Abstract
Background:
The compartmentalization involved in viewing the mouth separately from the rest of the body must cease. This is because oral health affects general health by causing considerable pain and suffering; and, by changing what people eat and their speech, can bring about a change in their quality of life and well-being. There are several instruments for measuring oral health related quality of life, and, OIDP (Oral Impact on Daily Performance) is one among them.
Aim:
The aim of this study is to assess the OIDP among dental students and to know whether students in different stages of the dental course had any difference in impact on their daily performance.
Materials and Methods:
372 students of Bachelor of Dental Sciences’ (BDS) course at Manipal College of Dental Sciences, Manipal, Karnataka, India, from the first to final year, and interns answered a structured questionnaire recording their demographic characteristics, behavioral characteristics and eight items of OIDP.
Results:
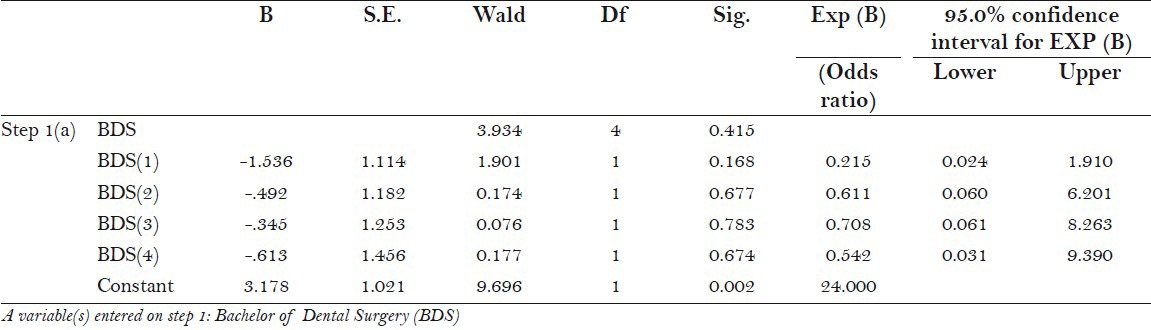
The mean OIDP Additive scores (ADD) and OIDP Simple count scores (SC) scores were 7.02 (sd = 3.3, range 8 - 40) and 2.16 (sd = 1.55, range 0 - 8), repectively. A total of 36.6%, 12.9% and 12.9% of the dental students confirmed difficulties with eating, enjoying contact with other people and carrying out major college work, respectively. Logistic regression analysis revealed that compared with the first BDS dental students, the Odds ratio (OR) for the second, third, fourth year and intern dental students for being without oral impacts, despite reporting poor oral health, were 0.21 (95% CI: 0.24 – 1.9), 0.61 (95% CI: 0.06 – 6.2), 0.70 (95% CI: 0.61 – 8.2) and 0.54 (95% CI: 0.3 – 9.3), respectively.
Conclusion:
The study reported the OIPD among dental students and provided evidence of importance of social and behavioral characteristics in shaping the response by dental students.
