Abstract
Background
The objective of this study is to examine practice-level variation in rates of guideline-recommended treatment for outpatients with heart failure and reduced ejection fraction (HFREF), and to examine the association between treatment variation and practice site, independent of patient factors.
Methods and Results
Cardiology practices participating in the NCDR PINNACLE registry from July 2008 – December 2010 were evaluated. Practice rates of treatment with angiotensin converting enzyme inhibitors/angiotensin receptor blockers (ACEI/ARB) and beta blockers (BB) and an optimal combined treatment measure were determined for patients with HFREF and no documented contraindications. Multivariable hierarchical regression models were adjusted for demographics, insurance status and comorbidities. A median rate ratio (MRR) was calculated for each therapy, which describes the likelihood that the treatment of a patient with given comorbidities would differ at two randomly selected practices. We identified 12,556 patients from 45 practices. The unadjusted practice-level prescription rates ranged from 44% to 100% for ACEI/ARB (median 85%; interquartile range [IQR] 75%–89%), from 49%–100% for BB (median of 92%; IQR 83%–95%) and from 37%–100% for optimal combined treatment (median of 79%; IQR 66%–85%). The adjusted MRR was 1.11 (95% confidence interval [CI] 1.08–1.18) for ACEI/ARB therapy, 1.08 (95% CI 1.05–1.15) for BB therapy and 1.17 (1.13–1.26) for optimal combined treatment.
Conclusions
Variation in the use of guideline-recommended medications for patients with HFREF exists in the outpatient setting. Addressing practice-level differences may be an important component of improving quality of care for patients with HFREF.
Keywords: heart failure, registry, drugs
Beta-blockers (BB) and angiotensin converting enzyme inhibitors (ACEI) or angiotensin receptor blockers (ARB) are guideline-recommended therapies for ambulatory patients with heart failure and reduced ejection fraction (HFREF).1 Among patients hospitalized for heart failure, the use of these therapies in routine practice has improved.2, 3 In contrast, few quality improvement programs have focused on ambulatory care of HFREF despite national performance measures which encourage the use of these therapies in the outpatient setting.4 One program, The Registry to Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting (IMPROVE HF), demonstrated improvements in use of guideline-recommended therapies among eligible patients with HREF in outpatient cardiology practices.5
Because most heart failure care occurs in the ambulatory setting, outpatient practices are a natural focus for investigating the quality of heart failure care. However, little is known about the contribution of practice site to practice-level variation in treatment of outpatients with HFREF. Prior knowledge is limited to IMPROVE HF which observed variation in treatment for HFREF by clinic at baseline6 but did not find an association between a number of practice characteristics and improvement in use of guideline recommended therapies over time.7 This raises the question of the degree to which practice site is associated with variation in care. An understanding of outpatient practice performance, variations in care across practices and factors contributing to unnecessary variation in use of recommended therapies for HFREF is critical for developing effective interventions that could improve the quality of HF care.
The National Cardiovascular Disease Registry (NCDR) Practice Innovation and Clinical Excellence (PINNACLE) registry captures care provided in outpatient cardiology clinics and provides an opportunity to understand variability in treatment patterns among a national sample of ambulatory patients with HFREF. The aims of this study were to determine the overall rates of ACEI/ARB and BB use, to examine the degree of practice-level variation in the rates of treatment with ACEI/ARB, BB and an optimal combined treatment rate for eligible patients with HFREF, and to determine the association between practice site and variation in care, independent of patient-level factors.
Methods
Data Source
Data from the NCDR PINNACLE Registry was used for analyses. The PINNACLE program is a national office-based cardiovascular quality improvement registry with voluntary participation.8, 9 Participating practices collect data at the point of care for each out-patient visit. Data is collected at the point of care using either PINNACLE paper-based chart abstraction forms or a validated mapping algorithm from each practice’s electronic medical record to comprehensively capture requisite data elements for PINNACLE program participation.5 Data collected in the registry includes demographics, insurance information and longitudinal data on symptoms, vital signs, medications, laboratory values and comorbidities. In addition, medications are documented as prescribed or not prescribed for a medical, patient or system reason. If a medication was documented as not prescribed for any reason, the patient was considered ineligible for that medication. Data collection is standardized through standard data definitions, uniform data entry and transmission requirements, and data quality checks.
Study Population
We identified patients with HFREF (left ventricular ejection fraction ≤40%) enrolled in the NCDR PINNACLE registry between July 2008 and December 2010. Beta-blocker and ACEI/ARB therapy was considered indicated for all patients. Patients with a documented reason for not prescribing any of the studied medication classes were considered ineligible and excluded from analyses for that particular class. As we were interested in examining practice-level rates of treatment in this study, we excluded practices with fewer than 10 eligible HFREF patients or with treatment rates of 0% (n=3 practices).
Outcomes
Of primary interest was the extent of practice variation in rates of treatment with each individual medication and a composite measure. Therefore, the primary outcomes were practice-level rates of treatment with ACEI/ARB, BB, and an optimal combined treatment measure. The optimal combined treatment measure was calculated based on a method used by the Joint Commission10 and was the percentage of patients treated with all of the medications for which they were eligible. Therefore, to meet the optimal combined treatment measure, if a patient was only eligible for one medication, that one medication had to be prescribed; if a patient was eligible for both medications, both medications (ACEI/ARB and BB) had to be prescribed. Thus, the total number of patients eligible for the optimal combined treatment measure was greater than the total number eligible for each individual measure. Primary analyses were based on each patient’s first encounter in the registry. A sensitivity analysis was conducted based on all encounters within one year from the index visit.
