Abstract
Context:
The biggest challenge in implementing the primary health care principles is of equitable distribution of health care to all. The rural masses and urban slum dwellers are most vulnerable to lack of access to health care.
Aim:
To study access to health services among slum dwellers and rural population.
Setting and Design:
A cross-sectional survey in an urban slum and surrounding rural areas in field practice area of a medical college.
Materials and Methods:
Structured instrument along with qualitative techniques such as focus group discussions, were used to collect information on access and utilization of health services from 865 individuals of both sexes and all ages selected from urban slums, villages, and indoor and outdoor patients. Access to basic determinants of good health such as housing, water, and sanitation was also elicited. Besides, health needs based on self-reported disease conditions were compiled.
Results:
More than 50% of respondents were living in poor housing and insanitary conditions. Besides the burden of communicable diseases and malnutrition (especially in children), risk of lifestyle diseases as evidenced by high Body mass index in 25% of adults surveyed was found. Private medical practitioners were more accessible than government facilities. More than 60% sought treatment from private medical facilities for their own ailments (for sickness in children this proportion was 74%). People who visited government facilities were more dissatisfied with the services (30.88%) than those who visited private facilities (18.31%). This difference was significant (OR=1.99, 95% confidence interval 1.40 to 2.88; χ2 =15.95, df=1, P=0.007). The main barriers to health care identified were waiting time long, affordability, poor quality of care, distance, and attitude of health workers.
Conclusion:
The underprivileged in India continue to have poor access to basic determinants of good health as well as to curative services from government sources during illness.
Keywords: Access, epidemiological, health, rapid, utilization
Introduction
India is attracting medical tourists from the developed world for affordable and accessible state of art medical treatment. Medical tourism is a growing sector in India. India's medical tourism sector is expected to experience an annual growth rate of 30%, making it a Rs. 9,500-crore industry by 2015.[1] Estimates of the value of medical tourism to India go as high as $2 billion a year by 2012. As medical treatment costs in the developed world balloon—with the United States leading the way—more and more Westerners are finding the prospect of international travel for medical care increasingly appealing. The Indian government is actively courting international patients.[1]
On the other hand, it is a grim irony that the poor in India do not have access to basic health care. Like most developing countries, in India, millions die from treatable conditions. Three diseases (all preventable and treatable)—diarrhea, pneumonia, and malaria—are responsible for 52% of child deaths worldwide.[2] Inadequate access in the area of reproductive health also exists. In South Asia less than half of pregnant women get an antenatal check up and only onefifth of births are supervised by someone with medical training.[2]
Because of gross underutilization of effective health care, there exist unrealized health gains in poor communities. Child deaths could be reduced by 63% if coverage rates of effective prevention and treatment interventions were to increase from current levels to 99%.[3] Raising coverage rates of maternal health intervention (the most important of which is essential obstetrics care) to the same level would reduce maternal deaths by three-fourths.[2] In India, the maternal mortality rate is over 200 per lakh childbirths, compared to less than 10 per lakh in developed countries.
Many factors are responsible for these missed opportunities. On the demand side, cultural and educational factors may obscure the recognition of illness and the potential benefits from health care, while economic constraints may suppress utilization, even if benefits are recognized. It is estimated that deficient care seeking behavior is a factor in 6–70% of child deaths.[4] In Bolivia, 60% of children who died during a study period were not taken for medical treatment during the fatal sickness episode.[5]
On the supply side, appropriate health services may not be available at all, particularly in rural areas and urban slums of our country. Lack of availability is the root of the problem in many instances[6] even though many effective interventions are not prohibitively expensive.[7] For example, over one half of preventable child deaths in sub-Saharan Africa could be realized through home-delivered interventions.[2]
Quality of health service is another determinant. The evidence is mixed on whether primary care clinics have any impact on population health.[8] This dismal conclusion is attributed to the poor quality of public primary health care in many parts of the country. There is evidence that demand is driven by quality.[7] A detailed survey in rural India found very low use of public health facilities despite these being in principle free.[9] The reason was the very poor quality of health care on offer.
