Abstract
Policy on medical education has a major bearing on the outcome of health care delivery system. Countries plan and execute development of human resource in health, based on the realistic assessments of health system needs. A closer observation of medical education and its impact on the delivery system in India reveals disturbing trends. Primary care forms backbone of any system for health care delivery. One of the major challenges in India has been chronic deficiency of trained human resource eager to work in primary care setting. Attracting talent and employing skilled workforce seems a distant dream. Talking specifically of the medical education, there are large regional variations, urban - rural divide and issues with financing of the infrastructure. The existing design of medical education is not compatible with the health care delivery system of India. Impact is visible at both qualitative as well as quantitative levels. Medical education and the delivery system are working independent of each other, leading outcomes which are inequitable and unjust. Decades of negligence of medical education regulatory mechanism has allowed cropping of multiple monopolies governed by complex set of conflict of interest. Primary care physicians, supposed to be the community based team leaders stand disfranchised academically and professionally. To undo the distorted trajectory, a paradigm shift is required. In this paper, we propose expansion of ownership in medical education with academic institutionalization of community health services.
Keywords: Community based medical education, medical education reforms, family medicine
“Any thoughtful observer of medical schools will be troubled by the regularity with which the educational system of these schools is isolated from the health service systems of the countries concerned. In many countries these schools and faculties are, indeed, the proverbial ivory towers. They prepare their students for certain high, obscure, ill-defined and allegedly international “academic standards” and for dimly perceived requirements of the twenty-first century, largely forgetting or even ignoring the pressing health needs of today's and tomorrow's society.”[1]
Dr. Mahler, Former Director General of WHO
Emerging India and Challenges in Health Sector
India is one of the fastest growing economies in the world. Indian economy is the ninth largest in the world considering nominal gross domestic product (GDP) and third largest considering purchase power parity (World Bank). India is also the second largest populous country in the world with a population of 1.21 billion (Census 2011). It is projected to become world's most populated country surpassing China by 2025.
Beginning in the 1990s, economic reforms have rapidly transformed financial landscape in India. While India's GDP gives an impression of its middle-income nation status, she is also faced with challenges of addressing poverty and inequity. Rapid economic advancement has also resulted into disparities and regional inequalities. India fares poorly in the health sector parameters on comparison with international standards.[2] The impressive growth and the creation of wealth with economic liberalization have not resulted in expected social development.
While the urban fast growing private specialty hospitals display internationals standards and state of art the facilities, and are able to attract revenues from medical tourism, country's government run primary health centers still reel under poor infrastructure, a shortage of qualified doctors and nursing staff. A large chunk of population still has to travel more than 100 km to access basic healthcare.[3] A vast majority (86%) of all medical trips are made by rural Indians.[4] A high proportion (70-80%) of health care expenditure in India is borne “out-of-pocket” by citizens and most of this is spent on outpatient treatment, mainly medicines.[5] Illness is therefore a common reason for families to be forced into poverty.
High population density and scarce resources have been considered reason for poor health outcomes of communities. Lacks of basic amenities such as housing, sanitation, food and nutrition, safe drinking water etc have been identified as underlying cause for ill health.
The healthcare expenditure in India is mainly incurred on curative services and is increasing by 12% per year and is expected to touch $125 billion by 2015. Experts explain that the reason for this high expenditure is lack of primary healthcare facilities and rapidly expanding tertiary and super specialty hospitals. The primary healthcare segment accounts for a majority (60%) of the healthcare delivery market, growing at 15% annually. The current market size is $30 billion, which is likely to reach $200-250 billion by 2025 (Technopak Advisors).[6]
India's Commitment for Health for All and Millennium Development Goals
The Indian government has continuously sought to address health care challenges through investment in social sector. As a signatory of Alma Ata Declaration, primary health care has remained the centre of policy thrust for various state and local governments. Since independence, the government of India has attempted to alleviate ill health through various national health programs. India is also a signatory of millennium declaration and is committed to achieve the Millennium Development Goals (MDGs). The MDGs set ambitious targets for reducing hunger, poverty, infant and maternal mortality for reversing the spread of AIDS, tuberculosis, and malaria and giving children basic education by 2015. These also included gender equality, environmental sustainability, and multisectoral and international partnerships.[7]
Panchayati Raj Act (1992) was enacted to give statutory status to Panchayati Raj institutions in order to facilitate local self governance and promote community participation in development. Local planning and governance based on Panchayati Raj institutions now provide the basic framework to several recently introduced developmental programs. NREGA (Mahatma Gandhi National Rural Employment Guarantee Scheme), Sarva Shiksha Abhiyan (Primary education), Rajiv Gandhi National Drinking Water Mission and the Total Sanitation Campaign have been introduced address crucial MDGs. The Reproductive and Child Health Program II, the Integrated Child Development Services, and the National Rural Health Mission have resulted in impressive investment in the health sector.
Several on-going reforms seek to further decentralize and democratize various institutions in order to ensure equitable distribution of resources. Food security act 2011 is likely to improve access to food and nutrition to the vast majority of population.
