Abstract
Context:
Survey.
Aims:
To evaluate dental awareness and periodontal health status in different socioeconomic groups in the population of Sundernagar, Himachal Pradesh, India.
Settings and Design:
Cross-sectional study.
Malerials and Methods:
This cross-sectional study was conducted in 300 patients with different socioeconomic status who visited Himachal Dental College, Sundernagar, and Dental OPD of the Civil Hospital, Sundernagar. Mouth mirror, CPI probe, and illuminated light source were used for examination. Periodontal health status was recorded using CPI index. Information about their lifestyle, education level, and socioeconomic status was recorded using a questionnaire and correlated with the periodontal status.
Statistical Analysis Used:
Chi-square test.
Results:
Majority of the subjects used toothbrush and toothpaste to clean their teeth once daily. Lower socioeconomic groups exhibited higher CPI scores characterized by bleeding gums and calculus deposition. The differences were statistically significant across various social strata (P < 0.01).
Conclusions:
The utilization of the questionnaire on dental awareness facilitates the inclusion of multiple aspects of patient information. The study revealed that oral hygiene awareness and periodontal condition were significantly associated with socioeconomic status. The socioeconomic status and oral hygiene practices were significantly associated with CPI (P < 0.01).
Keywords: Community periodontal index, dental awareness, periodontal disease, socioeconomic status
INTRODUCTION
The term inequality has a moral and ethical dimension. It refers to differences which are unnecessary and avoidable but, in addition, are also considered unfair and unjust.[1] Regarding oral health, the reasons of disparities are complex. There are differences caused by biological factors (such as aging), which are normal and inevitable in a balanced society. But there are also inequalities which can be avoided and are unacceptable in the modern society, being caused mainly by the socioeconomic differences.[2] The concept of socioeconomic inequalities in oral health can be defined as differences in the prevalence or incidence of oral health problems between higher and lower socioeconomic status.[3] Studies had shown that over the last decade, the differences in the oral health status between the individuals with a high socioeconomic status and those with a low socioeconomic status had markedly increased.[4]
Oral care, as part of general health self-care, comprises wide spectrum of activities ranging from care, prevention, and diagnosis to seeking professional care. Oral self-care practices have been proved to be an effective preventive measure at individual level for maintaining good oral health as a part of general health.[5] To improve the oral health of population, the WHO has set the promotion of self-care as one of the goals for the year 2020.[6]
Furthermore, periodontitis has been implicated as an emerging risk factor for a number of major systemic diseases or conditions, including cardiovascular disease, stroke, and diabetes, as well as for pre-term, low–birth-weight infants.[7,8,9] Prevention of and early intervention into periodontal disease is critical, and oral hygiene education is central to all stages of treatment. In addition to professional care, successful management of periodontal disease depends on the capacity of patient's oral self-care.[10,11] A change in patient's attitude and behavior is often desirable when periodontitis is treated. The information gathered relative to a patient's values and beliefs may be a useful guide in designing effective oral health care interventions.[12]
Presently, very few studies exist showing the effect of general education, lifestyle, and socioeconomic position on the prevalence of periodontal disease. Hence, in the present study, an attempt was made to investigate the effect of lifestyle, education, and socioeconomic status on the periodontal health of adult population in Sundernagar.
MATERIALS AND METHODS
A cross-sectional study design was used. Subjects were recruited from the patients who visited Himachal Dental College, Sundernagar, and Dental OPD of the civil hospital, Sundernagar, for initial assessment and treatment of periodontitis. Mouth mirror, CPI probe, and illuminated light source were used for examination. The sample size consisted of 300 dental patients in the age range 25-55 years. Patients were categorized according to the differences in socioeconomic status.
Inclusion criteria
Systemically healthy individuals aged 25–55 years
Presence of more than 15 teeth
Exclusion criteria
Patients with history of systemic disease
Pregnancy and lactation
Use of tobacco in any form
Undergone oral prophylaxis during the past 6 months
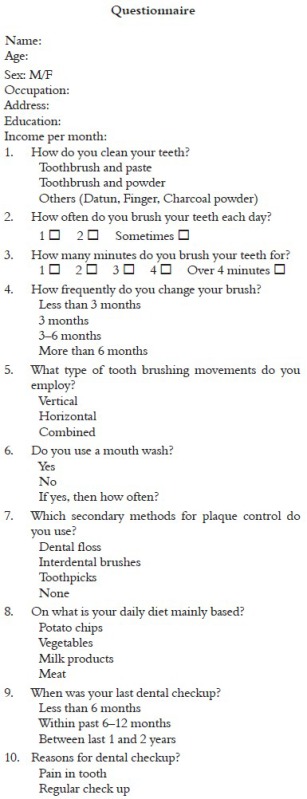
A questionnaire was administered by the examiner. From this questionnaire, information was obtained regarding dental awareness and socioeconomic status.