Another concern is that utilization is lowest among the poor who need it the most. Evidence shows that there is pro-rich bias in the distribution of health benefits.[10] The strongest evidence of inequitable distribution across socioeconomic strata, for even simple cheap health interventions, is from the Demographic Health Surveys.[11,12] Households were ranked by the index of assets possessed e.g. refrigerator, sanitary toilet, safe drinking water, etc. Averaging across forty countries in which surveys were conducted it was found that among the poorest 20% of households 56% cases of childhood diarrhea were treated with oral rehydration compared with 71% of cases in the richest fifth of the households.[11] Inequalities in immunization coverage were even greater. The full immunization coverage was 66% in the richest quintile of the households, compared to 38.5% in the poorest quintile.[13] Evidence from India suggests that income related inequalities in access to health care increased between 1986 and 87 and 1995 and 1996.[14]
Our country is caught up in an epidemiological mosaic i.e. a mix of disease patterns of both the developing and developed nations. On one hand we are still struggling with diseases of poverty both communicable (malaria, TB, HIV/AIDS) and non-communicable diseases such as protein energy malnutrition in children, anemia, and malnutrition among pregnant women, and so on. Simultaneously, we are fast catching up with diseases of developed nations brought about by a rapidly growing economy. Diabetes, coronary heart disease, and hypertension are to some extent driven by sedentary lifestyles, faulty dietary patterns and obesity.
To meet these rapidly emerging challenges, penetration of health services and their utilization by the population are essential. We have a very poor track record of equity in health care. The rural areas and urban slums have very poor access to health services. For rational policy making, inputs from studies among the underprivileged populations on access and utilization of health services are essential. As the economy gallops, the rapid transition from hunger to heart attacks among the presently poor can only be prevented if timely action is taken to ensure that these people do not adopt the lifestyles and diet patterns which facilitate emergence of diseases such as coronary heart disease and diabetes. This is the strategy of primordial prevention, the most pure form of primary prevention. With this background, the present study was carried out using the following strategy.
Access to health care has four dimensions: Availability, accessibility, affordability, and acceptability.[15] Health care delivery should be evaluated against these objectives. This has been referred to as effective coverage.[16]
The present study endeavored to study access to health services among the underprivileged represented by samples from urban slum and rural areas, using the above criteria.
Materials and Methods
Study site and population
The study was carried out in the field practice areas of a private medical college. Situated about 30 km from Pune, the rural field practice area includes seven villages around Alandi totaling a population of 40,000. The urban field practice area is situated at Bhosari, near Landevadi slum (Population 10, 000) about 5 km from the college.
Besides these two field practice areas, the outreach activities of the college extend to nearby villages in a radius of 100 km (total population 1 lakh) by way of health camps.
Study design
A cross sectional survey using rapid appraisal techniques.[17] Both quantitative and qualitative methods were used to collect information.
Period of data collection
1st October to 31st Dec 2010.
Study samples
A total of 865 persons of both genders were surveyed. Categories of respondents surveyed and methods of sampling were as follows: 437 (50.52%) of the study subjects were selected by house to house survey both in urban and rural field practice areas of the college; 198 (22.89%) were selected from the outpatients attending the teaching hospital; 194 (22.43%) were indoor patients; and 36 (4.16%) were persons accompanying patients.
Study instrument
A structured pre-tested questionnaire included information about physical activity, work, tobacco use, education, anthropometry, housing, water supply, and sanitation. Self-reported conditions in the past 6 months, treatment seeking behavior, and barriers to access health services were also recorded.
Ethical issues
The study proposal was cleared by the Institutional Ethics Committee. Besides, informed consent in the respondent's own language was taken before eliciting information from each respondent.
Creating the questionnaire, data entry and statistical analysis
Statistical and Epidemiological Software Epi Info 2002 (developed by WHO and Centre for Disease Control, Atlanta) was used for data management. Questionnaire was created on the software for computerized data entry using the feature “Make View.” Data entry checks were put to prevent wrong entry of data. Statistical analysis was carried out using “Data Analysis” feature of the software. Data was summarized by percentages, mean and standard deviation as applicable. Inferential statistics involved parametric tests such as Analysis of Variance (ANOVA) for interval data, chi-square and odds ratio with 95% confidence intervals were used for categorical data, and non-parametric tests were used for ordinal data.
Results
Age, gender and residence
Of the 865 respondents, 360 (41.6%) were males and 505 (58.4%) were females. The mean age was 27.33 years (SD 15.99 years). The study also included 183 under five children of both genders. Out of the total study subjects, 424 (49.02%) were from rural areas, and the rest 441 (50.98%) were from urban areas.
Major occupations
Among men majority were manual laborers (21.5%), followed by sedentary desk jobs (18.5%), 17.1% worked on the farms, 15.7% worked in shops or small businesses. The rest were employed in various odd jobs. Among women the vast majority were housewives (51%), followed by farm work (10.9%), desk job (9%), housemaids (6%), manual workers (6.6%), and small businesses (2.1%).
