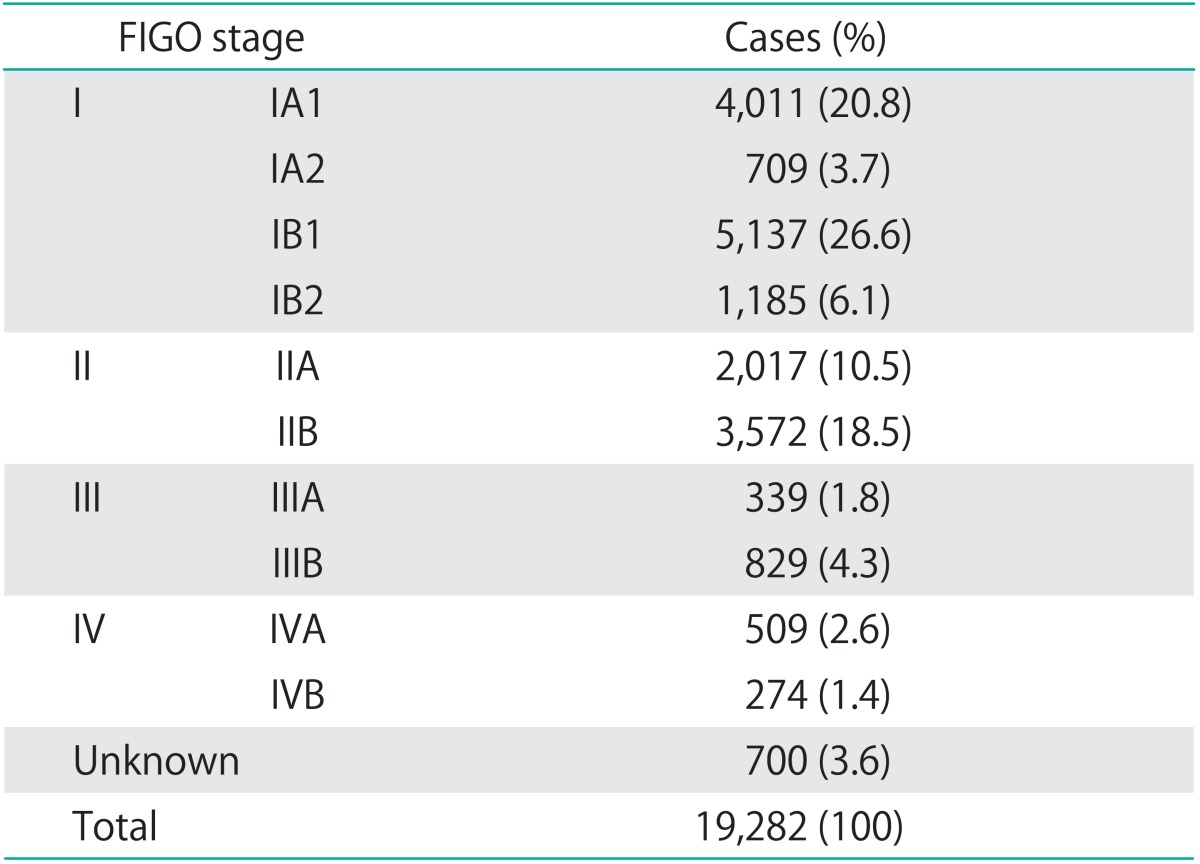
FIGO, International Federation of Gynecology and Obstetrics.
The age-standardized mortality rate per 100,000 women has been steadily declining and reached 2.9 in 2011, since the peak of 4.4 in 2003 (Fig. 5) [4]. Five-year survival rate from 1993 to 1995 was 77.5%. After that, 5-year survival rate improved slightly more than 80%. Unlike the expectation, however, 5-year survival rate seems to be stagnant between 80.0% and 81.2% over the last 15 years [4].
Fig. 5.
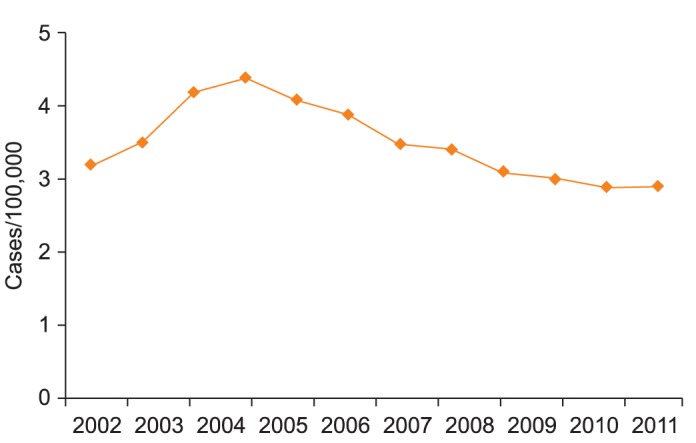
Age-standardized mortality rate of cervical cancer, 2003-2011.