Patient-level Factors
Patient-level variables were chosen a priori based on prior literature and clinical importance. Variables selected as candidates for the multivariable models included both: demographics (age, gender, insurance payer) and clinical factors (dyslipidemia, hypertension, diabetes, current smoker, peripheral artery disease, atrial fibrillation or flutter, history of stroke or transient ischemic attack, history of myocardial infarction (MI), angina, coronary artery bypass grafting (CABG) within the prior year, and percutaneous coronary intervention (PCI) within the prior year).
Statistical Analysis
Baseline characteristics between patients treated and not treated were compared using t tests for continuous variables and chi-square tests for categorical variables. Given that the primary unit of analysis for this study was the practice, treatment rates were determined for ACEI/ARB, BB and the composite measure for each practice and examined with descriptive plots.
Multivariable hierarchical modified Poisson regression models then were constructed to determine 1) practice-level variation in treatment rates and 2) the association between patient-level factors and treatment rates. These were 2-level hierarchical models with the practice modeled as a random effect and patient covariates as fixed effects. To quantify practice-level variation, the median rate ratio (MRR) was calculated. The MRR is determined from hierarchical models with only patient level factors included. The MRR estimates the typical rate ratio between two randomly selected practices for a patient with given covariates.11, 12 The MRR is always greater than 1.0 (an MRR of 1.0 suggests no variation between practices). Because the MRR is always greater than 1.0, the confidence intervals will be greater than 1.0 as well. The MRR allows meaningful qualitative comparisons with the effect sizes of patient factors included in hierarchical models, although a statistical measure of significance for this comparison is not available.12, 13 Thus, the magnitude of the MRR was examined relative to the magnitude of the demographic and clinical patient factors described above. No variable selection procedures were performed.
Several secondary analyses were performed. First, hypothesizing that practices with a greater number of patients with HFREF would have higher treatment rates, we evaluated the impact of the number of patients with HFREF at a practice in the multivariable models. Second, we examined the impact of the length of participation time in PINNACLE in the multivariable models. We hypothesized that practices may have a learning curve and that those with longer participation time may have higher treatment rates. Third, to exclude the possibility that higher treatment rates may represent better documentation rather than better performance, we examined the correlation between treatment rates and documentation of contraindications to medications. If better performance is due to better documentation, a high correlation between treatment rates and documented exclusions would be expected. Finally, we evaluated treatment rates by method of data collection (paper vs. via electronic health record) by adding this to the multivariable models.
The rate of missing data was 13.2% for smoking status, 5.8% for insurance status, 3.6% for PCI within 12 months, 3.4% for CABG within 12 months and 1.6% for history of MI. In order to avoid case-wise deletion of those cases with missing data points, for each of these variables a separate “missing” category was created and included in the models.
All analyses were performed using the SAS statistical package version 9.1 (SAS Institute, Cary, NC). The authors had full access to the data and take full responsibility for the integrity of the data. All authors have read and agree to the manuscript as written. The American College of Cardiology PINNACLE registry approved the analysis and the Mid America Heart Institute human investigation committee determined that informed consent was not applicable to the data collected by the registry.
Results
A total of 12,556 patients with HFREF from 43 practices were identified. Practices had a median of 13 physicians (IQR 2, 24) and 93% (n=40) were in an urban location. After accounting for contraindications to individual therapies, 12,046 patients were eligible for the ACEI/ARB treatment analyses, 12,384 for the BB treatment analyses, and 12,510 for the optimal combined treatment analyses.
At the patient level, the rate of treatment with ACEI/ARB was 79%, BB was 89% and the rate of meeting the composite was 74%. Characteristics of eligible patients who received and did not receive an ACEI/ARB, BB or the composite measure are presented in Table 1. Compared to those who did not receive treatment, those who were treated with an ACEI/ARB were younger, more frequently men and of white race; more likely to have a history of stroke, angina and atrial fibrillation; more likely to have had PCI or CABG within 12 months; and more likely to be treated with antiplatelet agents. Rates of CAD, hypertension and diabetes were similar among patients who were and were not prescribed an ACEI/ARB. Those not prescribed an ACEI/ARB were more likely to have private insurance.
Table 1.