National Rural Health Mission 2005
The National Rural Health Mission (NRHM) is a major reform strategy of government of India seeking to provide accessible, affordable and quality health care services to rural population. In NRHM, clear norms and standards for each level of care in terms of services provided, human resources, skills deployed, infrastructure and support services and systems have been defined and these are known as the Indian Public Health Standards (IPHS). During the first 5 year phase, NRHM has been able to make positive impact on health system in terms of infrastructure development and deployment of human resource. However, in 2010, 10% vacancies for doctors at the Primary Health Centers (PHCs) and 63% of the specialist posts at the Community Health Centers (CHCs), and 25% of the nursing posts at PHCs and CHCs combined remained unfilled. The situation for support staff is similar as 27% of pharmacist and 50% of laboratory technician posts also vacant as compared to the requirement for existing infrastructure. There was a shortfall of 62.8% of surgeons, 55.2% of obstetricians and gynecologists, 72% of physicians and 69.5% of pediatricians at the CHCs.[8]
Provision of Primary Health Care in Urban India
Every individual irrespective of paying capacity, affluence, educational status, age, gender and living location has a primary health care need. Majority (60%) of the health workers reside in urban areas and more than 70% of them are employed in the private sector. Public hospitals are characterized by poor infrastructure and high patient load.[8] During the last decade, a majority of specialty hospitals have come up mainly in the metropolitan cities. Affluent patients and insured persons routinely visit specialist doctors at corporate hospitals for their primary health care needs. Where as a large section of population has no access to qualified practitioners for their primary health care needs in the urban settlements.
Trends in Medical Education
Current medical education system in contributing to “widening disparities in India in health status and access to basic health care”.
“The medical education does not prepare the graduate to function effectively in areas of need. Students who have paid high fees for private medical education prefer to pursue careers where they are able to regain their investment. As a result, there is the problem of wide-scale foreign migration of medical graduates. Without the benefit of strong motivation imparted in their formative years, doctors are not inclined to work in rural locations and in difficult circumstances characterized by lack of adequate remuneration, difficulties in school education for children, and academic and social isolation. Medical colleges are not linked to and responsible for the health system (at the district and sub-district level) and for the health of a community in a geographical area. Thus, responsibility for the health of the community is not manifestly linked with medical education.
(The National Conference on Health Professional Education 2011 Vellore—Concluding statement).[9]
Medical qualifications and medical colleges are governed by Medical Council of India Act 1956. Medical council of India (MCI) sets standards for infrastructure and faculty for a medical college to be recognized by Ministry of Health and Family Welfare, Government of India.
Following trends in medical education highlight the status of skewed human resource development in health sector in India.
Private ownership
India has the largest numbers of medical colleges in the world. Developing over the period of past few decades, a majority of the medical colleges are now in the private sector. During the period 1995-2006, of the 106 medical colleges established, 84 were private. Today, of the 313 medical colleges, 163 are in the private sector. The privatization of medical education was well rooted even before economic reforms were rolled out in India.[10,11]
Regional imbalance
There is only one medical college for a population of 11.5 million in Bihar and 9.5 million in Uttar Pradesh, compared to Kerala and Karnataka where we have one medical college for a population of 1.5 million. States with the greatest human resource needs also have the lowest capacity to produce them. The five south-western states of Andhra Pradesh, Maharashtra, Karnataka, Kerala, and Tamil Nadu (with 31% of the country's population) account for 58% of medical colleges in India, both public and private.[8,11]
Constitutional status of health
Health is state subject, while family welfare is a concurrent subject. Medical education regulation is entirely centralized within Medical council of India (MCI) through an act of parliament. No regional flexibility with respect to infrastructure and faculty eligibility is allowed. All rules set by medical council of India have to be followed by book.
Training setting
A typical medical college includes a teaching hospital which is a tertiary care hospital. MBBS students are taught clinical subjects in specialty wards and out patient departments (OPDs). Community-based facilities such as district hospitals, community health centers, and primary health centers are not linked with medical colleges and operate with an entirely distinct administrative set up. Reorientation of medical education (ROME) launched in 1977 did not take off well due to lack of academic processes within community health system.
Faculty eligibility
A faculty aspirant must hold a post graduate (PG) qualification. Work experience at tertiary care medical college hospitals is considered essential for faculty eligibility. Primary care physicians (general practitioner and general duty medical officers) are not eligible to become faculty at undergraduate (UG) or post graduate (PG) level as majority of them do not hold any post graduate qualification. They are therefore not the ideal role models for students.[12]
Post graduate training opportunities
There are very limited post graduate (PG) training opportunities. Only one in three can get a PG seat. The post graduate qualifications are awarded by local universities/autonomous institutions (MD/MS/Diploma) or a federal body called National Board of Examinations (DNB). University awarded qualifications are divided into Degree (MD/MS) or Diploma based on the years of study. The postgraduate positions are differentiated into clinical and preclinical branches. These differences in nomenclature and differential eligibility for faculty positions have a significant influence over the career choices of young graduates. Most of the medical graduates are un likely to get into a specialization of their choice and aptitude, failing to achieve a satisfying career path irrespective of their talents.[13] Current selection process is based on an multiple choice question (MCQ) based examination which selects by elimination. By few decimal points the candidates ranks may vary and so also the opportunity to net the seat in a desired speciality.