The periodontal examination was conducted using mouth mirror and CPI probe and the CPI score was recorded.[13]
Codes and criteria of CPI index:
Code 0 = No periodontal disease (healthy periodontium)
Code 1 = Bleeding observed during or after probing
Code 2 = Calculus or other plaque-retentive factors either seen or felt during probing
Code 3 = Pathological pocket 4–5 mm in depth. Gingival margin situated on black band of the probe
Code 4 = Pathological pocket 6 mm or more in depth. Black band of the probe not visible
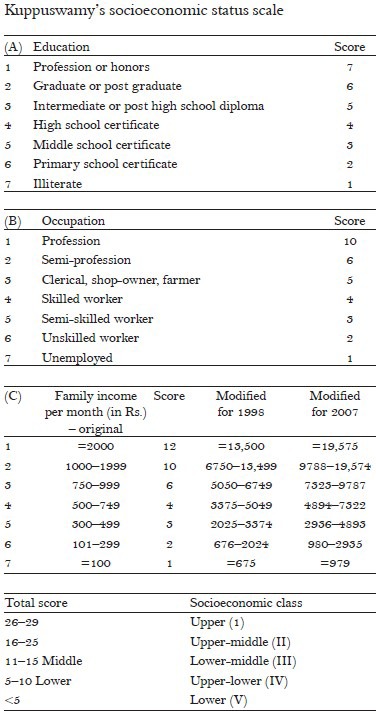
Modified Kuppuswamy's socioeconomic scale14 was utilized in this study for the stratification of the patients. The stratification was done under five classes comprising upper, upper-middle, lower-middle, upper-lower, and lower.
RESULTS
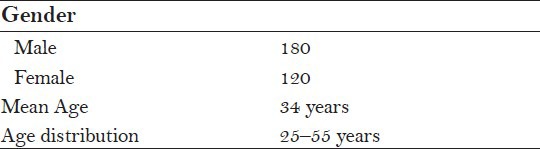
Out of 300 subjects (Males = 180, Females = 120). Number of cases in each socioeconomic group from class I to class V. The demographic characteristics of the subjects at baseline are shown in Table 1.
Table 1.
Demographic characteristics of the subjects at baseline (total N = 300)
On evaluating the dental awareness, it was revealed that both oral hygiene aids and frequency of cleaning teeth show significant difference in all socioeconomic classes. Majority of the subjects in all socioeconomic classes preferred to use toothbrush and paste as compared to other aids. It is reported that upper (100.0%) class used toothbrush and paste more as compared to upper-middle (93.33%), lower-middle (82.6%), upper-lower (67.14%), and lower (74.5%) classes. Only 15.7% and 16.36% in the upper-lower and lower socioeconomic classes used other oral hygiene aids such as datun (neem stick) and charcoal powder. Majority of them brushed once daily; around 30% among the upper socioeconomic class brushed their teeth twice daily (P < 0.01) [Table 2].
Table 2.
