Abstract
Acute pancreatitis is acute inflammatory disease of the pancreas. Nutrition has a number of anti-inflammatory effects that could affect outcomes of patients with pancreatitis. Further, it is the most promising nonspecific treatment modality in acute pancreatitis to date. This paper summarizes the best available evidence regarding the use of nutrition with a view of optimising clinical management of patients with acute pancreatitis.
1. Epidemiology and Economic Burden of Acute Pancreatitis
Acute pancreatitis is a common digestive disease and the most frequent disorder of the pancreas. It is observed in every part of the world, but the incidence of acute pancreatitis varies considerably between countries. Relatively low figures are reported from the United Kingdom (9.8 cases per 100,000 population per year), Germany (13.1 cases per 100,000 population per year), and Japan (15.4 cases per 100,000 population per year) [1–3]. Medium figures are reported from New Zealand (29.3 cases per 100,000 population per year), Iceland (32.3 cases per 100,000 population per year), and Norway (34.4 cases per 100,000 population per year) [4–6]. The highest figures in the literature are reported from the United States (73.0 cases per 100,000 population per year) and Finland (73.4 cases per 100,000 population per year) [7, 8]. However, direct comparison of incidences between countries is hardly legitimate because of diagnostic, aetiological, ethnic, and other differences between the study populations.
Several reports from the United States and Western Europe indicate that the frequency of this disease has increased dramatically [9–11]. In the United States, there were significant upward trends in both absolute numbers of hospitalisations for acute pancreatitis and annual incidence [7]. The absolute number of admissions was 101,000 in 1988 as compared with 201,000 in 2002. The annual incidence was also the lowest in 1988 at 41 cases per 100,000 population and peaked in 2002 at 73 cases per 100,000 population. In Denmark, the annual incidence increased from 17 cases per 100,000 population in 1981 to 32 cases per 100,000 population in 2000 [9]. Similarly, in Sweden, the annual incidence increased from 18 cases per 100,000 population in 1985 to 35 cases per 100,000 population in 1999 [10].
Most studies reporting on trends also indicate a steady decrease in the case-fatality rate over time. The case fatality for acute pancreatitis has decreased from 15%–21% in the earlier studies to 2%–7% in the recent studies [1, 12]. Although the case-fatality rate has decreased, several studies have reported that the population mortality rate has remained unchanged over time. The likely explanation for this is that, given that the case-fatality rate is a proportion of deaths within a designated population of people with acute pancreatitis and the population mortality is a rate per 100,000 population, better detection of mild cases within a population results in a decrease in case fatality but not in the population mortality rate. In addition, a proportional increase in the number of nonmild acute pancreatitis cases from an increase in the incidence may be offset by a decrease in mortality from earlier recognition and better treatment of local and systemic complications over time [13–15].
Patients with acute pancreatitis also pose a considerable financial burden to health care systems. An earlier study of patients with necrotising pancreatitis from the United Kingdom estimated that the actual cost of treatment ranged from £9296 to £33796, of which two-thirds was attributable to hospitalisation, 20% to surgical and endoscopic interventions, and 16% to investigations [1]. A recent study from the United States estimated that the total cost of acute pancreatitis admissions in 2003 was $2.2 billion (95% confidence interval 2.0–2.3 billion). Further, mean cost per hospitalisation was $9870 (95% confidence interval 9300–10,400) and mean cost per hospital day was $1670 (95% confidence interval 1620–1720) [9].
2. Role of Enteral Nutrition in Curtailing Inflammation of the Pancreas
Acute pancreatitis is a common disease with an increasing incidence. Still high morbidity and mortality in this disease as well as the overwhelming cost of treatment indicate significant room for improvement in clinical management. While there is no specific therapy for patients with acute pancreatitis as yet, adequate early treatment with established non-specific modalities has led to improved outcomes [16–19]. There have been several recent advances in the early non-specific management of acute pancreatitis. These include emergence of randomised controlled trials on fluid resuscitation and analgesia, more data (albeit conflicting) on the prophylactic use of antibiotics, and restriction of indications for early therapeutic endoscopic retrograde cholangiopancreatography to patients with coexisting acute cholangitis. However, the most notable and consistent improvement in outcomes over the last decade has come from the use of enteral nutrition in patients with acute pancreatitis [20–22].
The importance of providing nutritional support in patients with acute pancreatitis has been known since the 1970s. Parenteral nutrition was regarded as the standard of nutritional management for nearly four decades due to the advocacy of the “pancreatic rest” concept. The rationale for this concept was to rest the inflamed pancreas, thereby preventing stimulation of exocrine function and release of proteolytic enzymes. However, critics argued that, in addition to cost and catheter-related sepsis, parenteral nutrition might lead to electrolyte and metabolic disturbances, gut barrier alteration, and increased intestinal permeability. Comparison of total parenteral nutrition and total enteral nutrition in patients with predicted severe acute pancreatitis was the subject of eight randomised controlled trials (Table 1) [23–30]. The results were statistically aggregated in several meta-analyses, all of which demonstrated the benefits of enteral over parenteral nutrition. In particular, a meta-analysis of high-quality randomised controlled trials only has shown a significant 2.0-fold reduction in the risk of total and pancreatic infectious complications and a 2.5-fold reduction in the risk of death in patients receiving total enteral nutrition [31–33].
Table 1.
Randomised controlled trials of total enteral versus total parenteral nutrition in patients with predicted severe acute pancreatitis.
| Reference | Year | Setting | Patients (n) | Allocation concealment | Reduction of infectious complications and mortality | |
|---|---|---|---|---|---|---|
| Enteral nutrition | Parenteral nutrition | |||||
| Kalfarentzos et al. [70] | 1997 | Greece | 18 | 20 | Openlabel | Significantly lower rate of pancreatic infection in the total enteral nutrition group |
| Gupta et al. [43] | 2003 | UK | 8 | 9 | Openlabel | Non-significantly lower rate of pancreatic infection in the total enteral nutrition group |
| Louie et al. [71] | 2005 | Canada | 10 | 18 | Openlabel | Non-significantly lower rate of pancreatic infection in the total enteral nutrition group |
| Eckerwall et al. [41] | 2006 | Sweden | 23 | 25 | Openlabel | No significant difference in outcomes |
| Petrov et al. [72] | 2006 | Russia | 35 | 34 | Openlabel | Significantly lower rate of pancreatic infection and mortality in the total enteral nutrition group |
| Casas et al. [73] | 2007 | Spain | 11 | 11 | Openlabel | Non-significantly lower rate of pancreatic infection in the total enteral nutrition group |
| Doley et al. [74] | 2008 | India | 25 | 25 | Openlabel | No significant difference in the outcomes |
| Wu et al. [75] | 2010 | China | 53 | 54 | Openlabel | Significantly lower rate of pancreatic infection and mortality in the total enteral nutrition group |
Despite the evident clinical benefits of enteral over parenteral nutrition in terms of the reduction in risk of infectious complications and mortality, the exact mechanism of its favourable effect remains unclear [34–36]. It is believed that enteral nutrition may prevent or attenuate the mucosal barrier breakdown and subsequent bacterial translocation that play a pivotal role in the development of infectious complications in the course of severe acute pancreatitis. When monitoring mucosal barrier function, permeability of the structural mucosal barrier is often the main parameter measured. Unfortunately, there is no consistency in the clinical studies with regard to gut permeability. On the one hand, three clinical studies of acute pancreatitis showed increased intestinal permeability to both micromolecules and macromolecules in patients with predicted severe acute pancreatitis when compared with predicted mild acute pancreatitis and healthy volunteers [37–39]. On the other hand, the randomised controlled trial by Powell and colleagues, in which patients with predicted severe acute pancreatitis were randomised to receive either enteral nutrition or no artificial nutritional support, showed significantly increased intestinal permeability by day 4 in patients allocated to the enteral nutrition group [40]. Similarly, the randomised controlled trial of nasogastric versus parenteral feeding in predicted severe patients by Eckerwall and colleagues demonstrated impaired gut permeability on day 3 in the enteral nutrition group [41]. However, in fact, both randomised controlled trials included a considerable number of patients with mild acute pancreatitis (11 of 27 and 26 of 48, resp.), in which it is unlikely that intestinal permeability changed considerably.
Furthermore, concentrations of anti-endotoxin core antibodies for immunoglobulin M were also used as an indirect marker for intestinal permeability. Results of the randomised controlled trial by Windsor and colleagues showed that serum immunoglobulin M antibodies decreased significantly following 7 days of enteral nutrition when compared with the parenteral nutrition group (P < 0.05) [42]. Similarly, the randomised controlled trial by Gupta and colleagues demonstrated that immunoglobulin M antibodies fell significantly in the enteral nutrition group (P = 0.03) and tended to rise in the parenteral nutrition group over the week of treatment [43]. Conversely, the randomised controlled trial by Eckerwall and colleagues found decreasing levels of immunoglobulin M antibodies in both the enteral nutrition and parenteral nutrition groups, with no significant difference at any time point during ten days of observation [41]. The mechanism of beneficial influence of enteral nutrition in acute pancreatitis warrants further investigation, and more studies on the use of enteral nutrition in patients with acute pancreatitis are needed.
3. Optimal Route of Enteral Nutrition Delivery
The previous section has demonstrated that enteral nutrition is preferred to parenteral nutrition because it leads to significantly better glycemic control, decreases infectious complications, reduces the need for surgery, and reduces mortality. With these benefits apparent, one of the unanswered questions has been to determine if there is an optimal site for tube placement during feeding administration. The alternatives include postpyloric (mainly, nasojejunal) and prepyloric (nasogastric) tube placement. The former usually requires the assistance of an endoscopist or a radiologist, and this may result in a delay in commencing enteral nutrition. This delay may have an impact on the clinical outcome because it is now believed that enteral nutrition should commence as soon as possible after adequate fluid resuscitation in order to maximise clinical benefit. In contrast, a nasogastric feeding tube can usually be inserted immediately and with ease, such that prepyloric feeding can be started without delay.
The question of optimal site of enteral feeding in acute pancreatitis also relates to the “pancreatic rest” concept. The central tenet of this concept is that enteral nutrition delivered into any part of the upper gastrointestinal tract other than the jejunum stimulates pancreatic secretion and, consequently exacerbates the severity of acute pancreatitis [44–46]. Given that this concept remained unchallenged for decades, the majority of clinical studies in the field of acute pancreatitis were conducted using nasojejunal tube feeding. However, accumulating evidence from other fields, particularly critical care medicine, suggests that nasogastric feeding may be as safe and effective as nasojejunal feeding, at least in some patients. Thus, there is a need and justification for exploring questions concerning the optimal route of enteral nutrition delivery to be used in patients with acute pancreatitis.
A number of randomised controlled trials and the latest meta-analysis have demonstrated the equivalence of nasogastric and nasojejunal tube feeding in terms of safety and tolerance in critically ill patients [47, 48]. While this may be true for this group of patients, it is recognised that patients with acute pancreatitis are particularly prone to gastric ileus because of the subjacent inflamed pancreas. This has been given as a reason for preferentially providing enteral nutrition into the jejunum [49–51]. Another reason given is to avoid the provision of enteral nutrition proximal to the jejunum where there is concern that it might induce exocrine pancreatic stimulation and consequently a risk of increased severity of acute pancreatitis. Most studies in patients with acute pancreatitis have employed nasojejunal tube feeding, but there are some studies that employed nasogastric tube feeding.
Two systematic literature reviews on nasogastric feeding in acute pancreatitis are available in the literature. The first review attempted to define the feasibility of this route of nutrition by meta-analyzing the data from randomised controlled trials of nasogastric versus “conventional” nutrition [52]. The pooled estimates and variance of the treatment effect were based on the statistical aggregation of the results from studies with essentially different comparators, that is, total parenteral feeding and nasojejunal tube feeding. Such an approach might be misleading because parenteral feeding is no longer considered the first-line approach in acute pancreatitis. Moreover, there was a marked heterogeneity in baseline risk among the studies included in that meta-analysis, particularly in regard to age and gender ratio, and incorrect pooled estimates were presented due to inaccurate data input. Furthermore, that review did not determine the safety, tolerance, and efficacy of nasogastric tube feeding alone.
