Abstract
Drug rash with eosinophilia and systemic symptoms (DRESS) syndrome is a severe, idiosyncratic, multi-system reaction characterized by the clinical triad of fever, rash, and internal organ involvement. The mortality rate is estimated to be 8%, especially among patients with liver involvement, so early recognition is imperative. Drugs commonly associated with the development of DRESS syndrome include anticonvulsants, long-acting sulfonamides, and anti-inflammatory medications; however, there are no reported cases implicating anti-tuberculosis (anti-TB) medications. We report a case of DRESS syndrome from anti-TB therapy. A 68-year-old male with pulmonary TB presented with pruritic skin eruption and sore throat, 8 weeks after starting Rifampin, Isoniazid, Pyrazinamide, and Ethambutol (RIPE) therapy. He takes metformin and glyburide for diabetes. Physical exam was significant for diffuse, exfoliative erythematous macules with target lesions involving the entire skin surface, without mucosal involvement. Laboratory data was significant for mild transaminitis and new onset eosinophilia. Given suspicion of drug eruption, RIPE therapy was discontinued. Skin biopsy confirmed erythema multiforme. Despite discontinuation of the implicated medications, eosinophilia and transaminitis continued to worsen, and so systemic corticosteroids were started. After 4 weeks of discontinuation of RIPE therapy, the cutaneous eruption resolved and laboratory data returned to normal. The patient is finishing course of anti-TB with cycloserine and moxifloxacin. Upon follow up as outpatient, the rash was resolving and disappeared in 1 month. DRESS syndrome is always considered when there is high eosinophil counts and multisystem involvement with skin eruptions. It can be potentially life threatening with certain drugs and infectious agents in predisposed individuals. It is imperative to discontinue the causative medication and avoid re-exposure.
Keywords: Anti TB medication, DRESS syndrome, ethambutol, isoniazide (INH), pyrazinamide, rifampicin
Introduction
Drug rash with eosinophilia and systemic symptoms (DRESS) syndrome is a severe, idiosyncratic, multi-system reaction characterized by the clinical triad of fever, rash, and internal organ involvement. The mortality rate is estimated to be 8%, especially among patients with liver involvement, so early recognition is imperative. Drugs commonly associated with the development of DRESS syndrome include anticonvulsants, long-acting sulfonamides, and anti-inflammatory medications; however, there are no reported cases implicating anti-tuberculosis (anti-TB) medications. We report a case of DRESS syndrome from anti-TB therapy.
Case Report
A 68-year-old Filipino man with history of diabetes and newly diagnosed pulmonary tuberculosis (TB) on rifampin, INH, ethambutol, and pyrazinamide presented to clinic with diffuse skin eruption for past 7-10 days. The patient initially developed a pruritic rash that began on his neck and eventually covered most of his body. The patient reports soreness with swallowing that started 7 days ago but denies any regurgitation. Exam was significant for diffuse, confluent, blanching, erythematous macular rash on face, scalp, upper extremities, including palms and soles, abdomen, buttocks, upper and lower extremities, no bullae formation, and no excoriation. There were moist mucous membranes, lips slightly edematous, dry, cracking, no blistering, and good dentition without abscesses. There was no conjunctival involvement [Figure 1]. The patient was directly admitted form clinic to University Hospital. The patient was seen by both Dermatology and Allergy/Immunology service. All four TB medications were immediately discontinued because of possible suspicion of allergic reaction. Intravenous hydration was started with normal saline at 100 ml/h with electrolytes supplementation. On admission, the laboratory findings were significant for eosinophilia and transaminitis. The patient was started on steroid cream to face twice a day as per recommendations from Dermatology for erythema multiforme. Next day of admission, the patient had worsen eosinophilia and transaminitis. Punch biopsy skin was found to be erythema multiforme. During the hospital course, the patient had desquamation of skin so he was started on steroids and later was discharged on day 10 on TB therapy and 3-week tapering dose of prednisone as well as second-line TB therapy cycloserine and moxifloxacin, as an outpatient recommended by the Pulmonary team. After 2 weeks of follow up as outpatient, there was regression in rashes of the patient and after 1 month the rashes disappeared. The eosinophils normalized on repeat labs [Figure 2].
Figure 1.

Rash
Figure 2.

Rash before and after treatment
Discussion
To our knowledge, this is the first reported case of DRESS syndrome caused by anti-TB medications. A systemic allergic reaction to anticonvulsant therapy was first described in 1950 and was named anticonvulsant hypersensitivity syndrome when associated with phenytoin therapy.[1] Since then it has been known as drug hypersensitivity syndrome and is now more often referred to as DRESS syndrome, when it involves a case of “drug rash with eosinophilia and systemic symptoms.”[1,2] DRESS syndrome is a specific, severe, idiosyncratic drug reaction characterized by a skin rash with fever, facial edema, lymphadenopathy, and visceral involvement (hepatitis, pneumonitis, myocarditis, nephritis, and colitis). The diagnosis can be difficult because many of the clinical features can be nonspecific, and the syndrome often mimics infectious, neoplastic, or rheumatologic conditions.