DISCUSSION AND CONCLUSION
The total number and ASR of cervical cancer have been decreased steadily over the last two decades. Furthermore, the estimated ASRs of cervical cancer were 8.9 and 8.5 per 100,000 women in 2011 and 2012, respectively [7,8]. The decrease of cervical cancer incidence must be a result of the increased cervical cancer screening rate. The lifetime screening rate for cervical cancer in Korean women was 74.8% in 2011 [5]. And the screening rate of cervical cancer based on recommendation increased from 58.3% in 2004 to 62.4% in 2011 [5]. However, this was still lower than the 77.8%-79.0% in 2011/12 and 73.8% in 2010 observed in the UK and USA, respectively [16,17]. Currently, two population-based organized cancer screening program exit in Korea: the National Cancer Screening Program, and the National Health Insurance Cancer Screening Program, which is provided to the remainder of National Health Insurance beneficiaries [18]. The participation rates of National Health Insurance Cancer Screening Program for cervical cancer were 40.3% and 44.5% in 2010 and 2011, respectively [19]. And the annual participation rate of the National Cancer Screening Program for people in the lower income bracket is less than 20%. Furthermore, the participation rate in cervical screening of the National Cancer Screening Program was much lower than those of the stomach, liver, colon, and breast (30.7%-43.5% in 2010) in Korea [5]. Considering the improved screening rate of cervical cancer based on recommendation and the decrease of cervical cancer incidence, a significant portion of cervical cancer screening seems to be done by individual screening as well as by organized screening [5]. Thus, continuing development of strategies to improve the participation rate and the quality of organized screening program is an important aspect of controlling cervical cancer spread.
The incidence rate of cervical cancer decreased in all age groups except the 20-29 years and greater than 85 years groups. However, the reason for the increasing trends of age-specific incidence rate for the 20-29 years and greater than 85 years groups might be different. Increased life expectancy and improved accessibility to medical care could explain the increase in the greater than 85 years group, whereas the change of sexual culture, as well as increasing cancer screening, could explain the increasing cancer incidence in the 20-29 years group.
Another important issue is the variation in cancer incidence between geographic areas according to socio-economic status [3]. The ASRs of other areas were higher than that of Seoul. These results seem to reflect differences in medical care accessibility, economic level, population composition and education regarding the necessity of cancer screening between geographic areas, and are consistent with previous report that socioeconomic status and education levels could serve as important factors in cancer-related health inequalities [20].
Stage distribution seems to be in the dismals. In this report, about 50% of patients were diagnosed at a loco-regionally advanced stage ≥ IB2. More recent data from 2005 to 2010 for stage distribution are available from KCCR. These data were reported simply as localized, regional, distant and unknown stage. These data showed that only 54% of patients were diagnosed at a localized stage [4]. These findings might suggest that the current screening program does not work well in the general population; hence, many patients still seem to be diagnosed at a loco-regionally advanced stage.
Even though the five-year survival rate of cervical cancer in Korea is higher than those of the USA (70.4%), Canada (72%), and Japan (73.4%), it has not been significantly improved over the last two decades in spite of increasing cancer screening and advancement of treatment strategies [21-23]. It is uncertain whether this observation results from time lag between the screening and survival outcomes, a significant proportion of loco-regionally advanced cervical cancer, the increasing cancer incidence in the elderly or other factors.
In summary, several epidemiologic characteristics of cervical cancer in Korean women are present. With the widespread use of effective screening tests and early detection with proper management of premalignant lesions of the cervix, the incidence of cervical cancer has been decreasing steadily. However, the incidence of cervical cancer still varies by geographic area and a significant portion of cases are detected at a locoregionally advanced stage, reflecting the need for improvement in cancer screening program.
For many years to come, cervical screening tests such as the Pap smear should be the gold standard strategy to decrease the incidence and to improve the survival outcomes of cervical cancer. In addition, screening programs for cervical cancer should be designed, organized and directed within the context of a nationwide program for cancer control.