The second review aimed to determine the safety and tolerance of nasogastric tube feeding alone and to assess the relative efficacy of nasogastric versus nasojejunal feeding in patients with acute pancreatitis [53]. This was done by analyzing all of the literature (randomised and nonrandomised studies) relating to acute pancreatitis and use of nasogastric tube feeding. A computerised literature search of the Cochrane Central Register of Controlled Trials, EMBASE, and MEDLINE was conducted. The search strategy for the Cochrane Central Register of Controlled Trials was “acute pancreatitis” and “nutrition.” The search strategy for EMBASE included the terms “acute pancreatitis” and “enteral nutrition” or “enteral feeding.” The search strategy for MEDLINE was “acute pancreatitis” (title/abstract) and “enteral nutrition” (title/abstract) or “enteral feeding” (title/abstract). No language restrictions were applied. From the studies on enteral nutrition in acute pancreatitis, only data on patients receiving enteral feeding formula via nasogastric tube were extracted. Bibliographies of all selected articles that included information on nasogastric tube feeding in acute pancreatitis were reviewed for other relevant articles. The following selection criteria were used to identify published studies for inclusion in this systematic review:
study design—cohort study or randomised controlled trial;
population—patients with acute pancreatitis;
intervention—nasogastric tube feeding;
outcome—at least one of the following outcomes: tolerance, organ failure, infectious complications, and mortality.
A total of 397 publications were identified using the above search strategy. Of these, 392 articles did not meet the inclusion criteria and were subsequently excluded. A total of five studies were included in this systematic review. One study was a cohort study, whereas four other studies were randomised controlled trials. Table 2 demonstrates the characteristics of studies included in this review [54–57]. All the studies were conducted in patients with predicted severe acute pancreatitis (as defined by the authors). Overall, 131 patients who received nasogastric tube feeding were identified from these studies. The severity of the patients at admission was comparable in all five cohorts, based on Acute Physiology And Chronic Health Evaluation II scoring. Table 3 presents the baseline characteristics of patients who received nasogastric tube feeding.
Table 2.
Characteristics of studies of nasogastric tube feeding.
| Reference | Setting | Design | Control group | APACHE II Score | Feeding start |
Feeding formulation |
Duration of nutrition | Quality of studies§ |
|---|---|---|---|---|---|---|---|---|
| Eatock et al. 2000 [76] | UK | Cohort study | N/A | 10 (4–28)# | <48 hours of admission | Semielemental | Not stated | N/A |
| Eatock et al. 2005 [58] | UK | RCT | Nasojejunal | 10 (7–18)# | 72 (24–72) hours after onset | Semielemental | 5 days | 14 |
| Kumar et al. 2006 [59] | India | RCT | Nasojejunal | 10.5 ± 3.8‡ | 48–72 hours of admission | Semielemental | 7 days | 13 |
| Eckerwall et al. 2006 [41] | Sweden | RCT | Parenteral | 10 (8–13)# | <24 hours of admission | Polymeric | 6 (5–9)# days | 14 |
| Singh et al. 2012 [64] | India | RCT | Nasojejunal | 8.5 (2–19)# | 10 (4–23)# days after onset | Semielemental | 7 days | 13 |
§Range of quality score is 0 to 16; #values are median (range); ‡values are mean ± standard deviation. Abbreviations: APACHE: Acute physiology and chronic health evaluation; RCT: randomised controlled trial; N/A: not available.
Table 3.
Characteristics of patients receiving nasogastric tube feeding.
| Reference | Age | Male : female | Aetiology | ||
|---|---|---|---|---|---|
| Biliary | Alcohol | Other | |||
| Eatock et al. 2000 [76] | 47 (27–96)# | 12 : 14 | 18 | 5 | 3 |
| Eatock et al. 2005 [58] | 63 (47–74)# | 14 : 13 | 16 | 6 | 5 |
| Kumar et al. 2006 [59] | 43.3 ± 12.8‡ | 14 : 2 | 8 | 4 | 4 |
| Eckerwall et al. 2006 [41] | 71 (58–80)†# | 10 : 14† | 14† | 3† | 7† |
| Singh et al. 2012 [64] | 39.1 ± 16.7‡ | 28 : 11 | 12 | 12 | 15 |
†Before exclusion of protocol violator (one patient); #values are median (range); ‡values are mean ± standard deviation.
Nasogastric feeding-related outcomes, including safety and tolerance, are presented in Table 4. Full tolerance was achieved in 107 of 131 (82%) patients who did not require temporary reduction, stoppage, or withdrawal of nasogastric feeding. The 24 patients who had a modification of the nasogastric tube feeding regimen presented signs of gastric ileus (n = 7) and troublesome diarrhoea (n = 14) or repeatedly removed their feeding tube (n = 3).
Table 4.
Safety and tolerance of nasogastric tube feeding.
| Reference | Total patients | Troublesome diarrhoea n, (%) |
Tube removal n, (%) |
Gastric retention n, (%) | Exacerbation of pain following feeding, n, (%) | Achievement of nutritional goal | Full tolerance of feeding n, (%)† |
|---|---|---|---|---|---|---|---|
| Eatock et al. 2000 [76] | 26 | 3 (11.5) | 1 (3.8) | 3 (11.5) | 0 (0) | Not stated | 19 (73.1) |
| Eatock et al. 2005 [58] | 27 | 3 (11.1) | 1 (3.7) | 0 (0) | 2 (7.4) | 21 patients (78%) after 60 hours |
23 (85.1) |
| Kumar et al. 2006 [59] | 16 | 4 (25) | 1 (6.3) | 0 (0) | 1 (6.3) | 16 patients (100%) by day 7* |
11 (68.8) |
| Eckerwall et al. 2006 [41] | 23 | 0 (0) | 0 (0) | 3 (13) | Not stated | 15 patients (66%) by day 7 |
20 (86.9) |
| Singh et al. 2012 [64] | 39 | 4 (10.4) | 0 (0) | 1 (2.5) | 3 (7.7) | Not stated | 34 (85.6) |
|
| |||||||
| Total | 131 | 14 (10.7) | 3 (2.3) | 7 (5.3) | 6 (4.5) | N/A | 107 (82.0) |
†Did not require temporary reduction, stoppage, or withdrawal of feeding; *six patients were supplemented by parenteral nutrition during the commencement of feeding. N/A: not available.
The other clinically meaningful outcomes of the studies are summarised in Table 5. Sixty-one of 92 (45%) patients required ventilatory support. There was no evidence of aspiration pneumonia in any of the patients. Infected pancreatic necrosis was revealed in 15 (12%) patients. Multiple organ failure developed in 21 (16%) patients. The mortality rate was 15%.
Table 5.
Outcomes of patients who received nasogastric feeding.
| Reference | Total patients (n) | Patients on ventilatory support n, (%) |
Patients with MOF n, (%) |
Infected pancreatic necrosis n, (%) |
Surgery n, (%) |
Mortality n, (%) |
LOS, days |
|---|---|---|---|---|---|---|---|
| Eatock et al. 2000 [76] | 26 | 11 (42.3) | 6 (23.1) | 5 (19.2) | 10 (38.5) | 4 (15.4) | 17.5 (3–82) |
| Eatock et al. 2005 [58] | 27 | 7 (25.9) | Not stated | Not stated | Not stated | 5 (18.5) | 16 (10–22) |
| Kumar et al. 2006 [59] | 16 | 15 (93.8) | 3 (18.8) | 5 (31.3) | 1 (6.3) | 5 (31.3) | 24 ± 14.3 |
| Eckerwall et al. 2006 [41] | 23 | 2 (8.7) | 1 (4.3) | 1 (4.3) | 1 (4.3) | 1 (4.3) | 9 (7–14) |
| Singh et al. 2012 [64] | 39 | 26 (66.7) | 11 (28.2) | 4 (10.2) | 4 (10.2) | 4 (10.2) | 17 (1–73) |
|
| |||||||
| Total | 131 | 61 (46.5) | 21 (16.0) | 15 (11.5) | 16 (12.2) | 19 (14.5) | N/A |
MOF: multiple organ failure; LOS: length of hospital stay; NA: not available.
The meta-analysis was restricted to randomised studies of nasogastric versus nasojejunal feeding [55–57]. In three eligible trials, a total of 82 patients received enteral nutrition via the nasogastric route and 75 patients via the nasojejunal route. The use of nasogastric feeding resulted in a nonsignificant reduction in the risk of death (relative risk 0.71; 95% confidence interval 0.38 to 1.32; P = 0.28). The number of nutrition-associated adverse events was similar between the two groups. As a consequence, nasogastric feeding was associated with a nonsignificant increase in the risk of troublesome diarrhoea (relative risk 1.39; 95% confidence interval 0.57–3.36; P = 0.47) and a nonsignificant decrease in the risk of pain relapse following feeding (relative risk 0.84; 95% confidence interval 0.27–2.59; P = 0.76). Overall, patients in both groups did not differ significantly in terms of intolerance to feeding (relative risk 1.23; 95% confidence interval 0.59–2.55; P = 0.57). There was no heterogeneity between the study results for all comparisons (I 2 = 0%).
This systematic review has demonstrated the safety and tolerance of nasogastric tube feeding in at least four out of five patients with acute pancreatitis. The study population was limited to patients with a predicted severe course of acute pancreatitis and the clinical outcomes were within the expected range for this category of patients. Nasogastric tube feeding-related problems occurred in less than 20% of patients and they were relatively minor. There were no recorded cases of aspiration pneumonia.
Three randomised controlled trials included in the meta-analysis consistently yielded no tangible difference between nasogastric and nasojejunal feeding in terms of safety and tolerance [55–57]. It should be acknowledged that the trials had some flaws. In particular, it was argued that it is likely that jejunal feeding in the trial from Glasgow was actually duodenal (because true jejunal placement would have been difficult with the types of feeding tubes and placement techniques used), meaning that both feeding arms may have caused equivalent stimulation of pancreatic secretion [58]. The shortcoming of the randomised controlled trial by Kumar and colleagues was that there was a considerable delay (7.8 ± 6.5 and 5.7 ± 4.7 days after symptom onset in the nasogastric and nasojejunal groups, resp.) and that enteral nutrition was commenced late [59]. In addition, the authors observed a high mortality (31% and 29% in the nasogastric and nasojejunal groups, resp.) which might reflect the tendency towards conservative management of patients with infected pancreatic necrosis. The randomised controlled trial by Singh and colleagues suffered from the same shortcoming; that is, the feeding protocol in both groups was commenced relatively late (10 [4–21, 60, 61] and 11 [3–30, 34–39, 44–51, 60–63] days after symptom onset in the nasogastric and nasojejunal groups, resp.) [64]. Apart from these concerns, the three randomised controlled trials were insufficiently powered individually to detect any difference or to demonstrate equivalence between the studied groups in terms of mortality. An adequately powered randomised controlled trial would need to enrol nearly 200 patients per arm in order to show a decrease in mortality from 14% (average rate in the nasogastric group in the present review) to 6% (best results in the nasojejunal group of randomised controlled trials on enteral versus parenteral nutrition) with 80% power and α = 0.05 (two-sided). Such a sample size is appreciably large, even for a multicentre study.
Another relevant issue in considering nasogastric tube feeding is the effect on exocrine pancreatic function. It was shown by O'Keefe and colleagues that all forms of enteral nutrition stimulate pancreatic secretion [65, 66]. In particular, when compared with placebo saline, an oral liquid polymeric diet resulted in a significantly higher level of amylase (P < 0.01) and lipase (P < 0.01); a duodenal polymeric enteral formula led to increased levels of amylase (P < 0.01), lipase (P < 0.01), and trypsin (P < 0.01); and a duodenal elemental feeding formula resulted in an elevated level of lipase (P < 0.05). The same research group also compared the pancreatic secretory response to tube feeding delivered into the duodenum and the mid (40–60 cm distal to the ligament of Treitz) and distal (100–120 cm distal to the ligament of Treitz) jejunum [67, 68]. Even though the authors did not find a direct relationship between the decrease in enzyme secretion and distance down the mid-distal jejunum, they demonstrated significantly lower secretion of trypsin (P < 0.01) and lipase (P < 0.05) in response to the elemental formula delivered into the jejunum (40 cm or more distal to the ligament of Treitz) in comparison with the duodenum. Moreover, the trypsin and lipase secretory response in the mid-distal jejunum group was as low as in the control group (fasting).