Literacy
Out of the total sample interviewed, 83.4% had received formal education, 2.4% could read only, and 14.2% had not received any formal education. However, the mean years of schooling were 8.82 years (SD 4.1 years) for men and 7.4 years (SD 4.8 years) for women, indicating a high rate of school dropouts.
Income
The mean per capita income was Rs 1773 (SD Rs 1447) per month. Twenty five percent of the respondents has less then Rs 945 per month per capita income; 50% of the individuals studied had per capita income Rs 1250 and 75% had per capita income less than Rs 2142 per month.
Housing and related amenities
About half the study population (50.4%) was staying in improvised housing, the rest 49.6% wasstaying in cement concrete houses. Piped water to house was available in 55.8% of the households surveyed in urban areas, while 47.6% rural houses had piped water to house. Eighteen percent of the urban population and 20.5% of the rural population did not have sanitary toilets. Almost 80% of the rural houses and 82.4% of the urban slum inhabitants and 96.6% of urban non slum houses had access to mobiles. Access to mobiles was higher than access to toilets!! Overall, 35% of the population was exposed to indoor air pollution due to the type of cooking fuel used in their house such as kerosene, coal, wood, and dung cakes. This proportion was higher in rural population (44.5%). To aggravate the situation, most households (56.5%) lacked separate kitchen for cooking food. Only 20.8% of the surveyed population used mosquito nets. Poor drainage leading to mosquito breeding added to the problem.
Nature of work and physical activity
On an average people worked 40.3 h per week (SD 19.53 h). Only 25.8% of those having sedentary occupations indulged in physical activity (so as to work up some sweat), for at least 30 min three or more times a week.
Body mass index
In the study population the distribution of body mass index (BMI) among adults brought out both extremes—at one end of the spectrum 21% of the study subjects had BMI below 18.5 kg/ m2 indicating malnutrition, while 15% had BMI over 25 indicating overweight as per global standards, and 28% had BMI over 23 kg/ m2 suggesting overweight/obesity according to recent cut off for Asians.
Smoking and tobacco use
While smoking was more prevalent in adult males with 10% adult males admitting to smoking while only 0.7% women were smokers, tobacco chewing was fairly common both in men (35.5%) and women (21.5%).
Cooking oil, fresh fruits and vegetables
About 15% people were using saturated fats such as vanaspathi or ghee as cooking media. Only 3% consumed adequate amounts of fresh fruits or vegetables i.e. at least five helpings per day (one helping = 75 g).
Common illnesses
Communicable diseases
These (elicited by self reported sickness), mostly comprised of acute febrile illnesses (23.4%), main causes for which were malaria, typhoid fever, viral diseases such as jaundice, dengue, chikungunya (one outbreak of which was confirmed during the study period by serological studies). Diarrheal diseases were 8.1% in the study population followed by respiratory infections (3%) and skin diseases (2%). Tuberculosis was reported by 1% of the population.
Nutritional disorders
While about 21% of the adults were undernourished reflected by BMI <18.5 kg/m2, on the other hand, 15% of the adults showed tendency to overweight with BMI >25 kg/m2; however, as per recent cut off for Asians,[18] 28% would be classified as overweight with BMI >23 kg/m2. Among under five children, under nutrition was a problem with almost half of them (48%) showing signs of various grades of protein energy malnutrition (PEM).
Diseases in children under 5 years of age
About 28% of the under fives had suffered from episodes of diarrhea in the past 6 months. Less than 50% (49.8%) of the mothers gave oral rehydration solution (ORS) to the child during diarrhea. However, 37% gave homemade rehydration fluids to the child during diarrhea. Of concern is that 14% of the mothers were not aware of the importance of ORS or other home based rehydration fluids during diarrheal episode; 46.4% of the mothers stopped breast feeding and other feeds during spells of diarrhea. More than 15% under fives had episodes of respiratory infections in the past 6 months, and about 67% children below 5 years had episodes of fever in the recent 6 months.
Health seeking behavior during child's illness
Only 26% sought treatment from government sources during the child's illness. The majority (74%) sought treatment from various types of private sources.
Non communicable diseases
The major burden of non communicable diseases was due to various types of musculoskeletal disorders (7%), diabetes (2.7%), high blood pressure (1%), and heart diseases (0.7%).