ACKNOWLEDGEMENT
This paper was based on data from the Statistics Korea and National Cancer Center website. We sincerely thank the physicians, statisticians and administrative officers who collected the data and constructed the statistical portal system.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001;94:153–156. doi: 10.1002/ijc.1440. [DOI] [PubMed] [Google Scholar]
- 3.Lee JM. Screening of uterine cervical cancer in low-resource settings. J Gynecol Oncol. 2012;23:137–138. doi: 10.3802/jgo.2012.23.3.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Statistics Korea. Korean Statistical Information Service [Internet] Daejeon: Statistics Korea; 2012. [cited 2013 Apr 30]. Available from: http://kosis.kr. [Google Scholar]
- 5.National Cancer Center. National Cancer Information Center [Internet] Goyang: National Cancer Center; 2012. [cited 2013 Apr 30]. Available from: http://www.cancer.go.kr. [Google Scholar]
- 6.Shin HR, Won YJ, Jung KW, Kong HJ, Yim SH, Lee JK, et al. Nationwide cancer incidence in Korea, 1999~2001; first result using the national cancer incidence database. Cancer Res Treat. 2005;37:325–331. doi: 10.4143/crt.2005.37.6.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jung KW, Park S, Won YJ, Kong HJ, Lee JY, Park EC, et al. Prediction of cancer incidence and mortality in Korea, 2011. Cancer Res Treat. 2011;43:12–18. doi: 10.4143/crt.2011.43.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jung KW, Park S, Won YJ, Kong HJ, Lee JY, Seo HG, et al. Prediction of cancer incidence and mortality in Korea, 2012. Cancer Res Treat. 2012;44:25–31. doi: 10.4143/crt.2012.44.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chung HH, Jang MJ, Jung KW, Won YJ, Shin HR, Kim JW, et al. Cervical cancer incidence and survival in Korea: 1993-2002. Int J Gynecol Cancer. 2006;16:1833–1838. doi: 10.1111/j.1525-1438.2006.00708.x. [DOI] [PubMed] [Google Scholar]
- 10.Korean Society of Obstetrics and Gynecology. Annual report of gynecologic cancer registry program in Korean for 1999(Jan. 1, 1999 - Dec. 31, 1999) Korean J Obstet Gynecol. 2002;45:1665–1699. [Google Scholar]
- 11.Korean Society of Obstetrics and Gynecology. Annual report of gynecologic cancer registry program in Korea for 2000: Jan. 1, 2000 - Dec. 31, 2000. Korean J Obstet Gynecol. 2003;46:221–258. [Google Scholar]
- 12.Korean Society of Obstetrics and Gynecology. Annual report of gynecologic cancer registry program in Korean for 2001 (Jan. 1, 2001 - Dec. 31, 2001) Korean J Obstet Gynecol. 2003;46:1849–1887. [Google Scholar]
- 13.Lee MY, Cho CH, Kwon SH, Song DK, Chung SW, Kang HO, et al. Annual report of gynecologic cancer registry program in Korean for 2002 (Jan. 1st, 2002 - 2002 - Dec. 31st, 2002) Korean J Obstet Gynecol. 2004;47:1029–1070. [Google Scholar]
- 14.Korean Society of Obstetrics and Gynecology. Annual report of gynecologic cancer registry program in Korea for 2003 (Jan. 1st, 2003-Dec. 31st, 2003) Korean J Obstet Gynecol. 2006;49:762–812. [Google Scholar]
- 15.SOG Gynecologic Oncology Committee. Annual report of gynecologic cancer registry program in Korea for 2004 (Jan. 1st, 2004-Dec. 31st, 2004) Korean J Obstet Gynecol. 2007;50:28–78. [Google Scholar]
- 16.NHS Cancer Screening Programmes. NHS cervical screening programme: annual review 2009. Sheffield: NHS Cancer Screening Programmes; 2009. [Google Scholar]
- 17.National Cancer Institute. Cancer trends progress report: 2010/2011 update [Internet] Bethesda, MD: National Cancer Institute; c2013. [cited 2013 Jun 19]. Available from: http://progressreport.cancer.gov. [Google Scholar]
- 18.Lee YH, Choi KS, Lee HY, Jun JK. Current status of the National Cancer Screening Program for cervical cancer in Korea, 2009. J Gynecol Oncol. 2012;23:16–21. doi: 10.3802/jgo.2012.23.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Health Insurance Service, Health Insurance Review & Assessment Service. 2011 National Health Insurance statistical yearbook. Seoul: National Health Insurance Service, Health Insurance Review & Assessment Service; 2012. [Google Scholar]
- 20.Singh GK, Miller BA, Hankey BF, Edwards BK. Persistent area socioeconomic disparities in U.S. incidence of cervical cancer, mortality, stage, and survival, 1975-2000. Cancer. 2004;101:1051–1057. doi: 10.1002/cncr.20467. [DOI] [PubMed] [Google Scholar]
- 21.National Cancer Institute. Surveillance epidemiology and end results cancer statistics review 1975-2010 [Internet] Bethesda, MD: National Cancer Institute; c2013. [cited 2013 Jun 19]. Available from: http:// seer.cancer.gov. [Google Scholar]
- 22.Kachuri L, De P, Ellison LF, Semenciw R Advisory Committee on Canadian Cancer Statistics. Cancer incidence, mortality and survival trends in Canada, 1970-2007. Chronic Dis Inj Can. 2013;33:69–80. [PubMed] [Google Scholar]
- 23.Matsuda T, Ajiki W, Marugame T, Ioka A, Tsukuma H, Sobue T, et al. Population-based survival of cancer patients diagnosed between 1993 and 1999 in Japan: a chronological and international comparative study. Jpn J Clin Oncol. 2011;41:40–51. doi: 10.1093/jjco/hyq167. [DOI] [PubMed] [Google Scholar]


