Abstract
In the study reported here, we examined posttraumatic stress disorder (PTSD) symptoms in 746 Danish soldiers measured on five occasions before, during, and after deployment to Afghanistan. Using latent class growth analysis, we identified six trajectories of change in PTSD symptoms. Two resilient trajectories had low levels across all five times, and a new-onset trajectory started low and showed a marked increase of PTSD symptoms. Three temporary-benefit trajectories, not previously described in the literature, showed decreases in PTSD symptoms during (or immediately after) deployment, followed by increases after return from deployment. Predeployment emotional problems and predeployment traumas, especially childhood adversities, were predictors for inclusion in the nonresilient trajectories, whereas deployment-related stress was not. These findings challenge standard views of PTSD in two ways. First, they show that factors other than immediately preceding stressors are critical for PTSD development, with childhood adversities being central. Second, they demonstrate that the development of PTSD symptoms shows heterogeneity, which indicates the need for multiple measurements to understand PTSD and identify people in need of treatment.
Keywords: individual differences, posttraumatic stress disorder, war, child abuse
Soldiers deployed to service in war zones experience many situations involving danger to their lives and potential injury, which may lead to posttraumatic stress disorder (PTSD). Still, the majority of soldiers (ranging from 76% to 98% across different studies and wars) returns from service without PTSD (Magruder & Yeager, 2009).
The main cause of deployment-related PTSD is commonly assumed to be exposure to combat and war atrocities (such as witnessing aggression against civilians). Following this view, soldiers with more exposure to combat (e.g., more episodes involving firefights with perceived life threat) and war atrocities are more likely to develop PTSD than soldiers with less combat experience are. The symptoms are assumed to follow a homogeneous pattern across individuals: For those who develop PTSD, the symptoms will show shortly after the traumatic event and persist over time. Other individuals will show resilience by never developing symptoms or by manifesting rapidly decreasing symptom severity.
Testing this understanding requires a tracking of symptom severity at multiple occasions before, during, and after deployment in war zones. However, in spite of 30 years of PTSD research, such data do not exist for combat soldiers. We provide them here for the first time for a population of Danish combat soldiers deployed to Afghanistan. We measured the level of PTSD symptoms at five points before, during, and after deployment. This number of measurements is unique in the literature. Our findings challenge two important and interrelated assumptions in PTSD research. One is the assumption that an immediately preceding traumatic event is the causal factor in PTSD development. The other is the assumption of homogeneity in the development of PTSD symptoms after a stressful event.
The Assumption of a Recent Traumatic Event as the Cause for PTSD Symptoms
According to the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM–IV; American Psychiatric Association, 2000), PTSD is preceded by a stressful event involving life danger and intense fear, horror, and helplessness. Numerous studies have shown that traumatic events are indeed often followed by PTSD symptoms (see McNally, 2003). At the same time, several studies suggest that certain predisposing factors render some individuals more vulnerable than others to the development of PTSD (Brewin, Andrews, & Valentine, 2000; Ozer, Best, Lipsey, & Weiss, 2003) and that the memory of the event rather than the event per se may be the main cause of the symptoms (Rubin, Berntsen, & Bohni, 2008). However, because traumatic events usually come unexpectedly, most studies have no measurements of PTSD symptoms and potential predisposing factors before the traumatic event and thus suffer from a baseline problem.
In contrast to most other victims of trauma, combat soldiers are expected to be exposed to stressful events (i.e., military deployment to war zones is likely to involve episodes with life danger and fear). Therefore, combat soldiers can be used as a test for many assumptions associated with PTSD that otherwise would be hard to examine because of the generally unforeseen nature of traumatic events. Early studies of combat-related PTSD did not include predeployment measures, often because the deployment predated the diagnosis (e.g., Beckham, Feldman, & Kirby, 1998). A few more recent studies have addressed this baseline problem either by comparing PTSD symptoms in deployed versus nondeployed soldiers (Fear et al., 2010; Hoge et al., 2004; Smith, Ryan, et al., 2008; Vasterling et al., 2010) or by comparing symptoms measured before deployment with PTSD symptoms measured after return from deployment (Engelhard et al., 2007; Polusny et al., 2011; Rona et al., 2009; Smith, Ryan, et al., 2008; Vasterling et al., 2010).
The goal of such studies has been to identify new onsets of PTSD (i.e., cases with PTSD after, but not before, deployment) and their possible predictors. Many of these studies have found deployment and self-reported combat exposure to be associated with increased levels of PTSD symptoms after deployment (Polusny et al., 2011; Rona et al., 2009; Smith, Ryan, et al., 2008; Vasterling et al., 2010), but not all studies have found this relationship (Fear et al., 2010), and only a limited range of potential risk factors have been measured. For example, only a few studies have included measures of early traumatic events, such as childhood abuse (Polusny et al., 2011).
The Assumption of Homogeneity in the Development of PTSD Symptoms
It is generally assumed that the development of PTSD shows the same relatively homogeneous pattern across individuals: Those who develop PTSD will show elevated levels of symptoms immediately after the traumatic event, and these symptoms will persist over time. Other individuals will show resilience by never, or only temporarily, developing symptoms (Horowitz, 1986).
