Abstract
Objective
Descriptions of the inpatient experience for patients hospitalized with systolic heart failure (HF) are limited and lack a cross-sectional representation of the US population. While length of stay (LOS) is a primary determinant of resource use and post-discharge events, few models exist for estimating LOS.
Research design and methods
MarketScan® administrative claims data from 1/1/2005–6/30/2008 were used to select hospitalized patients aged ≥18 years with discharge diagnoses for both HF (primary diagnosis) and systolic HF (any diagnostic position) without prior HF hospitalization or undergoing transplantation.
Results
Among 17,597 patients with systolic HF; 4109 had commercial; 2118 had Medicaid; and 11,370 had Medicare payer type. Medicaid patients had longer mean LOS (7.1 days) than commercial (6.3 days) or Medicare (6.7 days). In-hospital mortality was highest for patients with Medicaid (2.4%), followed by Medicare (1.3%) and commercial (0.6%). Commercial patients were more likely to receive inpatient procedures. Renal failure, pressure ulcer, malnutrition, a non-circulatory index admission DRG, receipt of a coronary artery bypass procedure or cardiac catheterization, or need for mechanical ventilation during the index admission were associated with increased LOS; receipt of a pacemaker device at index was associated with shorter LOS.
Limitations
Selection of patients with systolic HF is limited by completeness and accuracy of medical coding, and results may not be generalizable to patients with diastolic HF or to international populations.
Conclusion
Inpatient care, LOS, and in-hospital survival differ by payer among patients hospitalized with systolic HF, although co-morbidity and inpatient procedures consistently influence LOS across payer types. These findings may refine risk stratification, allowing for targeted intensive inpatient management and/or aggressive transitional care to improve outcomes and increase the efficiency of care.
Keywords: Heart failure, Systolic, Hospitalization, Length of stay, Payer
Introduction
Heart failure (HF) is the primary diagnosis for more than 1 million hospitalizations in the US annually1, making HF the most common cause of hospitalization and re-admission among older Americans2. Annual direct medical costs for HF have been estimated at $39.2 billion1, of which more than 70% are attributable to inpatient care3.
Significant variation in the inpatient experience exists between patients hospitalized with HF. Among hospitals participating in Get With the Guidelines Heart Failure (GWTG-HF), HF LOS varied from 2 days at the 25th percentile to 6 days at the 75th percentile4. For the majority of patients with heart failure the only acute therapy delivered is intravenous diuretics5; however, for those patients who require vasoactive therapy and intensive care, costs and complications are much higher6. Inpatient experience can also vary by payer. GWTG-HF data show that patients lacking health insurance, with Medicaid, or with Medicare were less likely to receive a range of inpatient medications and procedures and had a longer length of stay (LOS) than those with commercial insurance7. Patients with Medicaid had the highest inhospital mortality7.
LOS is the primary driver of HF hospitalization costs6,8. Longer LOS is also associated with lower performance on quality-of-care measures9 and higher rates of subsequent readmission and mortality2,10. Mean HF LOS in the US has decreased in recent years; however, this trend is at least partially representative of shifts in care, as an increase in discharges to skilled nursing facilities as well as an increase in 30-day readmission rates were seen in the same period11.
The ability to accurately risk stratify patients for the length and complexity of hospitalization can help guide expectations for patients, clinicians, administrators, and even reimbursement policies. For example, identification during the hospital course of patients with HF who are likely to experience a longer and more complicated hospital stay may help to more appropriately tailor the level of inpatient care, timing of education, nature of discharge planning, and intensity of transitional programs.
Despite the relevance of such predictive information, existing studies of LOS and hospital course are limited4,6,12–14. Data used in some of these LOS risk models have come from small non-US populations12,14, where average HF LOS is much longer15,16. Others have lacked a comprehensive cross-sectional sampling of the hospitalized US HF population4,6,13. All of these studies grouped HF of any type into a single study population, ignoring the greater heterogeneity and less accurate identification of patients with HF and preserved left ventricular ejection fraction (LVEF)17,18. The specificity of ICD-9-CM algorithms in identifying heart failure is improved when it is confined to a diagnosis of systolic heart failure, the very population for whom many guideline recommendations are specifically indicated19. Perhaps because of these limitations, existing predictive models have failed to explain more than a limited portion of the variance in HF LOS (e.g., R2=4.8% in GWTG-HF) and/or have failed to find common use in the management of these patients4.
Therefore, we set out to characterize the range of inpatient experience for patients hospitalized with systolic HF, including LOS and in-hospital mortality, and to identify predictors of LOS in terms of patient demographics, underlying disease burden, and inpatient events for a broad sampling of patients covered under three payer types: commercial, Medicaid, and Medicare. Development of models based on common administrative data from a variety of payer sources may be particularly helpful in creating automated measures of inpatient risk and resource utilization.
Patients and methods
A retrospective, observational study was conducted to select patients by payer type with a hospitalization for systolic HF using administrative claims from three Truven Health MarketScan® Research Databases—the Commercial Claims and Encounters Database (Commercial), the Medicaid Multistate Database (Medicaid), and the Medicare Supplemental and Co-ordination of Benefits Database (Medicare). The Commercial database, constructed from claims and enrollment data provided by large employer-sponsored health plans from across the US, contains the healthcare experience of over 35 million privately insured individuals (employees, their spouses, and dependents) covered under a variety of fee-for-service, fully capitated, and partially capitated health plans. The Medicaid database contains the pooled healthcare experience of ~10 million Medicaid enrollees each year from multiple geographically dispersed states. The Medicare database contains the healthcare experience of ~2.5 million individuals annually with Medicare Supplemental insurance paid for by employers.
Data include medical claims for healthcare services performed in both the inpatient and outpatient setting, as well as outpatient pharmacy claims and enrollment data including member demographic information, eligibility, and benefits data. The MarketScan® Research Databases include persons from all US States and are de-identified and are fully compliant with the Health Insurance Portability and Accountability Act of 1996 (HIPAA). Because this study did not involve the collection, use, or transmittal of individually identifiable data, Institutional Review Board (IRB) review or approval was not required.
Patient selection
Patients aged 18 years and older were selected based on the occurrence of a hospitalization containing discharge diagnoses for both HF (primary diagnosis) and systolic HF (any diagnostic position) during the January 1, 2005 through June 30, 2008 time period. HF was defined by International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnosis codes 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, and 428.xx, as used in the Hospital Compare method, approved by National Quality Forum and publicly reported by the Centers for Medicare and Medicaid Services (CMS)20,21. Systolic HF was defined by ICD-9-CM diagnosis codes 428.1, 428.20, 428.21, 428.22, 428.23, 428.40, 428.41, 428,42, and 428.43. The first hospitalization meeting these diagnostic criteria (index admission) was used for the study analyses. Patients were required to have at least 12 months (pre-period) of continuous medical and pharmacy eligibility prior to the admission date (index date) of the index admission. Because LOS was to be evaluated for the first observed HF hospitalization, patients with evidence in the pre-period of a hospitalization claim for HF were excluded. Patients were also excluded if the index admission claim included codes consistent with heart transplantation due to the rare and atypical nature of these admissions. Systolic HF case groups were selected for each of the three payer types: commercial, Medicaid, and Medicare.