Keywords: Dental students, oral health, oral health related quality of life, Oral Impact on Daily Performance, socio – demographic factors
INTRODUCTION
The extension of people's life span and the enhancement of their quality of life are two central goals of Healthy People 2000 initiative. The emphasis on quality of life is consistent with the concept that health is a resource and not simply the absence of disease. Increasingly, quality-of-life assessment is being regarded as an essential component for assessing outcomes of health care, including outcomes for public health programs. Until a decade ago, there was a virtual absence of indices to measure quality of life related to oral health. However, there is now an impressive range of instruments that assess the impact of oral conditions on the well being and the quality of life of an individual.[1] The Oral Impact on Daily Performance (OIDP) scale[2] assesses the impact of oral health on an individual's daily life. This instrument is advantageous for use in population surveys, not only in terms of it being easier to use while measuring individual behaviors rather than feeling states, but also because it is brief. Thus, it is suitable even for surveys where the respondent burden is high, because of its simplicity of usage and ability to produce results quickly. The OIPD scale was designed by Locker in 1988, based on an explicit conceptual framework of the World Health Organization's (WHO) International Classification of Impairments, Disabilities and Handicaps (ICIDH),[3] by introducing certain amendments specific to dentistry.[4]
The ICIDH provides a basis for the empirical exploration of the links between different dimensions or levels of consequence and variables; and, consists of the following key concepts: impairments; functional limitations; pain and discomfort; and, disability and handicap. Impairments refer to the immediate biophysical outcomes of a disease, commonly assessed by clinical indicators.[5] Functional limitations are concerned with functioning of body parts; whereas, pain and discomfort refer to the experiential aspects of oral conditions in terms of symptoms. In addition to dissatisfaction with dental esthetics, they also comprise of the intermediate impacts caused by oral health status. Finally, the ultimate outcomes of disability and handicap refer to any difficulties in performing activities of daily living, and also to broader social disadvantages. The OIDP concentrates only on the third level of measurement and is calculated by multiplying frequency and severity scores of daily performances. As compared to using only the OIDP frequency or severity scores, applications of weighted scores have revealed no significant improvement.[6] Other socio-dental indicators have also been reported to be satisfactory in terms of unweighted instead of weighted scores.[7] For those reasons, the un-weighted or abbreviated version of the OIDP frequency scale was applied in our study.
The practice of dentistry has been widely acknowledged as being associated with high levels of stress. Stressors associated with dentistry include time and scheduling pressures, managing uncooperative patients, commercial issues, and the highly technical and intensive nature of work. The origins of this stress may also lie in the process of dental education. In recent years, the injurious effects of stress experienced by dental students have received much attention. Stress has been shown to manifest as fatigue, tension, dizziness, sleeplessness, tachycardia, gastrointestinal symptoms, irritability, anxiety, and cynicism. In addition to this, a negative association has been reported between stress and academic performance of dental students. Since the perception of stress is frequently influenced by sociocultural factors, the results of studies in one region cannot necessarily be generalized to the others.[8]
The aim of this study was to assess the OIDP among dental students, and to know whether students in different stages of the dental course had any difference in impact on their daily performance.
MATERIALS AND METHODS
Study area and study population
The study population consisted of students from Manipal College of Dental Sciences, Manipal, Karnataka, India. There was a total enrollment of 372 BDS students from the first to final year and interns who were completing their one year of compulsory rotatory internship. All the subjects (female = 40.59%, male = 59.41%, Mean age = 20.91 and Standard Deviation, SD = 2.52) completed a self administered questionnaire in English.
Survey instrument and measures
A structured questionnaire was prepared to record the demographic characteristics such as age, gender, year of study, domiciliary status, religion, parent's education and parent's occupation; oral health related behavior including tooth brushing frequency, dietary habits, alcohol and smoking habits; global oral health indicator; received dental treatment and relevant dental history, and eight items of OIDP. The responses for received dental treatment, global oral health indicator and alcohol intake were dichotomized as 1 = yes and 2 = no. Frequency of cleaning teeth yielding the categories of 1 = once, 2 = twice and 3 = more than twice were obtained and smoking habit was assessed under smoker and non smoker categories. Oral impact of daily performance was obtained by adding scores for eight frequency items. “During the past 6 months how often did you have problems with your mouth and teeth which caused you any difficulties with, 1) eating, 2) speaking and pronouncing clearly, 3) cleaning teeth, 4) sleeping and relaxing, 5) smiling without embarrassment, 6) maintaining emotional state, 7) enjoying contact with other people and 8) carrying out major school work. The scale used was in the range: (0) “never affected”, (1) “less than once a month”, (2) “once or twice a month”, (3) “once or twice a week” (4) “3–4 times a week”, (5) “every or nearly every day”. For analysis, dummy variables were constructed yielding the categories 0 = “never affected” (including the original category 0) and 1 = “affected less than once a month or more often” (including the original categories 1–5). Simple count scores (SC) were created by adding the 8 dummy variables. Additive scores (ADD) were created by adding the 8 OIDP items as assessed originally. Finally, the OIDP SC frequency scores were dichotomised, yielding the categories (0) “no daily performance affected” and (1) “at least one daily performance affected”. Previous work on OIPD[5] has shown the items to have acceptable reliability and validity.