Although a few studies have challenged this view by showing heterogeneity in the pattern of symptom development (for a review, see Bonanno, Westphal, & Mancini, 2011), the assumption of homogeneity generally goes unchallenged because testing it requires data from several occasions of measurements, which most studies do not have. This limitation also applies to studies of deployment-related PTSD with predeployment measurements. Although these studies are a major improvement over studies with no baseline PTSD measures, most include only one pre- and one postdeployment measure. This means that possible heterogeneity in PTSD development cannot be considered, although heterogeneity has been found in U.S. soldiers deployed to peacekeeping missions (Dickstein, Suvak, Litz, & Adler, 2010) and in U.S. military service members deployed to Afghanistan and Iraq (Bonanno et al., 2012). It also means that variations in symptom levels during and after deployment are usually not analyzed, for which reason at least some cases identified as new onsets of PTSD may reflect a temporary increase in symptoms rather than actual new cases. In other words, the identification of new-onset cases may vary as a function of when postdeployment measures are taken (Andrews, Brewin, Stewart, Philpott, & Heidenberg, 2009; Gray, Bolton, & Litz, 2004). Studies with only two measurements are, of course, also unable to show curvilinear trajectories in the development of PTSD symptoms.
In the present study, we addressed these limitations in several important ways. We measured PTSD symptoms in a team of soldiers deployed to Afghanistan at five different time points before, during, and after deployment. We employed latent class growth modeling (Muthén & Muthén, 2000; Nagin & Land, 1993) to empirically determine statistically distinct trajectories of change in PTSD symptoms over the five times. This allowed us to identify resilient versus nonresilient groups of soldiers and to identify specific patterns of nonresilient PTSD developments. Furthermore, we measured a wide range of relevant risk factors, with which we predicted membership in six groups representing reliably different developmental trajectories.
Method
Analysis sample and study design
The entire team of 746 Danish soldiers belonging to the Danish Contingent of the International Security Assistance Force 7 was asked to answer questionnaires addressing PTSD and measures of health and risk factors on five occasions related to a 6-month deployment to Afghanistan in 2009: before deployment, during deployment, 1 to 3 weeks after return from deployment, 2 to 4 months (~3 months) after return from deployment, and 7 to 8 months (~7 months) after return from deployment.1
We estimated trajectories characterizing the severity of PTSD symptoms from prior to deployment to at least 3 months after return from deployment to allow for the possibility of nonlinearity. We required at least three total scores from the Posttraumatic Stress Disorder Checklist (PCL; Blanchard, Jones-Alezander, Buckley, & Forneris, 1996) at separate assessments. Specifically, to be retained in the analysis sample, respondents must have provided data at the predeployment assessment, at either the deployment or the return assessment, and at one of the assessments that took place several months after return (3 months or 7 months).
Of the 746 respondents who provided data on at least one occasion, 144 (19%) did not provide PCL data at the predeployment assessment and were therefore excluded from the growth analyses. An additional 235 (32%) did not provide PCL data at both assessments during and immediately after deployment or at both assessments following their return home (of these, 37 were not deployed and thus only answered the predeployment assessment; 2 were killed; 2 were injured during combat; 6 were injured during work, during leisure activities, or in traffic accidents; 5 were repatriated for psychological reasons; and 11 were repatriated for other, unknown reasons). The predeployment PCL score for 1 of the remaining respondents was exceptionally high, and this case was thus removed. This left a final analysis sample of 366 soldiers (342 males, 24 females; mean age = 26.59 years) for whom PCL scores were available prior to deployment, during their tour in Afghanistan, and after their return home (Fig. 1). PCL scores from all five assessments were available for 125 respondents.
Fig. 1.
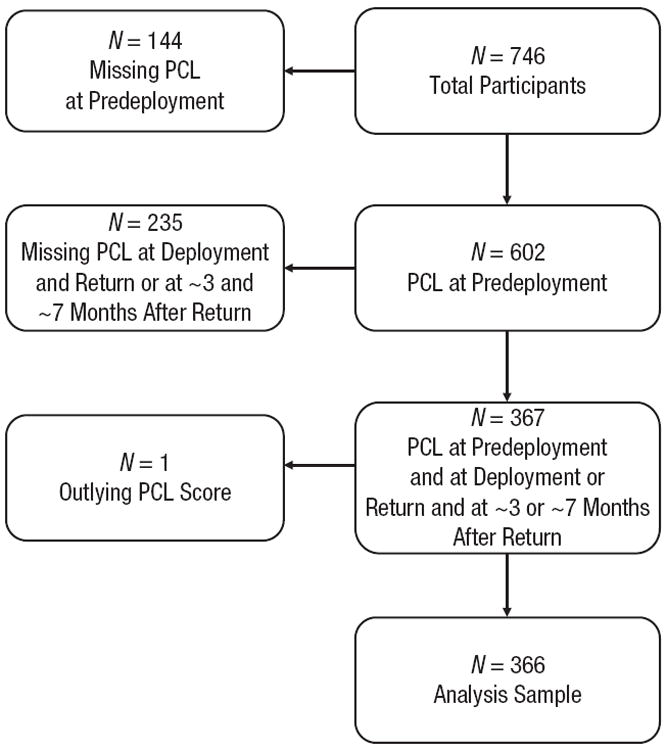
Flowchart showing attrition of the total sample through the five measurement occasions. PCL = Posttraumatic Stress Disorder Checklist (Blanchard, Jones-Alezander, Buckley, & Forneris, 1996).
Procedure and materials
Data for the predeployment assessment were collected by military psychologists 5 to 6 weeks before deployment during group sessions at a military camp in Denmark. The soldiers were informed about the study, including the fact that their responses were anonymous, would not be accessed by their leaders in the military, and would be used for research purposes only. Data for the deployment assessment were collected in Afghanistan. All respondents had been deployed for at least 2 and less than 5 months when they answered this set of questionnaires. The questionnaires were handed out by military personnel at Camp Bastion, Kabul International Airport, or Kandahar Airfield before the soldiers went home on leave. The soldiers submitted their answers in closed envelopes in secured (locked) mailboxes. The locked mailboxes were transported to the research team in Denmark.