Characteristics of eligible patients who were treated and not treated with an ACEI/ARB, BB and optimal combined measure
| ACEI/ARB among eligible N=12,046 |
P-Value | BB among eligible N=12,384 |
Composite of ACEI/ARB and/or BB among eligible N=12,510 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes n = 9,563 |
No n = 2,483 |
Yes n = 11,006 |
No n = 1,378 |
P-Value | Yes n = 9,206 |
No n = 3,304 |
P-Value | ||
| Age | < 0.001 | 0.005 | < 0.001 | ||||||
| <65 | 3498 (36.6%) | 751 (30.2%) | 3886 (35.3%) | 435 (31.6%) | 3340 (36.3%) | 1006 (30.4%) | |||
| 65 to <75 | 2681 (28.0%) | 667 (26.9%) | 3035 (27.6%) | 374 (27.1%) | 2543 (27.6%) | 900 (27.2%) | |||
| ≥75 | 3380 (35.4%) | 1065 (42.9%) | 4081 (37.1%) | 569 (41.3%) | 3319 (36.1%) | 1398 (42.3%) | |||
| Sex | 0.001 | 0.594 | 0.019 | ||||||
| Male | 6579 (68.8%) | 1628 (65.6%) | 7502 (68.2%) | 930 (67.5%) | 6315 (68.6%) | 2197 (66.5%) | |||
| Female | 2984 (31.2%) | 855 (34.4%) | 3504 (31.8%) | 448 (32.5%) | 2891 (31.4%) | 1107 (33.5%) | |||
| Race | 0.019 | 0.565 | 0.001 | ||||||
| White | 4478 (46.8%) | 1078 (43.4%) | 5070 (46.1%) | 612 (44.4%) | 4342 (47.2%) | 1425 (43.1%) | |||
| Black | 1007 (10.5%) | 283 (11.4%) | 1159 (10.5%) | 158 (11.5%) | 956 (10.4%) | 368 (11.1%) | |||
| Other | 43 (0.4%) | 9 (0.4%) | 47 (0.4%) | 7 (0.5%) | 39 (0.4%) | 15 (0.5%) | |||
| Missing | 4035 (42.2%) | 1113 (44.8%) | 4730 (43.0%) | 601 (43.6%) | 3869 (42.0%) | 1496 (45.3%) | |||
| Insurance | < 0.001 | < 0.001 | < 0.001 | ||||||
| None | 456 (4.8%) | 97 (3.9%) | 514 (4.7%) | 49 (3.6%) | 437 (4.7%) | 130 (3.9%) | |||
| Private | 4680 (48.9%) | 1383 (55.7%) | 5398 (49.0%) | 774 (56.2%) | 4406 (47.9%) | 1826 (55.3%) | |||
| Public | 3838 (40.1%) | 922 (37.1%) | 4420 (40.2%) | 511 (37.1%) | 3743 (40.7%) | 1241 (37.6%) | |||
| Unknown | 589 (6.2%) | 81 (3.3%) | 674 (6.1%) | 44 (3.2%) | 620 (6.7%) | 107 (3.2%) | |||
| Current Tobacco Use | 0.053 | < 0.001 | < 0.001 | ||||||
| No | 7228 (75.6%) | 1887 (76.0%) | 8446 (76.7%) | 972 (70.5%) | 7046 (76.5%) | 2476 (74.9%) | |||
| Yes | 1064 (11.1%) | 239 (9.6%) | 1193 (10.8%) | 133 (9.7%) | 1016 (11.0%) | 321 (9.7%) | |||
| Unknown | 1271 (13.3%) | 357 (14.4%) | 1367 (12.4%) | 273 (19.8%) | 1144 (12.4%) | 507 (15.3%) | |||
| CAD | 7199 (75.3%) | 1845 (74.3%) | 0.317 | 8314 (75.5%) | 996 (72.3%) | 0.008 | 6968 (75.7%) | 2439 (73.8%) | 0.033 |
| Dyslipidemia | 6635 (69.4%) | 1710 (68.9%) | 0.640 | 7720 (70.1%) | 877 (63.6%) | < 0.001 | 6435 (69.9%) | 2246 (68.0%) | 0.042 |
| Diabetes | 3080 (32.2%) | 806 (32.5%) | 0.793 | 3621 (32.9%) | 388 (28.2%) | < 0.001 | 3007 (32.7%) | 1034 (31.3%) | 0.154 |
| Hypertension | 7440 (77.9%) | 1938 (78.6%) | 0.459 | 8552 (77.8%) | 1055 (76.8%) | 0.409 | 7117 (77.4%) | 2574 (78.3%) | 0.283 |
| PAD | 1733 (18.1%) | 421 (17.0%) | 0.181 | 1932 (17.6%) | 260 (18.9%) | 0.230 | 1618 (17.6%) | 587 (17.8%) | 0.796 |
| Prior Stroke/TIA | 1689 (17.7%) | 340 (13.7%) | < 0.001 | 1763 (16.0%) | 287 (20.8%) | < 0.001 | 1536 (16.7%) | 528 (16.0%) | 0.355 |
| Angina | 1086 (11.4%) | 228 (9.2%) | 0.002 | 1238 (11.3%) | 141 (10.3%) | 0.261 | 1075 (11.7%) | 318 (9.7%) | 0.002 |
| Antiplatelet | 6912 (72.3%) | 1471 (59.2%) | < 0.001 | 7831 (71.2%) | 816 (59.2%) | < 0.001 | 6727 (73.1%) | 2009 (60.8%) | < 0.001 |
| Atrial Fibrillation | 2899 (30.3%) | 822 (33.1%) | 0.007 | 3430 (31.2%) | 425 (30.8%) | 0.799 | 2828 (30.7%) | 1072 (32.5%) | 0.063 |
| PCI within 12 months | < 0.001 | 0.080 | < 0.001 | ||||||
| No | 7247 (75.8%) | 2076 (83.6%) | 8540 (77.6%) | 1074 (77.9%) | 7019 (76.2%) | 2701 (81.7%) | |||
| Yes | 1975 (20.7%) | 345 (13.9%) | 2059 (18.7%) | 269 (19.5%) | 1819 (19.8%) | 520 (15.7%) | |||
| Unknown | 341 (3.6%) | 62 (2.5%) | 407 (3.7%) | 35 (2.5%) | 368 (4.0%) | 83 (2.5%) | |||
| CABG within 12months | < 0.001 | 0.017 | < 0.001 | ||||||
| No | 7856 (82.1%) | 1956 (78.8%) | 8947 (81.3%) | 1159 (84.1%) | 7573 (82.3%) | 2644 (80.0%) | |||
| Yes | 1384 (14.5%) | 471 (19.0%) | 1679 (15.3%) | 187 (13.6%) | 1286 (14.0%) | 586 (17.7%) | |||
| Unknown | 323 (3.4%) | 56 (2.3%) | 380 (3.5%) | 32 (2.3%) | 347 (3.8%) | 74 (2.2%) | |||
| History of MI | 0.425 | < 0.001 | 0.005 | ||||||
| No | 5938 (62.1%) | 1577 (63.5%) | 6772 (61.5%) | 944 (68.5%) | 5661 (61.5%) | 2132 (64.5%) | |||
| Yes | 3465 (36.2%) | 865 (34.8%) | 4061 (36.9%) | 409 (29.7%) | 3400 (36.9%) | 1115 (33.7%) | |||
| Unknown | 160 (1.7%) | 41 (1.7%) | 173 (1.6%) | 25 (1.8%) | 145 (1.6%) | 57 (1.7%) | |||
Compared to those who were not treated, those who were treated with a BB were younger, more likely non-smokers, and more likely to have CAD, dyslipidemia, diabetes, prior MI, CABG within the past 12 months and be treated with antiplatelet agents. Those not prescribed a BB were more likely to have private insurance and to have a history of stroke. Finally, patients meeting the optimal combined treatment measure were younger, more frequently men and of white race, more likely to have CAD, dyslipidemia, angina, a history of MI, PCI or within the past 12 months and more likely to be treated with antiplatelet agents. Those not meeting the composite measure were more likely to have private insurance.