Statistical analysis
Data was analyzed using Statistical Package for the Social Sciences [SPSS (version 11.5)] software. Non-parametric statistics were the primary choice because the OIDP frequency scores were not normally distributed. Chi-square test was used for categorical data analysis. The inter-item correlation coefficients among the 8 OIDP items were calculated. P ≤ 0.05 was considered statistically significant. Cronbach's alpha was used to test for internal consistency and reliability. Logistic regression analysis was done to find the extent of association of OIDP with the BDS years of study.
Ethical approval
Informed consent was obtained from each student before the questionnaire was distributed. Only those students willing to participate were asked to complete the questionnaire. The same was done for the interns posted in their respective departments in the dental school clinics.
RESULTS
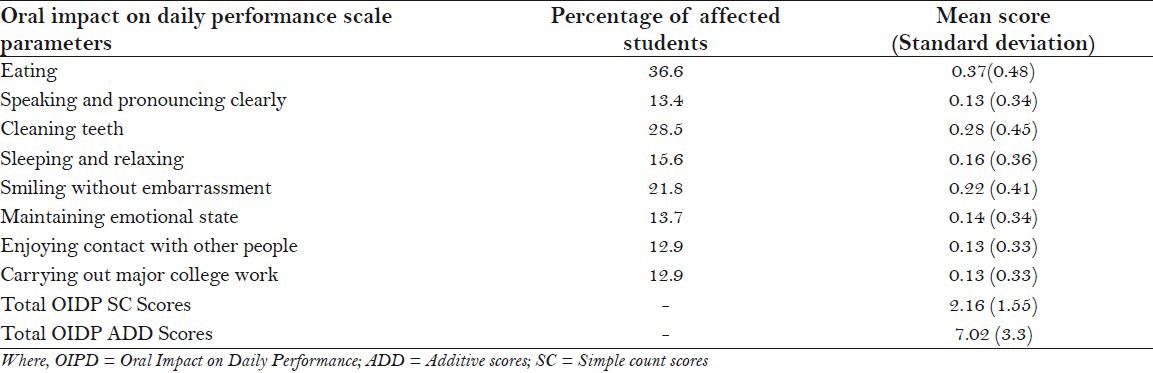
Table 1 shows the percentages of dental students who reported atleast one OIDP by socio – demographic and behavioral characteristics in the total sample. The prevalence of oral impact impacts did not vary significantly by gender, religion (dichotomized as Hindu and non Hindu), parent occupation, BDS year of study, and habit of smoking. Students with graduate parents, mixed diet, habit of alcohol consumption, previous dental treatment history and who were satisfied with oral health, had atleast one oral impact on their daily performance. The mean OIDP ADD and OIDP SC scores were 7.02 (sd = 3.3, range 8 - 40) and 2.16 (sd = 1.55, range 0 - 8), respectively [Table 2]. A total of 36.6%, 12.9% and 12.9% of the dental students confirmed difficulties with eating, enjoying contact with other people and carrying out major college work, respectively. The second most prevalent impact was difficulty with cleaning teeth (28.5%), followed by difficulties with smiling without embarrassment (21.8%). The floor effect was substantial in that a total of 45.7% had OIDP scores of zero using both the ADD and the SC scoring method. A total of 54.3% of the students experienced at least one impact during the six months preceding the survey.
Table 1.