The data for the return assessment were collected at a standard homecoming meeting organized by military psychologists and physicians. This data collection took place 1 to 3 weeks after the soldiers returned from deployment. The data for the 3-month follow-up assessment were collected at different military camps in Denmark or through the mail for those who had returned to civilian life. The data for the 7-month follow-up assessment were all collected through the mail as part of a routine survey of the soldiers. All respondents contacted by mail received two cinema tickets for their participation.
Soldiers were required to enter their personal identification number on the front page of the questionnaires so they could be tracked across the five waves of data collections. At each wave, they were informed that this page would be separated from their responses, not entered in the data base, and not stored with their responses. They were also assured that their responses would be accessed only by the research team.
The assessments included many measures, of which only some are relevant to the present analyses. These measures included the civilian version of the PCL (Blanchard et al., 1996); the second edition of the Beck Depression Inventory (BDI-II; Beck, Steer, & Brown, 1996); the scale for Neuroticism derived from the NEO Five Factor Inventory (Costa & McCrae, 1989); the Traumatic Life Event Questionnaire (TLEQ; Kubany et al., 2000), with 20 items accommodated to a population of Danish soldiers; the Combat Exposure Scale (Keane et al., 1989); and a Danger/Injury Exposure Scale constructed by the Danish military for the present and similar studies. The latter scale consists of 10 items measuring the degree of perceived war-zone stress but not the stress of direct combat.
In addition, we also included five single-item measures: earlier emotional problems addressed whether each soldier had previously received psychological or psychiatric treatment for any personal problems (1 = yes, 0 = no), emotional stress measured how often he or she had experienced emotionally stressful situations during deployment (on a scale from 1, never, to 4, very often), times when life was in danger measured the frequency with which the soldier felt that his or her own life was in direct danger or witnessed another’s life being in direct danger (on a scale from 0, never, to 6, more than five times), wounded-injured addressed whether the soldier was wounded or injured during deployment (1 = yes, 0 = no), and killed an enemy addressed whether the soldier killed an enemy combatant during deployment (1 = yes, 0 = no; see the Supplemental Material available online for additional information about all dependent variables).
Latent class growth modeling
The analysis sample differed only slightly from the sample of individuals excluded from the analysis by being slightly less extraverted and including more females. Only a few differences were found between individuals with complete data and those for whom one or more values would be imputed in the statistical modeling. There were no differences in PCL scores. We sorted the sample into the nine possible patterns of missingness and compared means or frequencies on 56 variables ranging from demographic characteristics to prior experiences of trauma to basic personality traits. These comparisons yielded 15 small but significant differences. These variables were included as auxiliary variables in the growth models to increase the likelihood that any systematic missingness could be treated as ignorable (Graham, 2003; see the Supplemental Material for additional information about the modeling procedure and details about estimating missing data).
We used latent class growth analysis to model trajectories of PTSD symptoms from predeployment to approximately 7 months after return from deployment (Kreuter & Muthén, 2007). We used full-information maximum likelihood estimation for all models. All models included auxiliary variables (see the Supplemental Material). We included linear and quadratic terms, and we estimated models assuming 1 to 10 classes. Fit indices associated with these models are shown in Table 1.
Table 1.
Fit Indices for the Estimated Growth Mixture Models
| Number of classes | Log likelihood | Akaike information criterion (AIC) | Bayesian information criterion (BIC) | Sample-size-adjusted Bayesian information criterion (BICSSA) |
|---|---|---|---|---|
| 1 | −5,104.52 | 10,225.65 | 10,256.87 | 10,231.49 |
| 2 | −4,833.80 | 9,691.60 | 9,738.43 | 9,700.36 |
| 3 | −4,749.40 | 9,530.81 | 9,593.25 | 9,542.49 |
| 4 | −4,687.64 | 9,415.28 | 9,493.33 | 9,429.88 |
| 5 | −4,653.92 | 9,355.84 | 9,449.50 | 9,373.36 |
| 6 | −4,625.35 | 9,306.70 | 9,415.97 | 9,327.14 |
| 7 | −4,601.09 | 9,266.19 | 9,391.07 | 9,289.55 |
| 8 | −4,595.31 | 9,262.62 | 9,403.12 | 9,288.90 |
| 9 | −4,563.08 | 9,206.16 | 9,362.27 | 9,235.36 |
| 10 | −4,571.58 | 9,231.16 | 9,402.87 | 9,263.28 |
Note: N = 366.
Simulation studies suggest that the sample-sized-adjusted Bayesian information criterion (BICSSA) performs best in terms of model selection based purely on statistical information. As Table 1 shows, the values of the BICSSA favored a model with 9 classes (as indicated by the increase for a model with 10 classes). Examination of the fitted curves and distribution of respondents across classes for this model suggested that it was not ideal, with some curves differing only slightly and membership in some classes being very low. We examined more closely the results of models with fewer classes, focusing specifically on models with between 5 and 8 classes. Ultimately, we selected a model with 6 classes, which balanced fit, interpretability, and distribution of respondents. The entropy value of this model was .91, which suggests good classification (i.e., probability near 1.0 for assignment to the most probable class and near 0 for assignment to other classes; see the Supplemental Material).