Patient Characteristics Independently Associated with Treatment
Patient characteristics associated with treatment rates in multivariable models are presented in Table 2. Independent factors associated with higher treatment rates of ACEI/ARB included PCI within 12 months and dyslipidemia. For BB, history of MI and history of PCI within 12 months were independently associated with higher rates of treatment. Increasing age was associated with a lower rate of treatment for each agent and the composite. Independent factors associated with meeting the optimal combined treatment measure were dyslipidemia and PCI within 12 months.
Table 2.
Patient characteristics associated with prescription rates
| ACEI/ARB | Beta-Blockers | Composite of ACEI/ARB and BB |
|
|---|---|---|---|
| Rate Ratio (95% CI) |
Rate Ratio (95% CI) |
Rate Ratio (95% CI) |
|
| Age: 65 –< 75 | 0.98 (0.96,1.00) | 0.98 (0.97, 0.99) | 0.96 (0.95,0.98) |
| Age: >= 75 | 0.93 (0.90,0.95) | 0.97 (0.95,0.99) | 0.91 (0.88,0.94) |
| Female | 0.97 (0.95–1.00) | 1.01 (0.99–1.02) | 0.99 (0.96–1.01) |
| Insurance: Private | 0.97 (0.93–1.02) | 0.97(0.94–1.01) | 0.97 (0.92–1.03) |
| Insurance: Public | 0.97 (0.93–1.02) | 0.99 (0.95–1.03) | 0.97 (0.92–1.03) |
| A-fib | 0.99 (0.97–1.02) | 1.00 (0.98–1.03) | 1.00 (0.97–1.03) |
| Dyslipidemia | 1.03 (1.01–1.06)* | 1.02 (0.99–1.05) | 1.04 (1.00–1.08) |
| Hypertension | 1.01 (0.98–1.03) | 1.01 (1.00–1.02) | 1.01 (0.98–1.04) |
| PAD | 1.00 (0.97–1.04) | 0.99 (0.97–1.02) | 1.00 (0.97–1.04) |
| Prior stroke | 1.01 (0.98–1.04) | 0.98 (0.94–1.03) | 0.99 (0.95–1.04) |
| Angina | 0.99 (0.96–1.03) | 0.99 (0.97–1.02) | 0.98 (0.95–1.02) |
| MI History | 1.01 (0.98–1.04) | 1.03 (1.01–1.04)* | 1.03 (0.99–1.06) |
| Current Smoker | 0.99 (0.97–1.01) | 0.99 (0.97–1.01) | 0.98 (0.95–1.01) |
| CABG w/in 12 months | 0.96 (0.87–1.06) | 1.01 (0.98–1.05) | 0.95 (0.84–1.06) |
| PCI w/in 12 months | 1.06 (1.03–1.09)* | 1.04 (1.01–1.06)* | 1.08 (1.04–1.13)* |
| Diabetes | 1.00 (0.97–1.03) | 1.02 (1.00–1.03) | 1.02 (0.98–1.05) |
| Practice Median Rate Ratio | 1.11 (1.08–1.18) | 1.08 (1.05–1.15) | 1.17 (1.13–1.26) |
Practice Variation in Treatment Rates
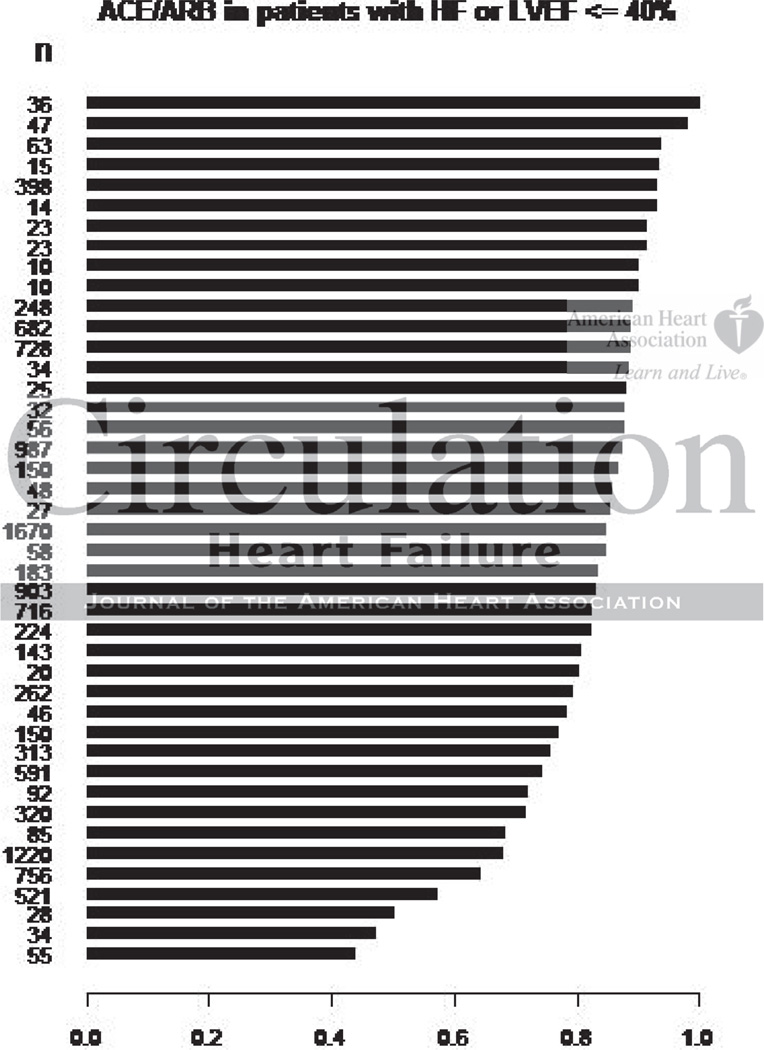
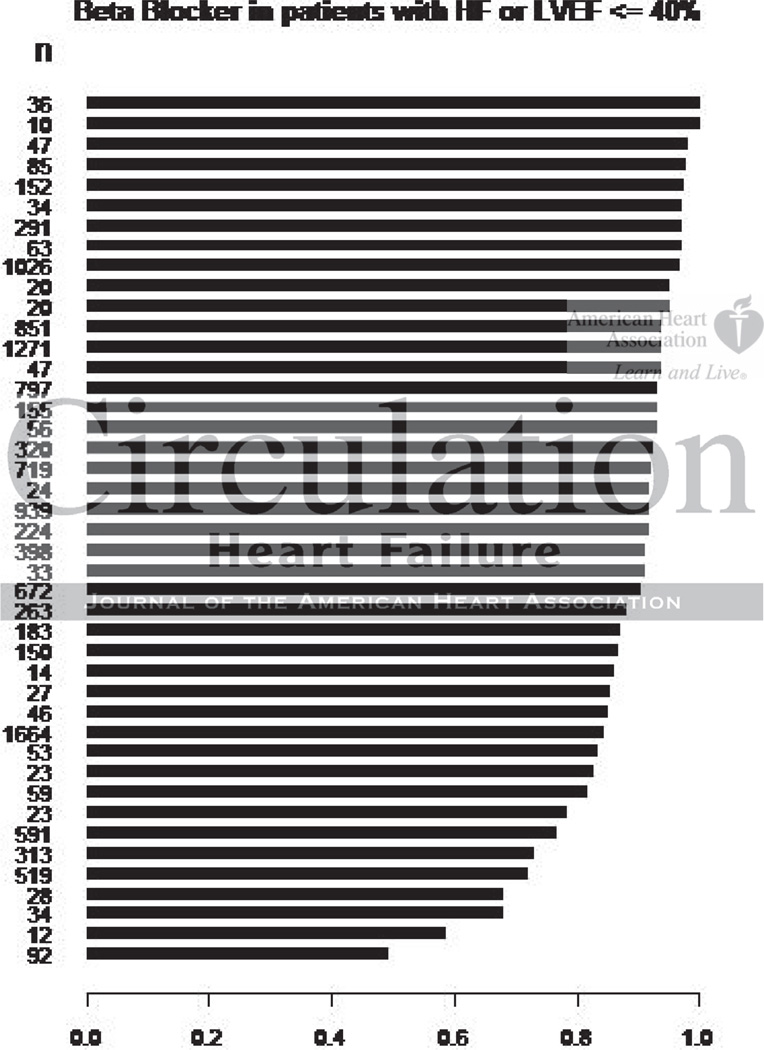
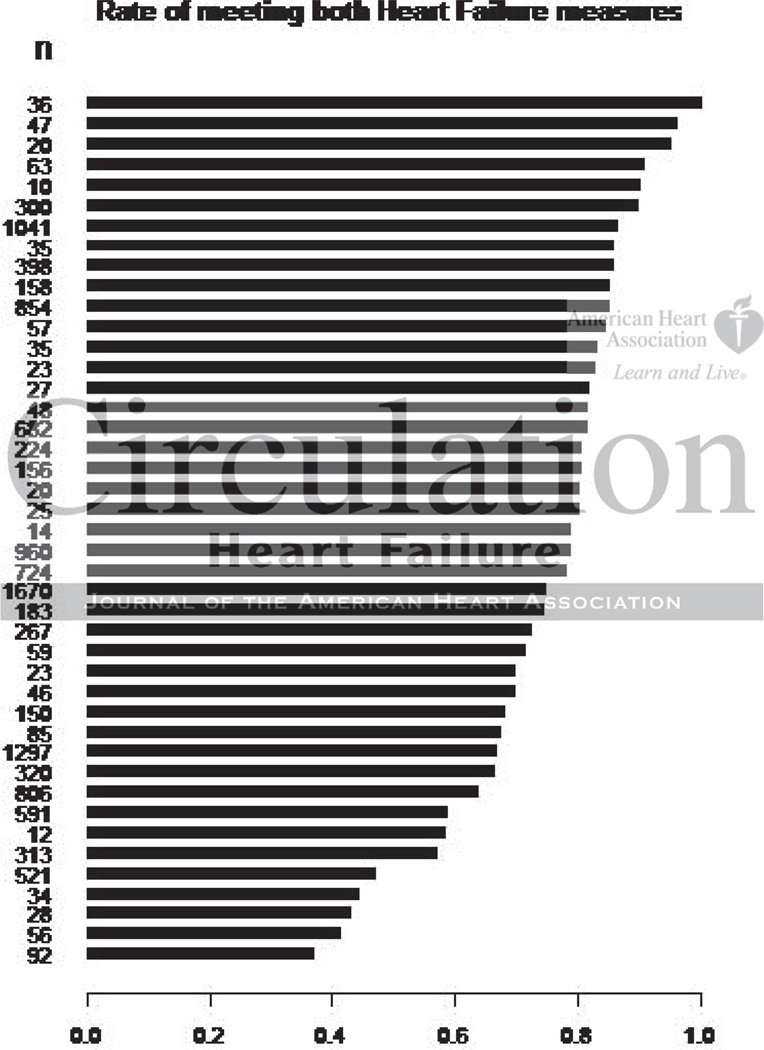