Vagabond period–young doctors in a fix
A large number of fresh medical graduates are not fruitfully engaged with the health care system due to limited PG training positions after MBBS.[14] Several doctors keep on attempting PG entrance tests several years after MBBS qualification. A growing number of students pursue coaching classes (memorizing high yielding texts to be able to solve multiple choice questions) during internship period to be able to clear PG entrance tests. Employment and learning clinical skills is not a priority till they are able to get a PG seat. Many who take up jobs as medical officers in state governments are not satisfied with the nature of their employment and this may be one reason for locally managed prolonged absenteeism. An ever increasing pool of unsuccessful PG aspirants set the market higher every year for private medical colleges to auction their PG seats like commodities in the wholesale market.
Migration of physicians
A large number of Indian doctors aspire to migrate abroad to countries such as USA, UK, Australia, Middle east due to lack of PG training opportunities and better career prospects. Many of them find opportunities in generalist streams such as family medicine. Tendency to migrate abroad is observed more among the physicians qualifying from best funded and top-ranked medical colleges. More than 50% of MBBS graduates qualifying from All India Institute of Medical Sciences (AIIMS) have migrated abroad since inception of AIIMS.[15]
Aspiration of Medical Students and Young Doctors
Young doctors and medical students do not hold any stake in medical education planning and regulation in India. There are very few studies available on their aspiration and career choices.
A recent study of interns in south India revealed that (1) majority consider PG qualification essential; (2) majority (95%) plan to pursue a clinical specialty; (3) four most common specialties chosen were medicine, surgery, obstetrics and gynecology and pediatrics; (4) very few prefer preclinical and paraclinical subjects for specialization; (5) only a few (10%) were eager to settle with a MBBS degree, if they could not get a PG residency seat even after 3 years of completing their MBBS degree; (6) income and future career prospects are a major determinant of choice of the post MBBS pathway; (7) role models from faculty and residents play an important role in career decisions.[14]
In an another study from Delhi among 282 medical students interviewed (1) Only a handful of students were considering a career in non-clinical subjects; (2) anatomy, biochemistry, physiology, forensic medicine, and pathology had absolutely no takers; (3) none chose community medicine–public health; (4) students who eventually join non-preferred subjects did so out of a lack of any other choice; (5) they may not have much passion for, or commitment to, the subject, resulting in mediocrity and frustration.[16]
In a yet another study from Uttar Pradesh (UP): (1) the vast majority (90%) of the MBBS students intended to pursue a post graduate course of study; (2) all medical students placed great emphasis on specialization despite the fact that the number of post graduate (PG) seats available in a given year is one third of number of graduating MBBS students; (3) better career opportunities, the perception that MBBS doctors have less status in society, and a belief that MBBS degree does not sufficiently qualify them to practice medicine drive them to pursue PG degree; (4) through several attempts at PG entrance examinations, study participants also expressed a high level of confidence that they will undertake PG studies despite the limited number of seats available; (5) all students expressed a very low preference for community medicine; (6) training in public health holds little attraction for medical students.[17]
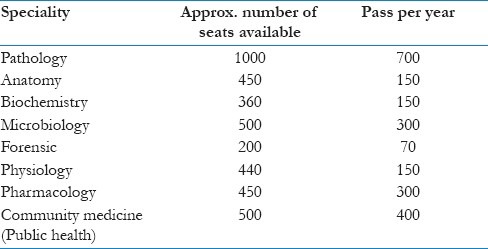
It can be safely assumed that majority of the students aspire to work as clinical specialists. This inference is reinforced by the gap in the total number of seats available in the preclinical departments in the entire country versus the number of pass outs per year as shown in Table 1.
Table 1.
Trends in career choice: PG training posts—Basic sciences and other specialties 2010[13]
Do our Young Doctors Want to Serve Rural and Underserved Communities?
More often young doctors are blamed for not showing eagerness to work in rural areas. They are often painted to be driven by greed, glamour, and comforts of life. This is more often a misrepresentation of the facts.
Most medical students in India join MBBS at a very young age (minimum age 17 years) straight out of their high schools. Totally disconnected from the general knowledge disciplines (humanities, general science, law, management, etc), they are largely unaware of the social, economical, and political context of their county and own education.
The cause of scarcity of skilled primary care physicians goes beyond unwillingness of young doctors. Its runs deep into the design of our medical education system, which is governed by narrow personal loyalties, multiple conflict of interest groups and regulatory mechanisms protecting monopolies.
In the author's own experience, 10 out of 45 students from his MBBS batch at a small community medical college in Jharkhand migrated to Delhi and Gujarat immediately after graduation due to lack of employment and PG training opportunity in their own state. All but one is working with the government system. All five who went to Gujarat joined primary health centers.
In many of the tertiary care institutions, where postgraduates are also trained the role played in patient care by the MBBS house man is limited to drawing blood for investigations, administering IV injections, clerical work like preparing discharge summary etc. Although this work is important, yet the limited period of one month to three months spent in a department spent mainly on non-clinical work(post graduate trainees are preferred for clinical work) deprives the house man of adequate opportunities to gain essential practical skills required to manage a primary care setting independently or under limited supervision.