Results
Using latent class growth modeling, we classified the analysis sample into six groups based on their PTSD-symptom trajectories (see Fig. 2). The majority of the sample (n = 306, or 84%) fell into two resilient groups (the resilient and extremely resilient groups) showing low levels of PTSD symptoms with no change over the five measurement times. The other four groups deviated from the resilient groups in unique ways. We identified a new-onset group showing few PTSD symptoms at predeployment and deployment, after which symptom levels increased considerably up to those normally consistent with a diagnosis of PTSD approximately 7 months after returning from deployment. The remaining three groups all showed temporary beneficial effects associated with deployment: All had high or moderate levels of PTSD symptoms at predeployment, but these levels decreased either at deployment, return from deployment, or approximately 3 months after return from deployment. We refer to these groups as the strong-benefit, mild-benefit, and late-benefit groups, according to the time or the level at which the decrease was greatest (see Fig. 2, lower panel). The overall pattern was more pronounced in the strong-benefit group than in the mild-benefit group (which showed the same pattern in a milder form) and in the late-benefit group (which showed a later onset of the beneficial effect). For all three benefit groups, the level of PTSD symptoms increased again after 3 or 7 months following return from deployment.
Fig. 2.
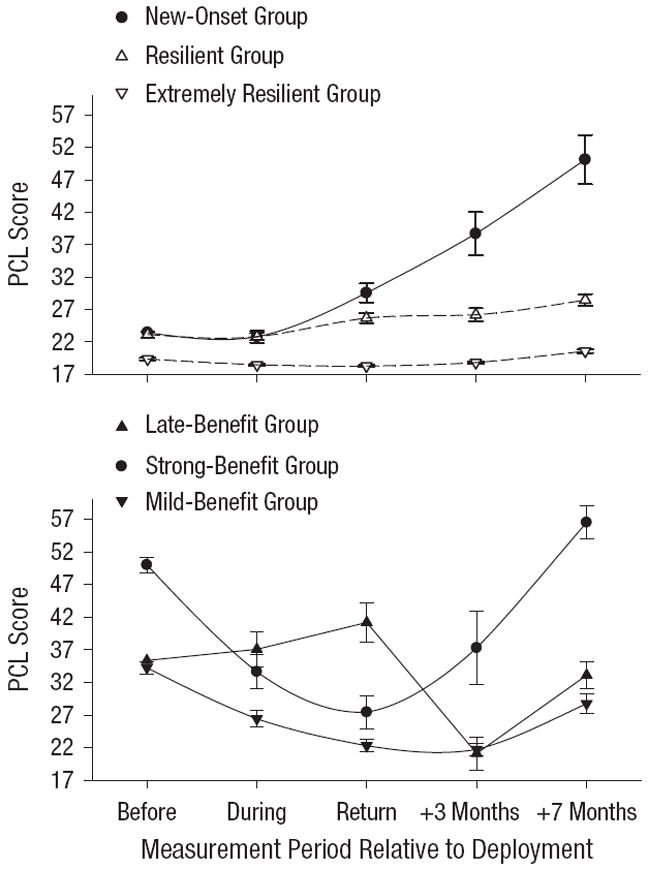
Scores on the Posttraumatic Stress Disorder Checklist (PCL; Blanchard, Jones-Alezander, Buckley, & Forneris, 1996) as a function of measurement occasion and group. The upper panel shows results for the extremely resilient group (n = 255, or 70% of the sample), the resilient group (n = 51, 14%), and the new-onset group (n = 14, 4%), and the lower panel shows results for the three benefit groups (i.e., those whose symptoms decreased at one or more measurement occasions during and following deployment): the strong-benefit group (n = 8, 2%), the mild-benefit group (n = 24, 7%), and the late-benefit group (n = 14, 4%). Error bars indicate standard errors.
Resilient versus nonresilient groups
Table 2 shows the means of health and risk factors for the six groups and the group differences. We first examined the overall differences between the two resilient groups versus the four nonresilient groups in a series of contrast analyses (or chi-square tests, when appropriate). The results are shown in Table 2. We then conducted a logistic regression analysis predicting resilient versus nonresilient group membership, with the significant predeployment measures (except PTSD symptoms, which defined the groups) and the significant stressors measured at return from deployment as the independent variables. This analysis showed effects of depression—Wald(1) = 15.17, b = −0.17, p < .0001, odds ratio = .84, 95% confidence interval (CI) = [.77, .92]; Neuroticism—Wald(1) = 17.53, b = −0.22, p < .0001, odds ratio = .80, 95% CI = [.72, .89]; previous traumas—Wald(1) = 10.35, b = −0.10, p < .005, odds ratio = .90, 95% CI = [.85, .96]; and previous emotional problems, Wald(1) = 4.76, b = −1.09, p < .05, odds ratio = .34, 95% CI = [.13, .90].
Table 2.