Study variables
Demographic variables as of index date included mean age, age group, gender, insurance plan type (managed care, fee-for-service, and other/unknown), and health plan capitation. In addition, year of index admission was included in the multivariate models to account for any temporal changes in LOS during the time period.
Clinical variables evaluated during the pre-period included a measure of comorbidity: the Charlson Comorbidity Index (Deyo version) (DCI)22,23. The DCI is a numeric scale based on the presence or absence of specific ICD-9-CM diagnosis codes consistent with 19 conditions, each assigned a weight, with higher scores indicating greater burden. Additional pre-period variables included the number and percentage of patients with specific cardiac-related diagnoses and procedures, with specific comorbidities, and with a hospitalization (any cause), in addition to inflation-adjusted mean overall healthcare expenditures.
Clinical variables evaluated for the index admission included the number and percentage of patients receiving care in specific hospital units such as the intensive care unit (ICU) and critical care unit (CCU) were also determined. In-hospital mortality was identified by a discharge status indicating death.
The LOS outcome variable, measured in days, was determined by subtracting the discharge date from the index date and then adding 1 day to ensure that all admissions were at least 1 day in length. Mean [standard deviation (SD)] and median LOS were reported for all patients as well as separately for those with and without death at discharge. LOS was also reported as a categorical variable centered on median LOS (the percentage of patients with a LOS ≤5 days and LOS>5 days).
Statistical analyses
Descriptive statistics were reported by payer for demographic, co-morbid, and clinical variables in the pre-hospitalization period as well as for index admission (including LOS) characteristics. Because LOS is a skewed variable, the multivariate analyses of factors associated with LOS utilized a generalized linear model (GLM) with a log link and a gamma error distribution. All model fitting was done using SAS version 9.2 (SAS Institute Inc., Cary, NC). Since PROC GENMOD does not have a stepwise regression capability, to perform stepwise regression the forward selection option of PROC GLMSELECT was used with a log transformation of LOS to identify the best fitting model for each of the three databases separately (Commercial, Medicaid, and Medicare). Model fit was assessed by various goodness-of-fit criteria such as adjusted R2, Akaike’s Information Criterion (AIC), and Schwartz’s Bayesian Criterion (SBC). The final model resulting from the stepwise regression was then fitted again using PROC GENMOD.
For ease of understanding the relation between model variables and LOS, results were presented as additional days of LOS above a baseline LOS for a reference ‘low risk’ systolic HF patient for each of the three databases. PROC GENMOD was used to predict the reference LOS for each database, as well as a LOS multiplication factor, or predicted effect size, above this reference for each variable retained in the model. The reference patients were defined as follows: male, 35–49 years old (commercial and Medicaid) or 65–69 years old (Medicare), Caucasian (Medicaid only), urban, Southern region (commercial and Medicare only), fee-for-service and non-capitated health plan, no study comorbidities, ≤10 3-digit ICD-9-CM codes in pre-period, HF DRG, no study inpatient procedures, no ICU or CCU stay, discharged alive. PROC GENMOD also produced the predicted additional days stay (shown in Tables 4–6 as ‘additional days’) from the reference LOS associated with a change in one variable (e.g., ‘no’ to ‘yes’), for a patient with one particular characteristic and all other factors the same as the reference. In addition to tables of additional predicted days, variables with a predicted change in LOS of 0.9 or greater (e.g., 0.9 more or fewer days than the low risk reference group) for at least one payer were highlighted.
Table 4.
Predictors of length of stay: Commercial database.
| Variables | Commercial database (n =4109)
|
|||||
|---|---|---|---|---|---|---|
| Reference category or value Reference* LOS =3.955 days | Multiplication factor | 95% CI
|
Additional days | p-value | ||
| Lower | Upper | |||||
| Demographic variables | ||||||
| Managed care | Fee-for-service | 0.931 | 0.888 | 0.976 | −0.274 | 0.0028 |
| Other/unknown health plan | “ ” | 0.813 | 0.743 | 0.889 | −0.740 | <0.0001 |
| Capitated health plan | Non-capitated | 0.914 | 0.877 | 0.953 | −0.339 | <0.0001 |
| Clinical variables: 12-month pre-period | ||||||
| CABG surgery | None in pre-period | 0.874 | 0.807 | 0.947 | −0.497 | 0.001 |
| Arrhythmias | “ ” | 1.101 | 1.064 | 1.140 | 0.401 | <0.0001 |
| Circulatory disease | “ ” | 1.157 | 1.107 | 1.210 | 0.621 | <0.0001 |
| Atherosclerosis | “ ” | 0.940 | 0.907 | 0.974 | −0.238 | 0.0008 |
| Stroke | “ ” | 1.185 | 1.075 | 1.307 | 0.732 | 0.0006 |
| Cardiorespiratory failure and shock | “ ” | 1.223 | 1.169 | 1.279 | 0.882 | <0.0001 |
| Pneumonia | “ ” | 1.17 | 1.13 | 1.22 | 0.680 | <0.0001 |
| Renal failure | “ ” | 1.273 | 1.217 | 1.331 | 1.079 | <0.0001 |
| Liver disease | “ ” | 1.191 | 1.105 | 1.285 | 0.757 | <0.0001 |
| GI disease or ulcer | “ ” | 1.179 | 1.125 | 1.235 | 0.707 | <0.0001 |
| Cancer | “ ” | 1.148 | 1.085 | 1.215 | 0.585 | <0.0001 |
| Diabetes | “ ” | 1.083 | 1.046 | 1.122 | 0.329 | <0.0001 |
| Malnutrition | “ ” | 1.421 | 1.225 | 1.648 | 1.664 | <0.0001 |
| Pressure/decubitus ulcer | “ ” | 1.344 | 1.232 | 1.466 | 1.360 | <0.0001 |
| Clinical variables: Index admission | ||||||
| Treated in ICU | Not in ICU | 1.109 | 1.071 | 1.149 | 0.431 | <0.0001 |
| Treated in CCU | Not in CCU | 1.083 | 1.040 | 1.126 | 0.326 | <0.0001 |
| ICD or pacemaker | “ ” | 0.833 | 0.781 | 0.889 | −0.660 | <0.0001 |
| CABG procedure | “ ” | 1.682 | 1.450 | 1.951 | 2.695 | <0.0001 |
| Cardiac catheterization | “ ” | 1.438 | 1.357 | 1.525 | 1.734 | <0.0001 |
| Mechanical ventilation procedure | “ ” | 1.201 | 1.055 | 1.367 | 0.794 | 0.0056 |
| Dialysis | “ ” | 1.240 | 1.119 | 1.373 | 0.947 | <0.0001 |
The following variables did not have a significant difference in LOS from the reference group for patients with commercial health insurance: age group, index year, gender, rheumatic heart disease, other heart disease, COPD, fibrosis of the lung, other urinary tract disorder, psychiatric disorder, and electrolyte disorder. Each of these variables was associated with a significant difference in LOS from the corresponding reference group for one of the other payers.