Status of MBBS Doctor, Hierarchy of Vocations in Medical Profession, and Career Choice in Community Health Services
Primary care physicians–a default career
The licensing procedure in India allows doctors to practice medicine immediately after completion of undergraduate qualification, i.e. MBBS. However, in the present scenario, the career of primary care physicians, who work as private general practitioner or medical office at primary health centers is not a “career of choice.” It is rather a “default career” of a MBBS graduate who is not successful in securing a PG training position.
The design of medical education
Unidirectional path for career progression toward specialties and subspecialties has an extremely detrimental effect on the mind-set of medical students and thereby on the availability of trained human resource in the community set up (districts hospitals, community health center and primary health centre) especially in the underserved areas.
MBBS training has failed to evolve
Due to long pending, medical education reforms, over the period of time MBBS training has become less competency based and therefore is not able to cater to the community needs. Due to rapid advancement of medical science in the last few decades, plain MBBS level general practice is not able to address to the primary health care needs of urban, semi urban, rural and remote populations. As a result, there has been a gradual decline in the prestige of MBBS level general practice.
Recognition of basic doctor
A basic MBBS doctor working at primary health center is presumed to be least qualified and often least paid with no option of career progression in the same location. No value is given to experience gained and skills developed while working in resource poor environment. The only natural career progression available is by lateral movement to organ-based specialist qualification.
Qualifications, license to practice, privilege to practice and perform procedural skills
Specialist medical qualifications have become mandatory to practice essential and lifesaving clinical skills, limiting certain privileges to a small group of physicians which has caused the development of monopolies in service delivery and in turn deprive these services from a large section of the community who cannot afford access to health care facilities where these specialists usually work. Furthermore the scope of practice of skills at MBBS level is shrinking fast because of lack of exposure and training, added to the rising public awareness and consumer protection regulations.
Fragmentation and specialization in education leading to development hierarchy of vocations within medical profession
Specialization by acquiring post graduate qualification is associated with following advantages:
(1) hospital attachments, (2) higher income, (3) social status, (4) personal and professional satisfaction, (5) faculty position, (6) opportunities for continuous skill enhancement, (7) academic and professional leadership positions, (8) opportunities for academic grants and funding, (8) peer recognition, (9) urban lifestyle [Figure 1].
Figure 1.
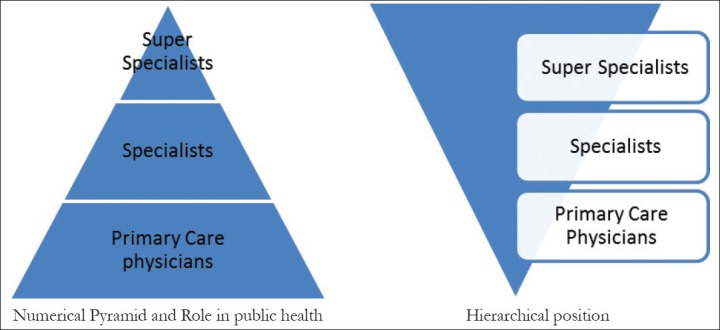
Hierarchy of vocations in medical profession (India)
Primary care physicians–disfranchised
Primary care physicians do not own any knowledge discipline or specialty. Although MBBS training is expected to produce basic community practitioner, family medicine or general practice is not taught as a specialty during MBBS course. A majority of the medical students and a large number of senior faculties are ignorant of the primary care practice as an independent knowledge discipline existing worldwide. Undergraduate students are trained by specialist doctors in tertiary care setting. More often these fresh doctors find themselves dysfunctional and disabled in community setting and complain of lack of tertiary care facilities. Once employed in state services, although designed to be governed by principles of public health, they are often entrusted with a huge non-clinical work load. As providers, they remain at lower bottom of the pyramid and stand disfranchised.
Solutions proposed so far: Reservation of 30% seats in PG training for in-service doctors
Of the several incentives (monetary and non monetary), giving preference and priority in PG selection to the in service doctors deserves special attention.
Several recent policy discussions recommend reservation of 10–30% seats in PG entrance tests for in-service doctors as a prescription to attract fresh medical graduates in community health services.[11] While this intervention may seem an administratively attractive proposition, it further aggravates crisis with in medical profession.
It fuels rat race for already scarce PG specialty seats and reinforces the direction of career part from basic doctor toward organ-based specialist streams. Only fewer will still get PG seats, while a majority will contribute to dissatisfied workforce. It is true that fittest would survive; however, it is designed to waste a large talent pool of youth. Making the profession extremely difficult to pursue will also render the profession unattractive for younger generation.
It is also a formal policy acceptance for a short career path design for primary care physicians, bypassing the key anomalies in mainstream medical education system. A short-term perceived gain leads to strategic short sightedness.
Seeking to maintain a hierarchical pyramid with large number of MBBS doctors at base cannot be a long-term solution. Vocation of primary care physicians must be developed to its fullest capacity with opportunity for academic and professional development at par with tertiary care doctors.