However, it should be noted that these studies of the effects of enteral feeding on exocrine pancreatic function were in healthy subjects. There is now convincing evidence that patients with acute pancreatitis have significantly lower rates of enzyme secretion compared with healthy subjects [68]. Furthermore, when patients with mild-to-moderate acute pancreatitis were compared with those with severe acute pancreatitis, a lower secretion of trypsin (6-fold), amylase (22-fold), and lipase (42-fold) was found in the latter group, suggesting that pancreatic enzyme secretion is inversely related to the severity of acute pancreatitis. In line with this finding, another study showed an 86% rate of pancreatic exocrine insufficiency (measured by faecal pancreatic elastase-1) in patients recovering from severe attacks of acute pancreatitis [69]. Moreover, the severity of pancreatic exocrine insufficiency correlated with the extent of pancreatic necrosis. These data suggest that injured acinar cells are not able to respond fully to the physiological stimuli of secretion which may go some way towards explaining the findings of this study that, contrary to popular belief, nasogastric tube feeding does not appear to aggravate the severity of acute pancreatitis [53].
4. Optimal Enteral Nutrition Formulation
The previous section has challenged the notion of putting the pancreas at rest by showing that tube feeding into the stomach is safe and well tolerated in the vast majority of patients with acute pancreatitis. However, it has been known since the groundbreaking experiments by Ivan Pavlov and his disciples that not only the site of feeding but also the composition of enteral feed may affect the pancreatic secretory response and, thus, the question of the optimal enteral nutrition formulation is important, both in the management of patients with acute pancreatitis and for the validity of the “pancreatic rest” concept.
The “pancreatic rest” concept has been regarded as a key element in the early management of patients with acute pancreatitis. As a consequence, for decades, these patients have received total parenteral nutrition in an attempt to avoid stimulation of pancreatic enzyme secretion. However, over the last decade, a number of randomised controlled trials have consistently shown the superiority of enteral over parenteral nutrition in terms of reducing the rate of infectious complications and death [20, 25–27]. Further, a recent meta-analysis of randomised controlled trials established the absolute value of enteral nutrition by demonstrating significantly reduced mortality in patients with acute pancreatitis who received enteral nutrition in comparison with those who did not receive any kind of nutrition [88].
Now that the benefits of enteral nutrition in patients with acute pancreatitis have become widely accepted, one of the key questions to answer is what is the optimal formulation to use [89]. There are more than 100 different enteral nutrition formulations available. These can be broadly classified into the following categories:
elemental—comprising amino acids or oligopeptides, maltodextrins, and medium—chain and long-chain triglycerides;
polymeric—comprising nonhydrolyzed proteins, maltodextrins, and oligofructosaccharides, as well as long-chain triglycerides;
immune-enhancing—comprising substrates that have been hypothesised to modulate the activity of the immune system, for example, immunonutrition (glutamine, arginine, and omega-3 fatty acids), probiotics, fibre-enriched formulation.
In patients with acute pancreatitis, the use of elemental over polymeric formulations presents a number of theoretical advantages because it is believed that an elemental formulation has superior absorption from the intestine, stimulates pancreatic secretions to a lesser degree, and is better tolerated [35, 90, 91]. On the other hand, the major disadvantage of an elemental formulation is its cost, which is reportedly 3–7-fold higher than that of a polymeric formulation. The cost of an immune-enhancing formulation is 3–5-fold higher than the cost of an elemental formulation, but whether this leads to better clinical outcomes is unknown [34, 47, 92–94]. Both elemental and immune-enhancing formulations have a higher osmolar load than polymeric formulations, which are isomolar and so may cause diarrhoea. In addition, increased mortality associated with the use of probiotics in patients with acute pancreatitis, observed in the recently published PROPATRIA trial, has highlighted the need for careful selection of enteral nutrition formulations in current clinical practice as well as in future basic and clinical research [31, 95].
A recent comprehensive systematic literature review has compared the safety, tolerance, and efficacy of all enteral nutrition formulations used in randomised controlled trials of patients with acute pancreatitis [89]. Potentially relevant studies were identified using electronic and manual searches. An electronic search was performed in Scopus, Cochrane Controlled Clinical Trials Register, and MEDLINE (searched through PubMed) databases using the terms “acute pancreatitis,” “enteral nutrition,” “glutamine,” “arginine,” “omega-3 fatty acids,” “probiotics,” and “dietary fibre.” Results were limited to trials in humans. This was also supplemented by scanning the bibliographies of retrieved articles and conference proceedings of selected scientific meetings (Digestive Disease Week, United European Gastroenterology Week, International Pancreatic Association, American Pancreatic Association, and European Pancreatic Club). All languages and types of publications were considered eligible.
In order to be included in the systematic review, a study had to
be a randomised controlled trial in patients with acute pancreatitis;
compare two different feeding regimens, at least one of which had to include enteral tube feeding (with type of the nutritional formulation used clearly specified);
report on feeding intolerance (defined as an episode of temporary reduction, stoppage, or withdrawal of feeding) and at least one of the following outcomes: total infectious complications and in-hospital mortality.
Studies investigating the tolerance of oral refeeding or combined enteral and parenteral nutrition or postoperative nutrition were excluded.
The titles and abstracts of 384 identified papers were screened and 348 were excluded after initial screening. Sixteen publications were subsequently excluded: four were on refeeding in patients with acute pancreatitis, four were republished in a non-English language, three were conducted in patients with acute pancreatitis after surgery, two compared nasogastric and nasojejunal routes of enteral nutrition, two studied enteral nutrition supplemented with parenteral nutrition, and one used the same study population as in another included randomised controlled trial. Thus, a total of 20 randomised controlled trials met all the inclusion criteria [32, 33, 36, 41, 43, 46, 62, 70–73, 75, 93–104]. All included articles were published in peer-reviewed journals.
Among the 20 included randomised controlled trials, 19 were single-centre trials and there was one multicentre trial. Patients received an elemental formulation in eight arms of the included trials, a polymeric formulation in seven arms, a fibre-enriched enteral formulation in six arms, enteral nutrition supplemented with probiotics in four arms, and immunonutrition (glutamine, arginine, and omega-3 fatty acids) in three arms.
The 20 randomised controlled trials comprised a total of 1070 patients with acute pancreatitis (825 with predicted severe and 245 with predicted mild course of acute pancreatitis) [32, 33, 36, 41, 43, 46, 62, 70–73, 75, 93–104]. Twelve studies were limited to patients with predicted severe acute pancreatitis only. Table 6 details the study characteristics of included trials.
Table 6.
Characteristics of randomised controlled trials of various enteral nutrition formulations.
| Reference | Year | Intervention group | Control group | Number of patients | |||
|---|---|---|---|---|---|---|---|
| Intervention group | Control group | Severe | Mild | ||||
| McClave et al. [77] | 1997 | Semielemental EN | PN | 15 | 15 | 6 | 24 |
| Kalfarentzos et al. [70] | 1997 | Semielemental EN | PN | 18 | 20 | 38 | 0 |
| Windsor et al. [42] | 1998 | Polymeric EN | PN | 16 | 18 | 13 | 21 |
| Powell et al. [40] | 2000 | Polymeric EN | NN | 13 | 14 | 27 | 0 |
| Hallay et al. [78] | 2001 | EN with fibre + glutamine + arginine | EN with fibre | 11 | 8 | 19 | 0 |
| Olah et al. [79] | 2002 | Elemental EN | PN | 41 | 48 | 17 | 72 |
| Abou-Assi et al. [80] | 2002 | Elemental EN | PN | 26 | 27 | 26 | 27 |
| Olah et al. [81] | 2002 | EN with fibre + probiotics | EN with fibre | 22 | 23 | 32 | 13 |
| Gupta et al. [43] | 2003 | Polymeric EN | PN | 8 | 9 | 17 | 0 |
| Louie et al. [71] | 2005 | Semielemental EN | PN | 10 | 18 | 28 | 0 |
| Lasztity et al. [82] | 2005 | Polymeric EN + n-3 PUFAs | Polymeric EN | 14 | 14 | 6 | 22 |
| Pearce et al. [83] | 2006 | EN with fibre + glutamine + arginine + omega-3 fatty acids | EN with fibre | 15 | 16 | 31 | 0 |
| Tiengou et al. [84] | 2006 | Semielemental EN | Polymeric EN | 15 | 15 | 19 | 11 |
| Eckerwall et al. [41] | 2006 | Polymeric EN | PN | 23 | 25 | 48 | 0 |
| Petrov et al. [72] | 2006 | Semielemental EN | PN | 35 | 34 | 69 | 0 |
| Casas et al. [73] | 2007 | Semielemental EN | PN | 11 | 11 | 22 | 0 |
| Olah et al. [80] | 2007 | EN with fibre + probiotics | EN with fibre | 33 | 29 | 62 | 0 |
| Karakan et al. [85] | 2007 | EN with fibre | Polymeric EN | 15 | 15 | 30 | 0 |
| besselink et al. [86] | 2008 | EN with fibre + probiotics | EN with fibre | 152 | 144 | 296 | 0 |
| Qin et al. [87] | 2008 | Semielemental EN + probiotics | PN | 36 | 38 | 19 | 55 |
EN: enteral nutrition; PN: parenteral nutrition; PUFA: polyunsaturated fatty acids.
4.1. Elemental versus Polymeric Formulation
One randomised controlled trial directly compared an elemental formulation with a polymeric formulation in 30 patients with mild or severe acute pancreatitis [104]. Given that direct meta-analysis was not possible, the two formulations were compared using the methodology of indirect adjusted meta-analysis. A total of 10 randomised controlled trials comprising 428 patients compared elemental and polymeric formulations indirectly, using parenteral nutrition as a reference treatment. In all patients with acute pancreatitis, the use of an elemental formulation did not result in a significant difference in risk of infectious complications (indirectly estimated relative risk 0.48; 95% confidence interval 0.06–3.76; P = 0.482) and death (indirectly estimated relative risk 0.63; 95% confidence interval 0.04–9.86; P = 0.741). The risk of feeding intolerance did not differ significantly between the two formulations (indirectly estimated relative risk 0.62; 95% confidence interval 0.10–3.97; P = 0.611). These effects were nonsignificant when only patients with severe acute pancreatitis were considered (Table 7).
Table 7.
Pooled estimates and sensitivity analysis.
| Comparison | Severity of acute pancreatitis | Feeding intolerance | Total infectious complications | Mortality | |||
|---|---|---|---|---|---|---|---|
| RR (95% CI) | P | RR (95% CI) | P | RR (95% CI) | P | ||
| (Semi)-elemental versus polymeric | Mild or severe | 0.62 (0.10–3.97)* | 0.61 | 0.48 (0.06–3.76)* | 0.48 | 0.63 (0.04–9.86)* | 0.74 |
| Severe only | 2.26 (0.32–15.27)* | 0.41 | 0.23 (0.03–1.86)* | 0.25 | 0.89 (0.28–4.90)* | 0.12 | |
|
| |||||||
| Fibre-enriched + probiotics versus fibre-enriched | Mild or severe | 0.69 (0.43–1.09)# | 0.11 | 0.71 (0.40–1.27)# | 0.25 | 0.85 (0.18–4.14)# | 0.85 |
| Severe only | 0.69 (0.43–1.09)# | 0.11 | 0.79 (0.40–1.56)# | 0.50 | 0.96 (0.12–7.83)# | 0.97 | |
|
| |||||||
| Fibre-enriched + immunonutrition versus fibre-enriched | Mild or severe | 1.60 (0.31–8.29)# | 0.58 | 0.93 (0.36–2.40)# | 0.88 | 0.60 (0.10–3.55)# | 0.58 |
| Severe only | 1.60 (0.31–8.29) # | 0.58 | 0.93 (0.36–2.40) | 0.88 | 0.60 (0.10–3.55)# | 0.58 | |
*Indirectly estimated RR and its 95% CI; #directly estimated RR and its 95% CI. CI: confidence interval; RR: relative risk.