At the practice level, substantial variation in treatment was observed. For ACEI/ARB, treatment rates ranged from 44% to 100% (median of 85%; interquartile range [IQR] 75%–89%). (Figure 1) For BB, practice-level treatment rates ranged from 49%–100% (median of 92%; IQR 83%–95%). (Figure 2) The practice-level rate of meeting the composite ranged from 37%–100% (median of 79%; IQR 66%–85%). (Figure 3) When encounters for the entire year following the index visit were considered, median rates of treatment at the practice level increased slightly (81% to 83% for ACEI/ARB; 87% to 91% for BB).
Figure 1.
Variation in rate of prescription of ACEI/ARB across practices.
Figure 2.
Variation in rate of prescription of BB across practices.
Figure 3.
Variation in composite prescription rate across practices.
After adjusting for differences in patient characteristics, practice-level variation in the treatment rates for ACEI/ARB, BB or optimal combined treatment persisted. The adjusted MRR for practice effect was 1.11 (95% confidence interval [CI] 1.08–1.18) for ACEI/ARB therapy, 1.08 (95% CI 1.05–1.15) for BB therapy and 1.17 (1.13–1.26) for optimal combined treatment. For each therapy as well as the optimal combined therapy measure, the effect size of the MRR was larger than the adjusted OR of any patient-level factor (Table 2), suggesting that the association between practice site and treatment was stronger than that of any individual patient factor.
In secondary analyses, the number of patients with HFREF at a practice was not associated with treatment and did not change the MRR for treatment for ACEI/ARB, BB or the optimal combined treatment measure. Similarly, length of time participating in PINNACLE was not associated with treatment and did not change the MRR for treatment with ACEI/ARB, BB or the optimal combined treatment measure. Paper data reporting was associated with higher treatment rates for all measures, but did not change the MRR for any of the measures. The rate of documented exclusions for ACEI/ARB was not correlated with treatment with ACEACEI/ARB (Spearman weighted correlation 0.13, p=0.40). However, a modest correlation was observed between the rate of documented exclusions for BB and treatment rates (Spearman weighted correlation 0.5, p=<0.001), although the absolute rate of documented exclusions for BB was low and varied little between practices (ranging from 1–5%).
Discussion