Need of Multi-skilled Competent Primary Care Physicians
Specialist qualifications, specialist skills and community needs
There is no need for every doctor to hold a “specialist qualification.” The need of the hour in medical education is to liberate “specialist skills” from water tight compartment of “specialist qualifications” and place them in the service of community. It is neither necessary nor possible to appoint specialist doctors at every primary health center.
Multi skilled physicians
It is more important to appoint “multi-skilled doctors” to deliver services and skills at district hospitals, community health centers, and primary health centers in accordance with the services guaranteed in the Indian Public Health Standards (IPHS). This felt need for a “set of skills & competencies” shall form the core curriculum for “community based doctors” which is the concept of family medicine. A Family Physician trained under supervision shall be a multi competent specialist in common illnesses rendering broad based essential services cutting across the domain of organ based specialists. “Family medicine—a specialty of skilled primary care physicians,” has been incorporated as a core strategy in several countries from most developed ones to the least developed ones as need-based medical education.[18]
Need based medical education
We need to educate doctors and license them to practice skills that match the community needs. However, at present, we have a reverse case scenario, where specialists learn and offer “certain skills”/“Services” which may not be in tandem with the community needs.
Family Medicine: Transferring Ownership to Primary Care Physicians
International developments
Family Medicine is a well evolved knowledge discipline and specialty for primary care physicians in countries such as USA, Canada, UK, Australia and New Zealand. Professional competency is acquired and certified through structured post graduate residency programs. Family Medicine came into existence as 20th specialty of medicine in USA in 1969.[19] Family medicine evolved as a counterculture in 1960s in response to rapid fragmentation of medical profession into various specialities post second world war period. Family medicine reflected community's need and desire for comprehensive health care. During last few decades family medicine departments have been established in several South Asian countries. There are well established programs such as “MD GP and Emergency” program at Tribhuwan University Teaching Hospital (TUTH) kathmandu and BPKIHS Dharan, “MD family medicine” at Post Graduate Institute of Medicine (PGIM) University of Colombo and four year residency program in family medicine at Aga Khan University Karachi etc.
Evolution of academic family medicine in India and current status: National Health Policy 2002
Family Medicine has been recognized specialty since 1983 by amendment in first schedule of Medical Council of India (MCI) act. DNB Family Medicine, regulated by National Board of Examination (www.natboard.nic.in) is a recognized post graduate qualification since 1983 and has evolved as a structured three year residency based training program. The National Health Policy 2002 emphasized on family medicine as one of the focus areas of human resource development. Family medicine received much need thrust again in 2005 through National Board of Examination affiliated DNB courses in order to full fill the human resource requirement of National Rural Health Mission. In 2008, there were approximately 700 DNB post graduate training posts available annually at 200 National Board of Examination (NBE) accredited health institutions in India. There is no MD family medicine yet any medical college regulated by Medical Council of India (MCI).
Why India lagged behind?
Lack of experience of the existing centers of medical education with community based learning opportunities has led to the biased growth of medical education in the favor of tertiary health care centered medical facilities. The rural and underserved populations are mostly dependent on publicly funded programs. The national health programs have largely operated in administrative framework rather than gaining strength from locally governed academic processes.
Why now?
Any government cannot ignore plight of huge underserved population and shy away from responsibility of welfare of its citizens. With huge financial and political commitment at stake, it is important that merit of such policy discussion should be tested through intense institutional policy discourse. MCI has been the case of institutional failure in past. MCI was dissolved by a presidential ordinance in 2010.[20] The “National Council for Human Resources in Health Bill 2011” presented in the parliament may set the momentum of change.
How it fits into the ongoing processes? MD family medicine curriculum has been notified recently
The concept of Family Medicine offers a unique solution for the on-going medical education reforms in India. Within the existing infrastructure and shortage of faculty for sub-specialties, thousands of PG family medicine seats can be created by initiating MD—Family Medicine. Three to four year training period for these family medicine PG seats may be spread over posting at medical college hospital, district hospitals and primary health centers, urban community health centers and GP practice sites.
Addressing community needs
Family Medicine approach will efficiently address the acute shortage of physicians in rural and underserved populations. Also, the availability of opportunities will effectively counter domestic and international migration of qualified doctors. Rural posting has always been offered as a negative incentive for young doctors. It has never been packaged as a path for career enhancement and academic accomplishment. There is an urgent need to build up an environment wherein a person opting for rural practice has an opportunity to become a “professor of rural medicine.”
Which model of family medicine education suits India ?
