Abstract
Background and Aim:
Readmission to the hospital within 30 days of discharge from the hospital is a common occurrence. Congestive heart failure is the most common cause of readmissions in the hospital. We hypothesized that irrespective of the admission diagnosis polypharmacy and potentially inappropriate use of medications (PIM) leads to readmissions within 30 days of discharge from the hospital.
Materials and Methods:
A retrospective study was carried out by reviewing the hospital records of 414 patients who were readmitted to the hospital within 30 days of discharge from the hospital between January 2008 and December 2009. The data was stratified to see which patients were on polypharmacy and/or on PIM. Polypharmacy was defined as use of more than 5 medications. PIM was defined as per the modified Beers criteria. Day 0 was defined as the day of discharge and day1 was defined as the day-after Admission to the hospital. Statistical analysis was carried out using a two-way analysis of variance (ANOVA) on the data to see if polypharmacy and/or PIM was related to readmission within 30 days of discharge irrespective of admission diagnosis.
Results:
Polypharmacy was related to hospital readmission at day 1 and day 0, however inappropriate drug use was found to be not related at any day. Polypharmacy and PIM combined had a positive correlation to readmission only on days 1 and 0 and it was statistically significant. The use of minimal and appropriate use of drugs was statistically significant compared to polypharmacy and PIM use.
Conclusions:
Polypharmacy and PIM are under recognized cause of readmissions to the hospital.
Keywords: Adverse drug reactions, Beer's Criteria, geriatric population, polypharmacy, potentially inappropriate medications, readmission
Introduction
Potentially inappropriate use of medications (PIM) use in the elderly places a significant burden on the healthcare system. In the United States incremental cost of PIM use in the elderly is estimated to be $7.2 billion,[1] PIM use in ambulatory elderly patients has been found to be 50 per 1,000 person years.[2] The elderly population is especially susceptible to use of PIM as up to 94% take at least one PIM.[3]
PIM is defined as use of a drug with risk of an adverse event that outweighs its clinical benefit, particularly when there is a safer or more effective alternative therapy for the same condition. Beers criteria to assess and reduce the risk of PIM in the elderly by identifying PIM has been developed.[4] The criteria was subsequently updated.[5,6] Utilization of this criteria has shown PIMs to be associated with a 25% increase in the risk of hospitalizations in elderly nursing home residents.[7] In addition, the incidence of PIM use has been reported to range from 22% to 66% during hospitalization, and 44% upon discharge.[8,9,10]
Geriatric population is very fragile and prone to medication side effects in view of changing physiological capacities of the body. Most notably there is a progressive linear decline in creatinine clearance.[11] The decline is much more rapid when co morbidities, especially diabetes and hypertension set in. There is a corresponding decline in other body systems, including: Cardiac, respiratory, gastrointestinal, and neurovascular. This results in accentuated drug side effects and toxicities secondary to slowed pharmacokinetics and pharmacodynamics. This is the subset of population where more and more use of polypharmacy and PIM use is observed.
However, there are very few studies available evaluating the association of PIMs with hospital readmission. Mansur and colleagues evaluated several objectives in a cohort of hospitalized elderly patients, including the relationship of PIMs with readmission and mortality, 3 months post discharge.[9] They found no significant difference in PIM use among patients who were readmitted or died as compared to those who were not readmitted or survived. However, this trial had several limitations, including a small sample size of 212 patients.
The present study was designed to see if polypharmacy and/or PIM use was related to readmission rates to the hospital irrespective of the admission diagnosis. The objective of this study was to evaluate the association of PIM use with hospital readmission within 30 days regardless of the admitting diagnosis. We hypothesized that PIM and polypharmacy would be associated with an increase in readmissions.