Reference: 2005, male, 35–49 years old, fee-for-service and non-capitated health plan, no study comorbidities, ≤10 3-digit ICD-9-CM codes in pre-period, no study inpatient procedures, no ICU or CCU stay, discharged alive.
Table 6.
Predictors of length of stay: Medicare database.
| Variables | Medicare database (n =11,370)
|
|||||
|---|---|---|---|---|---|---|
| Reference category or value Reference* LOS =4.058 days | Multiplication factor | 95% CI
|
Additional days | p-value | ||
| Lower | Upper | |||||
| Demographic Variables | ||||||
| Age group: <65 | 65–69 | 0.984 | 0.945 | 1.024 | −0.172 | 0.4235 |
| Age group: 70–74 | “ ” | 0.958 | 0.877 | 1.046 | −0.066 | 0.3374 |
| Age group: ≥75 | “ ” | 1.058 | 1.022 | 1.094 | 0.233 | 0.0013 |
| Index year: 2006 | 2005 | 1.033 | 1.006 | 1.062 | 0.134 | 0.0186 |
| Index year: 2007 | “ ” | 0.964 | 0.938 | 0.992 | −0.145 | 0.0108 |
| Index year 2008 | “ ” | 0.965 | 0.936 | 0.994 | −0.144 | 0.0202 |
| Female | Male | 1.075 | 1.053 | 1.098 | 0.304 | <0.0001 |
| Capitated health plan | Non-capitated | 0.870 | 0.843 | 0.898 | −0.526 | <0.0001 |
| Clinical variables: 12-month pre-period | ||||||
| CABG surgery | None in pre-period | 0.862 | 0.816 | 0.909 | −0.562 | <0.0001 |
| Arrhythmias | “ ” | 1.094 | 1.071 | 1.117 | 0.380 | <0.0001 |
| Rheumatic heart disease | “ ” | 1.026 | 1.002 | 1.049 | 0.104 | 0.0305 |
| Circulatory disease | “ ” | 1.132 | 1.103 | 1.162 | 0.535 | <0.0001 |
| Atherosclerosis | “ ” | 0.954 | 0.934 | 0.975 | −0.188 | <0.0001 |
| Other heart disease | “ ” | 1.093 | 1.062 | 1.125 | 0.377 | <0.0001 |
| Stroke | “ ” | 1.132 | 1.078 | 1.189 | 0.535 | <0.0001 |
| Cardiorespiratory failure and shock | “ ” | 1.214 | 1.179 | 1.250 | 0.868 | <0.0001 |
| COPD | “ ” | 1.087 | 1.061 | 1.113 | 0.352 | <0.0001 |
| Pneumonia | “ ” | 1.164 | 1.135 | 1.193 | 0.665 | <0.0001 |
| Fibrosis of the lung | “ ” | 1.205 | 1.152 | 1.261 | 0.832 | <0.0001 |
| Renal failure | “ ” | 1.245 | 1.212 | 1.277 | 0.992 | <0.0001 |
| Other urinary tract disorder | “ ” | 1.116 | 1.080 | 1.152 | 0.470 | <0.0001 |
| Liver disease | “ ” | 1.164 | 1.091 | 1.242 | 0.666 | <0.0001 |
| GI disease or ulcer | “ ” | 1.196 | 1.165 | 1.228 | 0.797 | <0.0001 |
| Cancer | “ ” | 1.068 | 1.036 | 1.101 | 0.275 | <0.0001 |
| Psychiatric disorder | “ ” | 1.125 | 1.086 | 1.165 | 0.506 | <0.0001 |
| Diabetes | “ ” | 1.031 | 1.009 | 1.055 | 0.128 | 0.0069 |
| Malnutrition | “ ” | 1.382 | 1.255 | 1.522 | 1.551 | <0.0001 |
| Electrolyte disorder | “ ” | 1.146 | 1.111 | 1.183 | 0.593 | <0.0001 |
| Pressure/decubitus ulcer | “ ” | 1.207 | 1.144 | 1.272 | 0.838 | <0.0001 |
| Clinical variables: Index admission | ||||||
| ICD or pacemaker | “ ” | 0.844 | 0.806 | 0.884 | −0.632 | <0.0001 |
| CABG procedure | “ ” | 1.925 | 1.714 | 2.162 | 3.754 | <0.0001 |
| Cardiac catheterization | “ ” | 1.234 | 1.181 | 1.290 | 0.950 | <0.0001 |
| Mechanical ventilation procedure | “ ” | 1.378 | 1.256 | 1.511 | 1.533 | <0.0001 |
| Dialysis | “ ” | 1.218 | 1.138 | 1.303 | 0.884 | <0.0001 |
The following variables did not have a significant difference in LOS from the reference group for Medicare eligible beneficiaries: health plan type, capitation status, ICU stay at index admission, and CCU stay at index admission. Each of these variables was associated with a significant difference in LOS from the corresponding reference group for one of the other payers.
Reference: 2005, male, 65–69 years old, urban, fee-for-service and non-capitated health plan, no study comorbidities, ≤10 3-digit ICD-9-CM codes in pre-period, HF DRG, no study inpatient procedures, no ICU or CCU stay, discharged alive.