Comparison of Risk Factors for the Six Groups
| Risk factor | Resilient groups
|
Nonresilient groups
|
Group differences
|
|||||
|---|---|---|---|---|---|---|---|---|
| Extremely resilient | Resilient | New onset | Strong benefit | Mild benefit | Late benefit | All groups | Resilient vs. nonresilient | |
| Predeployment measures | ||||||||
| Mean age (years) | 27.65 | 24.39 | 28.29 | 22.63 | 22.45 | 22.93 | F(5, 360) = 4.99** | t(360) = 1.70 |
| Female (%) | 5.10 | 5.88 | 14.29 | 25.00 | 8.33 | 14.29 | χ2(5, N = 366) = 8.21 | χ2(1, N = 366) = 5.38* |
| Enlisted rank (%) | 86.17 | 92.16 | 78.57 | 87.50 | 100.00 | 92.86 | χ2(5, N = 364) = 6.36 | χ2(1, N = 364) = 0.95 |
| Combat soldiers (%) | 34.65 | 56.86 | 42.86 | 37.50 | 75.00 | 85.71 | χ2(5, N = 365) = 31.82*** | χ2(1, N = 365) = 14.54** |
| Number of earlier missions | 1.19 | 0.54 | 0.54 | 0.29 | 0.54 | 0.46 | F(5, 349) = 2.96* | t(349) = 1.62 |
| Years in military | 7.09 | 3.31 | 9.54 | 3.75 | 2.13 | 2.07 | F(5, 359) = 5.84*** | t(359) = 0.73 |
| PTSD symptoms score | 19.35 | 23.13 | 23.45 | 50.00 | 34.25 | 35.36 | F(5, 360) = 234.65*** | t(360) = 26.53*** |
| Depression score | 3.35 | 5.88 | 7.71 | 20.83 | 12.55 | 13.42 | F(5, 350) = 39.94*** | t(350) = 11.25*** |
| Neuroticism score | 28.55 | 31.08 | 32.71 | 36.57 | 35.65 | 36.08 | F(5, 341) = 14.72*** | t(341) = 6.08*** |
| Earlier-traumas score | 8.59 | 7.78 | 15.71 | 23.25 | 16.00 | 13.50 | F(5, 352) = 9.84*** | t(352) = 6.65*** |
| Low education (%) | 22.13 | 17.65 | 28.57 | 75.00 | 45.83 | 42.85 | χ2(5, N = 364) = 21.11** | χ2(1, N = 364) = 14.80** |
| Earlier emotional problems (%) | 15.35 | 14.00 | 57.14 | 50.00 | 33.33 | 42.85 | χ2(5, N = 364) = 28.59*** | χ2(1, N = 364) = 25.12*** |
| Stressors measured during deployment | ||||||||
| Combat-exposure score | 10.59 | 14.62 | 12.00 | 7.00 | 15.72 | 16.17 | F(5, 288) = 4.00** | t(288) = 0.08 |
| Danger/injury-exposure score | 18.31 | 19.64 | 18.25 | 19.71 | 19.90 | 19.92 | F(5, 301) = 1.26 | t(301) = 0.61 |
| Emotional stress | 1.75 | 2.17 | 2.50 | 2.29 | 1.87 | 2.23 | F(5, 312) = 6.29*** | t(312) = 2.26* |
| Times when life was in danger | 2.96 | 3.45 | 2.58 | 2.29 | 2.74 | 3.38 | F(5, 308) = 0.77 | t(308) = 1.23 |
| Stressors measured 1 to 3 weeks after return from deployment | ||||||||
| Combat-exposure score | 14.88 | 19.95 | 17.56 | 11.00 | 21.64 | 21.64 | F(5, 277) = 3.62** | t(277) = 0.22 |
| Danger/injury-exposure score | 19.87 | 21.24 | 20.30 | 20.71 | 22.25 | 22.92 | F(5, 286) = 1.95 | t(286) = 1.16 |
| Emotional stress | 2.03 | 2.28 | 2.50 | 2.40 | 2.23 | 2.54 | F(5, 298) = 2.76* | t(298) = 1.99* |
| Times when life was in danger | 3.37 | 4.44 | 3.30 | 3.16 | 5.00 | 4.62 | F(5, 300) = 3.52** | t(300) = 0.27 |
| Wounded-injured (%) | 12.92 | 18.60 | 30.00 | 33.33 | 31.82 | 7.69 | χ2(5, N = 303) = 9.33 | χ2(1, N = 303) = 4.28* |
| Killed an enemy (%) | 20.69 | 25.00 | 30.00 | 33.33 | 40.91 | 53.85 | χ2(5, N = 294) = 11.15* | χ2(1, N = 294) = 8.83** |
Note: Symptoms of posttraumatic stress disorder (PTSD) were measured using the PTSD Checklist (Blanchard, Jones-Alezander, Buckley, & Forneris, 1996). Depression was measured using the second edition of the Beck Depression Inventory (Beck, Steer, & Brown, 1996). Neuroticism was measured using a scale derived from the NEO Five Factor Inventory (Costa & McCrae, 1989). Earlier traumas were measured using the Traumatic Life Event Questionnaire (Kubany et al., 2000). Combat exposure and danger/injury exposure were measured using the Combat Exposure Scale (Keane et al., 1989) and the Danger/Injury Exposure Scale constructed by the Danish military, respectively. Emotional stress was measured on a scale from 1 (never) to 4 (very often). The number of times when life was in danger was measured on a scale from 0 (never) to 6 (more than five times). All t tests are based on contrast analyses.
p < .05.
p < .01.
p < .0001.
Of interest is how each of the four nonresilient groups uniquely differed from the resilient groups. We used the resilient group for comparison because this group was similar to the new-onset group with regard to predeployment level of PTSD symptoms, age, military rank, and number of combat soldiers. The resilient group was similar to the three benefit groups with regard to age, military rank, number of combat soldiers, and years spent in the military (see Table 2).
Resilient group versus new-onset group
The new-onset group is of key theoretical interest for understanding the development of PTSD because it includes soldiers with no PTSD before deployment but high levels of symptoms after returning from deployment. This group differed from the resilient group by having spent more years in the military, t(359) = 2.85, p < .01, by reporting more previous traumas, t(352) = 3.07, p < .01, and by having more cases with earlier emotional problems for which they had received help, t(358) = 3.70, p < .0001. It did not differ from the resilient group on any other predeployment health or personality measure, or on any stressors measured during deployment and after return from deployment.