4.2. Fibre-Enriched Formulation Supplemented with Probiotics versus Fibre-Enriched Formulation
A total of three randomised controlled trials comprising 403 patients directly compared a fibre-enriched formulation supplemented with probiotics and a fibre-enriched formulation only [70, 93, 95]. In all patients with acute pancreatitis, the use of probiotics did not result in a significant difference in the risk of infectious complications (relative risk 0.71; 95% confidence interval 0.40–1.27; P = 0.250) or death (relative risk 0.85; 95% confidence interval 0.18–4.14; P = 0.850). The risk of feeding intolerance did not differ significantly between the two formulations (relative risk 0.69; 95% confidence interval 0.43–1.09; P = 0.110). These effects were nonsignificant when only patients with severe AP were considered (Table 7).
4.3. Additional Studies Not Included in the Meta-Analyses
Four randomised controlled trials were not included in the above meta-analyses because they were not able to be compared, directly or indirectly, with any other randomised controlled trials. One randomised controlled trial compared an elemental formulation supplemented with probiotics versus parenteral nutrition [94]. The use of an enteral feeding formulation resulted in a significantly reduced rate of septic complications (eight of 36 (22%) versus 21 of 38 (55%) patients; P = 0.008) and no difference in mortality (no deaths in both groups). Another trial compared a fibre-enriched formulation with a fibre-free formulation and demonstrated no difference in infectious complications (two of 15 (13%) patients in each group) or mortality (two of 15 (13%) patients versus four of 15 (27%) patients) [85]. All patients tolerated the fibre-enriched formulation, whereas feeding intolerance was observed in two patients who received the fibre-free formulation. One trial compared a polymeric formulation with no nutrition [62]. There was no difference between the groups with regard to rate of infectious complications or mortality. A final randomised controlled trial compared a polymeric formulation supplemented with n-3 polyunsaturated fatty acids with a polymeric formulation only [71]. There was no significant difference between the groups with regard to rate of infectious complications (five of 14 (36%) versus seven of 14 (50%) patients) or mortality (one of 14 (7%) versus two of 14 (14%) patients).
The major finding of this systematic literature review was that the use of a polymeric, in comparison with an elemental, enteral nutrition formulation was not associated with a statistically significant difference in tolerance of feeding, or risk of infectious complications and mortality [89]. In addition, it shows that a fibre-enriched formulation may be safely administered in patients with acute pancreatitis and its supplementation with immunonutrition or probiotics does not improve clinically meaningful outcomes.
This systematic literature review further questioned the “pancreatic rest” concept, which is perhaps the oldest postulate in the management of acute pancreatitis. As discussed in the preceding sections of this paper, a cornerstone of this concept is that avoidance or minimisation of the pancreatic enzyme secretory response might prevent exacerbation of the acute inflammatory process in the pancreas [40, 45, 105, 106]. At least in theory, this may be achieved by administration of a feeding formulation that does not require pancreatic enzymes for absorption (e.g., amino acids or oligopeptides). This was the reason why use of polymeric and fibre-enriched formulations was avoided for decades. However, only two prospective studies showed that a polymeric formulation increases pancreatic enzyme secretion into the duodenum in comparison with an elemental formulation, and both of these studies were conducted in healthy volunteers [67, 107]. Conversely, a randomised controlled trial of patients undergoing resection of the pancreas showed that a polymeric formulation did not increase pancreatic secretion compared with an elemental formulation [108]. The latter finding supports the results of the systematic review by Petrov and colleagues that demonstrated no increase in adverse effects with the use of polymeric and fibre-enriched formulations. Although one might argue that such an inference is premature and it is necessary to wait for a definitive randomised controlled trial, a power calculation shows that this is no simple undertaking. An adequately powered randomised controlled trial would need to enrol 1959 patients per study arm in order to demonstrate a 1.5% absolute reduction in the risk of death between the groups with 80% power and two-sided α = 0.05. Such a sample size appears to be unrealistically large, even for a multicentre trial.
It is also worth noting that elemental and polymeric feeding formulations were rigorously compared over the last two decades in a number of randomised controlled trials in patients with active Crohn's disease, which is perhaps the only disease, apart from AP, in which enteral feeding is used as an established key element of treatment [97, 109, 110]. By 1995, four randomised controlled trials were published, and subsequent meta-analyses failed to demonstrate a difference in efficacy between elemental and polymeric formulations [111]. By 2007, a total of 10 randomised controlled trials were published, but a Cochrane systematic review still found no difference in the induction of remission of active Crohn's disease when different formulations were compared [112]. Hence, it is argued that the use of polymeric feeding formulations is safe in patients with acute pancreatitis, and the research community may now focus on other issues in acute pancreatitis nutrition.
5. Timing of Enteral Nutrition
It is believed that gut dysfunction contributes to the inflammatory response and organ failure in severe acute pancreatitis. Theoretically, enteral feeding can prevent mucosal barrier dysfunction, small bowel bacterial overgrowth, and bacterial translocation and, therefore, should be instituted as early as possible in the course of disease [14, 15, 113, 114]. However, while some authors showed the clinical benefits of early enteral nutrition, others demonstrated the favourable effects of delayed enteral feeding [19, 29]. Unfortunately, such a strategical question as the timing of enteral nutrition in patients with acute pancreatitis has never been studied in randomised controlled trials. At the same time, some randomised controlled trials in critically ill patients suggest that enteral feeding start time has to be within hours of onset of disease.
In particular, burn patients were studied in the randomised controlled trial by Chiarelli and colleagues [115]. Patients were randomized to receive early enteral feeding within 4.4 ± 0.5 h postburn or delayed feeding administered a mean of 57.7 ± 2.6 h after injury. It was shown that patients with very early start of nutrition had fewer infections as well as a significantly shortened length of hospital stay. Furthermore, Graham and colleagues demonstrated with a randomised controlled trial the benefits of early (<36 h) enteral feeding compared with delayed (3–5 d) in 32 patients after head injury [116]. Infectious complications and length of hospital stay in the intensive care unit were reduced significantly with early feeding into the jejunum. In a randomised controlled trial conducted by Peng and colleagues, 22 patients with severe burns were randomized to either early enteral feeding (within 24 h) or delayed enteral feeding (after 48 h). The urinary lactulose levels and the urinary lactulose-mannitol ratios in the early group were significantly lower than in the delayed group as well as the levels of serum endotoxin and TNF-α. It was suggested that early enteral feeding may decrease intestinal permeability, preserve the intestinal mucosal barrier, and have a beneficial effect on the reduction of enterogenic infection. A recent randomised controlled trial from Slovenia in 52 patients with multiple injuries demonstrated that enteral nutrition administered on admission, as compared to enteral feeding started after 24 h of admission, was associated with a lower incidence of upper intestinal intolerance and nosocomial pneumonia. A meta-analysis by Marik and Zaloga demonstrated the benefits of early enteral nutrition (started from 2 to 24 h after operation) versus delayed feeding in terms of reducing episodes of infection and length of hospital stay in patients after abdominal surgery [117].
However, the usefulness of early onset of enteral feeding has not been shown in some other studies. In 2004, Peck and colleagues reported the results of their randomised controlled trial on 27 patients with burn injury. The study demonstrated that early enteral nutrition (<24 h of injury) had no beneficial effect on postburn hypermetabolism when compared with late (>7 d) enteral feeding and also did not result in a reduction of mortality, infectious complications, or hospital stay. In another trial, Dvorak and colleagues randomised 17 patients with acute spinal cord injury to early (initiated before 72 h after injury) or late (started more than 120 h after injury) enteral feeding. The randomised controlled trial failed to detect any differences in the incidence of infection, nutritional status, feeding complications, or length of stay between studied groups. Unfortunately, both randomised controlled trials were underpowered and thereby presented results should be interpreted with caution. Considering the results from randomised controlled trials on this subject in patients with surgical conditions, it seems that there is a sufficient body of evidence to state the need for high quality randomised controlled trial on the efficacy of early versus delayed enteral nutritional strategy in patients with severe acute pancreatitis.
6. Regimen of Enteral Nutrition
The impaired gastrointestinal motility is an important factor in the pathogenesis of complications of acute pancreatitis [51, 118–120]. It may lead to proximal stagnation, gastric and small intestinal bacterial overgrowth with subsequent bacterial translocation, and infection of pancreatic necrosis. Thereby, a recent study questioned the rationale of fasting patients with acute pancreatitis prior to oral refeeding and advocated the early enteral feeding to prevent or attenuate ileus. The logic behind early enteral nutrition is that feeding may stimulate motor migrating complex which is responsible for coordinated propulsive activity of the gastrointestinal tract. At the same time, gut hormones may have an important role in regulating gastrointestinal motility.
In particular, high cholecystokinin level is known to cause delay in gastric empting, and to regulate nutrient-induced jejunogastric feedback mechanism and, thereby, can have influence on the tolerance of enteral feeding [100, 103, 121]. Traditionally, continuous, as opposite to intermittent, EN has been recommended to increase the tolerance of nutrition. Nutritional diet is usually started at low rates (15 mL/h), with gradual advancement to ensure tolerance. However, this tactic has never been tested in randomised controlled trials. By contrast, it was reported in a randomised controlled trial on continuous versus cyclic jejunal nutrition in patients undergoing pylorus-preserving pancreatoduodenectomy that patients on cyclic (discontinuing the nutrition during the night) enteral nutrition had significantly lower levels of cholecystokinin during interruption of feeding. Clinically this finding was associated with shorter length of hospital stay (P < 0.05) and earlier resumption of oral diet (P < 0.05) in the intermittent group. In accordance with these data, a recent randomised controlled trial on continuous versus intermittent gastric feeding in critically ill trauma patients showed that the intermittent regimen patients (100 mL of enteral feed during a 30- to 60-minute period of time every 8 h) reached the nutritional goal faster (P = 0.01). However, there was no difference between groups in terms of complications and mortality.
The data mentioned above suggest that a randomised controlled trial on continuous versus intermittent enteral feeding may be of practical importance in patients with acute pancreatitis.
7. Further Directions
Findings from the randomised controlled trials discussed above have highlighted a number of major areas that require further investigations.
7.1. Further Randomised Trials of Nasogastric Tube Feeding in Patients with Acute Pancreatitis
Nasogastric tube feeding appears to be safe and well tolerated in the vast majority of patients with acute pancreatitis. However, the evidence base is limited, with only four rather small randomised controlled trials of nasogastric tube feeding. Larger-scale randomised controlled trials looking at the effect of nasogastric tube feeding in patients with acute pancreatitis are desirable. In particular, a quality randomised controlled trial is needed to investigate whether nasogastric tube feeding can prevent the progression of severity in patients with acute pancreatitis [122, 123]. The potential benefits which enteral nutrition may offer are dual, that is, improvement in tolerance of oral refeeding and prevention of progression in severity of acute pancreatitis (Figure 1). A further randomised controlled trial should also determine whether a decrease in the risk of pain relapse results in a statistically significant reduction in length of hospitalisation and, eventually, overall cost of treatment.
Figure 1.
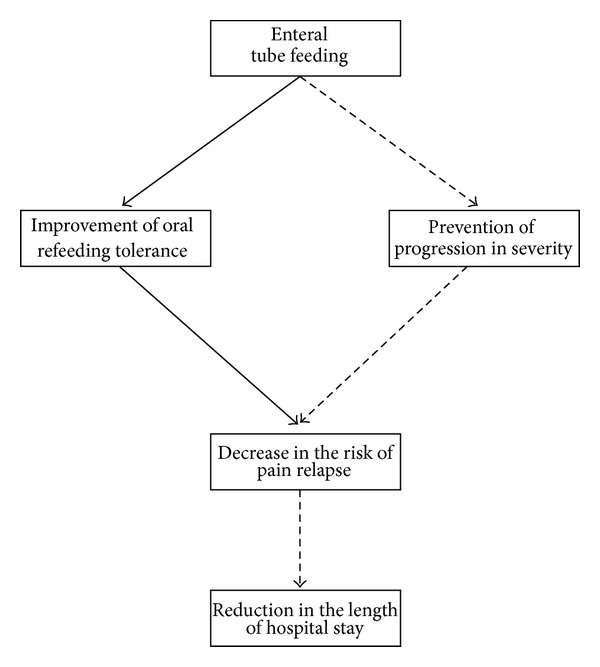
Hypotheses that need to be evaluated (dashed line) in further randomised controlled trials of nasogastric tube feeding in patients with acute pancreatitis.