Results
Demographic characteristics
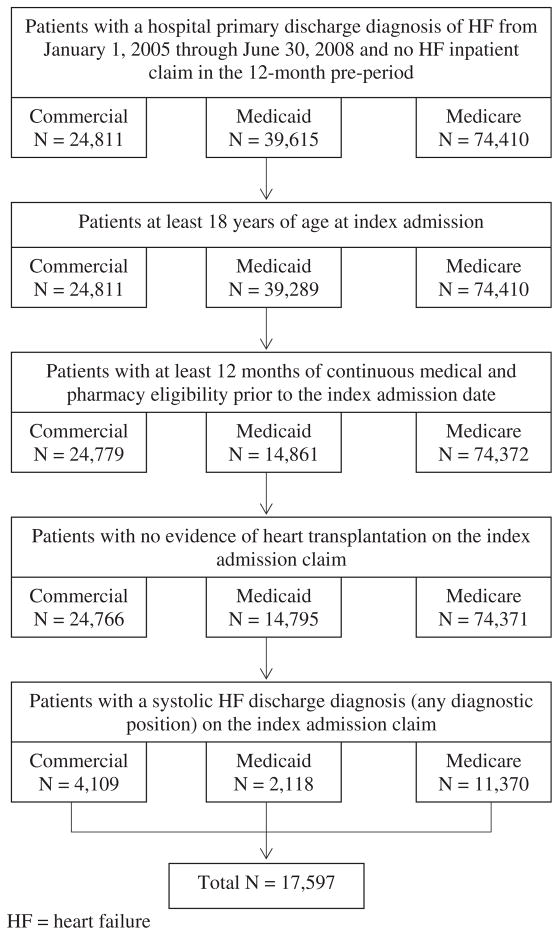
A total of 17,597 patients had a hospitalization for systolic HF from January 1, 2005 through June 6, 2008 and met the selection criteria for age, eligibility, and exclusionary diagnoses (Figure 1). Counts by payer were 4109 patients, 2118 patients, and 11,370 patients for commercial, Medicaid, and Medicare payers, respectively (Table 1). Mean age was 55 years for commercial, 61 for Medicaid, and 79 years for Medicare systolic HF patients. A greater percentage of systolic HF patients were male in the commercial and Medicare payer groups, while the reverse was true in the Medicaid payer group, a finding consistent with the eligibility criteria for Medicaid. Within the commercial payer group 82.3% of systolic HF patients received care under a fee-for-service plan, while in the Medicaid and Medicare payer groups the majority received care under managed care plans (69.9% and 58.0%, respectively).
Figure 1.
Patient attrition.
Table 1.
Demographic characteristics by payer type.
| Characteristic | Commercial database (n =4109) | Medicaid database (n =2118) | Medicare database (n =11,370) | p-value |
|---|---|---|---|---|
| Age (years), M (SD) | 55.4 (7.9) | 61.3 (15.3) | 79.4 (7.8) | <0.001 |
| Gender, n (%) | <0.001 | |||
| Male | 2591 (63.1) | 852 (40.2) | 6144 (54.0) | |
| Female | 1518 (36.9) | 1266 (59.8) | 5226 (46.0) | |
| Insurance plan type, n (%) | <0.001 | |||
| Managed care | 604 (14.7) | 1480 (69.9) | 6590 (58.0) | |
| Fee-for-service | 3383 (82.3) | 637 (30.1) | 4654 (40.9) | |
| Other/unknown | 122 (3.0) | 1 (<0.1) | 126 (1.1) | |
| Health plan capitation, n (%) | <0.001 | |||
| Capitated | 809 (19.7) | 637 (30.1) | 1497 (13.2) | |
| Non-capitated | 3300 (80.3) | 1481 (69.9) | 9873 (86.8) |
Comorbidities
The clinical characteristics of systolic HF patients differed among the three payers. Patients within the Medicaid payer group had higher mean DCI, Elixhauser Index, and more unique 3-digit ICD-9-CM codes in the pre-period than patients in either the commercial or Medicare payers (Table 2). Conditions occurring in at least 25% of systolic HF patients in at least one of the payer groups included renal failure, chronic obstructive pulmonary disease (COPD), pneumonia, diabetes and diabetes mellitus complications, peptic ulcer/hemorrhage/other GI disorders, and disorders of fluid/electrolyte/acid-base, with a greater percentage of Medicaid patients having each of these six conditions compared to the commercial and Medicare payer groups (p<0.001 for all). In only one condition, diabetes and diabetes mellitus complications, was the rate at least 25% in all three of the payer groups. The most commonly occurring cardiovascular-related diagnoses in the pre-period were chronic atherosclerosis, arrhythmias, and valvular and rheumatic heart disease.
Table 2.
Clinical characteristics by payer type.
| Characteristic | Commercial database (n =4109) | Medicaid database (n =2118) | Medicare database (n =11,370) | p-value |
|---|---|---|---|---|
| During 12-month pre-period | ||||
| Comorbidity Indicators, M (SD) | ||||
| Deyo Charlson Comorbidity Index | 2.8 (2.0) | 3.2 (2.0) | 3.1 (2.0) | <0.001 |
| Elixhauser Index | 1.2 (1.5) | 2.7 (1.9) | 0.7 (1.1) | <0.001 |
| Unique 3-digit ICD-9-CM codes | 17.8 (9.8) | 22.4 (11.2) | 19.0 (9.1) | <0.001 |
| Cardiovascular-related diagnoses/procedures, n (%) | ||||
| Coronary artery bypass graft (CABG) | 266 (6.0) | 151 (7.0) | 567 (5.0) | <0.001 |
| Acute coronary syndrome | 692 (17.0) | 306 (14.0) | 1629 (14.0) | <0.001 |
| Arrhythmias | 1545 (38.0) | 783 (37.0) | 5920 (52.0) | <0.001 |
| Cardiorespiratory failure and shock | 767 (19.0) | 493 (23.0) | 1829 (16.0) | <0.001 |
| Valvular and rheumatic heart disease | 1141 (28.0) | 752 (36.0) | 3165 (28.0) | <0.001 |
| Vascular or circulatory disease | 740 (18.0) | 404 (19.0) | 2315 (20.0) | 0.004 |
| Chronic atherosclerosis | 1671 (41.0) | 852 (40.0) | 5169 (45.0) | <0.001 |
| Other and unspecified heart disease | 755 (18.0) | 560 (26.0) | 1665 (15.0) | <0.001 |
| Comorbidities, n (%) | ||||
| Stroke | 119 (3.0) | 94 (4.0) | 516 (5.0) | <0.001 |
| Dialysis | 152 (4.0) | 146 (7.0) | 325 (3.0) | <0.001 |
| Renal failure | 798 (19.0) | 563 (27.0) | 2613 (23.0) | <0.001 |
| Nephritis | 70 (2.0) | 59 (3.0) | 74 (1.0) | <0.001 |
| Other urinary tract disorders | 390 (9.0) | 303 (14.0) | 1371 (12.0) | <0.001 |
| Chronic obstructive pulmonary disease (COPD) | 705 (17.0) | 649 (31.0) | 2677 (24.0) | <0.001 |
| Asthma | 216 (5.0) | 127 (6.0) | 287 (3.0) | <0.001 |
| Pneumonia | 921 (22.0) | 580 (27.0) | 2676 (24.0) | <0.001 |
| Fibrosis of lung and other chronic lung disorders | 226 (6.0) | 127 (6.0) | 621 (5.0) | 0.610 |
| Diabetes and diabetes mellitus complications | 1514 (37.0) | 839 (40.0) | 3531 (31.0) | <0.001 |
| Liver and biliary disease | 211 (5.0) | 130 (6.0) | 287 (3.0) | <0.001 |
| Peptic ulcer, hemorrhage, other GI disorders | 796 (19.4) | 559 (26.4) | 2646 (23.3) | <0.001 |
| Dementia, senility, psychiatric disorders | 392 (9.5) | 357 (1.2) | 1179 (3.7) | <0.001 |
| Drug/alcohol abuse/dependence/psychosis | 377 (9.0) | 346 (16.0) | 155 (1.0) | <0.001 |
| Cancer | 463 (11.3) | 113 (5.3) | 1589 (14.0) | <0.001 |
| Iron deficiency, anemias, hematologic disorders | 648 (15.8) | 431 (20.3) | 2053 (18.1) | <0.001 |