Distribution of subjects in relation to socioeconomic status, oral hygiene aids used, and frequency of cleaning teeth
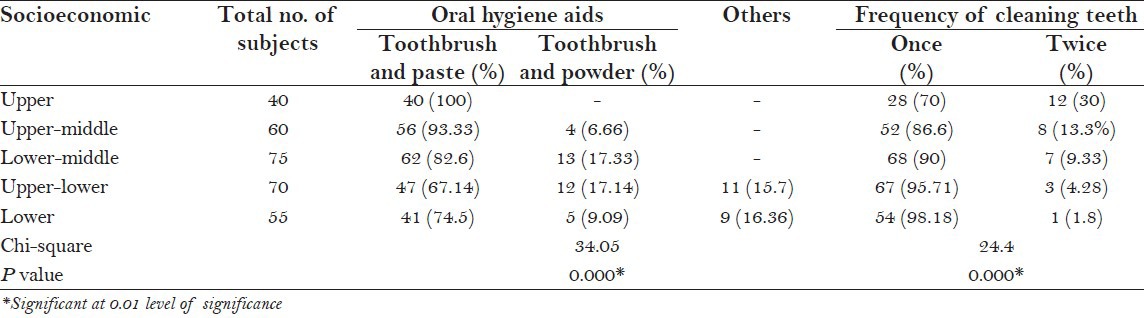
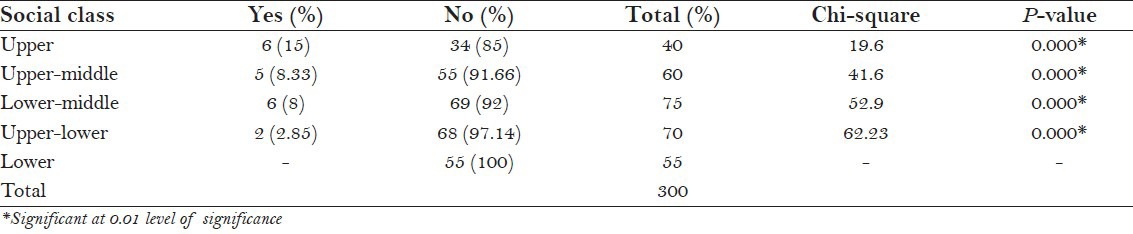
Table 3 indicates that the socioeconomic status is associated with the regular attendance at dental clinics. There was a statistically significant difference between subjects from different socioeconomic classes (P < 0.01).
Table 3.
Regular visit to the dentist during the last 6–12 months according to socioeconomic status
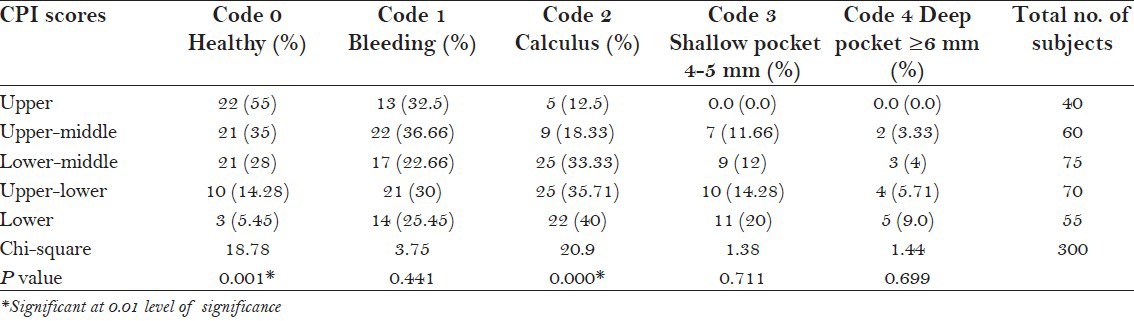
According to CPI, Code 0 (χ2 = 18.7, P < 0.01) and Code 2 (χ2 = 20.9, P < 0.01) were statistically significant at P < 0.01 level. Code 1 (χ2 = 3.75, P > 0.05), Code 3 (χ2 = 1.38, P > 0.05), and Code 4 (χ2 = 1.44, P > 0.05) were statistically nonsignificant across the various social strata. It is reported that Code 0 was more in upper (55.0%) and upper-middle (35.5%) classes, while Code 2 was more in lower-middle (33.33%), upper-lower (35.71%), and lower (40.0%) socioeconomic classes [Table 4].
Table 4.
Relation between CPI codes and the socioeconomic status
DISCUSSION
Socioeconomic factors have been identified as predisposing factors in the development of periodontal disease and other oral diseases. People from lower educational, occupational, and income groups go to dentist for preventive care less than those of higher status do. Changing this pattern is not simply a matter of making services free. It requires both the change of dental attitudes and habits of low-income groups and finding new methods of organizing and paying for both preventive and restorative dental cares.
The variation in the oral hygiene practices between upper and lower socioeconomic groups may be attributed to lack of oral hygiene education in lower socioeconomic groups which is reflected in their oral hygiene maintenance.
Our study showed a positive association between higher socioeconomic groups and better periodontal status. This is in accordance with the report of Neuman et al.[14] who identified a lower occupational status limiting the use of dental services.
Our study demonstrated higher prevalence rate among low socioeconomic group children than in middle and higher socioeconomic group children. These results agree with the studies of Russell,[15] Nikias et al.,[16] and Waerhaug,[17] which showed that prevalence of periodontal disease was inversely related to increasing family income.