Percentage of the dental students participating in the study, who reported at least one oral impact on daily performance by socio – demographic and behavioral characteristics
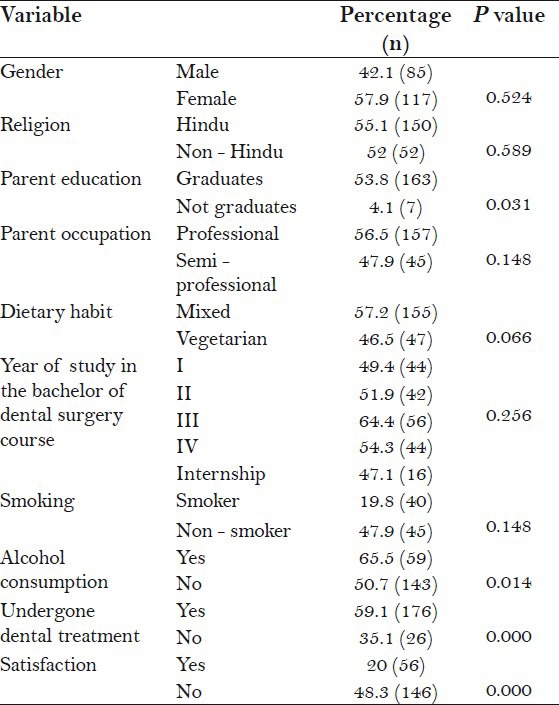
Table 2.
Percentage distribution (percentage of students affected less than once a month or more) and mean frequency scores (standard deviation) for eight oral impact on daily performance additive scores and oral impact on daily performance simple count scores
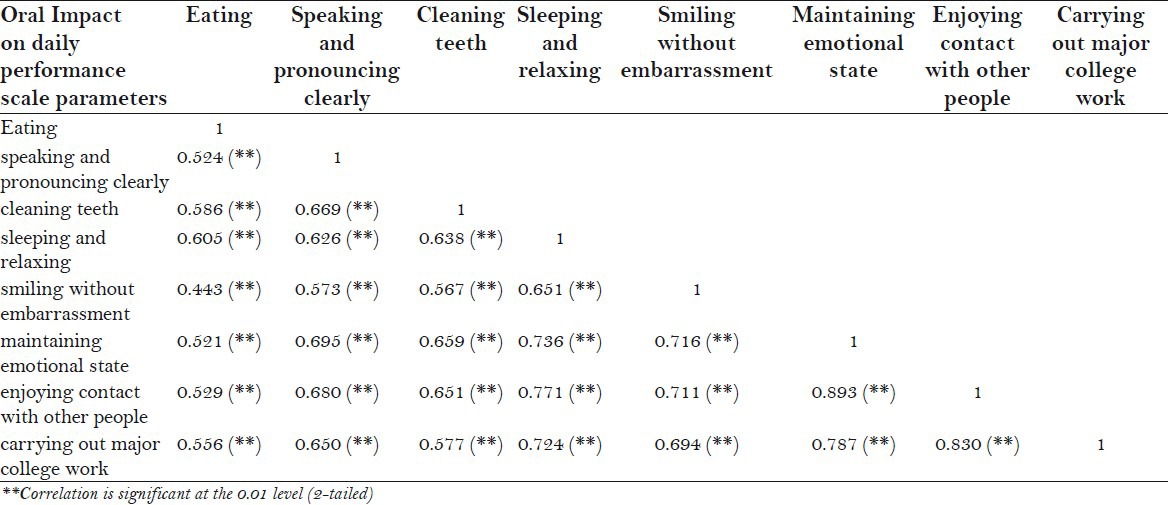
The inter item correlation coefficients among the 8 OIDP items ranged from 0.443 (between eating and smiling without embarrassment) to 0.893 (between enjoying contact with other people and maintaining emotional state) [Table 3]. No correlation was negative indicating homogeneity among the items and no correlation was high enough for any item to be redundant. The corrected item total correlation ranged from 0.443 – 0.893, being above the minimum recommended level of 0.20 for inclusion of items in a scale, and meeting the stringent criterion of item convergent validity of > 0.40.
Table 3.