We need family doctors who are skilled to take care of high volume of patients, who have developed higher level of skills by training and are able to function with minimum level of resources. Family medicine programs developed in Nepal, South Africa and Brazil may be best suited for Indian conditions.[21,22,23]
Advantages of family medicine
Family medicine is not only a knowledge discipline but also a concept of medical education/delivery of health care services, facilitating equitable distributions of resources in a given community/ population. It is important to emphasize at this stage that family medicine should not be imported as western concept. It should be seen as logical outcome of decades of policy discussions in India.[24,25,26,27,28,29]
Skill set
For other specialties and sub specialties, the focus of training and knowledge base is vertical in nature, i.e. skills to manage rarest of the rare diseases. The approach of family medicine is horizontal and training focus is on developing skills for managing common illnesses, encompassing a wide spectrum of medical science. Within NRHM, several short-term training programs are being offered to MBBS doctors such as life saving anesthetic skills LSAS (18 weeks) and an emergency obstetric care training (16 weeks) including C–section, basic emergency obstetric care, medical termination of pregnancy (15 days), female sterilization (12 days), male sterilization (5 days), F-IMNCI, Newborn care (2 days), blood storage unit training (3 days), RTI/STIs (2 days), immunization (2 days).[18] These trainings are meant to ensure 24×7 delivery of services and should be included in core competency of family medicine training.
Expected outcomes
Family Medicine is about decentralization and democratization of clinical skills for the benefit of the community, so that individuals can avail quality care, at a price that they can easily afford. It is well-established fact that skilled family physicians can manage up to 90% of illness related problems in a given community. Other likely outcomes are following: (1) academic leadership position for primary care physicians; (2) strengthen local clinical governance; (3) research in primary care; (4) enhanced local accountability; (5) constructive feedback; (6) personalized care and increased user satisfaction; (6) maintenance of continuum of care; (7) provision of comprehensive care; (8) need based innovation in primary care.
Expansion of Ownership in Medical Education: Challenges and Proposed Interventions
We propose an integrated community based medical education model as shown in Figure 2. Pragmatic thinking and bold interventions are required in order to address the challenges for a successful implementation of such a proposal.
Figure 2.
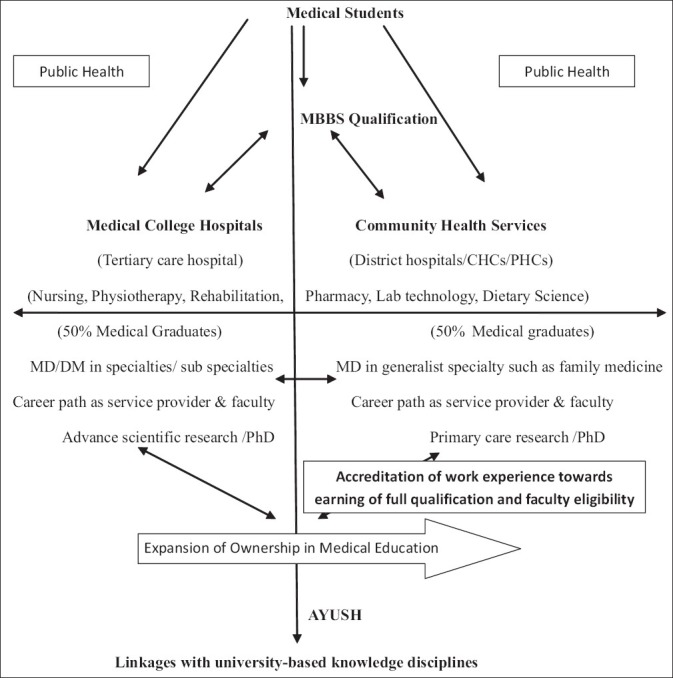
Community based integrated model of medical education (CBIMME). “Provision for full academic and professional career path for community based primary care physicians”
Training setting
Inclusion of community health services (District hospital, Community health centers and primary health centers) with tertiary health care teaching hospitals in the mainstream medical education system on equivalent basis is proposed.
Fast tract faculty development: Multiple pathways
(1) DNB family medicine—any experience after post graduate training to be considered towards faculty eligibility; (2) Post graduation in broad specialty such as general medicine, pediatrics, OBG, general surgery and public health working in community (DH + CHC + PHC) to be considered as faculty eligibility for family medicine; (3) New faculty: for MBBS doctors working in community, dual program of PG qualification and faculty development should be designed; (4) With in NRHM, trainers of short-term training programs such as EOC, LSAS should be designated as faculty for family medicine; (6) International family medicine faculty of Indian origin could be engaged; (7) Accreditation of existing work force (GPs) through international collaborations such as MRCGP (International) qualification with RCGP UK towards faculty eligibility.
Practice location of faculty and practitioners
Faculty should be placed and allowed full growth essentially in community setting. They shall have all privileges at par with faculty located at tertiary health care based medical college. They shall be allowed to have necessary unlimited access to educational resources located at medical colleges. Academic accreditation of the family practice clinics shall also be required.
District community medical college
Shift in conceptual design from traditional tertiary care based medical college to community based medical education with strong horizontal spread and component is required. The clinical departments shall be in the community setting and MBBS students be posted directly at community health centers.
Competencies and module-based curriculum
Competencies based on community needs should be defined. Modular rearrangement should be allowed with respect to time and content, allowing local flexibility. No differentiation and preferential treatment should be allowed once full qualification has been attained. Regional flexibility in curriculum and competency skills should be allowed.
Formal delinking of “license to practice (MBBS qualification)” and “faculty eligibility” for basic science and public health
Non-availability of faculty for non-clinical subjects is one of the major bottlenecks in equitable distribution of medical education. This barrier is monopolistic as strong resistance from the professional groups is observed against inclusion of faculty from non-medical background.