Materials and Methods
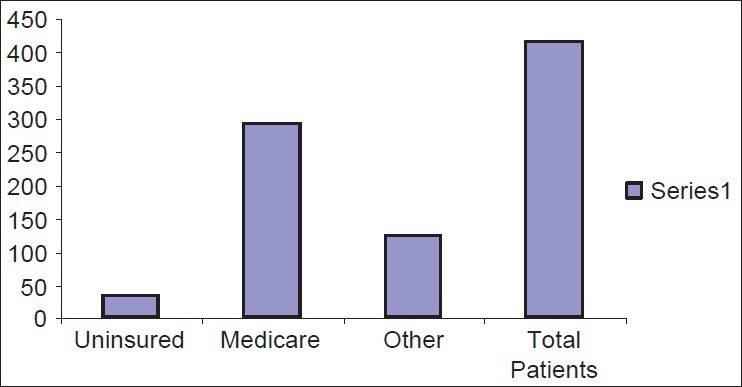
This nested case-control study included all patients readmitted within 30 days of discharge to a 250 bed community hospital located in Scranton, Pennsylvania USA. All patients 65 years of age or older admitted between January 2008 and December 2009 were eligible for study enrollment. Exclusion criteria included patients not receiving prescription medications at the time of admission. The study was conducted with approval from the hospital institutional review board. Polypharmacy was defined as use of more than five medications. PIM was defined as per the modified Beers criteria. Day 0 was defined as the day of discharge and day1 was defined as the day-after surgery. The present study included all the consecutive readmissions and no controls were used for comparison. The modified Beer's Criteria is the most widely followed drug list that is used to screen potentially inappropriate drug use in the geriatric population [Table 1].
Table 1.
Modified Beer criteria showing list of the potential associated with inappropriate usage of medicines
Selection of patients
This was a retrospective case record review of 414 patients who were hospitalized within 30 days of discharge from the hospital between January 2008 and December 2009. Four hundred and fourteen readmitted patients were randomly selected. There was no bias in the selection of patients on the basis of age, sex, co morbidities, height, weight, marital status, ethnicity, and socio-economic status.
Study design