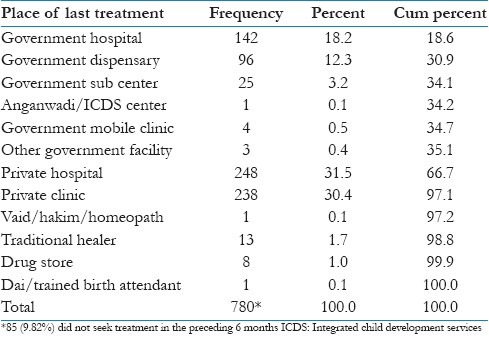
Treatment seeking behavior
The majority of people who had sought treatment in the past 6 months, preferred non government sources as shown in Table 1. Private clinic and private hospital were the most preferred source for medical treatment, (more than 60%) of those who had sought treatment in the preceding 6 months. Contrary to expectations, very few had sought treatment from practitioners of alternative systems of medicine such as homeopath or other traditional healers.
Table 1.
Treatment seeking behavior
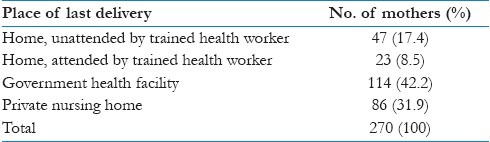
Utilization of maternal health services among women who had borne children
Place of delivery of the last child
There were 270 women who had borne children in the past 5 years. The place of last delivery is shown in Table 2. It is a matter of concern that about 17.4% of the deliveries were at home without supervision from a trained birth attendant. On qualitative interviews, a majority of these were among migrant workers who send their wives to their home villages for childbirth. Facilities for institutional deliveries in these villages are not accessible and acceptable due to distance and unsatisfactory standard of care. Even among mothers who opted for institutional deliveries, only 42.2% had availed of government health facilities.
Table 2.
Place of delivery of last child among women who had borne children
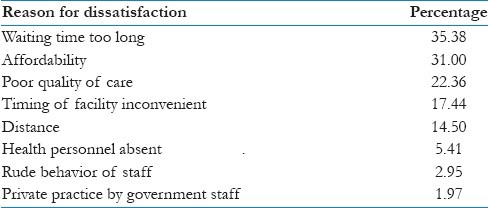
Satisfaction during last health visit and barriers to access to health care
This is shown in Table 3. More people were dissatisfied with government health facilities compared to private facility. While 18.31% expressed dissatisfaction with private treatment facility, 30.88% revealed unhappiness with government health facilities, this difference being statistically significant (OR=1.99, 95% CI 1.40 to 2.85, χ2 =15.95, df=1, P=0.0007). Further details on reasons for dissatisfaction have been shown in Table 4. The most common barriers were too long a waiting time and affordability of medical treatment. On qualitative probing of affordability factor (since treatment at government facilities is supposed to be free), most people complained of short supply of drugs at government hospitals and dispensaries because of which cost had to be borne by the patients from their pocket. Also because of distance from residence to government facility affordability of cost of transport was also a factor in some cases. Other view offered, mostly those working as casual workers, was the loss of wages at work due to time spent in government hospitals waiting for their turn to be attended.
Table 3.
Satisfaction during health visit
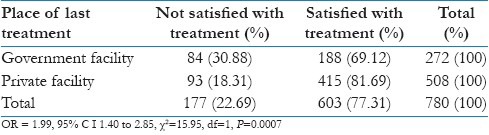
Table 4.
Barriers to access to health care as perceived by the people
Physical accessibility to health facility
Private medical practitioners had more penetration. While 25% of the people reported that the nearest government health facility was more than 5 km from their house, only 3% reported that the nearest private practitioner was more than 5 km from their house. This difference was statistically significant (odds ratio=10.7, 95% CI=6.9 to 16.73; χ2 =171, df=1, P<0.0001)
Inputs from qualitative interviews and focus group discussion
Perception of people regarding role of government for improving health accessibility
Most felt that the government needs to do much more than at present on health issues. The recurring themes were as follows:
The government should establish and maintain adequate health facilities.
Cost control of drugs.
Focus on public health measures such as water, sanitation and immunization.
Most community leaders and women groups approached felt that basic amenities such as adequate drinking water, toilet, and sanitation facilities require more attention from the concerned authorities. Awareness of lack of safe water and proper sanitation as a cause of disease burden was found to be good among the surveyed population.