| Hemiplegia, paraplegia, paralysis, functional disability | 65 (2.0) | 77 (4.0) | 190 (2.0) | <0.001 |
| Decubitus ulcer or chronic skin ulcer | 158 (4.0) | 76 (4.0) | 446 (4.0) | 0.762 |
| Protein-calorie malnutrition | 52 (1.0) | 71 (3.0) | 129 (1.0) | <0.001 |
| Disorders of fluid/electrolyte/acid-base | 618 (15.0) | 561 (26.0) | 1450 (13.0) | <0.001 |
| Utilization and Expenditures, n (%) | ||||
| Pre-period hospitalization, all-cause | 957 (23.0) | 489 (23.0) | 2870 (25.0) | 0.012 |
| Overall healthcare expenditures, M (SD) | $23,381 ($50,467) | $16,912 ($30,853) | $17,331 ($32,095) | <0.001 |
| During index admission | ||||
| DRG categories, n (%) | ||||
| Heart failure (HF) and shock | 2090 (51.0) | 1588 (75.0) | 7784 (68.0) | <0.001 |
| Circulatory systems diagnoses | 850 (21.0) | 269 (13.0) | 1115 (10.0) | <0.001 |
| Heart failure-related procedures, n (%) | ||||
| ICD or pacemaker | 486 (12.0) | 148 (7.0) | 917 (8.0) | <0.001 |
| Coronary artery bypass graft (CABG) | 76 (2.0) | 13 (1.0) | 127 (1.0) | <0.001 |
| Cardiac catheterization | 1255 (31.0) | 329 (16.0) | 1514 (13.0) | <0.001 |
| Left ventricular assist device | 7 (<0.1) | 0 (0.0) | 1 (<0.1) | <0.001 |
| Percutaneous coronary intervention/stent | 159 (4.0) | 31 (1.0) | 299 (3.0) | <0.001 |
| Mechanical ventilation | 72 (2.0) | 63 (3.0) | 148 (1.0) | <0.001 |
| Invasive hemodynamic monitoring | 5 (<0.1) | 0 (0.0) | 8 (<0.1) | 0.240 |
| Intra-aortic pump balloon | 59 (1.0) | 10 (<0.1) | 49 (<0.1) | <0.001 |
| Dialysis | 122 (3.0) | 131 (6.0) | 289 (3.0) | <0.001 |
| Hospital care unit, n (%) | ||||
| Intensive Care Unit (ICU) | 1435 (35.0) | 812 (38.0) | 3128 (28.0) | <0.001 |
| Critical Care Unit (CCU) | 949 (23.0) | 590 (28.0) | 1982 (17.0) | <0.001 |
| Telemetry | 187 (5.0) | 120 (6.0) | 478 (4.0) | 0.011 |
| General medicine | 2134 (52.0) | 1262 (60.0) | 4908 (43.0) | <0.001 |
Only about half of all commercially-insured systolic HF patients had HF as the primary DRG upon their index admission, despite HF being the primary ICD-9 diagnosis, while 75% and 68% of systolic HF patients with Medicaid or Medicare payers, respectively, had a HF DRG (Table 2). Circulatory disorders were the next most common DRG, with remaining DRGs primarily representing procedures and complications. The most common non-HF DRGs were for circulatory or respiratory conditions including pneumonia and pleurisy, pulmonary edema and respiratory failure, and chronic obstructive pulmonary disease.
In-hospital events
During the index admission, a higher percentage of commercial systolic HF patients had cardiac catheterization than either Medicaid or Medicare systolic HF patients (31.0%, 16.0%, and 13.0%, respectively; p<0.001) (Table 2). Other inpatient procedures (ICD/pacemaker, coronary artery bypass graft surgery (CABG), left ventricular assist device (LVAD), percutaneous coronary intervention (PCI)/stent) also differed substantially among payers, with highest rates in patients with commercial insurance. Also, a lower percentage of Medicare systolic HF patients spent time in the ICU or CCU, compared to commercial and Medicaid systolic HF patients.
In-hospital death occurred infrequently regardless of payer group (Table 3), although the percentage of Medicaid systolic HF patients who died during the index admission (2.4%) was 4-times the percentage in the commercial payer group (0.6%) and nearly twice the percentage in the Medicare payer group (1.3%) (p<0.001).
Table 3.
Length of stay by payer type and live discharge status.
| Measure | Commercial database (n =4109) | Medicaid database (n =2118) | Medicare database (n =11,370) | p-value |
|---|---|---|---|---|
| LOS, All patients, n (%) | 4109 (100) | 2118 (100) | 11,370 (100) | |
| Mean (SD) | 6.3 (6.2) | 7.1 (7.4) | 6.7 (7.0) | <0.001 |
| Median (IQR) | 5.0 (4.0) | 5.0 (4.0) | 5.0 (4.0) | 1.000 |
| LOS ≤5 days, n (%) | 2412 (58.7) | 1126 (53.2) | 6095 (53.6) | <0.001 |
| LOS >5 days, n (%) | 1697 (41.3) | 992 (46.8) | 5275 (46.4) | <0.001 |
| LOS, Alive at discharge, n (%) | 4086 (99.4) | 2068 (97.6) | 11,224 (98.7) | <0.001 |
| Mean (SD) | 6.2 (5.7) | 6.9 (7.2) | 6.7 (7.0) | <0.001 |
| Median (IQR) | 5.0 (4.0) | 5.0 (4.0) | 5.0 (4.0) | 1.000 |
| LOS ≤5 days, n (%) | 2406 (58.9) | 1110 (53.7) | 6050 (53.9) | <0.001 |
| LOS >5 days, n (%) | 1680 (41.1) | 958 (46.3) | 5174 (46.1) | <0.001 |
| LOS, Death at discharge, n (%) | 23 (0.6) | 50 (2.4) | 146 (1.3) | <0.001 |
| Mean (SD) | 19.4 (31.0) | 12.4 (11.0) | 10.2 (9.6) | <0.001 |
| Median (IQR) | 9.0 (9.0) | 9.5 (11.0) | 7.0 (7.0) | <0.001 |
| LOS ≤5 days, n (%) | 6 (26.1) | 16 (32.0) | 45 (30.8) | 0.001 |
| LOS >5 days, n (%) | 17 (73.9) | 34 (68.0) | 101 (69.2) | <0.001 |
Length of stay
Medicaid systolic HF patients had a longer mean LOS (7.1 days) than either commercial (6.3 days) or Medicare (6.7 days) systolic HF patients (Table 3). Median LOS was the same, regardless of payer type (5 days). A similar pattern for mean and median LOS was observed in the sub-set of patients alive at discharge. However, within the sub-set of patients who died during the index admission, systolic HF patients within the commercial payer group had the longest mean LOS (19.4 days) compared to that of Medicaid (12.4 days) and Medicare (10.2 days) systolic HF patients.