The Institutional Review Board of Hospital approved the study and waived the requirement for informed consent for the retrospective review of medical records. The goal of the study was to identify the patient characteristics associated with readmission to the hospital within 30 days of discharge from the hospital. All the patients were screened for polypharmacy and PIM. Day 0 was defined as readmission on the same day before midnight and any readmission after midnight was defined as 1st day. Rest of the readmissions were defined as within 30 days of discharge but after day 1.
Data collection
Demographic and laboratory data was retrieved from an electronic hospital database. After merging data from the different sources, automated and manual data verification was performed.
Statistical analysis
Statistical analysis was carried out using a two-way ANOVA on the data to see if polypharmacy and/or PIM use was related to readmission within 30 days of discharge irrespective of admission diagnosis.
Results
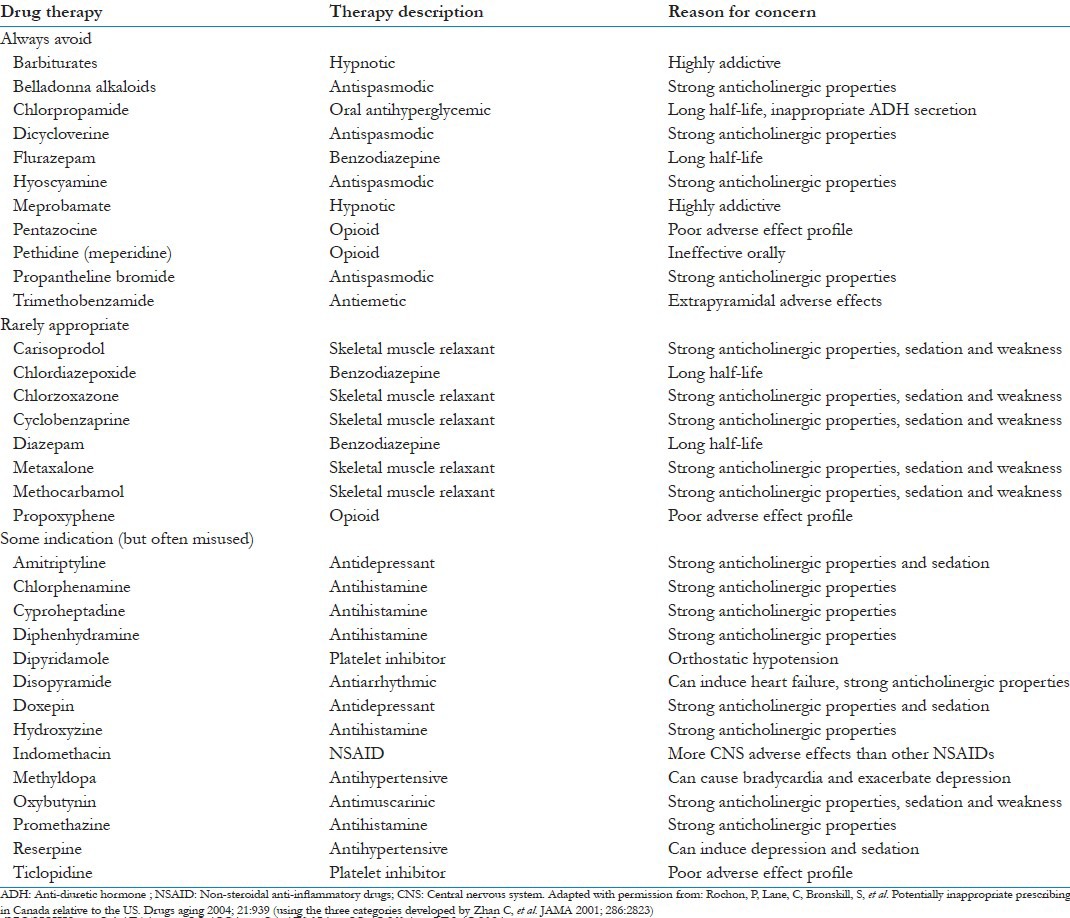
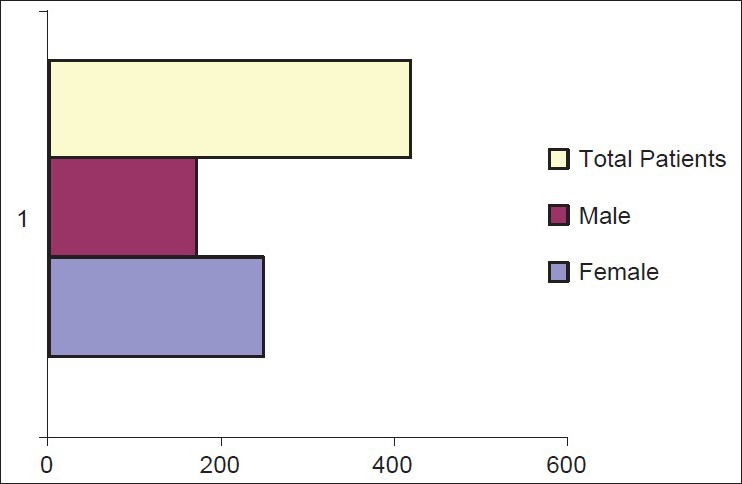
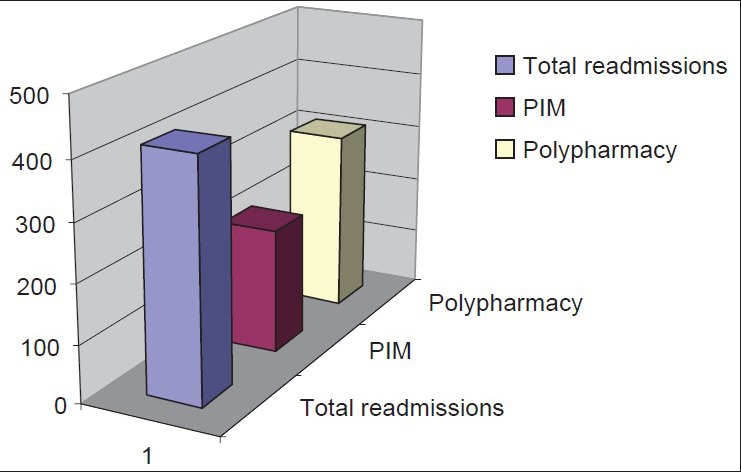
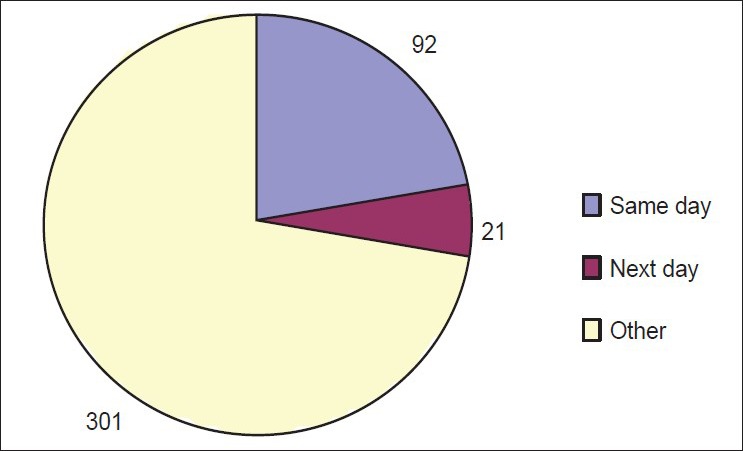
Average age of all the patients included in the study was 79.25. There were a total of 244 females and 170 males [Figure 1]. The average length of stay was 5.15 days. Of the 414 patients analyzed, 214 patients were found to be on PIM. A total of 312 patients were on polypharmacy (five or more medications at the time of admission) Figure 2. Majority of patients had medicare as their insurance Figure 3.