Discussion
Health care reforms have to be placed within a national effort to provide food, water, shelter, sanitation, education, and other basic needs.[19]
The study found a large number of respondents living in overcrowded and insanitary conditions. We have to address the socioeconomic determinants of health.[20]
A study on socioeconomic factors and longevity found higher income households had longer life expectancy as compared to deprived persons.[21] As in our study, most respondents belonged to lower socio-economic status economic development and job opportunities coupled with availability of basic amenities such as good housing, safe water, and sanitation would have a positive impact on health status.
These factors are always changing and it is important to re-assess these needs from time to time.[22] For example, India is in a state of rapid social transition due to globalization and a galloping economy both posing fresh health challenges due to changing lifestyles and sedentary habits.
The study indicates preference for the private sector while seeking health care. Increasing government infrastructure has not solved this preference in the past. Patient satisfaction is subjective which can show lack of agreement between patients and health care providers.[23] Some qualitative inputs have therefore been included in the present study.
According to the National Family Health Survey–3 report, cited by Ray,[24] almost half of the children below 5 years of age (48%) are stunted and 43% are underweight. To tackle the problem of child malnutrition, in the early 1990s, the united nations children's fund (UNICEF) and the State and Central governments were committed to promote baby friendly hospital initiative (BFHI) in the hospitals, continued feeding during illness, exclusive breast feeding, and timely complementary feeding, care of pregnant woman, and so on. According to our findings, these simple measures have not penetrated down to the slum and rural areas of our field practice area, as appreciable number of mothers stopped feeding the child during episodes of illness such as diarrhea. There were some gaps in care of pregnant women also.
The nutritional status of the adult population in the present study is paradoxical. We seem to have a double burden of both undernourishment as indicated by 21% of the study sample having BMI below 18.5 kg/m2 and overweight/obesity as shown by 28% having BMI over 23 kg/m2. This paradox may be due to the fact that among the poor who rapidly acquire some affluence there is a tendency to sedentary lifestyle and faulty eating habits leading to obesity, while those who continue in impoverishment remain undernourished.
In childhood, poor living conditions and the parents’ social class have a strong impact on cardiovascular health status.[25] In middle age, life style factors such as tobacco use, physical inactivity, and unhealthy diet increase risk of cardiovascular disease. The present study showed only about 25% of those with sedentary jobs indulging in adequate physical activity. There is increasing evidence of higher risk of disadvantaged populations because of poor availability of health foods such as fruits and vegetables (only 3% in the present study consumed adequate portions of fresh fruits/vegetables), quality of food, and constrains to adopting health lifestyles, such as lack of access to physical activity.[25] These inequities can be addressed only if there is increase in public spending coupled with efficient use of resources and investment in strong prevention measures. Such measures will particularly benefit the poor who suffer most from the consequences of high cost of diagnostic tests and drugs coupled with inadequate accessibility to health care.
Technological innovations such as widespread penetration of mobile telephony can be used for health education. Treatment follow up in diseases like tuberculosis can also be facilitated by mobile telephony.
Conclusion
The present study was carried out using rapid epidemiological methods.[17] These methods may provide less detailed or accurate information than would be provided by more rigorous methods. To a large extent, we used “quick and dirty” techniques. However, in spite of the inherent inaccuracies and deficiencies we hope the results may be useful to emphasize the major health needs and difficulties in access to health care faced by the population living in the “dark underbelly” of a “Shining India.” It is better to have an approximate estimate of important health problems, rather than have a perfect estimate of insignificant health issues. Although the sample studied may not be representative of all rural and slum areas in the country, it is important to note that this dismal situation prevails in the field practice area of a medical college in a big city of a comparative prosperous state. The situation elsewhere is likely to be worse than better.
Footnotes
Source of Support: India Health Progress New Delhi (www.indiahealthprogress.in)
Conflict of Interest: None declared.