The diagnosis of DRESS syndrome involves three criteria as follows.
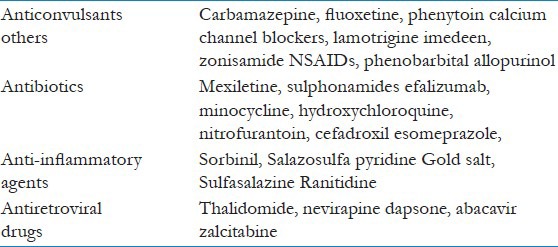
1) Drug-induced skin eruption. 2) Eosinophilia ≥1.5 × 109/L or atypical lymphocytes. 3) At least one of the following systemic abnormalities: Enlarged lymph nodes at least 2 cm in diameter, hepatitis, interstitial nephropathy, interstitial lung disease, or myocardial involvement. The pathogenesis is likely to be a drug-induced hypersensitivity caused by abnormalities in the production and detoxification of its active metabolites. A genetic predisposition may also exist, as evidenced by an increased risk in patients with a family history of DRESS syndrome. The syndrome may be related to epoxide hydrolase deficiency, which leads to accumulation of toxic metabolites, known as arene oxides that may trigger an immunologic response. An association between human herpesvirus 6 infection and the development of DRESS syndrome has been suggested in susceptible patients.[3,4,5] DRESS syndrome can be life threatening and it has a documented mortality rate of about 10%,[6] especially in patients who have liver involvement. All kinds of drugs can be involved. The syndrome is most frequently seen in association with anticonvulsants and antibiotic agents. An overview is shown in Table 1.
Table 1.
Other diagnoses for skin abnormalities after drug use include Stevens-Johnson Syndrome (SJS)/Toxic Epiderma Necrolysis (TEN), pustular drug eruptions, and erythematous drug eruptions in general. The causative drugs for SJS/TEN are for the greater part similar to those of DRESS syndrome. Also, carbamazepine-induced fulminant hepatic failure in the setting of DRESS syndrome has been described.[4,5] Cases of DRESS syndrome associated with colitis have also been described.[17] To our knowledge, this is the first report of concomitant subfulminant hepatitis and colitis in the patient. Early withdrawal of the offending medication is the first best step. The recovery from this condition has been reported to be slow, lasting several weeks to months; recurrences have also been reported.[14] Glucocorticoids remain the most widely used agents for treatment of DRESS syndrome and can result in clinical improvement although well-controlled clinical trials are lacking. No randomized controlled trials of corticosteroids in the treatment of DRESS syndrome are available. Relapse can occur during the tapering of glucocorticoids.[15] Successful use of IV immune globulin in nevirapine-induced DRESS syndrome has been reported.[3] In our patient, use of glucocorticoid helped to prevent progression of disease. Avoiding re-exposure is recommended and first-degree relatives of an afflicted individual have a four-fold increased risk of drug sensitivity; therefore, family counseling is recommended.
Conclusion
DRESS syndrome is always considered when there is high eosinophil count and multisystem involvement with skin eruptions. It can be a potentially life-threatening condition with certain drugs and infectious agents in predisposed individuals. It is imperative to discontinue the causative medication and avoid re-exposure.[20]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (drug rash with eosinophilia andsystemiic symptoms: DRESS) Semin Cutan Med Surg. 1996;15:250–7. doi: 10.1016/s1085-5629(96)80038-1. [DOI] [PubMed] [Google Scholar]
- 2.Chang CC, Shiah IS, Yeh CB, Wang TS, Chang HA. Lamotrigine-associated anticonvulsant hypersensitivity syndrome in bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30:741–4. doi: 10.1016/j.pnpbp.2005.11.033. [DOI] [PubMed] [Google Scholar]
- 3.Claudio GA, Martin AF, de Dios Perrino S, Velasco AA. DRESS syndrome associated with nevirapine therapy. Arch Intern Med. 2001;161:2501–2. doi: 10.1001/archinte.161.20.2501. [DOI] [PubMed] [Google Scholar]
