Abstract
Systemic Lupus Erythematosus (SLE) is a connective-tissue disorder commonly affecting females of reproductive age group. Lupus Cerebritis is a serious neurological complication encountered in a good percentage of SLE cases. In this report, we discuss two Lupus Cerebritis patients, who were successfully diagnosed and treated. The first case, presented with generalized seizure, severe metabolic acidosis, and shock, with a history of fever of one-month duration. The second case manifested with an attack of generalized seizure after suffering from low-grade intermittent fever and joint pains for a duration of one-and-a-half months. Central Nervous System (CNS) involvement in SLE is caused by an inflammatory response of the autoimmune system, precipitated by an increased concentration of cytokines. Prompt identification of Lupus Cerebritis is extremely difficult, mainly because there is no single laboratory or radiological confirmatory test. Assessment of the clinical features and neurological signs, along with detection of antibodies in the serum and cerebrospinal fluid are necessary to arrive at a diagnosis. Lupus Cerebritis should be included in the provisional diagnosis of a female patient of reproductive age group, who presents with complicated neurological manifestations and with no clear-cut clinical, pathological, or image finding.
Keywords: Anti phospholipid antibody, antidouble stranded DNA, antinuclear antibody, lupus cerebritis, polyserositis, systemic lupus erythematosus
Introduction
Neuropsychiatric manifestations (depression, mania, seizures, stroke, and myopathy), at some stage of illness, occur in a good percentage of SLE patients.[1,2] Lupus Cerebritis is a CNS inflammatory response. CNS involvement in SLE is perhaps of higher incidence than diagnosed and reported. A difficult, but treatable condition, Lupus-Cerebritis can pose as a major diagnostic challenge. CNS involvement may even be the first presenting feature in undetected SLE.[2] We report two cases where the history, presenting features, and physical findings, were potentially misleading, causing significant difficulty and delay in diagnosis.
Case Reports
Case I
An unconscious middle-aged female with generalized seizure, severe metabolic acidosis, and shock, following one-month of fever, was intubated and admitted in the Intensive Care Unit (ICU). There was an indistinct discoid rash over her face and neck region. The provisional diagnosis was bacterial or viral meningitis and treatment was initiated along with fluid and electrolyte correction and hemodialysis. Injection dexamethasone was started (4 mg every eight hours) to correct hypotension and shock. Hemoglobin was 5.7 gm per dl and the total WBC count was 6400 per cmm. The computed tomography (CT) scan of the brain was normal. The cerebrospinal fluid (CSF) study was not suggestive of infective pathology. There was raised protein, total cell count 50 per cmm with 100% lymphocytes, and the adenosine deaminase (ADA) test was negative. There was effusion in the right lung base and enlarged cardiac shadow on the chest X-ray. Echocardiography reported normal left-ventricular function and minimal pericardial effusion.
The patient improved clinically during the first 24 hours and was extubated on the second day. She maintained complete alertness for the next two days, although low-grade intermittent fever persisted. The steroid was gradually tapered down, while other supportive treatment and antibiotics were continued.
The patient's condition suddenly deteriorated once the steroid was withdrawn. She suffered high fever with generalized convulsions. The hemoglobin, platelet, and WBC counts were 9 gm per dl, 105000 per cmm, and 2300 per cmm, respectively.
Her level of consciousness deteriorated further on the eighth day. She had to be re-intubated. The CT scan of the brain revealed cerebral edema. Ultrasound of the abdomen showed minimal ascites with bilateral pleural effusion. Fever was continuously high. The sepsis markers were normal (C Reactive Protein 11.7, Procalcitonin 0.07).
Ventilator support and treatment continued. There was confusion regarding the diagnosis. A board meeting was convened where it was revealed by the relatives that the patient had been on Hydroxychloroquine and naproxen tablets for joint pains, from a local physician. A connective-tissue disorder was suspected. Laboratory tests were ordered accordingly. The patient's condition remained critical and she continued to be nonresponsive. C Reactive Protein (CRP) continued to rise, while serial procalcitonin levels were normal.
Diagnosis of Systemic Lupus vasculitis with neurological involvement was confirmed on the fifteenth day, post admission. Both ANA and anti DsDNA levels were very high (174 and 315.5, respectively). C-ANCA was 0.7; P-ANCA was 2.5, and RA factor 3.07. Magnetic resonance imaging (MRI) of the brain revealed multiple microinfarctions.