An analysis of the scores for specific event categories in the TLEQ showed that the new-onset group differed from the resilient group in four categories, three of which were associated with interpersonal violence, especially in childhood: Being physically punished while growing up in a way that resulted in bruises, burns, cuts, or broken bones, t(360) = 3.91, p < .0001; witnessing family violence while growing up, t(360) = 5.57, p < .0001; being slapped, punched, kicked, beaten up, or otherwise physically hurt by a spouse or an intimate partner, t(360) = 3.26, p < .005; and having an abortion or having a partner who had an abortion, t(360) = 3.67, p < .0001. A logistic regression analysis with these trauma measures as predictor variables and new-onset versus resilient group as the dependent variable showed a significant effect of witnessing family violence while growing up, Wald(1) = 5.39, b = 0.65, p < .01, odds ratio = 1.92, 95% CI = [1.11, 3.33]. (See the Supplemental Material for additional results.)
Resilient group versus benefit groups
It was surprising that some soldiers showed an improvement in PTSD symptoms after deployment (the three benefit groups) because this suggests that there are temporary emotional improvements associated with deployment. We compared the three benefit groups with the resilient group in a series of contrast analyses. The three benefit groups had higher levels of predeployment PTSD symptoms, t(360) = 21.99, p < .0001, higher levels of predeployment depression, t(350) = 11.25, p < .0001, and higher levels of neuroticism, t(341) = 3.89, p < .0001, than the resilient group did. In addition, the three benefit groups reported more previous traumas, t(352) = 5.25, p < .0001, more previous emotional problems, t(358) = 3.35, p < .005, and more cases with low education, t(358) = 4.00, p < .0001. The benefit groups did not differ from the resilient group on any deployment-related stressor measured during deployment and at return from deployment.
With regard to the specific previous traumas reported in the TLEQ, the benefit groups differed from the resilient group by reporting more predeployment incidences of interpersonal violence, including having someone threatening to kill them or cause them serious physical harm, t(358) = 3.91, p < .0001; being physically punished while growing up in a way that resulted in bruises, burns, cuts, or broken bones, t(360) = 4.21, p < .0001; witnessing family violence while growing up, t(360) = 4.58, p < .0001; being stalked, t(360) = 3.26, p < .005, and having accidents with serious injury, t(360) = 3.10, p < .005. They also more frequently reported events they could not talk about, t(305) = 4.24, p < .0001. A logistic regression analysis with these trauma measures as predictor variables and benefit groups versus resilient group as the dependent variable showed a significant effect of witnessing family violence while growing up, Wald(1) = 4.32, b = 0.55, p < .05, odds ratio = 1.74, 95% CI = [1.03, 2.94], and a marginally significant effect of being stalked, Wald(1) = 3.74, b = 1.01, p = .05, odds ratio = 2.76, 95% CI = [0.99, 7.71]. (See the Supplemental Material for additional results.)
Comparison with traditional analytic strategies
Only a few studies have examined pre- to postdeployment changes in PTSD symptoms. Most have used a single before and after measure and found combat-related stress to be a significant predictor of postdeployment PTSD (Polusny et al., 2011; Rona et al., 2009; Smith, Ryan, et al., 2008; Vasterling et al., 2010). We replicated these findings in this study for two of three postdeployment PTSD measures using similar analytic strategies: We conducted three multiple linear regression analyses with PTSD symptoms measured at return from deployment, approximately 3 months after return from deployment, and approximately 7 months after return from deployment as the dependent variables, respectively. Each analysis included the commonly used predictors combat exposure, pre-deployment PTSD, age, gender, enlisted rank, level of education, and years in the military. The analyses showed significant effects of combat exposure for PTSD symptoms measured at return from deployment, t(399) = 3.20, p < .005, and 7 months after return from deployment, t(179) = 2.96, p < .005, but not at 3 months after return from deployment, t(219) = 0.16, p > .8. Similar results were obtained when we limited the regression analyses to individuals who had answered the PCL at all three postdeployment occasions, which indicates that our findings did not just reflect sampling bias due to nonresponse. Thus, we replicated the predictive value of combat exposure when using analytic strategies similar to the ones used in previous prospective studies, but we also found that the predictive value of combat exposure varied with the timing of measuring postdeployment PTSD symptoms.
Discussion
Using latent class growth modeling, we identified six reliably different developmental trajectories of PTSD symptoms among combat soldiers. These trajectories consisted of two resilient groups, one new-onset group, and three groups showing temporary benefits of deployment. The majority of the sample fell into the two resilient groups, a finding consistent with previous work (Bonanno et al., 2012; Dickstein et al., 2010). Resilience was negatively related to depression, neuroticism, previous traumatic events, and emotional problems prior to deployment. Deployment-related stressors did not predict nonresilient symptom patterns, a result consistent with some previous work (Fear et al., 2010).
The new-onset group had the same low level of PTSD symptoms before and during deployment as did the resilient group. However, the symptoms showed a marked linear increase through return from deployment, 3 months after return from deployment, and 7 months after return from deployment, which indicates that cases identified as new onsets in the present study were reliable (and not due to fluctuation or the timing of the postdeployment measurement). The number of new-onset cases (4%) in the present study is comparable to that in previous work (Rona et al., 2009; Smith, Ryan, et al., 2008). A key variable differentiating the new-onset and the resilient group was the number of previous traumas they had experienced. Traumas involving interpersonal violence in childhood appeared especially central. This finding adds to previous work showing the importance of childhood traumas as a risk factor for PTSD later in life (Bremner, Southwick, Johnson, Yehuda, & Charney, 1993; Iversen et al., 2007; Polusny et al., 2011; Smith, Wingard, et al., 2008); however, this effect may be limited to childhood traumas involving PTSD (Breslau, Peterson, & Schultz, 2008). We observed no effects of deployment-related stressors, such as combat exposure.