National medical faculty eligibility test
To overcome faculty shortage a national medical faculty eligibility test is proposed on the pattern of University Grant Commission National Eligibility Test (UGC NET). This shall function as one of the several enabling mechanisms toward faculty eligibility.
Continuous professional development and distance education
Advance IT enabled distance education, digital knowledge library and equitable access to community medical colleges shall be imbibed with in the infrastructure development design. Essentiality and availability of continuing medical education (CME), and continuous professional development (CPD) shall form core strategy for maintaining academic standards.
Addressing monopolistic regulations and conflict of interests
Identification of monopolistic regulations and conflict of interests within human resource in health planning is essential to develop a rational vision of medical education. Although, a pediatric endocrinologist working at a corporate hospital in a metropolitan city and a primary care physician working at primary health center in Jharkhand state belong to same profession, both pursue entirely different vocations. They cannot be substituted for each other. In the present scenario, the primary care physicians are not eligible to become faculty and are not represented anywhere within the medical education delivery system. The professionals pursuing other vocations are likely to carry a vocational bias in their observations and recommendations.
Academic accreditation of community health services
Development of background papers for infrastructure, faculty development, administrative processes, financial planning, support staff etc is required. In spite of funding from NRHM, to start DNB family medicine at district hospitals in several states, the scheme did not take off properly due to the absence of any authoritative and definitive guidelines for administrators to organize training.
Standardization of examination
The current examination pattern in the mainstream medical colleges is outdated and does not examine candidates objectively for competencies. There is no objective evaluation for consultation skills, counseling and clinical skills etc. This may be one of the reasons for deteriorating doctor patient relationship. Often, a lag is observed between earning of qualification and developing competencies. Also required is the development of a standardized examination and assessment system to award academic qualifications to those who have acquired skills and competencies by experience through the practice route.
Research in primary care
Large workforce of primary care physicians, engaged in private and government sector do not engage in academic audit and research. Operating within administrative framework, the untold rule is “treat but do not report” resulting in aberrations in assessment of morbidity. Primary care physicians though take care of large sections of populations and come across variety of clinical conditions, however do not have any process of recording their experience. Lack of academic authority positions them at the bottom of the administrative hierarchy and therefore renders them unable to exert positive feedback.
Role in national programs
Externally funded and remotely controlled programs designed to achieve time bound targets without local academic governance and audit is bound to precipitate large scale administrative inefficiency and financial irregularities as evident in few states implementing National Rural Health Mission (NRHM).[30] Community-based academic processes strengthen accountability, accuracy in data gathering and development of comprehensive community need-based interventions.
Conclusion
This paper discusses medical education only for the practical purpose. An effective primary care system requires team work of physicians as well as empowered paramedical professionals. Reform in medical education seeking to designate primary care physicians with needful recognition and status is also expected to give due space and equivalent opportunity to professionals such as nurses, pharmacists, lab technicians etc in the health system. The concept of community-based medical education challenges the existing medical education design in India and seeks to ease key bottlenecks in medical education reforms. This proposal runs risk of resistance and outright rejection. Not an easy one, however, this is the way forward.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Sathe PV, Sathe AP. epidemiology and management for health care for all. 1st ed. Mumbai: Popular Prakashan Pvt. Ltd; 1991. Medical education and management training; pp. 171–94. [Google Scholar]
- 2.World Health Organisation. World Health Statistics 2011. [Last cited on 2012 Jan 15]. Available from: http://www.who.int/gho/publications/world_health_statistics/EN_WHS2011_Full.pdf .
- 3.Key Highlights from Rural Health Statistics in India 2010. [Last cited on 2012 Jan 15]. Available from: http://nrhm-mis.nic.in/UI/RHS/RHS%202010/RHS%202010/Key%20Highlights%20from%20Rural%20Health%20Statistics%20in%20India.pdf .
- 4.Shrinivasan R. ‘86% of all medical trips are made by rural Indians’ - The Times of India 2010 Nov 11. [Last cited on 2012 Jan 15]. Available from: http://www.articles.timesofindia.indiatimes.com/2010-11-11/india/28253232_1_trips-medical-tourism-rural-areas .
- 5.Kumar AK, Chen LC, Choudhury M, Ganju S, Mahajan V, Sinha A, et al. Financing healthcare for all: Challenges and opportunities. Lancet. 2011;377:668–79. doi: 10.1016/S0140-6736(10)61884-3. [DOI] [PubMed] [Google Scholar]
- 6.Samal I. Primary healthcare catches on Business Standard Chennai/ Hyderabad 2012 January 6. [Last cited on 2012 Jan 15]. Available from http://www.business-standard.com/india/news/primaryhealthcare-catches-on/460842 .
- 7.Millennium Development Goals, India Country Report 2005. [Last cited on 2012 Jan 15]. Available from: http://www.unicef.org/india/ssd04_2005_final.pdf .
- 8.Annual report on health to the people of India - Ministry of Health and Family Welfare Government of India 2010. [Last cited on 2012 Jan 15]. Available from: http://www.mohfw.nic.in/WriteReadData/l892s/9457038092AnnualReporthealth.pdf .