Correlation matrix for oral impact on daily performance frequency scores (1-8)
Discordance between Oral Impact on Daily Performance scores and reported satisfaction with oral health across different years of Bachelor of Dental Sciences Study course
To explore the dependency of BDS year on oral impact, and the degree of discordance between two the indicators further, OIDP SC and reported satisfaction with oral health were cross tabulated. Among internees, 2.9% perceived no oral impact, despite reporting dissatisfaction with their oral health. The corresponding figure among first year dental students was 1.1%. In contrast, 38.2% of the internees had at least one oral impact, whilst they nonetheless reported satisfaction with their oral health. This disagreement was common, 50.5% and 42% in the third and final year students, respectively [Figure 1]. Logistic regression analysis revealed that compared with the first BDS dental students, the OR for being without oral impacts, despite reporting poor oral health, were 0.21 (95% CI: 0.24 - 1.9), 0.61 (95% CI: 0.06 – 6.2), 0.70 (95% CI: 0.61 – 8.2) and 0.54 (95% CI: 0.3 – 9.3) in the second, third, fourth year and intern dental students, respectively [Table 4]. However, the result was not statistically significant.
Figure 1.
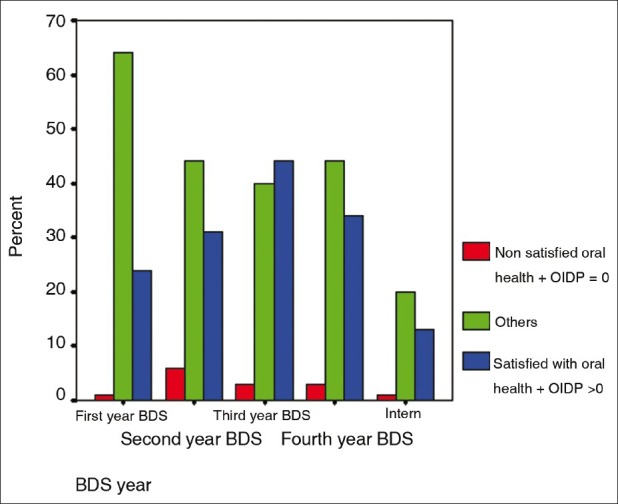
Percentage of dental students who reported not satisfied with their oral health and atleast one oral impact on daily performance in various years of study of bachelor of dental surgery course
Table 4.
Odds ratio and 95% confidence interval for respondents’ of oral impact on daily performance scale and oral impact on daily performance simple count scores (without oral impact) by the year of study of the bachelor of dental surgery course compared with the scores of the first year students of the bachelor of dental surgery course
DISCUSSION
Cross – cultural adaptation of socio – dental indicators requires rigorous translation and validation to make the adopted instrument culturally relevant for the local population. The participants of the present study were familiar with English as a second language, thus a rigorous translation and back translation was deemed necessary. To ensure interpretability and cultural equivalence, the OIDP was pre – tested among the students and supervised by a group of competent teaching faculty. The process concluded with a minor rephrasing of the question about major work and social role, which was modified into “carrying out major college work”.