References
- 1.Shetty P. Medical tourism booms in India, but at what cost? Lancet. 2010;376:671–2. doi: 10.1016/s0140-6736(10)61320-7. [DOI] [PubMed] [Google Scholar]
- 2.Washington, D C: World Bank; 2004. World Bank. The millennium development goals for health: Rising to the challenges. [Google Scholar]
- 3.Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS Bellagio Child Survival Study Group. How many child deaths can we prevent this year? Lancet. 2003;362:66–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- 4.Hill Z, Kirkwood B, Edmond K. London: Public Health Intervention Research Unit, Department of Epidemiology and Population Health, London School of Hygiene; 2003. Family and community practices that promote child survival, growth and development. [Google Scholar]
- 5.Agullar AM, Alvarado R, Cordero D, Kelly P, Zamora A, Salgado R. Technical Report. Arlington: Basic Support for Institutionalizing Child Survival; 1998. Mortality survey in Bolivia: The final report. Investigating and identifying the causes of death for children under five. [Google Scholar]
- 6.Geneva: World Health Organization; 2001. Commission on Macroeconomics and Health. Macroeconomics and Health: Investing in health for economic development. [Google Scholar]
- 7.O’Donnell O. Access to health care in developing countries: Breaking down demand size barriers. Cad. Saude Publica Rio de Janeiro dez. 2007;23:2828–34. doi: 10.1590/s0102-311x2007001200003. [DOI] [PubMed] [Google Scholar]
- 8.Filmer D, Hammer J, Pritchett L. Weak links in the chain: A diagnosis of health policy in poor countries. World Bank Res Obs. 2000;15:199–224. [Google Scholar]
- 9.Banerjee A, Deaton A, Duflo E. Health Care Delivery in rural Rajasthan. Econ Polit Wkly. 2004;39:944–9. [Google Scholar]
- 10.Gwatkin DR. Washington, D C: World Bank; 2001. Overcoming the inverse care law: Designing health care programs to serve disadvantaged population groups in developing countries. [Google Scholar]
- 11.Gwatkin DR, Rustein S, Johnson K, Pande RP, Wagstaff A. Washington, DC: World Bank, Health, Population and Nutrition Group; 2000. Socioeconomic differences in health, nutrition and population. [Google Scholar]
- 12.Gwatkin DR, Rustein S, Johnson K, Pande RP, Wagstaff A. Washington, DC: World Bank; Health, Population and Nutrition Group; 2003. Initial country level information about socioeconomic differentials in health, nutrition and population. [Google Scholar]
- 13.Gwatkin DR, Devishwar, Bahl G. Washington, D C: World Bank; 2001. Immunization coverage inequalities: An overview of socioeconomic and gender differentials in developing countries. [Google Scholar]
- 14.Sen G, Aditi I, Asha G. Structural reforms and health equity: A comparison of the NSS Surveys, 1986 – 87 and 1995 – 96. Econ Polit Wkly. 2002;37:1342–52. [Google Scholar]
- 15.Penchansky B, Thomas JW. The concept of access: Definition and relationship to consumer satisfaction. Med Care. 1981;19:127–40. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Shengelia B, Murray CJ, Adams O. Beyond access and utilization: Defining and measuring health system coverage. In: Murray CH, Evans DB, editors. Health Systems Performance Assessment: Debates, methods and empiricism. Geneva: WHO; 2003. pp. 221–34. [Google Scholar]
- 17.Abramson JH, Abramson ZH. Research methods in Community Medicine. 6th ed. West Sussex PO19 8SQ, England: John Wiley and Sons Ltd; 2008. Rapid epidemiological methods; pp. 313–24. [Google Scholar]
- 18.WHO expert consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 19.Narayan R. Universal Health Care in India: Missing core determinants. Lancet. 2011;377:883–5. doi: 10.1016/S0140-6736(10)62045-4. [DOI] [PubMed] [Google Scholar]
- 20.Blas E, Kurup AS. Introduction. In: Blas E, Kurup AS, editors. Equity, social determinants and public health programmes. Geneva: WHO; 2010. pp. 3–11. [Google Scholar]
- 21.Sauvaget C, Ramadas K, Fayett J, Thomas G, Thara S, Sankaranarayanan R. Socioeconomic factors and longevity in a cohort of Kerala State, India. Indian J Med Res. 2011;133:479–86. [PMC free article] [PubMed] [Google Scholar]
- 22.Wright J, Kyle D. Assessing Health Needs. In: Guest C, Melzer D, Muir Gray JA, editors. Oxford Handbook of Public Health Practice. 2nd ed. Oxford: Oxford University Press; 2006. pp. 20–31. [Google Scholar]
- 23.Zodpey S. Can primary health care reinvent itself to impact health care utilization? Indian J Public Health. 2010;54:55–6. doi: 10.4103/0019-557X.73270. [DOI] [PubMed] [Google Scholar]
- 24.Ray SK. Evidence based preventive interventions for targeting under-nutrition in the Indian context. Indian J Public Health. 2011;55:1–6. doi: 10.4103/0019-557X.82531. [DOI] [PubMed] [Google Scholar]
- 25.Mardis S, Banerjee A. Cardiovascular disease: Equity and social determinants. In: Blas E, Kurup AS, editors. Equity, social determinants and public health. Geneva: World Health Organization; 2010. pp. 31–48. [Google Scholar]