A particular emphasis in future studies must be in relation to study populations. Given that the use of predictive criteria of severity was advocated by the Atlanta classification, the majority of randomised controlled trials conducted to date have enrolled patients on the basis of various criteria of predicted severity with different thresholds (Ranson score > 3, Acute Physiology And Chronic Health Evaluation II score > 8, Acute Physiology And Chronic Health Evaluation II score > 7, Acute Physiology And Chronic Health Evaluation II score > 6, C reactive protein > 150, C reactive protein > 120). Unfortunately, the field is hampered by suboptimal definitions of that for which prediction is sought. A recent systematic review showed that there was remarkable heterogeneity between the studies in this regard [124]. The endpoints for the prediction of severity included multiple factor prognostic scores (Acute Physiology And Chronic Health Evaluation II ≥ 8 and/or Ranson ≥ 3), death, local, and/or systemic complications (as defined by the Atlanta symposium), Japanese criteria of severity, organ failure, pancreatic necrosis, infected pancreatic necrosis, length of hospitalisation, intensive care unit admission, and need for surgery. This is one of the main reasons why modern prognostic scores can, on average, correctly predict severity in only 60%–80% of patients. Moreover, a randomised controlled trial from a well-known group with an interest in acute pancreatitis employed an Acute Physiology And Chronic Health Evaluation II score ≥ 8 to enrol patients with a predicted severe course of acute pancreatitis and found that actual severe acute pancreatitis (as defined by the Atlanta symposium) occurred in only 46% [41]. That is inferior to tossing a coin and definitely more labour intensive and time consuming! The important implication for nutritional management of patients with acute pancreatitis is that the exact (actual) population of patients with acute pancreatitis who benefit from enteral nutrition is still largely unknown [125].
That is why future studies in the field should employ the new classification of severity, which is based on actual determinants of severity, to enrol patients in the trial and assess the effect of treatment [126–128]. This will ensure that nutritional management is tailored to patients with each category of actual severity. In particular, randomised controlled trials are needed to investigate the optimal nutritional management in the most challenging patients, that is, those with severe and critical acute pancreatitis. Given that these patients are not prevalent in routine practice, a multicentre (international) collaboration will be required.
7.2. Pilot Randomised Trial of Early Nasogastric Tube Feeding versus Oral Feeding Ad Libitum in Patients with Mild-to-Moderate Acute Pancreatitis
The benefits of early (within 24 hours of hospital admission) nasogastric tube feeding in comparison with a nil-by-mouth regimen were demonstrated in the EFAP (Enteral Feeding in Acute Pancreatitis) trial [129]. This randomised trial showed that early administration of nasogastric tube feeding is safe and does not exacerbate the course of acute pancreatitis. Furthermore, the use of nasogastric tube feeding significantly reduces the intensity and duration of initial pain and prevents pain relapse after oral refeeding. At the same time, a recent randomised controlled trial from Sweden compared early (within 24 hours of hospital admission) oral feeding ad libitum with nil-by-mouth and showed that oral feeding does not exacerbate the course of acute pancreatitis and even reduces the total length of hospital stay, but no significant effect on the intensity and duration of initial pain was observed [96]. A pilot randomised controlled trial is now warranted to compare directly the interventions used in the two trials, that is, nasogastric tube feeding and oral feeding ad libitum (Figure 2). A randomised controlled trial of this design would be of both practical and theoretical importance. From a practical perspective, it would help to determine the optimal early feeding regimen in patients with acute pancreatitis. From a theoretical perspective, it would provide a definitive answer as to whether the “pancreas rest” concept can be buried or not.
Figure 2.
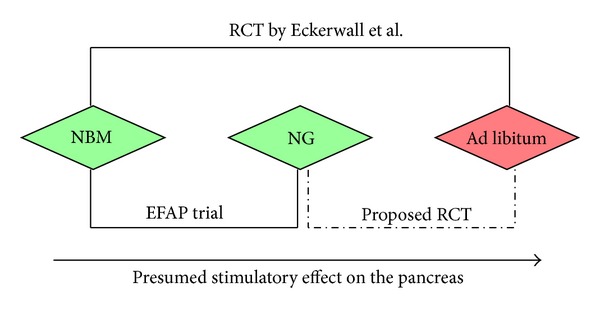
Place of proposed pilot RCT of early nasogastric tube feeding versus oral feeding ad libitum in the literature. NBM: nil-by-mouth; NG: nasogastric tube feeding; RCT: randomised controlled trial.
7.3. Definitive Randomised Controlled Trial of Fibre-Enriched Enteral Nutrition in Acute Pancreatitis
Enteral nutrition is associated with a relatively high rate of adverse effects in patients with acute pancreatitis, in particular diarrhoea. A meta-analysis of 13 randomised controlled trials comparing fibre-enriched and fibre-free enteral feeding formulations showed a significant reduction of diarrhoea in patients receiving the former [45]. This makes fibre-enriched formulations a promising and clinically relevant approach to minimise the risk of diarrhoea in patients with acute pancreatitis. To date, the effect of fibre has been evaluated in only one randomised controlled trial in patients with predicted severe acute pancreatitis [85]. That study demonstrated no cases of diarrhoea in 15 patients receiving a fibre-enriched formulation, compared with two of 15 patients receiving a fibre-free formulation. Taking into account the limited sample size of the study, an adequately powered randomised controlled trial of a fibre-enriched versus fibre-free formulation in patients with acute pancreatitis appears to be warranted.
The call for such a trial was also supported by the eagerly awaited and very disappointing results of the PROPATRIA trial [95]. A common interpretation of this study is that the use of probiotics in patients with predicted severe AP led to a significantly increased risk of intestinal ischaemia, multiple organ failure, and mortality. However, this is not entirely correct because, in fact, the intervention group in the PROPATRIA received a fibre-enriched formulation supplemented with six strains of probiotics, whereas the control group received a fibre-enriched formulation alone. Therefore, one can only conclude from this study that the given combination of probiotics and fibres was harmful, whereas the fact that mortality was only 6% in the control group and that no cases of intestinal necrosis were observed, shows that a fibre-enriched formulation is safe in patients with acute pancreatitis.
7.4. Further Studies on Immunonutrition in Acute Pancreatitis
To date, only three randomised controlled trials on the use of immunonutrition are available in the literature, and they did not demonstrate any clinical beneficial effect of enteral nutrition enriched with glutamine, arginine, and/or omega-3 fatty acids when compared with standard enteral nutrition in patients with acute pancreatitis [92, 130]. At first sight, given that the sample sizes of all the randomised controlled trials were too small, it seems that no definitive conclusions can be drawn from them. Nevertheless, an authoritative meta-analysis of several hundred critically ill and elective surgery patients, which was greater in terms of study population, found a statistically significant benefit of immunonutrition (reduced risk of infectious complications) only in the subgroup of patients who received a high-arginine-content formula. However, excessive arginine supplementation could have a potentially damaging effect on the pancreas, probably due to the excessive production of nitric oxide. It is also known that administration of omega-3 fatty acids decreases antioxidant capacity [131]. Nevertheless, the relevance of these experimental observations is difficult to evaluate in the clinical setting because immunonutrition is usually administered in a compound and it is hard to ascribe a beneficial or harmful effect of an immunonutritional formulation to any single immune-enhancing agent. Thus, further clinical and animal studies should focus on individual immune-enhancing agents, of which glutamine seems to have the greatest beneficial potential in the setting of acute pancreatitis.
7.5. Pilot Study of Antioxidant-Enriched Enteral Nutrition in Acute Pancreatitis
Although oxidative stress has been implicated as an important factor in the pathogenesis of acute pancreatitis for nearly three decades, the therapeutic effect of antioxidants in patients with acute pancreatitis has been investigated in only a few inconclusive randomised controlled trials. The only high-quality trial enrolled 43 patients with predicted severe acute pancreatitis (Acute Physiology And Chronic Health Evaluation II score ≥ 8 within 48 hours of admission) and showed no benefit of intravenous antioxidant therapy (n-acetylcysteine, selenium, and vitamin C) administered for 7 days [132]. Moreover, the study was terminated at the time of interim analysis because some data suggested that the intervention might even be harmful. Following the publication of this study in 2007, some authors rushed to conclude that “the book on the antioxidant story in the treatment of acute pancreatitis has closed” [133]. However, while the trial clearly showed that the given combination of antioxidants is not effective in patients with acute pancreatitis when administered intravenously, it is quite possible that antioxidants administered via another route will be beneficial. In particular, there is a growing body of clinical evidence from other disease settings that supplementation of enteral nutrition with antioxidants might be beneficial. Given that the benefits of standard enteral nutrition in patients with acute pancreatitis are well proven, the use of antioxidant-enriched enteral nutrition may be a sensible direction of clinical research in acute pancreatitis.
8. Conclusion
The frontiers in nutritional management of patients with acute pancreatitis continue to advance. The findings presented in this review highlight the importance of enteral nutrition in curtailing of acute inflammation of the pancreas. There is ample evidence in the literature that the use of nasojejunal tube feeding improves outcomes in patients with predicted severe course of acute pancreatitis. Several studies have demonstrated the safety and efficacy of nasogastric tube feeding in these patients. Furthermore, for the first time, it has been shown in a randomised trial that early nasogastric tube feeding may have benefits for patients with actual mild-to-moderate acute pancreatitis. Lastly, optimal enteral feeding formulations have been determined based on the best available data. Further expansion of frontiers in nutritional management of acute pancreatitis represents a formidable opportunity for improving patient care. As long ago as 1928, Bertrand Russell wrote “the extent to which beliefs are based upon evidence is very much less than believers suppose.” This still pretty much holds true today in the management of the most frequent disease of the pancreas.
Conflict of Interests
The author has no conflict of interests.