A total of 54.3 percent of the participants reported experiencing an oral impact that affected their daily life in the past six months. The eight impact prevalence rates ranged from 12.9 percent to 36.6 percent, and floor effect of 45.7 percent was reported. This was relatively low as compared to another study done on a cross- sectional study population of 1146 adolescents in Uganda,[5] where the eight impact prevalence rates ranged from 30 percent to 40 percent. and floor effect of 32 percent was calculated. This may be predominantly attributed to the fact that our study population was of dental students and also that the chances of desirability bias cannot be ruled out. This result was consistent with the results reported in previous OIDP surveys, where difficulty with eating and enjoying food, and with cleaning teeth, were the impacts most frequently reported. The total impact prevalence rate was comparable with, but lesser than 51 percent, which was observed in a[9] Tanzanian study, using a similar methodology and the English version of the the questionnaire. It was also below the 70 percent prevalence observed in another population of western people with high dental disease levels, and in a low – oral disease Thai population.[2]
In the present study, those who reported satisfaction with their oral health, but complained of oral impact, were the largest discordant group across various years of BDS study. This result is in accordance with that of the study performed by Astrom et al. in 2006[10] where the OIDP was calculated for the Norwegian population. The only difference in the two studies is that, in the former study on the Norwegian population, oral health (good oral health/ bad oral health) and atleast one oral impact on daily performance was considered with the age groups, instead of the BDS year of study, as in our survey. The OIDP frequency scores were applicable across age and gender, showed satisfactory reliability and were subject to low levels of non response. The OIDP frequency score showed item to scale correlations that are similar to those obtained in previous application;[11] and, the internal consistency reliability in terms of a Cronbach's alpha of 0.85 indicates excellent psychometric properties if the recommended level of 0.70 is used.[12] Previous applications of the OIDP scale to various populations have yielded internal consistency values ranging from 0.67 to 0.85.[2,9,11]
The study was limited owing to the self report method employed. The possibility that socially desired and undesired acts have been, respectively, over – and under estimated cannot be overlooked. The present study suggested that an abbreviated OIDP inventory is applicable for use among dental students and the oral impact on daily performance is relatively low in them. However, the oral impact differences between the various BDS years of study were not confirmed. The item level characteristics and the reliability add to our confidence that the scale measures a construct comparable to the original. Moreover, the present study indicated that the social and behavioral context is important in shaping the response of the dental students. This study constituted the first step to highlight the limits of focusing on normative needs; and, suggests the incorporation of oral quality of life measures into the oral health care services for the budding dentists in India.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–90. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 2.Adulyanon S, Vourapukjaru J, Sheiham A. Oral impacts affecting daily performance in a low dental disease Thai population. Community Dent Oral Epidemiol. 1996;24:385–9. doi: 10.1111/j.1600-0528.1996.tb00884.x. [DOI] [PubMed] [Google Scholar]
- 3.Badley EM. The ICIDH: format, application in different settings and distinction between disability and handicap. Int Disabil Stud. 1987;9:122–5. doi: 10.3109/03790798709166338. [DOI] [PubMed] [Google Scholar]
- 4.Locker D. Measuring oral health: A conceptual framework. Community Dent Health. 1988;5:3–18. [PubMed] [Google Scholar]
- 5.Astrom AN, Okullo I. Validity and reliability of the Oral Impacts on Daily Performance (OIDP) frequency scale: A cross – sectional study of adolescents in Uganda. BMC Oral Health. 2003;3:5. doi: 10.1186/1472-6831-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adulyanon S, Sheiham A. Oral Impacts on Daily Performances. In: Slade GD, editor. Measuring oral health and quality of life. Chapel Hill: University of North Carolinas; 1997. [Google Scholar]
- 7.Allen PF, Locker D. Do item weights matter? An assessment using the oral health impact profile. Community Dent Health. 1997;14:133–8. [PubMed] [Google Scholar]
- 8.Acharya S. Factors affecting stress among Indian dental students. J Dent Educ. 2003;67:1140–8. [PubMed] [Google Scholar]
- 9.Masalu J, Åstrøm AN. Social and behavioral correlates of oral quality of life studied among university students in Tanzania. Acta Odontol Scand. 2002;60:353–9. doi: 10.1080/000163502762667388. [DOI] [PubMed] [Google Scholar]
- 10.Astrøm AN, Haugejorden O, Skaret E, Trovik TA, Klock KS. Oral Impacts on Daily Performance in Norwegian adults: The influence of age, number of missing teeth, and socio-demographic factors. Eur J Oral Sci. 2006;114:115–21. doi: 10.1111/j.1600-0722.2006.00336.x. [DOI] [PubMed] [Google Scholar]
- 11.Tsakos G, Marcenes W, Sheiham A. Evaluation of a modified version of the index of oral impacts on Daily performances (OIDP) in elderly populations in two European countries. Gerodontology. 2001;18:121–30. doi: 10.1111/j.1741-2358.2001.00121.x. [DOI] [PubMed] [Google Scholar]
- 12.Mc Dowell I, Newell C. New York: Oxford University Press; 1996. Measuring Health. A guide to rating scales and questionnaires. [Google Scholar]