Multivariate predictors of LOS
The adjusted R2 for LOS was 0.294 in the commercial payer model, 0.274 in the Medicaid payer model, and 0.232 in the Medicare payer model. Tables 4–6 present the results of the multivariate predictors of LOS by payer type. Female gender and age were only significant in the Medicare population; no demographic variables were significant in Medicaid or commercially insured patients. Several comorbidities in the 12-month pre-period also had a significant association with LOS. Presence of renal failure was associated with 1.08, 1.43, and 0.99 additional days LOS in commercial, Medicaid, and Medicare payer patients, respectively. Cardiorespiratory failure and shock was associated with 0.88, 0.43, and 0.87 additional days LOS in commercial, Medicaid, and Medicare payer patients, respectively. Indicators of frailty or disability were also associated with longer LOS.
Malnutrition was associated with additional days LOS of 1.66 and 1.55 in the commercial and Medicare payer patients, respectively. A history of pressure or decubitus ulcers was associated with increased LOS by 1.36 days in commercial systolic HF patients and 0.84 days in Medicare systolic HF patients. Saturated model results by payer, which include all demographic and clinical variables used in the multivariate analyses, are available as supplemental materials in Tables S1–S3.
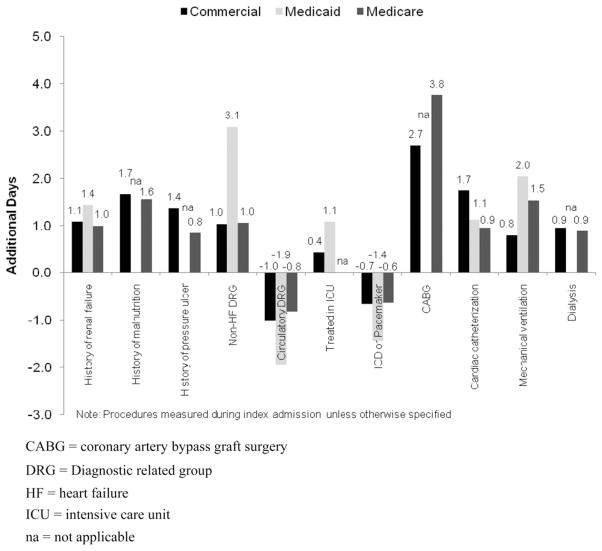
The statistical models identified inpatient procedures during the index admission as being associated with the greatest increases in LOS (Figure 2), although the direction and magnitude of association was dependent on the procedure type, procedure timing, and payer type. For example, CABG during the index hospitalization was associated with an increase in LOS by as much as 3.75 days among Medicare patients following adjustment for other factors. In contrast, LOS was approximately half a day shorter among Medicare patients with CABG in the pre-period vs those without it. Cardiac catheterization was associated with a range of 0.95–1.73 additional days LOS across payer types. Conversely, receipt of an implantable cardioverter defibrillator (ICD) or pacemaker was associated with 0.63–1.44 fewer days LOS, depending on the payer. Initiation of mechanical ventilation was associated with 0.79–2.04 additional days LOS.
Figure 2.
Model predicted additional days by payer type.
A circulatory DRG at index admission was associated with a decreased LOS of 1.02, 1.94, and 0.81 fewer days for commercial, Medicaid, and Medicare systolic HF patients, respectively. Patients who had a HF DRG at index admission had a shorter LOS compared to patients with a non-HF DRG: 1.03 fewer days for commercial payer patients, 3.09 fewer days for Medicaid payer patients, and 1.04 fewer days for Medicare payer patients.
Discussion
This study of the inpatient experience during hospitalization for systolic HF identified important differences among payer types, including disease burden, care received, LOS, and mortality. Overall, renal failure, pressure ulcer, malnutrition, non-circulatory DRG, receipt of a CABG procedure or cardiac catheterization, or need for mechanical ventilation during the index admission were most significantly associated with increased LOS. Receipt of an ICD or pacemaker at index was the variable most strongly associated with a decreased LOS, which may be due to the likelihood that these were scheduled elective procedures despite a primary discharge diagnosis of HF. These models derived from administrative claims-based data had a modest predictive capacity for LOS, with adjusted R2 ranging from 0.232–0.294. The longest LOS across all payer types was seen in patients who ultimately died during hospitalization, further highlighting the need for advanced and/or novel therapies for sicker patients, or early involvement of palliative care and hospice when appropriate.
These findings complement and extend other predictors of LOS and descriptions of HF hospitalization by payer type. The most comprehensive existing information comes from data on nearly 100,000 patients hospitalized between 2005–2009 at hospitals participating in the GWTG-HF quality improvement initiative4,7. Although LOS risk models were developed in GWTG-HF, they were not developed by payer type and do not provide estimates of additional days of hospitalization, as performed in our study. The median LOS of 4 days in GWTG-HF4 was slightly shorter than seen in our data. Higher numbers of comorbidities, including renal impairment, cardiac and respiratory conditions, and diabetes, were associated with increased LOS, while performance of fewer procedures during the hospital stay was associated with decreased LOS. Not surprisingly, other studies have shown similar increases in LOS for patients with greater comorbidity and undergoing non-elective procedures6,12–14.
The MarketScan databases-derived models presented here have important advantages over these prior data. Our data quantify the days added to LOS for specific comorbidities, DRG codes, and various procedures among this broad US systolic HF population of 17,597 patients representing commercial, Medicaid, and Medicare payers. The R2 values here are notably higher than the R2 of 0.048 identified in the GWTG-HF LOS model4. Our restriction to those patients with a diagnosis of systolic HF, while truncating sample size and generalizability to the wider HF population, reduces the variability found in the overall HF population without limiting diversity resulting from disease severity or treatment. This is likely to explain a portion of our superior model performance, despite reliance on administrative data. Many guideline-indicated HF therapies are confined to those with reduced LVEF (i.e., systolic HF)24–26, potentially increasing the value of early risk stratification in this HF sub-group. Therefore, our focus on patients with systolic HF provides a clearer understanding of differences in inpatient care, LOS, and in-hospital mortality among those very patients most likely to benefit from HF-targeted care decisions.