References
- 1.Goldacre MJ, Roberts SE. Hospital admission for acute pancreatitis in an English population, 1963–98: database study of incidence and mortality. British Medical Journal. 2004;328(7454):1466–1469. doi: 10.1136/bmj.328.7454.1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lankisch PG, Karimi M, Bruns A, Maisonneuve P, Lowenfels AB. Temporal trends in incidence and severity of acute pancreatitis in Lüneburg County, Germany: a population-based study. Pancreatology. 2009;9(4):420–426. doi: 10.1159/000209217. [DOI] [PubMed] [Google Scholar]
- 3.Sekimoto M, Takada T, Kawarada Y, et al. JPN Guidelines for the management of acute pancreatitis: epidemiology, etiology, natural history, and outcome predictors in acute pancreatitis. Journal of Hepato-Biliary-Pancreatic Surgery. 2006;13(1):10–24. doi: 10.1007/s00534-005-1047-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phillips A, Lawes C, Ng A, Cooper G, Collins J, Windsor JA. Ethnic disparity of acute pancreatitis in South Auckland. New Zealand Medical Journal. 2003;116(1168):5–6. [Google Scholar]
- 5.Birgisson H, Möller PH, Birgisson S, et al. Acute pancreatitis: a prospective study of its incidence, aetiology, severity, and mortality in Iceland. European Journal of Surgery. 2002;168(5):278–282. doi: 10.1002/ejs.46. [DOI] [PubMed] [Google Scholar]
- 6.Halvorsen F-A, Ritland S. Acute pancreatitis in Buskerud County, Norway: incidence and etiology. Scandinavian Journal of Gastroenterology. 1996;31(4):411–414. doi: 10.3109/00365529609006419. [DOI] [PubMed] [Google Scholar]
- 7.Fagenholz PJ, Castillo CF-D, Harris NS, Pelletier AJ, Camargo CA., Jr. Increasing United States Hospital Admissions for Acute Pancreatitis, 1988-2003. Annals of Epidemiology. 2007;17(7):491–e1. doi: 10.1016/j.annepidem.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 8.Jaakkola M, Nordback I. Pancreatitis in Finland between 1970 and 1989. Gut. 1993;34(9):1255–1260. doi: 10.1136/gut.34.9.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Floyd AK, Pedersen L, Lauge Nielsen G, Thorlacius-Ussing O, Sorensen HT. Secular trends in incidence and 30-day case fatality of acute pancreatitis in North Jutland County, Denmark: a register-based study from 1981–2000. Scandinavian Journal of Gastroenterology. 2002;37(12):1461–1465. doi: 10.1080/003655202762671369. [DOI] [PubMed] [Google Scholar]
- 10.Lindkvist B, Appelros S, Manjer J, Borgström A. Trends in incidence of acute pancreatitis in a Swedish population: is there really an increase? Clinical Gastroenterology and Hepatology. 2004;2(9):831–837. doi: 10.1016/s1542-3565(04)00355-6. [DOI] [PubMed] [Google Scholar]
- 11.Eland IA, Sturkenboom MJCM, Wilson JHP, Stricker BHC. Incidence and mortality of acute pancreatitis between 1985 and 1995. Scandinavian Journal of Gastroenterology. 2000;35(10):1110–1116. doi: 10.1080/003655200451261. [DOI] [PubMed] [Google Scholar]
- 12.Fagenholz PJ, Fernández-Del Castillo C, Harris NS, Pelletier AJ, Camargo CA., Jr. Direct medical costs of acute pancreatitis hospitalizations in the United States. Pancreas. 2007;35(4):302–307. doi: 10.1097/MPA.0b013e3180cac24b. [DOI] [PubMed] [Google Scholar]
- 13.Frey CF. Classification of pancreatitis: state-of-the-art, 1986. Pancreas. 1986;1(1):62–68. doi: 10.1097/00006676-198601000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Sarner M, Cotton PB. Classification of pancreatitis. Gut. 1984;25(7):756–759. doi: 10.1136/gut.25.7.756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singer MV, Gyr K, Sarles H. Revised classification of pancreatitis. Report of the Second International Symposium on the Classification of Pancreatitis in Marseille, France, March 28–30, 1984. Gastroenterology. 1985;89(3):683–685. [PubMed] [Google Scholar]
- 16.Sarles H, Adler G, Dani R, et al. The pancreatitis classification of Marseilles-Rome 1988. Scandinavian Journal of Gastroenterology. 1989;24(6):641–642. doi: 10.3109/00365528909093102. [DOI] [PubMed] [Google Scholar]
- 17.Bradley EL, III, Frey CF. A clinically based classification system for acute pancreatitis: summary of the International Symposium on Acute Pancreatitis, Atlanta, Ga, September 11 through 13, 1992. Archives of Surgery. 1993;128(5):586–590. doi: 10.1001/archsurg.1993.01420170122019. [DOI] [PubMed] [Google Scholar]
- 18.Larvin M, McMahon MJ. APACHE-II score for assessment and monitoring of acute pancreatitis. The Lancet. 1989;2(8656):201–205. doi: 10.1016/s0140-6736(89)90381-4. [DOI] [PubMed] [Google Scholar]
- 19.Ranson JHC, Rifkind KM, Roses DF. Objective early identification of severe acute pancreatitis. American Journal of Gastroenterology. 1974;61(6):443–451. [PubMed] [Google Scholar]
- 20.The Working Group. Revision of the Atlanta classification of acute pancreatitis. 2009, http://pancreasclub.com/wp-content/uploads/2011/11/AtlantaClassification.pdf.
- 21.Bhatia M. Novel therapeutic targets for acute pancreatitis and associated multiple organ dysfunction syndrome. Current Drug Targets—Inflammation & Allergy. 2002;1(4):343–351. doi: 10.2174/1568010023344517. [DOI] [PubMed] [Google Scholar]
- 22.Windsor JA, Hammodat H. Metabolic management of severe acute pancreatitis. World Journal of Surgery. 2000;24(6):664–672. doi: 10.1007/s002689910108. [DOI] [PubMed] [Google Scholar]
- 23.Blamey SL, Finlay IG, Carter DC, Imrie CW. Analgesia in acute pancreatitis: comparison of buprenorphine and pethidine. British Medical Journal. 1984;288(6429):1494–1495. doi: 10.1136/bmj.288.6429.1494-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ebbehoj N, Friis J, Svendsen B. Indomethacin treatment of acute pancreatitis. A controlled double-blind trial. Scandinavian Journal of Gastroenterology. 1985;20(7):798–800. doi: 10.3109/00365528509088825. [DOI] [PubMed] [Google Scholar]
- 25.Jakobs R, Adamek MU, Von Bubnoff AC, Riemann JF. Buprenorphine or procaine for pain relief in acute pancreatitis. A prospective randomized study. Scandinavian Journal of Gastroenterology. 2000;35(12):1319–1323. doi: 10.1080/003655200453692. [DOI] [PubMed] [Google Scholar]
- 26.Kahl S, Zimmermann S, Pross M, Schulz H-U, Schmidt U, Malfertheiner P. Procaine hydrochloride fails to relieve pain in patients with acute pancreatitis. Digestion. 2004;69(1):5–9. doi: 10.1159/000076541. [DOI] [PubMed] [Google Scholar]
- 27.Peiró AM, Martínez J, Martínez E, et al. Efficacy and tolerance of metamizole versus morphine for acute pancreatitis pain. Pancreatology. 2008;8(1):25–29. doi: 10.1159/000114852. [DOI] [PubMed] [Google Scholar]
- 28.Stevens M, Esler R, Asher G. Transdermal fentanyl for the management of acute pancreatitis pain. Applied Nursing Research. 2002;15(2):102–110. doi: 10.1053/apnr.2002.29532. [DOI] [PubMed] [Google Scholar]
- 29.Loveday BPT, Srinivasa S, Vather R, et al. High quantity and variable quality of guidelines for acute pancreatitis: a systematic review. American Journal of Gastroenterology. 2010;105(7):1466–1476. doi: 10.1038/ajg.2010.137. [DOI] [PubMed] [Google Scholar]
- 30.Gardner TB, Vege SS, Pearson RK, Chari ST. Fluid Resuscitation in Acute Pancreatitis. Clinical Gastroenterology and Hepatology. 2008;6(10):1070–1076. doi: 10.1016/j.cgh.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 31.Petrov MS, Van Santvoort HC, Besselink MGH, Van Der Heijden GJMG, Van Erpecum KJ, Gooszen HG. Early endoscopic retrograde cholangiopancreatography versus conservative management in acute biliary pancreatitis without cholangitis: a meta-analysis of randomized trials. Annals of Surgery. 2008;247(2):250–257. doi: 10.1097/SLA.0b013e31815edddd. [DOI] [PubMed] [Google Scholar]
- 32.Petrov MS, Uchugina AF, Kukosh MV. Does endoscopic retrograde cholangiopancreatography reduce the risk of local pancreatic complications in acute pancreatitis? A systematic review and metaanalysis. Surgical Endoscopy and Other Interventional Techniques. 2008;22(11):2338–2343. doi: 10.1007/s00464-008-9964-2. [DOI] [PubMed] [Google Scholar]
- 33.Petrov MS, Van Santvoort HC, Besselink MGH, Van Der Heijden GJMG, Windsor JA, Gooszen HG. Enteral nutrition and the risk of mortality and infectious complications in patients with severe acute pancreatitis: a meta-analysis of randomized trials. Archives of Surgery. 2008;143(11):1111–1117. doi: 10.1001/archsurg.143.11.1111. [DOI] [PubMed] [Google Scholar]
- 34.Muddana V, Whitcomb DC, Papachristou GI. Current management and novel insights in acute pancreatitis. Expert Review of Gastroenterology and Hepatology. 2009;3(4):435–444. doi: 10.1586/egh.09.27. [DOI] [PubMed] [Google Scholar]
- 35.Mao E-Q, Fei J, Peng Y-B, Huang J, Tang Y-Q, Zhang S-D. Rapid hemodilution is associated with increased sepsis and mortality among patients with severe acute pancreatitis. Chinese Medical Journal. 2010;123(13):1639–1644. [PubMed] [Google Scholar]
- 36.Mao E-Q, Tang Y-Q, Fei J, et al. Fluid therapy for severe acute pancreatitis in acute response stage. Chinese Medical Journal. 2009;122(2):169–173. [PubMed] [Google Scholar]
- 37.Wu BU, Hwang JQ, Gardner TH, et al. Lactated Ringer's solution reduces systemic inflammation compared with saline in patients with acute pancreatitis. Clinical Gastroenterology and Hepatology. 2011;9(8):710–707. doi: 10.1016/j.cgh.2011.04.026. [DOI] [PubMed] [Google Scholar]
- 38.Howes R, Zuidema GD, Cameron JL. Evaluation of prophylactic antibiotics in acute pancreatitis. Journal of Surgical Research. 1975;18(2):197–200. doi: 10.1016/0022-4804(75)90016-5. [DOI] [PubMed] [Google Scholar]
- 39.Craig RM, Dordal E, Myles L. The use of ampicillin in acute pancreatitis. Annals of Internal Medicine. 1975;83(6):831–832. doi: 10.7326/0003-4819-83-6-831. [DOI] [PubMed] [Google Scholar]
- 40.Powell JJ, Murchison JT, Fearon KCH, Ross JA, Siriwardena AK. Randomized controlled trial of the effect of early enteral nutrition on markers of the inflammatory response in predicted severe acute pancreatitis. British Journal of Surgery. 2000;87(10):1375–1381. doi: 10.1046/j.1365-2168.2000.01558.x. [DOI] [PubMed] [Google Scholar]
- 41.Eckerwall GE, Axelsson JB, Andersson RG. Early nasogastric feeding in predicted severe acute pancreatitis: a clinical, randomized study. Annals of Surgery. 2006;244(6):959–965. doi: 10.1097/01.sla.0000246866.01930.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Windsor ACJ, Kanwar S, Li AGK, et al. Compared with parenteral nutrition, enteral feeding attenuates the acute phase response and improves disease severity in acute pancreatitis. Gut. 1998;42(3):431–435. doi: 10.1136/gut.42.3.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gupta R, Patel K, Calder PC, Yaqoob P, Primrose JN, Johnson CD. A randomised clinical trial to assess the effect of total enteral and total parenteral nutritional support on metabolic, inflammatory and oxidative markers in patients with predicted severe acute pancreatitis (APACHE II ≥6) Pancreatology. 2003;3(5):406–413. doi: 10.1159/000073657. [DOI] [PubMed] [Google Scholar]
- 44.Sainio V, Kemppainen E, Puolakkainen P, et al. Early antibiotic treatment in acute necrotising pancreatitis. The Lancet. 1995;346(8976):663–667. doi: 10.1016/s0140-6736(95)92280-6. [DOI] [PubMed] [Google Scholar]
- 45.Delcenserie R, Yzet T, Ducroix JP. Prophylactic antibiotics in treatment of severe acute alcoholic pancreatitis. Pancreas. 1996;13(2):198–201. [PubMed] [Google Scholar]