Figure 1.
Gender profile of readmissions
Figure 2.
Readmissions
Figure 3.
Insurance coverage
Polypharmacy and its relationship to readmission to the hospital on the same day for readmission and readmission the immediate day after discharge was statistically significant. PIM was not related to re admission on any day of readmission. The impact of polypharmacy and PIM combined on hospital readmission was statistically significant only when the readmission occurred on the same day or immediate next day. No polypharmacy and no inappropriate drugs were statistically significant as compared to polypharmacy and PIM.
At day 1 and day 0, data for all the readmissions was compiled and statistical analysis was carried out. The statistical comparison is expressed as significant (P < 0.05) and highly significant (P < 0.001) with regard to polypharmacy and PIM.
At day 1
No polypharmacy + no inappropriate drugs versus polypharmacy + inappropriate drugs: (P < 0.001)
Polypharmacy + no inappropriate drugs versus no polypharmacy + inappropriate drugs: (P < 0.05)
Poypharmacy + no inappropriate drugs versus polypharmacy + inappropriate drugs: (P < 0.05)
No polypharmacy + inappropriate drugs versus polypharmacy + inappropriate drugs: (P < 0.001)
No polypharmacy versus polypharmacy: (P < 0.001).
At day 0
No polypharmacy + no inappropriate drugs versus polypharmacy + inappropriate drugs: (P < 0.05)
No polypharmacy + inappropriate drugs versus polypharmacy + inappropriate drugs: (P < 0.05)
No polypharmacy versus polypharmacy: (P < 0.01).