Except for the oldest age group in the Medicare cohort (age≥ 75 years in Medicare was associated with a modest 0.233 additional days LOS), age was not a significant predictor of LOS. Similarly, Medicare-insured females had a modestly longer LOS than males (predicted 0.304 additional days), and otherwise gender was not identified as a predictor of LOS in the commercial or Medicaid databases. These findings indicate that LOS is dictated by disease severity, comorbidities, and inpatient procedures to a much greater extent than usual demographic measures.
Ultimately, our model, like others, had only modest predictive capacity for LOS. This is likely due to a variety of reasons. LOS, like readmission, appears to be more difficult to predict than mortality27. This may be due to failure to include those factors most closely associated with LOS in the model, such as symptomatology and social factors. It may also be that determinants of LOS are inherently more stochastic than the clinical course leading up to death. LOS is also more subjectively determined than death. Criteria for hospital discharge are multiple and not rigidly defined. The continental differences between HF LOS illustrate this point15,16.
To derive our models we used both variables that can be assessed at the time of admission as well as inpatient events. Inpatient events—procedures, transfer to critical care, or even death—that are strongly associated with LOS may help our understanding of what determines LOS. However, it should be noted that inpatient events, and predictive models that use such variables, may be less helpful than variables present on admission for clinicians, nurses, case managers, and administrators who may be trying to triage patients to an appropriate intensity of care early in the hospital course.
Comparisons among payer type provide important insights into these distinct US systolic HF patient populations. Although different in study design, the findings of this study regarding the inpatient experience for systolic HF patients are similar to those in GWTG-HF of a broader HF cohort7 in that patients with Medicaid, followed by Medicare, were less likely to receive a variety of inpatient medications and procedures than those with commercial insurance. For example, in our study, rates of ICD/pacemaker, CABG, cardiac catheterization, and PCI/coronary stent were up to twice as high among commercially-insured patients than among patients with Medicaid or Medicare. Very rare procedures including left ventricular assist device, invasive hemodynamic monitoring, and intra-aortic pump balloon also were more common among commercially-insured than Medicare or Medicaid beneficiaries. In our analyses Medicaid patients had the highest comorbidity burden, longest LOS, and the highest rate of mortality. In GWTG-HF, Medicare, followed by Medicaid, patients had the greatest comorbidities and longest LOS, while, as in our study, in-hospital mortality was highest for those with Medicaid7. Among commercially-insured patients in our study, those with managed care plans had 0.274 days shorter hospital stay than those with fee-for-service plans. These differences raise questions regarding financial influences on treatment choices for patients among various payer types. In our study, models of LOS differed by payer type, but this may have been more a function of sample size and collinearity rather than actual differences in determinants of LOS among patients with different payer types.
Several additional limitations to the study should be noted. First, this was a retrospective, observational study based on administrative claims data, and therefore selection of patients with systolic HF is limited by completeness and accuracy of medical coding. Patients coded with ICD-9-CM 428.0 ‘Congestive heart failure, unspecified’, even if they had reduced LVEF, would have been excluded from the analysis. However, selection of patients was based on primary hospital discharge diagnosis codes which have been shown to have good specificity and positive predictive value for HF28. Second, this study purposely focused on systolic HF in the US and thus is not generalizable to patients with diastolic HF or to international populations. Third, management, particularly outpatient and inpatient drug therapy, was not assessed. Therefore, the extent to which prescribing patterns are associated with characteristics of hospitalization and LOS is not examined in this study. Finally, the Medicare population in this study is for patients with employer-paid Medicare supplemental insurance, and the Medicaid population was not representative of the entire US Medicaid population. Therefore, the results are not generalizable to the overall US Medicare or Medicaid populations.
Conclusion
Our study identified notable differences in the inpatient experience across payer types (including disease burden, care received, LOS, and mortality) that warrant further consideration, which supports the results found in recent work. Presence of comorbidity and receipt of inpatient procedures had the greatest impact on LOS for patients with systolic HF hospitalizations for all payer types. These findings may refine risk stratification for the hospitalized systolic HF population, allowing for improved targeting of intensive inpatient management and/or aggressive transitional care designed to improve outcomes and increase the efficiency of care.
Supplementary Material
Table 5.
Predictors of length of stay: Medicaid database.
| Variables | Medicaid database (n =2118)
|
|||||
|---|---|---|---|---|---|---|
| Reference category or value Reference* LOS =3.837 days | Multiplication factor | 95% CI
|
Additional days | p-value | ||
| Lower | Upper | |||||
| Clinical variables: 12-month pre-period | ||||||
| Arrhythmias | “ ” | 1.122 | 1.067 | 1.180 | 0.468 | <0.0001 |
| Rheumatic heart disease | “ ” | 1.082 | 1.030 | 1.137 | 0.314 | 0.0018 |
| Circulatory disease | “ ” | 1.155 | 1.086 | 1.228 | 0.594 | <0.0001 |
| Cardiorespiratory failure and shock | “ ” | 1.112 | 1.044 | 1.183 | 0.428 | 0.0009 |
| COPD | “ ” | 1.100 | 1.044 | 1.159 | 0.383 | 0.0003 |
| Pneumonia | “ ” | 1.103 | 1.044 | 1.165 | 0.394 | 0.0005 |
| Renal failure | “ ” | 1.374 | 1.299 | 1.452 | 1.434 | <0.0001 |
| GI disease or ulcer | “ ” | 1.137 | 1.073 | 1.204 | 0.525 | <0.0001 |
| Electrolyte disorder | “ ” | 1.116 | 1.056 | 1.180 | 0.445 | 0.0001 |
| Clinical variables: Index admission | ||||||
| Treated in ICU | Not in ICU | 1.281 | 1.217 | 1.348 | 1.078 | <0.0001 |
| Treated in CCU | Not in CCU | 1.097 | 1.039 | 1.158 | 0.370 | 0.0008 |
| ICD or pacemaker | “ ” | 0.624 | 0.543 | 0.718 | −1.442 | <0.0001 |
| Cardiac catheterization | “ ” | 1.292 | 1.162 | 1.437 | 1.121 | <0.0001 |
| Mechanical ventilation procedure | “ ” | 1.532 | 1.324 | 1.774 | 2.043 | <0.0001 |
The following variables did not have a significant difference in LOS from the reference group for Medicaid eligible beneficiaries: age group, index year, gender, urbanization, plan type, capitation status, previous CABG surgery, atherosclerosis, other heart disease, stroke, fibrosis of the lung, other urinary tract disorder, liver disease, cancer, psychiatric disorder, diabetes, malnutrition, pressure/decubitus ulcer, index admission CABG surgery, and index admission dialysis. Each of these variables was associated with a significant difference in LOS from the corresponding reference group for one of the other payers.
Reference: 2005, male, 35–49 years old, fee-for-service and non-capitated health plan, no study comorbidities, ≤10 3-digit ICD-9-CM codes in pre-period, HF DRG, no study inpatient procedures, no ICU or CCU stay, discharged alive.