- 46.Schwarz M, Isenmann R, Meyer H, Beger HG. Antibiotics in necrotizing pancreatitis. Results of a controlled study. Deutsche Medizinische Wochenschrift. 1997;122(12):356–361. doi: 10.1055/s-2008-1047621. (Ger). [DOI] [PubMed] [Google Scholar]
- 47.Røkke O, Harbitz TB, Liljedal J, et al. Early treatment of severe pancreatitis with imipenem: a prospective randomized clinical trial. Scandinavian Journal of Gastroenterology. 2007;42(6):771–776. doi: 10.1080/00365520601173855. [DOI] [PubMed] [Google Scholar]
- 48.Xue P, Deng L-H, Zhang Z-D, et al. Effect of antibiotic prophylaxis on acute necrotizing pancreatitis: results of a randomized controlled trial. Journal of Gastroenterology and Hepatology. 2009;24(5):736–742. doi: 10.1111/j.1440-1746.2008.05758.x. [DOI] [PubMed] [Google Scholar]
- 49.Špičák J, Hejtmánková S, Hubaczová M, et al. Antibiotic prophylaxis of infectious complications of acute pancreatitis—the results of randomised study by meropenem. Ceska a Slovenska Gastroenterologie a Hepatologie. 2003;57(6):222–227. [Google Scholar]
- 50.Isenmann R, Rünzi M, Kron M, et al. Prophylactic antibiotic treatment in patients with predicted severe acute pancreatitis: a placebo-controlled, double-blind trial. Gastroenterology. 2004;126(4):997–1004. doi: 10.1053/j.gastro.2003.12.050. [DOI] [PubMed] [Google Scholar]
- 51.Dellinger EP, Tellado JM, Soto NE, et al. Early antibiotic treatment for severe acute necrotizing pancreatitis: a randomized, double-blind, placebo-controlled study. Annals of Surgery. 2007;245(5):674–683. doi: 10.1097/01.sla.0000250414.09255.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jiang K, Chen X-Z, Xia Q, Tang W-F, Wang L. Early nasogastric enteral nutrition for severe acute pancreatitis: a systematic review. World Journal of Gastroenterology. 2007;13(39):5253–5260. doi: 10.3748/wjg.v13.i39.5253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Petrov MS, Correia MITD, Windsor JA. Nasogastric tube feeding in predicted severe acute pancreatitis. A systematic review of the literature to determine safety and tolerance. Journal of the Pancreas. 2008;9(4):440–448. [PubMed] [Google Scholar]
- 54.Avard B, Fergusson J. Necrotizing pancreatitis and antibiotic prophylaxis. to use or not to use. that is the question. Journal of Gastroenterology and Hepatology. 2009;24(5):710–711. doi: 10.1111/j.1440-1746.2009.05837.x. [DOI] [PubMed] [Google Scholar]
- 55.Howard TJ. As good as it gets: the study of prophylactic antibiotics in severe acute pancreatitis. Annals of Surgery. 2007;245(5):684–685. doi: 10.1097/01.sla.0000261458.39058.fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Petrov MS. Meta-analyses on the prophylactic use of antibiotics in acute pancreatitis: many are called but few are chosen. American Journal of Gastroenterology. 2008;103(7):1837–1838. doi: 10.1111/j.1572-0241.2008.01959_5.x. [DOI] [PubMed] [Google Scholar]
- 57.Bai Y, Gao J, Zou D-W, Li Z-S. Prophylactic antibiotics cannot reduce infected pancreatic necrosis and mortality in acute necrotizing pancreatitis: evidence from a meta-analysis of randomized controlled trials. American Journal of Gastroenterology. 2008;103(1):104–110. doi: 10.1111/j.1572-0241.2007.01575.x. [DOI] [PubMed] [Google Scholar]
- 58.Eatock FC, Chong P, Menezes N, et al. A randomized study of early nasogastric versus nasojejunal feeding in severe acute pancreatitis. American Journal of Gastroenterology. 2005;100(2):432–439. doi: 10.1111/j.1572-0241.2005.40587.x. [DOI] [PubMed] [Google Scholar]
- 59.Kumar A, Singh N, Prakash S, Saraya A, Joshi YK. Early enteral nutrition in severe acute pancreatitis: a prospective randomized controlled trial comparing nasojejunal and nasogastric routes. Journal of Clinical Gastroenterology. 2006;40(5):431–434. doi: 10.1097/00004836-200605000-00013. [DOI] [PubMed] [Google Scholar]
- 60.Yadav D, Lowenfels AB. Trends in the epidemiology of the first attack of acute pancreatitis: a systematic review. Pancreas. 2006;33(4):323–330. doi: 10.1097/01.mpa.0000236733.31617.52. [DOI] [PubMed] [Google Scholar]
- 61.Fenton-Lee D, Imrie CW. Pancreatic necrosis: assessment of outcome related to quality of life and cost of management. British Journal of Surgery. 1993;80(12):1579–1582. doi: 10.1002/bjs.1800801228. [DOI] [PubMed] [Google Scholar]
- 62.Finch WT, Sawyers JL, Schenker S. A prospective study to determine the efficacy of antibiotics in acute pancreatitis. Annals of Surgery. 1976;183(6):667–671. doi: 10.1097/00000658-197606000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pederzoli P, Bassi C, Vesentini S, Campedelli A. A randomized multicenter clinical trial of antibiotic prophylaxis of septic complications in acute necrotizing pancreatitis with imipenem. Surgery Gynecology and Obstetrics. 1993;176(5):480–483. [PubMed] [Google Scholar]
- 64.Singh N, Sharma B, Sharma M, et al. Evaluation of early enteral feeding through nasogastric and nasojejunal tube in severe acute pancreatitis: a noninferiority randomized controlled trial. Pancreas. 2012;41(1):153–159. doi: 10.1097/MPA.0b013e318221c4a8. [DOI] [PubMed] [Google Scholar]
- 65.O'Keefe SJ, McClave SA. Feeding the injured pancreas. Gastroenterology. 2005;129(3):1129–1130. doi: 10.1053/j.gastro.2005.06.077. [DOI] [PubMed] [Google Scholar]
- 66.O'Keefe SJ, Lee RB, Anderson FP, et al. Physiological effects of enteral and parenteral feeding on pancreaticobiliary secretion in humans. American Journal of Physiology. 2003;284(1):G27–G36. doi: 10.1152/ajpgi.00155.2002. [DOI] [PubMed] [Google Scholar]
- 67.Mazaki T, Ishii Y, Takayama T. Meta-analysis of prophylactic antibiotic use in acute necrotizing pancreatitis. British Journal of Surgery. 2006;93(6):674–684. doi: 10.1002/bjs.5389. [DOI] [PubMed] [Google Scholar]
- 68.Villatoro E, Bassi C, Larvin M. Antibiotic therapy for prophylaxis against infection of pancreatic necrosis in acute pancreatitis. Cochrane Database of Systematic Reviews. 2006;(4) doi: 10.1002/14651858.CD002941.pub2.CD002941 [DOI] [PubMed] [Google Scholar]
- 69.Boreham B, Ammori BJ. A prospective evaluation of pancreatic exocrine function in patients with acute pancreatitis: correlation with extent of necrosis and pancreatic endocrine insufficiency. Pancreatology. 2003;3(4):303–308. doi: 10.1159/000071768. [DOI] [PubMed] [Google Scholar]
- 70.Kalfarentzos F, Kehagias J, Mead N, Kokkinis K, Gogos CA. Enteral nutrition is superior to parenteral nutrition in severe acute pancreatitis: results of a randomized prospective trial. British Journal of Surgery. 1997;84(12):1665–1669. [PubMed] [Google Scholar]
- 71.Louie BE, Noseworthy T, Hailey D, Gramlich LM, Jacobs P, Warnock GL. 2004 MacLean-Mueller Prize Enteral or parenteral nutrition for severe pancreatitis: a randomized controlled trial and health technology assessment. Canadian Journal of Surgery. 2005;48(4):298–306. [PMC free article] [PubMed] [Google Scholar]
- 72.Petrov MS, Kukosh MV, Emelyanov NV. A randomized controlled trial of enteral versus parenteral feeding in patients with predicted severe acute pancreatitis shows a significant reduction in mortality and in infected pancreatic complications with total enteral nutrition. Digestive Surgery. 2007;23(5-6):336–345. doi: 10.1159/000097949. [DOI] [PubMed] [Google Scholar]
- 73.Casas M, Mora J, Fort E, et al. Total enteral nutrition vs. total parenteral nutrition in patients with severe acute pancreatitis. Revista Espanola de Enfermedades Digestivas. 2007;99(5):264–269. doi: 10.4321/s1130-01082007000500004. [DOI] [PubMed] [Google Scholar]
- 74.Doley RP, Yadav TD, Wig JD, et al. Enteral nutrition in severe acute pancreatitis. Journal of the Pancreas. 2009;10(2):157–162. [PubMed] [Google Scholar]
- 75.Wu X-M, Ji K-Q, Wang H-Y, Li G-F, Zang B, Chen W-M. Total enteral nutrition in prevention of pancreatic necrotic infection in severe acute pancreatitis. Pancreas. 2010;39(2):248–251. doi: 10.1097/MPA.0b013e3181bd6370. [DOI] [PubMed] [Google Scholar]
- 76.Eatock FC, Brombacher GD, Steven A, Imrie CW, McKay CJ, Carter R. Nasogastric feeding in severe acute pancreatitis may be practical and safe. International Journal of Pancreatology. 2000;28(1):25–29. doi: 10.1385/IJGC:28:1:23. [DOI] [PubMed] [Google Scholar]
- 77.Mcclave SA, Greene LM, Snider HL, et al. Comparison of the safety of early enteral vs parenteral nutrition in mild acute pancreatitis. Journal of Parenteral and Enteral Nutrition. 1997;21(1):14–20. doi: 10.1177/014860719702100114. [DOI] [PubMed] [Google Scholar]
- 78.Hallay J, Kovacs G, Kiss Sz S, et al. Changes in the nutritional state and immune-serological parameters of esophagectomized patients fed jejunally with glutamine-poor and glutamine-rich nutriments. Hepatogastroenterology. 2002;49(48):1555–1559. [PubMed] [Google Scholar]
- 79.Oláah A, Pardavi G, Beláagyi T, Nagy A, Issekutz Á, Mohamed GE. Early nasojejunal feeding in acute pancreatitis is associated with a lower complication rate. Nutrition. 2002;18(3):259–262. doi: 10.1016/s0899-9007(01)00755-9. [DOI] [PubMed] [Google Scholar]
- 80.Abou-Assi S, Craig K, O'Keefe SJ. Hypocaloric jejunal feeding is better than total parenteral nutrition in acute pancreatitis: results of a randomized comparative study. The American Journal of Gastroenterology. 2002;97(9):2255–2262. doi: 10.1111/j.1572-0241.2002.05979.x. [DOI] [PubMed] [Google Scholar]
- 81.Oláh A, Belágyi T, Issekutz Á, Gamal ME, Bengmark S. Randomized clinical trial of specific lactobacillus and fibre supplement to early enteral nutrition in patients with acute pancreatitis. British Journal of Surgery. 2002;89(9):1103–1107. doi: 10.1046/j.1365-2168.2002.02189.x. [DOI] [PubMed] [Google Scholar]
- 82.Lasztity N, Hamvas J, Biró L, et al. Effect of enterally administered n-3 polyunsaturated fatty acids in acute pancreatitis—a prospective randomized clinical trial. Clinical Nutrition. 2005;24(2):198–205. doi: 10.1016/j.clnu.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 83.Pearce CB, Sadek SA, Walters AM, et al. A double-blind, randomised, controlled trial to study the effects of an enteral feed supplemented with glutamine, arginine, and omega-3 fatty acid in predicted acute severe pancreatitis. Journal of the Pancreas. 2006;7(4):361–371. [PubMed] [Google Scholar]
- 84.Tiengou L-E, Gloro R, Pouzoulet J, et al. Semi-elemental formula or polymeric formula: is there a better choice for enteral nutrition in acute pancreatitis? Randomized comparative study. Journal of Parenteral and Enteral Nutrition. 2006;30(1):1–5. doi: 10.1177/014860710603000101. [DOI] [PubMed] [Google Scholar]
- 85.Karakan T, Ergun M, Dogan I, Cindoruk M, Unal S. Comparison of early enteral nutrition in severe acute pancreatitis with prebiotic fiber supplementation versus standard enteral solution: a prospective randomized double-blind study. World Journal of Gastroenterology. 2007;13(19):2733–2737. doi: 10.3748/wjg.v13.i19.2733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Besselink MGH, Van Santvoort HC, Buskens E, et al. Probiotic prophylaxis in patients with predicted severe acute pancreatitis: a randomised, double-blind, placebo-controlled trial. Nederlands Tijdschrift voor Geneeskunde. 2008;152(12):685–696. [PubMed] [Google Scholar]