We identified three groups that have hitherto been overlooked in studies of deployment-related PTSD, although they accounted for 13% of the sample. All three groups showed temporary beneficial effects of deployment. They differed from the resilient group by having more emotional problems, depression, PTSD symptoms, and previous traumas before deployment and by being less well educated. In these benefit groups, 50% had no completed education beyond 9 to 10 years of obligatory public school. In the general Danish population of males at their age (20–25 years), only 35% (Statistics Denmark, 2011) have no education beyond public school, χ2(1, N = 46) = 4.70, p < .05. The three benefit groups were thus less well educated than their cohort in general.
Traumatic events with interpersonal violence, especially when the individuals were growing up, were commonly reported in the three benefit groups. The low educational level combined with pronounced emotional problems before deployment leaves the impression of a group who may experience more social support and life satisfaction within their team of fellow soldiers during military deployment than at home. Thus, recognition and comradeship in the unit may be central factors underlying the temporary mental-health benefits. Hughes et al. (2005) also found beneficial effects of military deployment on mental health, but it is not clear whether this effect was temporary, because only one postdeployment measure was obtained in their study.
Our findings have three important implications. First, other factors than immediately preceding stressors are critical for new cases of PTSD after deployment, with childhood stressors appearing to be a key factor. This does not defy a dose-response view of PTSD—that is, the view that the magnitude of the trauma predicts the severity of the symptoms (e.g., Neuer et al., 2004)—but suggests that such a view be considered in a more complex life-span developmental perspective (e.g., Bremner et al., 1993; Breslau et al., 2008; Koenen, Moffit, Poulton, Martin, & Caspi, 2007). Second, the predictive value of combat exposure varies as a function of when postdeployment measures are taken. This shows that several measurements are needed to disentangle this complex relation and possibly resolve some of the conflicting findings in earlier work (Fear et al., 2010; Polusny et al., 2011; Rona et al., 2009; Smith, Ryan, et al., 2008; Vasterling et al., 2010). Third, the development of PTSD symptoms in combat soldiers shows heterogeneity, which indicates that multiple measurements of the same individuals are necessary to understand the complexity of the disorder and to identify individuals in need of treatment.
Supplementary Material
Acknowledgments
We thank Robert Jonasen, Per Bach, Christoffer Holmgård Pedersen, and Anne Scharling Rasmussen for their assistance, and Gary Bennett and two anonymous reviewers for comments.
Funding
This research was funded by the Danish National Research Foundation, the Danish Council for Independent Research: Humanities, the Royal Danish Defense College, and National Institutes of Health Grant No. R01MH066079.
Footnotes
Coincidentally, soldiers from this team took part in the award-winning documentary, Armadillo (Fridthjof & Pedersen, 2010), which graphically depicts conditions on the Helmand frontline in Afghanistan.
Declaration of Conflicting Interests
The authors declared that they had no conflicts of interest with respect to their authorship or the publication of this article.
Additional supporting information may be found at http://pss.sagepub.com/content/by/supplemental-data
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. [Google Scholar]
- Andrews B, Brewin CR, Stewart L, Philpott R, Heidenberg J. Comparison of immediate-onset and delayed-onset posttraumatic stress disorder in military veterans. Journal of Abnormal Psychology. 2009;118:767–777. doi: 10.1037/a0017203. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory. 2. San Antonio, TX: The Psychological Corp; 1996. [Google Scholar]
- Beckham JC, Feldman ME, Kirby AC. Atrocities exposure in Vietnam combat veterans with chronic posttraumatic stress disorder: Relationship to combat exposure, symptom severity, guilt, and interpersonal violence. Journal of Traumatic Stress. 1998;11:777–785. doi: 10.1023/A:1024453618638. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alezander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behaviour Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Mancini AD, Horton JL, Powell TM, Leardmann CA, Boyko EJ, et al. Millennium Cohort Study Team. Trajectories of trauma symptoms and resilience in deployed US service members: Prospective cohort study. The British Journal of Psychiatry. 2012;200:317–323. doi: 10.1192/bjp.bp.111.096552. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Westphal M, Mancini AD. Resilience to loss and potential trauma. Annual Review of Clinical Psychology. 2011;7:511–535. doi: 10.1146/annurev-clinpsy-032210-104526. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Southwick SM, Johnson DR, Yehuda R, Charney DS. Childhood physical abuse and combat-related posttraumatic stress disorder in Vietnam veterans. American Journal of Psychiatry. 1993;150:235–239. doi: 10.1176/ajp.150.2.235. [DOI] [PubMed] [Google Scholar]
- Breslau N, Peterson EL, Schultz LR. A second look at prior trauma and the posttraumatic stress disorder effects of subsequent trauma. Archives of General Psychiatry. 2008;65:431–437. doi: 10.1001/archpsyc.65.4.431. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. Supplement to the NEO Personality Inventory/NEO Five Factor Inventory manual. Odessa, FL: Psychological Assessment Resources; 1989. [Google Scholar]
- Dickstein BD, Suvak M, Litz BT, Adler AB. Heterogeneity in the course of posttraumatic stress disorder: Trajectories of symptomatology. Journal of Traumatic Stress. 2010;23:331–339. doi: 10.1002/jts.20523. [DOI] [PubMed] [Google Scholar]