Acknowledgments
We gratefully acknowledge the programming assistance of Kelly Oh and Chandrasekar Balakrishnan of Truven Health Analytics, formerly of Thompson Reuters, and the input on the initial study concept from Matthew Gitlin of Amgen, Inc. and William Padula of University of Colorado, in addition to Michele Shaw of Naples, FL for her medical writing expertise.
Footnotes
Transparency
Declaration of funding
Funding for this project was provided by Amgen, Inc.
Declaration of financial/other relationships
LAA was a consultant hired by Amgen and Johnson and Johnson, and has received grant funding from NIH, NHLBI, and K23 of the National Cancer Institute. KST is a former employee of Thompson Reuters, and has received funding from Amgen. KLW and DMS are current employees of Truven Health Analytics, formerly of Thompson Reuters, which was contracted by Amgen to work in collaboration on this study. IA is an employee and stockholder of Amgen, Inc.
The peer reviewers on this manuscript have disclosed that they have no relevant financial relationships.
Contributor Information
Larry A. Allen, Section of Advanced Heart Failure and Transplantation, University of Colorado Anschutz Medical Campus, Aurora, CO, USA
Karen E. Smoyer Tomic, Oxford PharmaGenesis Inc., Newtown, PA, USA
Kathleen L. Wilson, Truven Health Analytics Inc., Washington, DC, USA
David M. Smith, Truven Health Analytics Inc., Washington, DC, USA
Irene Agodoa, Amgen, Inc., Thousand Oaks, CA, USA.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. NEJM. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 3.Whellan DJ, Greiner MA, Schulman KA, et al. Costs of inpatient care among Medicare beneficiaries with heart failure, 2001 to 2004. Circ Cardiovasc Qual Outcomes. 2010;3:33–40. doi: 10.1161/CIRCOUTCOMES.109.854760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whellan DJ, Zhao X, Hernandez AF, et al. Predictors of hospital length of stay in heart failure: findings from get with the guidelines. J Card Fail. 2011;17:649–56. doi: 10.1016/j.cardfail.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Adams KF, Jr, Fonarow GC, Emerman CL, et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE) Am Heart J. 2005;149:209–16. doi: 10.1016/j.ahj.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 6.Hauptman PJ, Swindle J, Burroughs TE, et al. Resource utilization in patients hospitalized with heart failure: insights from a contemporary national hospital database. Am Heart J. 2008;155:978–85.e1. doi: 10.1016/j.ahj.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 7.Kapoor JR, Kapoor R, Hellkamp AS, et al. Payment source, quality of care, and outcomes in patients hospitalized with heart failure. J Am Coll Cardiol. 2011;58:1465–71. doi: 10.1016/j.jacc.2011.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stock GN, McDermott C. Operational and contextual drivers of hospital costs. J Health Organ Mana. 2011;25:142–58. doi: 10.1108/14777261111134392. [DOI] [PubMed] [Google Scholar]
- 9.Krantz MJ, Tanner J, Horwich TB, et al. Get With the Guidelines Steering Committee and Hospitals Influence of hospital length of stay for heart failure on quality of care. Am J Cardiol. 2008;102:1693–7. doi: 10.1016/j.amjcard.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 10.van Walraven C, Dhalla IA, Bell C, et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ. 2010;182:551–7. doi: 10.1503/cmaj.091117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010;303:2141–7. doi: 10.1001/jama.2010.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Formiga F, Chivite D, Manito N. Admission characteristics predicting longer length of stay among elderly patients hospitalized for decompensated heart failure. Eur J Intern Med. 2008;19:198–202. doi: 10.1016/j.ejim.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 13.Philbin EF, Rocco TA, Jr, Lynch LJ, et al. Predictors and determinants of hospital length of stay in congestive heart failure in ten community hospitals. J Heart Lung Transplant. 1997;16:548–55. [PubMed] [Google Scholar]
- 14.Wright SP, Verouhis D, Gamble G, et al. Factors influencing the length of hospital stay of patients with heart failure. Eur J Heart Fail. 2003;5:201–9. doi: 10.1016/s1388-9842(02)00201-5. [DOI] [PubMed] [Google Scholar]
- 15.Blair JE, Zannad F, Konstam MA, et al. Continental differences in clinical characteristics, management, and outcomes in patients hospitalized with worsening heart failure results from the EVEREST (Efficacy of Vasopressin Antagonism in Heart Failure: Outcome Study with Tolvaptan) program. J Am Coll Cardio. 2008;52:1640–8. doi: 10.1016/j.jacc.2008.07.056. [DOI] [PubMed] [Google Scholar]
- 16.Nieminen MS, Brutsaert D, Dickstein K, et al. EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J. 2006;27:2725–36. doi: 10.1093/eurheartj/ehl193. [DOI] [PubMed] [Google Scholar]
- 17.Paulus WJ, Tschöpe C, Sanderson JE, et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J. 2007;28:2539–50. doi: 10.1093/eurheartj/ehm037. [DOI] [PubMed] [Google Scholar]
- 18.Paulus WJ, van Ballegoij JJ. Treatment of heart failure with normal ejection fraction: an inconvenient truth. J Am Coll Cardiol. 2010;55:526–37. doi: 10.1016/j.jacc.2009.06.067. [DOI] [PubMed] [Google Scholar]
- 19.Li Q, Glynn RJ, Dreyer NA, et al. Validity of claims-based definitions of left ventricular systolic dysfunction in Medicare patients. Pharmacoepidemiol Drug Saf. 2011;20:700–8. doi: 10.1002/pds.2146. [DOI] [PubMed] [Google Scholar]
- 20.Keenan PS, Normand SL, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 21.Ross JS, Chen J, Lin Z, et al. Recent national trends in readmission rates after heart failure hospitalization. Circ Heart Fail. 2010;3:97–103. doi: 10.1161/CIRCHEARTFAILURE.109.885210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 23.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Eur J Heart Fail. 2008;10:933–89. doi: 10.1016/j.ejheart.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 25.Hunt SA, Abraham WT, Chin MH, et al. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009;119:e391–479. doi: 10.1161/CIRCULATIONAHA.109.192065. [DOI] [PubMed] [Google Scholar]
- 26.Lindenfeld J, Albert NM, et al. Heart Failure Society of America. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010;16:e1–194. [Google Scholar]
- 27.Amarasingham R, Moore BJ, Tabak YP, et al. An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical record data. Med Care. 2010;48:981–8. doi: 10.1097/MLR.0b013e3181ef60d9. [DOI] [PubMed] [Google Scholar]
- 28.Go AS, Lee WY, Yang J, et al. Statin therapy and risks for death and hospitalization in chronic heart failure. JAMA. 2006;296:2105–11. doi: 10.1001/jama.296.17.2105. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.