- 87.Qin H-L, Zheng J-J, Tong D-N, et al. Effect of Lactobacillus plantarum enteral feeding on the gut permeability and septic complications in the patients with acute pancreatitis. European Journal of Clinical Nutrition. 2008;62(7):923–930. doi: 10.1038/sj.ejcn.1602792. [DOI] [PubMed] [Google Scholar]
- 88.Petrov MS, Pylypchuk RD, Emelyanov NV. Systematic review: nutritional support in acute pancreatitis. Alimentary Pharmacology and Therapeutics. 2008;28(6):704–712. doi: 10.1111/j.1365-2036.2008.03786.x. [DOI] [PubMed] [Google Scholar]
- 89.Petrov MS, Loveday BPT, Pylypchuk RD, McIlroy K, Phillips ARJ, Windsor JA. Systematic review and meta-analysis of enteral nutrition formulations in acute pancreatitis. British Journal of Surgery. 2009;96(11):1243–1252. doi: 10.1002/bjs.6862. [DOI] [PubMed] [Google Scholar]
- 90.Fan S-T, Lai ECS, Mok FPT, Lo C-M, Zheng S-S, Wong J. Early treatment of acute biliary pancreatitis by endoscopic papillotomy. The New England Journal of Medicine. 1993;328(4):228–232. doi: 10.1056/NEJM199301283280402. [DOI] [PubMed] [Google Scholar]
- 91.Neoptolemos JP, London NJ, James D, Carr-Locke DL, Bailey IA, Fossard DP. Controlled trial of urgent endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy versus conservative treatment for acute pancreatitis due to gallstones. The Lancet. 1988;2(8618):979–983. doi: 10.1016/s0140-6736(88)90740-4. [DOI] [PubMed] [Google Scholar]
- 92.Petrov MS. Early use of ERCP in acute biliary pancreatitis with(out) jaundice: an unjaundiced view. Journal of the Pancreas. 2009;10(1):1–7. [PubMed] [Google Scholar]
- 93.Acosta JM, Galli OMR, Rossi R, Chinellato AV, Pellegrini CA. Effect of duration of ampullary gallstone obstruction on severity of lesions of acute pancreatitis. Journal of the American College of Surgeons. 1997;184(5):499–504. [PubMed] [Google Scholar]
- 94.Fölsch UR, Nitsche R, Lüdtke R, Hilgers RA, Creutzfeldt W. Early ERCP and papillotomy compared with conservative treatment for acute biliary pancreatitis. The New England Journal of Medicine. 1997;336(4):237–242. doi: 10.1056/NEJM199701233360401. [DOI] [PubMed] [Google Scholar]
- 95.Oría A, Cimmino D, Ocampo C, et al. Early endoscopic intervention versus early conservative management in patients with acute gallstone pancreatitis and biliopancreatic obstruction: a randomized clinical trial. Annals of Surgery. 2007;245(1):10–17. doi: 10.1097/01.sla.0000232539.88254.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Krumberger JM. Acute pancreatitis. Critical Care Nursing Clinics of North America. 1993;5(1):185–202. [PubMed] [Google Scholar]
- 97.Roberts PR. Nutritional support in acute pancreatitis: an update on management issues. Seminars in Respiratory and Critical Care Medicine. 2001;22(1):29–34. doi: 10.1055/s-2001-13838. [DOI] [PubMed] [Google Scholar]
- 98.Ammori BJ. Role of the gut in the course of severe acute pancreatitis. Pancreas. 2003;26(2):122–129. doi: 10.1097/00006676-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 99.Dervenis C. Enteral nutrition in severe acute pancreatitis: future development. Journal of the Pancreas. 2004;5(2):60–63. [PubMed] [Google Scholar]
- 100.Doley RP, Yadav TD, Wig JD, et al. Enteral nutrition in severe acute pancreatitis. Journal of the Pancreas. 2009;10(2):157–162. [PubMed] [Google Scholar]
- 101.Quan H, Wang X, Guo C. A meta-analysis of enteral nutrition and total parenteral nutrition in patients with acute pancreatitis. Gastroenterology Research and Practice. 2011;2011:9 pages. doi: 10.1155/2011/698248.698248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Marik PE, Zaloga GP. Meta-analysis of parenteral-nutrition versus enteral nutrition in patients with acute pancreatitis. British Medical Journal. 2004;328(7453):1407–1410. doi: 10.1136/bmj.38118.593900.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Al-Omran M, Albalawi ZH, Tashkandi MF, Al-Ansary LA. Enteral versus parenteral nutrition for acute pancreatitis. Cochrane Database of Systematic Reviews. 2010;(1) doi: 10.1002/14651858.CD002837.pub2.CD002837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lehocky P, Sarr MG. Early enteral feeding in severe acute pancreatitis: can it prevent secondary pancreatic (super) infection? Digestive Surgery. 2000;17(6):571–577. doi: 10.1159/000051964. [DOI] [PubMed] [Google Scholar]
- 105.Ammori BJ, Leeder PC, King RFGJ, et al. Early increase in intestinal permeability in patients with severe acute pancreatitis: correlation with endotoxemia, organ failure, and mortality. Journal of Gastrointestinal Surgery. 1999;3(3):252–262. doi: 10.1016/s1091-255x(99)80067-5. [DOI] [PubMed] [Google Scholar]
- 106.Nagpal K, Minocha VR, Agrawal V, Kapur S. Evaluation of intestinal mucosal permeability function in patients with acute pancreatitis. American Journal of Surgery. 2006;192(1):24–28. doi: 10.1016/j.amjsurg.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 107.Xiong G-S, Wu S-M, Wang Z-H. Role of prophylactic antibiotic administration in severe acute pancreatitis: a meta-analysis. Medical Principles and Practice. 2006;15(2):106–110. doi: 10.1159/000090913. [DOI] [PubMed] [Google Scholar]
- 108.Duerksen DR, Bector S, Parry D, Yaffe C, Vajcner A, Lipschitz J. A comparison of the effect of elemental and immune-enhancing polymeric jejunal feeding on exocrine pancreatic function. Journal of Parenteral and Enteral Nutrition. 2002;26(3):205–208. doi: 10.1177/0148607102026003205. [DOI] [PubMed] [Google Scholar]
- 109.Buter A, Imrie CW, Carter CR, Evans S, McKay CJ. Dynamic nature of early organ dysfunction determines outcome in acute pancreatitis. British Journal of Surgery. 2002;89(3):298–302. doi: 10.1046/j.0007-1323.2001.02025.x. [DOI] [PubMed] [Google Scholar]
- 110.Johnson CD, Abu-Hilal M. Persistent organ failure during the first week as a marker of fatal outcome in acute pancreatitis. Gut. 2004;53(9):1340–1344. doi: 10.1136/gut.2004.039883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Fernandez-Banares F, Cabre E, Esteve-Comas M, Gassull MA. How effective is enteral nutrition in inducing clinical remission in active Crohn’s disease? A meta-analysis of the randomized clinical trials. Journal of Parenteral and Enteral Nutrition. 1995;19(5):356–364. doi: 10.1177/0148607195019005356. [DOI] [PubMed] [Google Scholar]
- 112.Zachos M, Tondeur M, Griffiths AM. Enteral nutritional therapy for induction of remission in Crohn’s disease. Cochrane Database of Systematic Reviews. 2007;(1) doi: 10.1002/14651858.CD000542.pub2.CD000542 [DOI] [PubMed] [Google Scholar]
- 113.Pannala R, Kidd M, Modlin IM. Acute pancreatitis: a historical perspective. Pancreas. 2009;38(4):355–366. doi: 10.1097/MPA.0b013e318199161c. [DOI] [PubMed] [Google Scholar]
- 114.Xue P, Deng L-H, Zhang Z-D, et al. Infectious complications in patients with severe acute pancreatitis. Digestive Diseases and Sciences. 2009;54(12):2748–2753. doi: 10.1007/s10620-008-0668-1. [DOI] [PubMed] [Google Scholar]
- 115.Chiarelli A, Enzi G, Casadei A, Baggio B, Valerio A, Mazzoleni F. Very early nutrition supplementation in burned patients. American Journal of Clinical Nutrition. 1990;51(6):1035–1039. doi: 10.1093/ajcn/51.6.1035. [DOI] [PubMed] [Google Scholar]
- 116.Grahm TW, Zadrozny DB, Harrington T. The benefits of early jejunal hyperalimentation in the head-injured patient. Neurosurgery. 1989;25(5):729–735. doi: 10.1097/00006123-198911000-00007. [DOI] [PubMed] [Google Scholar]
- 117.Marik PE, Zaloga GP. Gastric versus post-pyloric feeding: a systematic review. Critical Care. 2003;7(3):R46–R51. doi: 10.1186/cc2190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Garg PK, Madan K, Pande GK, et al. Association of extent and infection of pancreatic necrosis with organ failure and death in acute necrotizing pancreatitis. Clinical Gastroenterology and Hepatology. 2005;3(2):159–166. doi: 10.1016/s1542-3565(04)00665-2. [DOI] [PubMed] [Google Scholar]
- 119.Dionigi R, Rovera F, Dionigi G, Diurni M, Cuffari S. Infected pancreatic necrosis. Surgical Infections. 2006;7(2):S-49–S-52. doi: 10.1089/sur.2006.7.s2-49. [DOI] [PubMed] [Google Scholar]
- 120.Larvin M. Management of infected pancreatic necrosis. Current Gastroenterology Reports. 2008;10(2):107–114. doi: 10.1007/s11894-008-0030-y. [DOI] [PubMed] [Google Scholar]
- 121.Heinrich S, Schäfer M, Rousson V, Clavien P-A. Evidence-based treatment of acute pancreatitis: a look at established paradigms. Annals of Surgery. 2006;243(2):154–168. doi: 10.1097/01.sla.0000197334.58374.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Mole DJ, McClymont KL, Lau S, et al. Discrepancy between the extent of pancreatic necrosis and multiple organ failure score in severe acute pancreatitis. World Journal of Surgery. 2009;33(11):2427–2432. doi: 10.1007/s00268-009-0161-9. [DOI] [PubMed] [Google Scholar]
- 123.Banks PA, Freeman ML, Fass R, et al. Practice guidelines in acute pancreatitis. American Journal of Gastroenterology. 2006;101(10):2379–2400. doi: 10.1111/j.1572-0241.2006.00856.x. [DOI] [PubMed] [Google Scholar]
- 124.Sigounas DE, Tatsioni A, Christodoulou DK, Tsianos EV, Ioannidis JPA. New prognostic markers for outcome of acute pancreatitis: overview of reporting in 184 studies. Pancreas. 2011;40(4):522–532. doi: 10.1097/MPA.0b013e31820bf8ac. [DOI] [PubMed] [Google Scholar]
- 125.Petrov MS, Pylypchuk RD, Uchugina AF. A systematic review on the timing of artificial nutrition in acute pancreatitis. British Journal of Nutrition. 2009;101(6):787–793. doi: 10.1017/S0007114508123443. [DOI] [PubMed] [Google Scholar]
- 126.Bruennler T, Hamer OW, Lang S, et al. Outcome in a large unselected series of patients with acute pancreatitis. Hepato-Gastroenterology. 2009;56(91-92):871–876. [PubMed] [Google Scholar]
- 127.Brun A, Agarwal N, Pitchumoni CS. Fluid collections in and around the pancreas in acute pancreatitis. Journal of Clinical Gastroenterology. 2011;45(7):614–625. doi: 10.1097/MCG.0b013e318213ef3e. [DOI] [PubMed] [Google Scholar]
- 128.Sakorafas GH, Tsiotos GG, Sarr MG. Extrapancreatic necrotizing pancreatitis with viable pancreas: a previously under-appreciated entity. Journal of the American College of Surgeons. 1999;188(6):643–648. doi: 10.1016/s1072-7515(99)00045-9. [DOI] [PubMed] [Google Scholar]
- 129.McIlroy K, Grayson L, Phillips AR, Windsor JA. Early nasogastric tube feeding versus nil per os in mild to moderate acute pancreatitis: a randomized controlled trial. Clinical Nutrition. 2013;32:697–703. doi: 10.1016/j.clnu.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 130.Hegde A, Bhatia M. Neurogenic inflammation in acute pancreatitis. Journal of the Pancreas. 2005;6(5):417–421. [PubMed] [Google Scholar]
- 131.Winterbourn CC, Buss IH, Chan TP, Plank LD, Clark MA, Windsor JA. Protein carbonyl measurements show evidence of early oxidative stress in critically ill patients. Critical Care Medicine. 2000;28(1):143–149. doi: 10.1097/00003246-200001000-00024. [DOI] [PubMed] [Google Scholar]
- 132.Mole DJ, Olabi B, Robinson V, Garden OJ, Parks RW. Incidence of individual organ dysfunction in fatal acute pancreatitis: analysis of 1024 death records. HPB. 2009;11(2):166–170. doi: 10.1111/j.1477-2574.2009.00038.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Johnson CD. Antioxidants in acute pancreatitis. Gut. 2007;56(10):1344–1345. doi: 10.1136/gut.2007.122101. [DOI] [PMC free article] [PubMed] [Google Scholar]