The PINNACLE Registry provides contemporary information on the real-world use of guideline-recommended medications for HFREF in the outpatient setting from over 40 cardiology practices across the US. Although rates of ACEI /ARB and BB use among patients with HFREF treated in outpatient cardiology clinics are relatively high, variations in care exist. We observed variation by practice for individual and combined measures of therapy. In all cases, fully-adjusted models suggested that practice was a stronger predictor of treatment than any individual patient characteristic. These findings suggest that efforts to improve the use of evidence-based therapies in the outpatient setting should focus on practice site, in addition to patient factors.
Our findings are consistent with a prior study, IMPROVE HF, which reported similar rates of use of guideline-recommended therapies in eligible patients across a sample of cardiology or multispecialty practices between 2005 and 2007.6 When these data are compared with more contemporary data from PINNACLE, the rate of ACEI/ARB use is not different (80% in IMPROVE HF vs. 79% in PINNACLE), and the rate of BB use is slightly higher (86% in IMPROVE HF vs. 89% in PINNACLE). At the practice level, similar mean practice rates of treatment were observed for ACEI/ARB (80% in IMPROVE HF vs. 81% in PINNACLE) and BB (88% in IMPROVE vs. 87% in PINNACLE). Although average rates of medication prescription are relatively high and may suggest a ceiling effect of these performance measures, observed practice variation indicates that these remain important targets for quality improvement efforts.
A number of practice-level factors may contribute to variation in care. However, IMPROVE HF did not find a significant association between improvement in care and a number of practice-level factors, including geographic location, practice type, number of cardiologists, number of electrophysiologists, affiliation with a hospital or transplant center, presence of a device-based clinic, annual average number of patients treated, number of HF-devoted advanced practice nurse or physician assistant (APN/PA) staff, and the presence or absence of a dedicated HF clinic.7 This suggests that other practice-level factors may be involved, such as differences in guideline familiarity, culture of practice, or implementation of tools and systems, such as those that can be programmed into EHRs, to ensure that recommended care is provided. Further work is needed to understand the characteristics and processes of high-performing practices and to disseminate those processes to all practices to improve the use of guideline-based therapies for HFREF in the outpatient setting.