Discussion
In USA, Medicare is expected to keep decreasing the healthcare reimbursements.[12] There is a trend to pay for performance and hospitals are not being reimbursed for so-called never events. The list of the never events has been gradually increasing over the last couple of years. The expansion of never events and hospital acquired conditions by Center of Medicare and Medicaid (CMS) would have a substantial financial impact on tertiary care facilities. This is in sharp contrast to earlier trends when hospitals were reimbursed irrespective of the quality of the services offered. Costs have continued to rise at double-digit rates, and quality is far from optimal.[13]
In the 21st century, we see aging of the population; the fastest growing population being people over 85 years of age.[14] We are increasingly seeing an umbrella of disease processes that accompany the aging population. Adverse drug events, which can be especially problematic in older adults, often can be prevented by detecting potential risk factors. “Many primary care doctors possess a poor knowledge of PIM and are unaware of prescribing guidelines such as the Beers Criteria.”[15] Also there is poor communication of drugs potential side effects profile between the physician and the patient.[16]
This study revealed that polypharmacy was strongly related to readmissions to the hospital. PIM was contributory but in itself did not lead to readmissions in our study. Hospital readmission within 30 days of discharge from the hospital is a multifaceted dragon which has to be dealt with a multipronged approach. A substantial amount of economic resources are spent on readmissions, especially in terms of finances. The most common cause of readmission by admitting diagnosis is congestive heart failure followed by psychosis [Figure 4]. The usual approach is to blame it on the disease process without addressing the patients’ co-morbidities. At the hospital, where this study was conducted, a substantial readmission rates in the hospitalist's service was observed. This study was designed to quantify the use of inappropriate medications among older adult outpatients.
Figure 4.
Statistically significant readmission related to polypharmacy
Polypharmacy is a multifactorial problem. Patients have a more difficult time trying to remember their drug regimen daily and can infringe on quality of life. Not to forget to mention the cost of the polypharmacy. Healthcare spending is also increased with more follow-up visits to doctor's offices. Healthcare spending can also involve the side effects caused by polypharmacy that can include acute drug reactions and readmissions.
Tracking the number of patients who experience unplanned readmissions to a hospital after a previous hospital stay is another category of data used to judge the quality of hospital care.
In USA, CMS Services began to look into the issue after a national push by the Obama administration. In USA, the president's health-care reform has identified readmission rates as a key target for medical care savings.
The Hospital Compare site allows patients to compare hospitals based on the how the rate of readmission for three treatments – Heart attack, heart failure, and pneumonia – Compare with the national average. Rates of readmission for each hospital are compared to the US National rate. The rates take into account how sick patients were before they were admitted to the hospital.[17]
The modified Beer's Criteria is the most widely followed drug list that is used to screen potentially inappropriate drug use in the geriatric population. For a complet e list of medications included in the Beer's Criteria refer to Table 1. Although it remains a useful screening tool to screen for PIM, its practical application in acute-care settings remains obscure. Critics of the Beer's Criteria opine that it is too big to be implemented in its entirety in the acute-care settings. In fact ADRs could contribute to accelerated functional decline in elderly hospitalized patients independently of the use of Beers’ listed PIMs.[4,18]
The Beer's Criteria does not include some of the common PIM. For example, pregabalin is very poorly tolerated by geriatric population and is not included in the Beer's Criteria. Furthermore, potentially any medication could be inappropriate in the geriatric population if it is not titrated by the physiological decline, especially renal decline. In this subset of population, serum creatinine is not indicative of the actual glomerular filteration rate. In our opinion, all anticholinergics, opiods, and benzodiazepams should raise a red flag, especially at the time of medication reconciliation. This would be the most practical approach to minimize the use of PIM. Consideration should be placed on benefit to risk ratio when a new medication is added. On each hospitalization there should be a diligent review of the drug profile and every effort should be made to minimize medications. Screening tool of older persons PIM (STOPP) have recently found favor as a tool for screening PIM.[19]
In the hospital setting, proton pump inhibitors (PPI) are very commonly prescribed and are the most over prescribed medications.[20] It is often continued even after the patient is discharged from the hospital. This not only compounds the cost of healthcare delivery but is detrimental to the patients’ medical management by increasing morbidity. Along with the over prescribed PPI's, a significant portion of the geriatric population is on clopidogrel because of coexistent coronary artery disease. PPI added in conjunction with Plavix has a 64% higher risk of re hospitalization for myocardial infraction MI or coronary stent placement than patients receiving Plavix alone.[21] There is also an increase in stent thrombosis in patients who are on both Plavix and PPIs.[21] Healthcare professionals should be vigilant patient advocates when it comes to polypharmacy or at least be cautious of all the side effects.