Dental visit is still not considered a positive dental behavior; at present, it only depends on treatment needs. Thus, people from the lower income group fail to make prophylactic visits to a dentist, thus giving them poorer dental health behavior.[18] A few shortcomings of this study were the self-reporting of all variables and the sample of 300 may not truly represent trends in the community on the whole. So, a larger, more representative sample would have to be studied for more direct correlations.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Whitehead M. WHO Regional Office for Europe; 2000. The concepts and principles of equity in health. [Google Scholar]
- 2.US Department of Health and Human Services; 2000. Healthy people 2010. [PubMed] [Google Scholar]
- 3.Locker D, Ford J. Using area-based measures of socioeconomic status in dental health services research. J Public Health Dent. 1996;56:69–75. doi: 10.1111/j.1752-7325.1996.tb02399.x. [DOI] [PubMed] [Google Scholar]
- 4.USA: The National Institute of Dental and Craniofacial Research; 2002. Oral health U.S. [Google Scholar]
- 5.Axelsson P, Albander JM, Rams TE. Prevention and control of periodontal diseases in developing and industrialized nations. Periodontal. 2002;29:235–46. doi: 10.1034/j.1600-0757.2002.290112.x. [DOI] [PubMed] [Google Scholar]
- 6.Hobdell M, Petersen PE, Clarkson J, Johnson N. Global goals for oral health 2020. Int Dent J. 2003;53:285–8. doi: 10.1111/j.1875-595x.2003.tb00761.x. [DOI] [PubMed] [Google Scholar]
- 7.Offenbacher S. Periodontal diseases: Pathogenesis. Ann Periodontol. 1996;1:821–78. doi: 10.1902/annals.1996.1.1.821. [DOI] [PubMed] [Google Scholar]
- 8.Page RC. The pathology of periodontal diseases may affect systemic diseases: Inversion of a paradigm. Ann Periodontol. 1998;3:108–20. doi: 10.1902/annals.1998.3.1.108. [DOI] [PubMed] [Google Scholar]
- 9.Rose LF, Genco RJ, Cohen DW, Mealey BL, editors. St. Louis: BC Decker; 2000. Periodontal medicine. [Google Scholar]
- 10.Löe H. Oral hygiene in the prevention of caries and periodontal disease. Int Dent J. 2000;50:129–39. doi: 10.1111/j.1875-595x.2000.tb00553.x. [DOI] [PubMed] [Google Scholar]
- 11.Axelsson P, Nyström B, Lindhe J. The long-term effect of a plaque control program on tooth mortality, caries and periodontal disease in adults. Results after 30 years of maintenance. J Clin Periodontol. 2004;31:749–57. doi: 10.1111/j.1600-051X.2004.00563.x. [DOI] [PubMed] [Google Scholar]
- 12.Vick VC, Harfst S. The oral risk assessment and early intervention system - A clinician's tool for integrating the bio/psycho/social risk into oral disease interventions. Compend Contin Educ Dent Suppl. 2000;30:57–64. [PubMed] [Google Scholar]
- 13.The Indian Journal of Pediatrics. 2007:74. [Google Scholar]
- 14.Newman JF, Gift HC. Regular pattern of preventive dental services: A measure of access. Soc Sci Med. 1992;35:997–1001. doi: 10.1016/0277-9536(92)90239-m. [DOI] [PubMed] [Google Scholar]
- 15.Russell AL. A social factor associated with severity of periodontal disease. J Dent Res. 1957;36:922–6. doi: 10.1177/00220345570360061701. [DOI] [PubMed] [Google Scholar]
- 16.Nikias M, Fink R, Sollecito W. Oral health status in relation to socioeconomic and ethnic characteristics of urban adult in the USA. Community Dent Oral Epidemiol. 1977;5:200–6. doi: 10.1111/j.1600-0528.1977.tb01641.x. [DOI] [PubMed] [Google Scholar]
- 17.Waerhaug J. Prevalence of periodontal disease in Ceylon. Association with age, sex, oral hygiene, socio-economic factors, vitamin deficiencies, malnutrition, betel and tobacco consumption and ethnic group. Final report. Acta Odontol Scand. 1967;25:205–31. doi: 10.3109/00016356709028749. [DOI] [PubMed] [Google Scholar]
- 18.Sander AE, Slade GD, Turell G, John Spencer A, Marcenes W. The shape of the socioeconomic oral health gradient: Implications for theoretical explanations. Community Dent Oral Epidemiol. 2006;34:310–9. doi: 10.1111/j.1600-0528.2006.00286.x. [DOI] [PubMed] [Google Scholar]