We considered additional explanations for the observed variability in treatment rates across practices, including differences in the duration of participation in PINNACLE, differences in the number of patients with HFREF in a practice and differential documentation of contraindications. Our analyses did not suggest that differences in case volume or duration of participation within PINNACLE accounted for treatment variation across practices. We did find a modest correlation between documentation of exclusions for and rate of treatment with BB. The rate and variation in documentation of exclusions was low, making the observed correlation less likely to be of clinical significance. However, this finding may indicate that documentation might, in part, explain our findings and suggest that quality improvement efforts should focus on both improving documentation and clinical practice.
The focus of quality improvement for HFREF has largely been at the hospital level, with several national performance improvement programs designed to assess and improve care in the hospital setting.14–16 Policies such as 30-day readmission penalties, while implemented at the hospital level, have brought attention to care provided outside of the hospital. Such policies may stimulate change in the ambulatory setting, particularly among integrated healthcare systems and accountable care organizations. Although much of the care for heart failure occurs in the ambulatory setting, few quality improvement programs have focused on ambulatory care of HFREF. IMPROVE HF demonstrated that a practice-based performance improvement program consisting of clinician education, clinical decision support tools, data collection and benchmarked quality reports resulted in improvement in the overall adherence to performance metrics for heart failure in the ambulatory setting.5 However, we found that in contemporary practice, practice site continues to be an important contributor to variability in treatment. Thus, addressing practice-level factors remains an important opportunity to improve the use of evidence-based heart failure therapies in the outpatient setting.
Several limitations should be considered in the interpretation of this study. First, PINNACLE practices may be highly motivated for quality improvement. Therefore, observed treatment rates may be higher than in practices not participating in PINNACLE. In particular, care in internal medicine and family practice clinics is unknown and may differ substantially from that of the PINNACLE sites. Further, practices participating in PINNACLE were predominantly urban, which may also limit the generalizability of our findings. Second, documentation of contraindications may not be complete or accurate and does not include information on specific adverse reactions or contraindications. However, PINNACLE has data completeness and quality requirements for participation in the registry. Further, to the extent that participating practices depend on the PINNACLE program to report for their pay-for-performance measures, it is in the best interest of the practices to submit complete data. Third, we were unable to explore the role of specific practice-level factors because limited data were available regarding practice characteristics. Finally, we were unable to assess other important aspects of heart failure care (e.g. use of aldosterone antagonists, implantable cardioverter defibrillators). Although these other aspects of care are Class I guideline indications, they are not established consensus performance measures for heart failure care.4
In conclusion, we found significant variation among outpatient practices in prescription of evidence-based therapies for patients with HFREF. This variation was independent of differences in case mix and was greatly influenced by the practice at which patients received care. Thus, efforts to improve the use of evidence-based HFREF therapies in the outpatient setting should target practice-level factors.
Acknowledgments
Dr. Allen serves as a consultant for Amgen, Janssen Scientific Affairs and for the Robert Wood Johnson Foundation. Dr. Masoudi has a contract with the American College of Cardiology Foundation. Dr. Masoudi has research support from NHLBI, AHRQ, and the American College of Cardiology Foundation. Dr. Spertus has grant support from the NIH, the American Heart Association, Genentech, Lilly and EvaHeart. Dr. Spertus serves as a consultant to United Healthcare, St. Jude Medical, Genentech and Amgen.
Sources of Funding
Dr. Allen is supported by a Career Development Grant Award from the NHLBI (5K23HL05896). Dr. Chan is supported by a Career Development Grant Award (K23HL102224) from the NHLBI. Dr. Maddox is supported by a VA Health Services Research and Development Career Development Award. Dr. Peterson is supported by a K08 award (1K08HS019814-01) from AHRQ. Dr. Spertus has a research contract with the American College of Cardiology Foundation to support analyses of the PINNACLE Registry.
Role of Sponsors: None of the funders had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript. The views in this article are those of the authors and do not necessarily reflect the views of the Department of Veterans Affairs.
Footnotes
Disclosures
None of the other authors have any conflicts of interest to disclose.