- 9.National Conference on Health Professions Education 2011 – Concluding Statement. The Hindu 2011 October 19. [Last cited on 2012 Jan 15]. Available from: http://www.thehindu.com/news/resources/article2551581.ece#.Tqi8zkY8N5w.mailto .
- 10.Rao S. Medical education: It is time for a health check, Indian Express, 2011 Fri Feb 25. [Last cited on 2012 Jan 15]. Available from: http://www.indianexpress.com/news/medical-education-it-is-time-fora-health-c/754613 .
- 11.High Level Expert Group report on universal health coverage in India. The Planning Commission. 2011. [Last cited on 2012 Jan 15]. Available from: http://www.planningcommission.nic.in/reports/genrep/rep_uhc0812.pdf .
- 12.About Medical Council of India. [Last cited on 2012 Jan 15]. Available from: http://www.mciindia.org/AboutMCI/Introduction.aspx .
- 13.Report of the Working Group on the Tertiary Care Institutions for 12th Five Year Plan (2012-2017) [Last cited on 2012 Jan 15]. Available from: http://www.planningcommission.nic.in/aboutus/committee/wrkgrp12/health/WG_2tertiary.pdf .
- 14.Bhat S, D’souza L, Fernandez J. Factors influencing the career choices of medical graduates, JCDR doi: 3652 (published online first 7th Jan 2012) [Last cited on 2012 Jan 15]. Available from: http://www.jcdr.net/articles/PDF/1820/3652_E(V)_F(J)_Pf3(V)_PFA(A_).pdf .
- 15.Kaushik M, Jaiswal A, Shah N, Mahal A. High-end physician migration from India. Bull World Health Organ. 2008;86:40–5. doi: 10.2471/BLT.07.041681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumar R, Dhaliwal U. Career choices of undergraduate medical students. Natl Med J India. 2011;24:166–9. [PubMed] [Google Scholar]
- 17.Raha S, Berman P, Saran I, Verma T, Bhatnagar A, Awasthi S, et al. Career preferences of medical and nursing students in Uttar Pradesh: A Qualitative Analysis”. HRH technical report 3. [Last cited on 2012 Jan 15]. Available from: http://www.hrhindia.org/assets/images/Paper-III.pdf .
- 18.Report of the Working Group on National Rural Health Mission (NRHM) for the Twelfth Five Year Plan (2012-2017) [Last cited on 2012 Jan 15]. Available from: http://www.planningcommission.nic.in/aboutus/committee/wrkgrp12/health/WG_1NRHM.pdf .
- 19.Gyeman JP. Family practice in evolution: Progress, problems and projections. N Engl J Med. 1978;298:593–601. doi: 10.1056/NEJM197803162981104. [DOI] [PubMed] [Google Scholar]
- 20.PTI. President Pratibha Patil dissolves Medical Council of India, The Times of India 2010 May 15. [Last cited on 2012 Jan 15]. Available from: http://www.articles.timesofindia.indiatimes.com/2010-05-15/india/28317112_1_mci-president-medical-educationindian-medical-council-act .
- 21.Butterworth K, Hayes B, Neupane B. Retention of general practitioners in rural Nepal – A qualitative study. Aust J Rural Health. 2008;16:201–6. doi: 10.1111/j.1440-1584.2008.00976.x. [DOI] [PubMed] [Google Scholar]
- 22.Mash B, Couper I, Hugo J. Building consensus on clinical procedural skills for South African family medicine training using the Delphi technique SA. Fam Pract. 2006;48:14. [Google Scholar]
- 23.Harris M, Haines A. Brazil's family health programme. BMJ. 2010;341:c4945. doi: 10.1136/bmj.c4945. [DOI] [PubMed] [Google Scholar]
- 24.Health Committee and Commission Reports 1946-2005. [Last cited on 2012 Jan 15]. Available from: http://www.nrhm-mis.nic.in/ui/who/GOIwho-link.htm .
- 25.National Health Policy 2002 (India) MOHFW GOI. [Last cited on 2012 Jan 15]. Available from: http://www.mohfw.nic.in/NRHM/Documents/National_Health_policy_2002.pdf .
- 26.National Knowledge Commission: Recommendations. [Last cited on 2012 Jan 15]. Available from: http://www.knowledgecommission.gov.in/recommendations/medical2.asp .
- 27.Report: Task Force on Medical Education for the National Rural Health Mission. [Last cited on 2012 Jan 15]. Available from: http://www.mohfw.nic.in/NRHM/Documents/Task_Group_Medical_Education.pdf .
- 28.Vision 2015: Medical Council of India. [Last cited on 2012 Jan 15]. Available from: http://www.mciindia.org/tools/announcement/MCI_booklet.pdf .
- 29.Sinha K. Family doc concept back in business, Times of India 2012 Jan 3. [Last cited on 2012 Jan 15]. Available from: http://www.afpionline.com .
- 30.PTI. NRHM scam: Rs 5,000 crore unaccounted spending, The Hindu 2012, 21st Jan. [Last cited on 2012 Jan 15]. Available from: http://www.thehindu.com/news/states/other-states/article2820437.ece .