Injection methylprednisolone 125 mg every eight hours was started. The fever subsided. The hemoglobin, platelet, and WBC count improved, and the pleural effusion as well as ascites resolved. Her level of consciousness improved. She was weaned from the ventilator and maintained on oxygen saturation with a tracheostomy tube. Unfortunately, it was difficult for the family to continue treatment in this institution. She was shifted to a government hospital in Kolkata with the diagnosis of Lupus-Cerebritis.
Case II
A thirty-one-year-old woman, with an episode of generalized seizure, presented to the Emergency, with a history of low-grade intermittent fever and joint pain and swelling for a duration of one-and-a-half months. She was also suffering from irregular menstrual cycles and menorrhagia. She was diagnosed by her primary physician as a case of severe rheumatoid-arthritis with anemia.
The bouts of seizures continued and she required intubation. Arterial blood gas analysis showed mild metabolic acidosis. A CT scan of the brain revealed a moderate degree of cerebral edema. Treatment was initiated with the provisional diagnosis of bacterial or viral meningitis and vasculitis.
Her level of alertness gradually deteriorated. Low-grade, intermittent fever persisted. The sepsis markers were not raised. Hemoglobin, WBC, and platelet counts were low. The CSF report revealed absolute lymphocytosis (100%) and raised protein. There were abnormal diffuse encephalitic changes in the electroencephalogram recordings. ANA by the Hep2 cell method showed a positive, homogeneous pattern. Anti DsDNA was positive. The C3 value was 88.2 mg per dl, while C4 was 21.6 mg per dl, both on the lower side of normal. Antiphospholipid antibody estimates were significant. IgG was 12.92 GPlU per ml and IgM was 3.76 MPl per ml. The final diagnosis was SLE with neuropathy, in the form of cerebritis with nephropathy, anemia, and associated disorder in the mechanism of blood clotting.
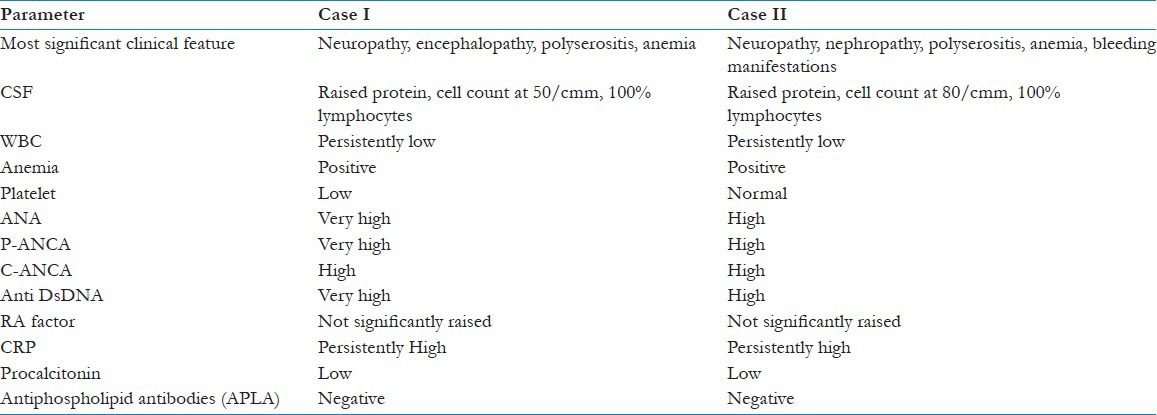
If we compare the two cases we find certain common features. The initial presentation was confusing. Only a high degree of clinical suspicion could lead to the diagnosis. We summarize the clinical, pathological, and biochemical similarities between the two subjects in Table 1.
Table 1.