References
- 1.Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EM, Smith SC, Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult--Summary Article: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): Developed in Collaboration With the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: Endorsed by the Heart Rhythm Society. Circulation. 2005;112:1825–1852. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 2.Fonarow GC, Yancy CW, Heywood JT for the ADHERE Scientific Advisory Committee SGaI. Adherence to Heart Failure Quality-of-Care Indicators in US Hospitals: Analysis of the ADHERE Registry. Arch Intern Med. 2005;165:1469–1477. doi: 10.1001/archinte.165.13.1469. [DOI] [PubMed] [Google Scholar]
- 3.Peterson PN, Rumsfeld JS, Liang L, Hernandez AF, Peterson ED, Fonarow GC, Masoudi FA on behalf of the American Heart Association Get With the Guidelines-Heart Failure Program. Treatment and Risk in Heart Failure: Gaps in Evidence or Quality? Circ Cardiovasc Qual Outcomes. 2010;3:309–315. doi: 10.1161/CIRCOUTCOMES.109.879478. [DOI] [PubMed] [Google Scholar]
- 4.Bonow RO, Ganiats TG, Beam CT, Blake K, Casey DE, Jr, Goodlin SJ, Grady KL, Hundley RF, Jessup M, Lynn TE, Masoudi FA, Nilasena D, Pina IL, Rockswold PD, Sadwin LB, Sikkema JD, Sincak CA, Spertus J, Torcson PJ, Torres E, Williams MV, Wong JB American College of Cardiology Foundation, American Heart Association Task Force on Performance Measures, American Medical Association-Physician Consortium for Performance Improvement. ACCF/AHA/AMA-PCPI 2011 Performance Measures for Adults With Heart Failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures and the American Medical Association-Physician Consortium for Performance Improvement. Circulation. 2012;125:2382–2401. doi: 10.1161/CIR.0b013e3182507bec. [DOI] [PubMed] [Google Scholar]
- 5.Fonarow GC, Albert NM, Curtis AB, Stough WG, Gheorghiade M, Heywood JT, McBride ML, Inge PJ, Mehra MR, O'Connor CM, Reynolds D, Walsh MN, Yancy CW. Improving Evidence-Based Care for Heart Failure in Outpatient Cardiology Practices. Circulation. 2010;122:585–596. doi: 10.1161/CIRCULATIONAHA.109.934471. [DOI] [PubMed] [Google Scholar]
- 6.Fonarow GC, Yancy CW, Albert NM, Curtis AB, Stough WG, Gheorghiade M, Heywood JT, McBride ML, Mehra MR, O'Connor CM, Reynolds D, Walsh MN. Heart Failure Care in the Outpatient Cardiology Practice Setting. Circulation: Heart Failure. 2008;1:98–106. doi: 10.1161/CIRCHEARTFAILURE.108.772228. [DOI] [PubMed] [Google Scholar]
- 7.O'Connor CM, Albert NM, Curtis AB, Gheorghiade M, Heywood JT, McBride ML, Inge PJ, Mehra MR, Reynolds D, Walsh MN, Yancy CW, Fonarow GC. Patient and Practice Factors Associated With Improvement in Use of Guideline-Recommended Therapies for Outpatients With Heart Failure (from the IMPROVE HF Trial) The American Journal of Cardiology. 2011;107:250–258. doi: 10.1016/j.amjcard.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 8.Chan PS, Oetgen WJ, Buchanan D, Mitchell K, Fiocchi FF, Tang F, Jones PG, Breeding T, Thrutchley D, Rumsfeld JS, Spertus JA. Cardiac Performance Measure Compliance in Outpatients: The American College of Cardiology and National Cardiovascular Data Registry's PINNACLE (Practice Innovation And Clinical Excellence) Program. J Am Coll Cardiol. 2010;56:8–14. doi: 10.1016/j.jacc.2010.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan PS, Oetgen WJ, Spertus JA. The Improving Continuous Cardiac Care (IC3) Program and Outpatient Quality Improvement. The American Journal of Medicine. 2010;123:217–219. doi: 10.1016/j.amjmed.2009.09.019. [DOI] [PubMed] [Google Scholar]
- 10.Kahn CN, III, Ault T, Isenstein H, Potetz L, Van GS. Snapshot of hospital quality reporting and pay-for-performance under Medicare. Health Aff. 2006;25:148–162. doi: 10.1377/hlthaff.25.1.148. [DOI] [PubMed] [Google Scholar]
- 11.Larsen K, Petersen JH, Budtz-J++rgensen E, Endahl L. Interpreting Parameters in the Logistic Regression Model with Random Effects. Biometrics. 2000;56:909–914. doi: 10.1111/j.0006-341x.2000.00909.x. [DOI] [PubMed] [Google Scholar]
- 12.Larsen K, Merlo J. Appropriate Assessment of Neighborhood Effects on Individual Health: Integrating Random and Fixed Effects in Multilevel Logistic Regression. Am J Epidemiol. 2005;161:81–88. doi: 10.1093/aje/kwi017. [DOI] [PubMed] [Google Scholar]
- 13.Goldstein H, Browne W, Rasbash J. Partitioning Variation in Multilevel Models. Understanding Statistics. 2002;1:223. [Google Scholar]
- 14.Fonarow GC, Abraham WT, Albert NM, Gattis SW, Gheorghiade M, Greenberg BH, O'Connor CM, Pieper K, Sun JL, Yancy CW, Young JB OPTIMIZE-HF Investigators and Hospitals. Influence of a performance-improvement initiative on quality of care for patients hospitalized with heart failure: results of the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure (OPTIMIZE-HF) Arch Intern Med. 2007;167:1493–1502. doi: 10.1001/archinte.167.14.1493. [DOI] [PubMed] [Google Scholar]
- 15.Fonarow GC, Heywood JT, Heidenreich PA, Lopatin M, Yancy CW ADHERE Scientific Advisory Committee and Investigators. Temporal trends in clinical characteristics, treatments, and outcomes for heart failure hospitalizations, 2002 to 2004: findings from Acute Decompensated Heart Failure National Registry (ADHERE) American Heart Journal. 2007;153:1021–1028. doi: 10.1016/j.ahj.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 16.Piccini JP, Hernandez AF, Dai D, Thomas KL, Lewis WR, Yancy CW, Peterson ED, Fonarow GC for the Get With the Guidelines Steering Committee and Hospitals. Use of Cardiac Resynchronization Therapy in Patients Hospitalized With Heart Failure. Circulation. 2008;118:926–933. doi: 10.1161/CIRCULATIONAHA.108.773838. [DOI] [PubMed] [Google Scholar]