Neither Plavix nor PPI's figure in any criteria which define PIM. But the drug interaction is consistent with increased mortality and morbidity. This is to drive home the point that PIM use be at the back of the mind with a larger goal to minimize polypharmacy. Antidepressants are another class of medications, which is widely used in the geriatric population but does not figure into the Beer's Criteria. Considering the benefit to risk ratio the widespread use of antidepressants need to be minimized. If we look at the natural course of depression, 60% of the cases are self-resolving. Medication response rate to depression is 80%. So the actual net response rate to medication treatment is just 20%.[22] If we consider the side effects profile to antidepressants, there is an extensive list and of course like most other medication, side effects are more pronounced in the elderly. Antidepressants have been attributed to falls in the elderly.[23] The minimal response time is 4 weeks. Most patients are on antidepressants forever because most physicians are hesitant to taper them off.
A good discharge plan should include a meticulous medication reconciliation especially weighing the benefit to risk ratio. We would also recommend a mandated continued medical education on PIM on renewal of state license.
Conclusions
A good surgeon knows when not to operate and a good physician knows when not to give medicines. Polypharmacy is a big contributor to increasing healthcare cost and increasing morbidity as well as mortality in the elderly population. There should be focused attention on all patients whether in hospital, or in physician's follow-up clinic towards minimizing polypharmacy. If clinicians practice polypharmacy, they are bound to lead to use of PIM. In our opinion, internship year should be geared towards orienting the physicians to focus on the geriatric aspect of medicine and improve medication use in elderly population. This is important because India is seeing rapid surge of elderly with infrastructure and health care system ill equipped to handle it.
This study looked at a small picture of readmissions in a single hospital. We would need a larger prospective multicenter randomized controlled intervention study to assess the effect of optimization strategies on the appropriateness of prescribing in elderly people.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Fu AZ, Jiang JZ, Reeves JH, Fincham JE, Liu GG, Perri M., 3rd Potentially inappropriate medication use and healthcare expenditures in the US community-dwelling elderly. Med Care. 2007;45:472–6. doi: 10.1097/01.mlr.0000254571.05722.34. [DOI] [PubMed] [Google Scholar]
- 2.Gurwitz JH, Field TS, Harrold LR, Rothschild J, Debellis K, Seger AC, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003;289:1107–16. doi: 10.1001/jama.289.9.1107. [DOI] [PubMed] [Google Scholar]
- 3.Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States: The Slone survey. JAMA. 2002;287:337–44. doi: 10.1001/jama.287.3.337. [DOI] [PubMed] [Google Scholar]
- 4.Curtis LH, Østbye T, Sendersky V, Hutchison S, Dans PE, Wright A, et al. Inappropriate prescribing for elderly Americans in a large outpatient population. Arch Intern Med. 2004;164:1621–5. doi: 10.1001/archinte.164.15.1621. [DOI] [PubMed] [Google Scholar]
- 5.Beers MH. Explicit criteria for determining potentially inappropriate medication use by the elderly. An update. Arch Intern Med. 1997;157:1531–6. [PubMed] [Google Scholar]
- 6.Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: Results of a US consensus panel of experts. Arch Intern Med. 2003;163:2716–24. doi: 10.1001/archinte.163.22.2716. [DOI] [PubMed] [Google Scholar]