Comparison between the presenting features, clinical and laboratory findings of the two cases the two cases
Discussion
Early presenting features in Lupus-Cerebritis can be potentially misleading and can create a significant diagnostic dilemma. The range of neurological symptoms varies from non-specific features like depression, anxiety, headaches, and seizures, while severe symptoms (major seizures, vision problems, dizziness, behavior changes, stroke, or psychosis) are commonly encountered in 15% of the cases. Prompt identification of Lupus-Cerebritis is extremely difficult and challenging. There is no definitive laboratory or radiological test to confirm a possible diagnosis. Assessment of the clinical features with presence of antibodies in the serum and CSF are necessary to conclude diagnosis. CNS involvement of SLE may occur, in association with other systemic manifestations of the disease or in isolation. Neurological signs can be categorized into focal, nonspecific, and neuropsychiatric.[1]
Loss of the normal control mechanism of the immune system is the basic pathological response in SLE, resulting in loss of inhibition on body's autoimmune response. On the contrary, increased plasma levels of complement breakdown products (C3a, C3d) and the formation of immune complexes in the tissues is precipitated by an enhanced complement system. Circulating auto-antibodies are formed due to the recruitment of B-lymphocytes by these immune complexes. These autoantibodies may be present in the system even before presentation of the complete clinical picture of SLE.[3] The inflammatory response of the autoimmune system, precipitated by an increased concentration of cytokines occurs during any SLE exacerbation. The circulating immune-complexes precipitate inflammatory responses causing disruption of the blood–brain barrier. C5a, another complement activation by-product has been identified as one responsible factor causing such disruptive effects, which could also be controlled with the help of a C5a receptor antagonist or a C5a antibody. Thus, it can be conjectured that the absence of a functional alternative complement pathway alleviates Lupus Cerebritis. These experimental findings have prompted researchers to suggest alternative neuroprotective approaches to SLE treatment. The alternative pathway might serve as a therapeutic target for Lupus Cerebritis, as it is the key mechanism through which complement activation occurs in the brain.[4,5]
Microinfarcts and thrombosis are mostly caused by antiphospholipidantibodies. Antiphospholipid antibodies are one of the multiple auto-antibodies in SLE that may be associated with local arterial or venous thrombosis, hemorrhagic diathesis, myelopathy, and spontaneous abortion. Vasculitis is not uncommon in Lupus-Cerebritis, often presenting with seizures, and occurs in 10% of cerebral lupus patients.[6]
Coagulopathy, described as an antiphospholipidantibodysyndrome, is precipitated by two antibodies, namely, anticardiolipin and lupus anticoagulant, which are often associated with Lupus Cerebritis cases.[1] The anticardiolipinantibodies cause pathological changes, including, endothelial damage, platelet aggregation, inflammation, and fibrosis, while the lupus anticoagulant antibody prolongs the coagulation process. Various manifestations of stroke-like disorders such as pulmonary emboli, miscarriage, thrombocytopenia, and arterial or venous thrombi, are seen in 30 to 50% of the SLE patients.[1] The second patient with menorrhagia was affected by a coagulation disorder.
A CSF study can indicate the possibility of CNS involvement in SLE by the presence of pleocytosis with a cell count typically between 100-300 cells per mm3, with predominance of lymphocytes as was the case in both the cases reported earlier in the text.[2] CSF also shows high protein levels in patients with Lupus-Cerebritis.[7] Interleukin-6 and interferon alfa may be significantly higher in the CSF of Lupus-Cerebritis patients. In severe manifestations, CSF sometimes has elevated levels of nitric oxide. Researchers have suggested that the presence of nitrates or nitrites in CSF could be used to monitor the progression of Cerebritis.[8] The neuron-reactive autoantibodies or lymphocytotoxic antibodies (LCAs) are seen in the CSF of 80% of the Lupus Cerebritis cases.[6]
Serum antibody levels are assessed to diagnose Lupus Cerebritis. The antiphospholipid antibodies, lupus-anticoagulant antibodies (i.e., IgG, IgA, IgM) antineuronal antibodies, brain-lymphocyte cross-reactive antibodies, anti-ribosomal P antibodies, antiphospholipid antibodies, anti-ganglioside antibodies, and anticardiolipin are commonly detected in the serum of such patients.[9] Complement components (C3 and C4) of a coagulation cascade show low serum and CSF concentrations. Determination of an immunological marker in the CSF is more specific of CNS involvement than that of the serum.[1] There is still an ongoing search for any specific antibody marker(s) as a gold standard for routine laboratory diagnosis, for neuropsychiatric lupus.[8,9]
Computed tomography scans in Lupus-Cerebritis may show variable features like normal brain or cerebral atrophy, calcification, infarcts, intracranial hemorrhage, or subdural fluid collections. EEG abnormalities are seen in 50 to 90% of the cases.[6] An MRI is a more sensitive diagnostic tool for Lupus-Cerebritis.[2] An abnormal MRI scan is seen in patients who presented with seizures. However, none of these imaging tools can provide definitive clue toward the diagnosis of neuropsychiatric SLE. Higher neurodiagnostic technologies are presently being applied, namely magnetic resonance spectroscopy, diffusion and perfusion weighted imaging, and magnetization transfer imaging, to arrive at early and definitive diagnosis of neuropsychiatric systemic lupus erythematosus.[10]
We have described herewith two cases of Lupus-Cerebritis, with distinct presenting features. The first patient had CNS involvement that represented limbic encephalitis. However, neither meningeal signs nor pathological reflexes were found. The diagnosis of SLE in this case was based on the presence of serositis (pleural effusion, pericardial effusion, ascites), anemia, pancytopenia, discoid rash, and neuropathy, with very high ANA and anti-DsDNA levels. Even as the general condition of the patient waxed and waned with the natural course of the disease, we failed to get a response from treatment, and the scenario became complicated with super-added infections and iatrogenic complications. Fortunately, it was not too late when an indication was available and the diagnosis was made.
