Abstract
Rubella is a common cause of rash and fever during childhood. However, its public health importance relates to the teratogenic effects of primary rubella infection occurring in pregnant women, which can lead to fetal death with spontaneous abortion or to congenital defects in surviving infants. Most of the cases are asymptomatic and difficult to diagnose on clinical grounds. Detection of specific IgM antibodies by the enzyme-linked immunosorbent assay (ELISA) technique is a useful method for diagnosis. The present study was conducted on 180 pregnant women attending antenatal clinics at Government Maternity Hospital, Tirupati. All the serum samples were tested for Rubella-specific IgM antibodies. A seropositivity of 12.67% was observed among cases with bad obstetric history and 6.67% in normal pregnant women. Within the test group, high sero-positivity (13.33%) was observed in women with repeated abortions followed by in cases of intrauterine death (12.73%). The results indicate high prevalence of rubella in our population. All antenatal cases should be routinely screened for rubella, so that early diagnosis will help in proper management and fetal outcome.
Keywords: Rubella IgM, bad obstetrical history, antenatal Care, intrauterine death
Introduction
Rubella is a well-known viral disease which typically manifest as a self-limited disease characterized by erythematous maculopapular rash, low-grade fever, and mild respiratory symptoms.[1] Infection in any pregnant women can cause miscarriage, stillbirth, or multiple congenital rubella syndrome, characterized by cataract, patent ductus arteriosus, septaldefects, pulmonary artery stenosis, sensorineural deafness, meningoencephalitis, Intrauterine growth retardation (IUGR), and osseous changes. The major concern of this disease is that it can cause a serious, often fatal, congenital rubella syndrome (CRS) in newborns, especially when infection occurs during the first trimester.[1] The percentage of infection in the fetuses of mothers infected by Rubella during first trimester of pregnancy is greater than 80%. Seroprevalence of rubella infection in pregnant women in India varies from 6.5% in asymptomatic to 26.8% in pregnant females with bad obstetric history. Detection of specific IgM by enzyme-linked immunosorbent assay (ELISA) is a useful method for diagnosis of rubella infection and may be helpful in determining the causative role of rubella in abortions and still births.[2]
Materials and Methods
A this study was conducted on 180 blood samples taken from antenatal women who attended Government Maternity Hospital, attached to Sri Venkateswara Medical College, Tirupati. The cases were divided into two groups. Group I (study group) included 150 blood samples from antenatal women in the reproductive age group with history of previous unfavorable fetal outcome in terms of two or more consecutive fetal deaths, intra-uterine growth retardation, still birth, early neonatal death, and/or congenital anomalies. In group II included blood from 30 antenatal women with normal pregnancy outcome in previous pregnancies as the control group. Among the test group, 90 samples were from antenatal women with history of repeated abortions, 55 from cases with history of intra uterine death, 4 from preterm delivery, and 1 from case with history of congenital anomalies during previous pregnancy. All the samples were screened for Rubella-specific IgM antibodies by ELISA using “RUB IgM” kit (Immuno Vision, USA) following the manufacturer's instructions.
Results
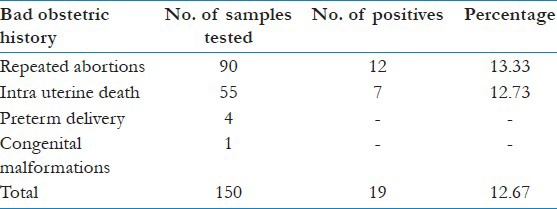
Of the 180 samples tested, 150 were from women with Bad obstetric history (BOH) and the remaining 30 were from the women with previous normal deliveries. Of the test group, 12.67% (n=19) were positive whereas in the control group, 6.67% (n=2) were positive for IgM antibodies to Rubella [Table 1]. In our study within the test group highest percentage (13.33%) of sero-positivity was observed in pregnant women with repeated abortions followed by in intra-uterine death cases (12.73%). Twelve seropositive cases belong to pregnant women with history of abortion (13.33%) and seven seropositive cases belong to pregnant women with history of intrauterine death (12.73%) [Table 2].
Table 1.
Results of IgM antibodies among test and control groups
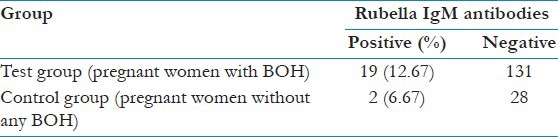
Table 2.