- 7.Ruggiero C, Dell’Aquila G, Gasperini B, Onder G, Lattanzio F, Volpato S, et al. Potentially inappropriate drug prescriptions and risk of hospitalization among older, Italian, nursing home residents: The ULISSE project. Drugs Aging. 2010;27:747–58. doi: 10.2165/11538240-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 8.Laroche ML, Charmes JP, Nouaille Y, Fourrier A, Merle L. Impact of hospitalisation in an acute medical geriatric unit on potentially inappropriate medication use. Drugs Aging. 2006;23:49–59. doi: 10.2165/00002512-200623010-00005. [DOI] [PubMed] [Google Scholar]
- 9.Mansur N, Weiss A, Beloosesky Y. Is there an association between inappropriate prescription drug use and adherence in discharged elderly patients? Ann Pharmacother. 2009;43:177–84. doi: 10.1345/aph.1L461. [DOI] [PubMed] [Google Scholar]
- 10.Harugeri A, Joseph J, Parthasarathi G, Ramesh M, Guido S. Potentially inappropriate medication use in elderly patients: A study of prevalence and predictors in two teaching hospitals. J Postgrad Med. 2010;56:186–91. doi: 10.4103/0022-3859.68642. [DOI] [PubMed] [Google Scholar]
- 11.Musso CG, Oreopoulos DG. Aging and physiological changes of the kidneys including changes in glomerular filtration rate. Nephron physiol. 2011;119(Supp1):1–5. doi: 10.1159/000328010. [DOI] [PubMed] [Google Scholar]
- 12.Satin DJ, Miles J. Performance-based bundled payments: Potential benefits and burdens. Minn Med. 2009;92:33–5. [PubMed] [Google Scholar]
- 13.Bodenheimer T. High and rising health care costs. Part 1: Seeking an explanation. Ann Intern Med. 2005;142:847–54. doi: 10.7326/0003-4819-142-10-200505170-00010. [DOI] [PubMed] [Google Scholar]
- 14.Anderson GF, Hussey PS. Population aging: A comparison among industrialized countries. Health Aff (Millwood) 2000;19:191–203. doi: 10.1377/hlthaff.19.3.191. [DOI] [PubMed] [Google Scholar]
- 15.Ramaswamy R, Maio V, Diamond JJ, Talati AR, Hartmann CW, Arenson C, et al. Potentially inappropriate prescribing in elderly: Assessing doctor knowledge, confidence and barriers. J Eval Clin Pract. 2011;17:1153–9. doi: 10.1111/j.1365-2753.2010.01494.x. [DOI] [PubMed] [Google Scholar]
- 16.Wilson IB, Schoen C, Neuman P, Strollo MK, Rogers WH, Chang H, et al. Physician-patient communication about prescription medication nonadherence: A 50-state study of America's seniors. J Gen Intern Med. 2007;22:6–12. doi: 10.1007/s11606-006-0093-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fazzi R, Agoglia R, Mazza G, Glading-DiLorenzo J. The Briggs National Quality Improvement/Hospitalization Reduction Study. Caring. 2006;25:70–5. [PubMed] [Google Scholar]
- 18.Corsonello A, Pranno L, Garasto S, Fabietti P, Bustacchini S, Lattanzio F. Potentially inappropriate medication in elderly hospitalized patients. Drugs Aging. 2009;26:31–9. doi: 10.2165/11534640-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 19.Gallagher P, O’Mahony D. STOPP (Screening tool of older persons’ potentially inappropriate prescriptions): Application to acutely ill elderly patients and comparison with Beers’ criteria. Age Ageing. 2008;37:673–9. doi: 10.1093/ageing/afn197. [DOI] [PubMed] [Google Scholar]
- 20.Gupta R, Garg P, Kottoor R, Munoz JC, Jamal MM, Lambiase LR, et al. Overuse of acid suppression therapy in hospitalized patients. South Med J. 2010;103:207–11. doi: 10.1097/SMJ.0b013e3181ce0e7a. [DOI] [PubMed] [Google Scholar]
- 21.Stockl KM, Le L, Zakharyan A, Harada AS, Solow BK, Addiego JE, et al. Risk of rehospitalization for patients using clopidogrel with a proton pump inhibitor. Arch Intern Med. 2010;170:704–10. doi: 10.1001/archinternmed.2010.34. [DOI] [PubMed] [Google Scholar]
- 22.Spinewine A. Adverse drug reactions in elderly people: The challenge of safer prescribing. BMJ. 2008;336:956–7. doi: 10.1136/bmj.39520.686458.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gallagher PF, Barry PJ, Ryan C, Hartigan I, O’Mahony D. Inappropriate prescribing in an acutely ill population of elderly patients as determined by Beers’ Criteria. Age Ageing. 2008;37:96–101. doi: 10.1093/ageing/afm116. [DOI] [PubMed] [Google Scholar]