The second case was diagnosed earlier, as there were suggestions of connective-tissue disorder. Laboratory reports and radiological findings were soon available and treatment was initiated. Recovery was earlier and complications were much less in the second patient.
Conclusion
Systemic lupus erythematosus is a connective-tissue disorder, commonly affecting females of the reproductive age group. Neurological involvement in SLE and its complications worsen the prognosis of the disease and treatment outcome. Therefore, among patients presenting with altered neurological features over the background of joint pain or fever or headache or confusion or psychosis, Lupus-Cerebritis should always be included in the provisional diagnosis, in order to avoid delay in diagnosis and loss of valuable time.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Kajs-Wyllie M. Lupus cerebritis: A case study. J Neurosci Nurs. 2002;34:176–83. doi: 10.1097/01376517-200208000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Raj R, Murin S, Matthay RA, Wiedemann HP. Systemic Lupus Erythematosus in the intensive care unit. Crit Care Clin. 2002;18:781–803. doi: 10.1016/s0749-0704(02)00024-6. [DOI] [PubMed] [Google Scholar]
- 3.Lalani TA, Kanne JP, Hatfield GA, Chen P. Imaging Findings in Systemic Lupus Erythematosus. Radiographics. 2004;24:1069–86. doi: 10.1148/rg.244985082. [DOI] [PubMed] [Google Scholar]
- 4.Alexander JJ, Jacob A, Vezina P, Sekine H, Gilkeson GS, Quigg RJ. Absence of functional alternative complement pathway alleviates lupus cerebritis. Eur J Immunol. 2007;37:1691–701. doi: 10.1002/eji.200636638. [DOI] [PubMed] [Google Scholar]
- 5.Jacob A, Hack B, Chiang E, Garcia JG, Quigg RJ, Alexander JJ. C5a alters blood-brain barrier integrity in experimental lupus. FASEB J. 2010;24:1682–8. doi: 10.1096/fj.09-138834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bruyn GA. Controversies in lupus: Nervous system involvement. Ann Rheum Dis. 1995;54:159–67. doi: 10.1136/ard.54.3.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Calabrese LV, Stern TA. Neuropsychiatric manifestations of systemic lupus erythematosus. Psychosomatics. 1995;36:344–59. doi: 10.1016/S0033-3182(95)71644-9. [DOI] [PubMed] [Google Scholar]
- 8.Brundin L, Svenungsson E, Morcos E, Andersson M, Olsson T, Lundberg I, et al. Central nervous system nitric oxide formation in cerebral systemic lupus erythematosus. Ann Neurol. 1998;44:704–6. doi: 10.1002/ana.410440421. [DOI] [PubMed] [Google Scholar]
- 9.Greenwood DL, Gitlits VM, Alderuccio F, Sentry JW, Toh BH. Autoantibodies in neuropsychiatric lupus. Autoimmunity. 2002;35:79–86. doi: 10.1080/08916930290016547. [DOI] [PubMed] [Google Scholar]
- 10.Govoni M, Castellino G, Padovan M, Borrelli M, Trotta F. Recent advances and future perspective in neuroimaging in neuropsychiatric systemic lupus erythematosus. Lupus. 2004;13:149–58. doi: 10.1191/0961203304lu1000rr. [DOI] [PubMed] [Google Scholar]