- Engelhard IM, van den Hout MA, Weerts J, Arntz A, Hox JJ, McNally RJ. Deployment-related stress and trauma in Dutch soldiers returning from Iraq: Prospective study. British Journal of Psychiatry. 2007;191:140–145. doi: 10.1192/bjp.bp.106.034884. [DOI] [PubMed] [Google Scholar]
- Fear NT, Jones M, Murphy D, Hull L, Iversen AC, Coker B, Wessely S, et al. What are the consequences of deployment to Iraq and Afghanistan on the mental health of UK armed forces? A cohort study. The Lancet. 2010;375:1783–1797. doi: 10.1016/S0140-6736(10)60672-1. [DOI] [PubMed] [Google Scholar]
- Fridthjof R, Pedersen JM. Armadillo [Motion picture] Denmark: Fridthjof Film; 2010. Producer, Director. [Google Scholar]
- Graham JW. Adding missing-data-relevant variables to FIML-based structural equation models. Structural Equation Modeling. 2003;10:80–100. [Google Scholar]
- Gray MJ, Bolton EE, Litz BT. A longitudinal analysis of PTSD symptom course: Delayed-onset PTSD in Somalia peacekeepers. Journal of Consulting and Clinical Psychology. 2004;72:909–913. doi: 10.1037/0022-006X.72.5.909. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Horowitz MJ. Stress response syndromes. 2. New York, NY: Jason Aronson; 1986. [Google Scholar]
- Hughes JH, Cameron F, Eldridge R, Devon M, Wessely S, Greenberg N. Going to war does not have to hurt: Preliminary findings from the British deployment to Iraq. The British Journal of Psychiatry. 2005;186:536–537. doi: 10.1192/bjp.186.6.536. [DOI] [PubMed] [Google Scholar]
- Iversen AC, Fear NT, Simonoff E, Hull L, Horn O, Greenberg N, Wessely S, et al. Influence of childhood adversity on health. British Journal of Psychiatry. 2007;191:506–511. doi: 10.1192/bjp.bp.107.039818. [DOI] [PubMed] [Google Scholar]
- Keane T, Fairbank J, Caddell J, Zimering R, Taylor K, Mora C. Clinical evaluation of a measure to assess combat exposure. Psychological Assessment. 1989;1:53–55. [Google Scholar]
- Koenen KC, Moffit TE, Poulton R, Martin J, Caspi A. Early childhood factors associated with the development of post-traumatic stress disorder: Results from a longitudinal birth cohort. Psychological Medicine. 2007;37:181–192. doi: 10.1017/S0033291706009019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreuter F, Muthén B. Longitudinal modeling of population heterogeneity: Methodological challenges to the analysis of empirically derived criminal trajectory profiles. In: Hancock GR, Samuelsen KM, editors. Advances in latent variable mixture models. Charlotte, NC: Information Age Publishing; 2007. pp. 53–75. [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12:210–224. doi: 10.1037//1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Magruder K, Yeager DE. The prevalence of PTSD across war eras and the effects of deployment on PTSD: A systematic review and meta-analysis. Psychiatric Annals. 2009;39:778–788. [Google Scholar]
- McNally RJ. Progress and controversy in the study of posttraumatic stress disorder. Annual Review of Psychology. 2003;54:229–252. doi: 10.1146/annurev.psych.54.101601.145112. [DOI] [PubMed] [Google Scholar]
- Muthén B, Muthén L. Integrating person-centered and variable-centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism: Clinical & Experimental Research. 2000;24:882–891. [PubMed] [Google Scholar]
- Nagin DS, Land KC. Age, criminal careers, and population heterogeneity: Specification and estimation of a nonparametric, mixed Poisson model. Criminology. 1993;31:327–362. [Google Scholar]
- Neuer F, Schauer M, Karunakara U, Klaschik C, Robert C, Elbert T. Psychological trauma and evidence for enhanced vulnerability for posttraumatic stress disorder through previous trauma among West Nile refugees. BMC Psychiatry. 2004;4:34. doi: 10.1186/1471-244X-4-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Polusny MA, Erbes CR, Murdoch M, Arbisi PA, Thuras P, Rath MB. Prospective risk factors for new-onset post-traumatic stress disorder in National Guard soldiers deployed to Iraq. Psychological Medicine. 2011;41:687–699. doi: 10.1017/S0033291710002047. [DOI] [PubMed] [Google Scholar]
- Rona RJ, Hooper R, Jones M, Iversen AC, Hull L, Murphy D, Wessely S, et al. The contribution of prior psychological symptoms and combat exposure to post Iraq deployment mental health in the UK military. Journal of Traumatic Stress. 2009;22:11–19. doi: 10.1002/jts.20383. [DOI] [PubMed] [Google Scholar]
- Rubin DC, Berntsen D, Bohni KM. A memory based model of posttraumatic stress disorder: Evaluating basic assumptions underlying the PTSD diagnosis. Psychological Review. 2008;115:985–1011. doi: 10.1037/a0013397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith TC, Ryan MAK, Wingard DL, Slymen DJ, Sallis JF, Kritz-Silverstein D. New onset and persistent symptoms of post-traumatic stress disorder self reported after deployment and combat exposures: Prospective population based US military cohort study. British Medical Journal. 2008;336:366–371. doi: 10.1136/bmj.39430.638241.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith TC, Wingard DL, Ryan AK, Kritz-Silverstein D, Slymen DJ, Sallis JF Millennium Cohort Study Team. Prior assault and posttraumatic stress disorder after combat deployment. Epidemiology. 2008;19:505–512. doi: 10.1097/EDE.0b013e31816a9dff. [DOI] [PubMed] [Google Scholar]
- Statistics Denmark. Statistikbanken [Statbank] 2011 Retrieved from http://www.statistikbanken.dk/statbank5a/default.asp?w=1400.
- Vasterling JJ, Proctor SP, Friedman MJ, Hoge CW, Heeren T, King LA, King DW. PTSD symptom increases in Iraq-deployed soldiers: Comparison with nondeployed soldiers and associations with baseline symptoms, deployment experiences, and postdeployment stress. Journal of Traumatic Stress. 2010;23:41–51. doi: 10.1002/jts.20487. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