Test results among various subgroups of pregnant women with bad obstetric history
Discussion
Infection with rubella virus can be disastrous in early gestation. The virus may affect all organs and cause a variety of congenital defects. Infection may lead to intra uterine death, spontaneous abortion, or preterm delivery. Infection with rubella virus is initially unapparent and asymptomatic and it is difficult to diagnose on clinical grounds. Several studies in India and other countries showed the seroprevalence of rubella as 4.66% to 28.6% in women of the reproductive age group. In India, pregnant women belonging to the low socioeconomic group may be exposed to a variety of infections due to poor environment and hygiene. Maternal infections such as rubella can be considered as a significant factor in the causation of poor pregnancy outcome. Ahmed et al.[3] at Karachi, Pakistan, reported that seropositivity for rubella IgM was 18% in women with BOH and 7% in normal pregnant women.[1] In another study, Cao et al.[4] at Hefei, China, reported that 16.29% were positive for rubella IgM antibodies. Yashodara et al. in Hyderabad reported that 11 (12.5%) cases were positive for rubella IgM antibodies.[2] Mathur et al. reported that 13.8% were positive for rubella IgM antibodies.[5] Ahmed et al. reported that 26.12% were positive for rubella IgM antibodies.[6] Chopra et al. reported that 17.5% women were positive for rubella IgM antibodies.[7] Naveen Thapliyal et al reported that 28.6% cases were positive for rubella IgM antibodies.[8] In the present study, 12.67% women were positive for Rubella IgM antibodies with previous bad obstetric history and the results were similar in the studies conducted in the same state Andhra Pradesh.
Kaur et al. at Maulana Azad Medical College, New Delhi, reported that the seropositivity for rubella IgM antibodies was 8.3% with previous normal delivery.[9] In another study conducted by Zheng et al. it was reported that the seropositivity was 7.4% (109/1471).[10] In the present study, 6.67% were positive for rubella IgM antibodies with previous normal delivery showing the similar findings. This indicates that the normal pregnant women may also have rubella antibodies. It is observed that there is considerable variation in the prevalence of rubella among women of childbearing age in different geographical areas in our country.
Conclusions
The present study demonstrated a strong association between rubella infection and BOH in women. It is evident that maternal infection like rubella play a critical role in pregnancy wastage and their occurrence in women with BOH is a significant factor. A previous history of pregnancy wastage and a positive serological reaction during current pregnancy must be considered while managing BOH cases to reduce the adverse fetal outcome. Early detection and timely intervention can prevent morbidity and mortality of infants born to such mothers. All antenatal cases with BOH should be routinely screened for rubella, so that early diagnosis and appropriate intervention of these infections will help in proper management of fetal outcome. In addition to this, there is a need to modify vaccine strategies to immunize all adolescent girls and/or women of child-bearing age before conception to reduce incidence of congenital rubella syndrome and bad obstetric outcome.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Boonruang S, Buppasiri P. Rubella antibodies in normal pregnant women at Srinagarind hospital, KhonKaen Thailand. J Med Assoc Thai. 2005;88:455–9. [PubMed] [Google Scholar]
- 2.Yashodhara P, Rama Lakshmi BA, Raman L, Nadamuni Naidu. Rubella IgM positivity during pregnancy. Indian J Med Microbiol. 1998;16:121–2. [Google Scholar]
- 3.Ahmed MU. IgM and IgG antibodies specific to rubella in child bearing women. J Pak Med Assoc. 1992;42:121–2. [PubMed] [Google Scholar]
- 4.Cao Y, Qiu L, Zhang Q. Study on the relationship between the history of abnormal pregnancy and TORCH infection in pregnant women. Zhonghua Fu Chan KeZaZhi. 1999;34:517–20. [PubMed] [Google Scholar]
- 5.Mathur MS, Rele MC, Turbadkar D. Barcelona Spain: Proceedings of the XIV International AIDS Conference; 2002 July 7-12; Seroprevalence of HIV infection in bad obstetrical history and its correlation with TORCH and VDRL. [Google Scholar]
- 6.Fomda BA, Thokar MA, Farooq U, Sheikh A. Seroprevalence of rubella in pregnant women in Kashmir. Indian J Pathol Microbiol. 2004;47:435–7. [PubMed] [Google Scholar]
- 7.Chopra S, Arora U, Aggarwal A. Prevalence of IgM antibodies to toxoplasma, rubella and cytomegalovirus infections during pregnancy. J K Sci. 2004;6:190–2. [Google Scholar]
- 8.Thapliyal N, Shukla PK, Kumar B, Upadhyay S, Jain G. TORCH infection in women with bad obstetric history a pilot study in Kumaon region. Indian J Pathol Microbiol. 2005;48:551–3. [PubMed] [Google Scholar]
- 9.Kaur R, Gupta N, Nair D, Kakkar M, Mathur MD. Screening for TORCH infections in pregnant women: A report from Delhi. Southeast Asian J Trop Med Public Health. 1999;30:284–6. [PubMed] [Google Scholar]
- 10.Zheng F, Du J, Hu Y. A study of rubella infection during pregnancy. Zhonghua Fu Chan KeZaZhi. 2002;37:391–4. [PubMed] [Google Scholar]