- 4.Syn WK, Naisbitt DJ, Holt AP, Primohamed M, Mutimer DJ. Carbamazepine-induces acute liver failure as part of the DRESS syndrome. Int J Clin Pract. 2005;50:988–91. doi: 10.1111/j.1368-5031.2005.00550.x. [DOI] [PubMed] [Google Scholar]
- 5.Aouam K, BelHadj Ali H, Youssef M, Chaabane A, Amri M, Boughattas NA, et al. Carbamazepine-induced DRESS and HHV6 primary infection: The importance of skin tests. Epilepsia. 2008;49:1630–3. doi: 10.1111/j.1528-1167.2008.01660.x. [DOI] [PubMed] [Google Scholar]
- 6.Ghislain PD, Roujeau JC. Treatment of severe drug reactions: Stevens-Johnson syndrome, toxic epidermal necrolysis and hypersensitivity syndrome. Dermatol Online J. 2002;8:5. [PubMed] [Google Scholar]
- 7.Markel A. Allopurinol-induced DRESS syndrome. Isr Med Assoc J. 2005;7:656–60. [PubMed] [Google Scholar]
- 8.Michel F, Navellou JC, Ferraud D, Toussirot E, Wendling D. DRESS syndrome in a patient on sulfasalazine for rheumatoid arthritis. Joint Bone Spine. 2005;72:82–5. doi: 10.1016/j.jbspin.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Zuliani E, Zwahlen H, Gilliet F, Marone C. Vancomycin-induced hypersensitivity reaction with acute renal failure: Resolution following cyclosporine treatment. Clin Nephrol. 2005;64:155–8. doi: 10.5414/cnp64155. [DOI] [PubMed] [Google Scholar]
- 10.Savard S, Desmeules S, Riopel J, Agharazii M. Linezolid-associated acute interstitial nephritis and drug rash with eosinophilia and systemic symptoms (DRESS) syndrome. Am J Kidney Dis. 2009;54:e17–20. doi: 10.1053/j.ajkd.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 11.Shaughnessy KK, Bouchard SM, Mohr MR, Herre JM, Salkey KS. Minocycline-induced drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome with persistent myocarditis. J Am Acad Dermatol. 2010;62:315–8. doi: 10.1016/j.jaad.2009.05.046. [DOI] [PubMed] [Google Scholar]
- 12.Velema MS, Voerman HJ. DRESS syndrome caused by nitrofurantoin. Neth J Med. 2009;67:147–9. [PubMed] [Google Scholar]
- 13.Peyrière H, Dereure O, Breton H, Demoly P, Cociglio M, Blayac JP, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: Does a DRESS syndrome really exist? Br J Dermatol. 2006;155:422–8. doi: 10.1111/j.1365-2133.2006.07284.x. [DOI] [PubMed] [Google Scholar]
- 14.Van Leeuwen JF, van der Hooft CS, Vos LE, Bekkenk MW, van Zuuren EJ, Stricker BH. [Drug rash with eosinophilia and systemic symptoms (DRESS) attributed to the oral skin-care supplement Imedeen] Ned Tijdschr Geneeskd. 2005;149:1353–6. [PubMed] [Google Scholar]
- 15.White JM, Smith CH, Robson A, Ash G, Barker JN. DRESS syndrome caused by efalizumab. Clin Dermatol. 2007;33:50–2. doi: 10.1111/j.1365-2230.2007.02604.x. [DOI] [PubMed] [Google Scholar]
- 16.Volpe A, Marchetta A, Caramaschi P, Biasi D, Bambara LM, Arcaro G. Hydoxychloroquine-induced DRESS syndrome. Clin Rheumatol. 2008;27:537–9. doi: 10.1007/s10067-007-0772-1. [DOI] [PubMed] [Google Scholar]
- 17.Atkinson RJ, Dennis G, Cross SS, McAlindon ME, Sharrack B, Sanders DS. Eosinophilic colitis complicating anti-epileptic hypersensitivity syndrome: An indication forcolonoscopy? Gastrointest Endosc. 2004;60:1034–6. doi: 10.1016/s0016-5107(04)02233-3. [DOI] [PubMed] [Google Scholar]
- 18.Caboni S, Gunera-Saas N, Ktiouet-Abassi S, Berard F, Nicolas JF. Esomeprazole-induced DRESS syndrome. Studies of cross-reactivity among proton-pump inhibitor drugs. Allergy. 2007;62:1341–2. doi: 10.1111/j.1398-9995.2007.01428.x. [DOI] [PubMed] [Google Scholar]
- 19.Suswardana, Hernanto M, Yudani BA, Pudjiati SR, Indrastuti N. DRESS syndrome from cefadroxil confirmed by positive patch test. Allergy. 2007;62:1216–7. doi: 10.1111/j.1398-9995.2007.01392.x. [DOI] [PubMed] [Google Scholar]
- 20.Kano Y, Hiraharas K, Sakuma K, Shiohara T. Several herpes viruses can reactivate in a severe drug-induced multiorgan reaction in the same sequential order as in graft-versus-host disease. Br J Dermatol. 2006;155:301–6. doi: 10.1111/j.1365-2133.2006.07238.x. [DOI] [PubMed] [Google Scholar]


