Abstract
Introduction:
Plaque accumulation and oral microorganisms are the main predisposing factors to various orodental infections and targeting these, therefore, can prove to be an effective way of combating these diseases. Herbal extracts have been of particular interest these days owing to various side effects associated with conventional modes of treatment.
Aims and Objectives:
The present study was conducted to compare the efficacy of a commercially available homeopathic mouthwash with chlorhexidine on plaque status, gingival status, and salivary Streptococcus mutans count.
Materials and Methods:
Total sample of 55 children, aged 8-14 years, were randomly divided into two groups. Group A (35) and Group B (20) were given 10 mL of test mouthwash “Freshol” and chlorhexidine respectively during phases 1 and 3 of the clinical trial which was of 10 days each. Phase 2 of 14 days in between was the washout period during which no mouthwash was given.
Result:
Freshol was found to be better than chlorhexidine in reducing the salivary mutans streptococci count and equieffective to chlorhexidine in altering plaque and gingival scores.
Conclusion:
Herbal alternatives can prove to be an effective and safe alternative to conventional modes of treatment.
Keywords: Chlorhexidine, gingival status, herbal mouthwash, plaque status, Streptococcus mutans
INTRODUCTION
With the exponential advancement in the field of dentistry, various preventive measures have emerged targeting the causative factors of the oral diseases.[1] Plaque accumulation is one such factor which predisposes the individual to both dental caries and periodontal disease.[2,3,4] Salivary microfloras like Streptococcus mutans and other predisposing factors lay an important role in the initiation and progression of dental diseases such as dental caries.[5,6] Chemotherapeutic and antimicrobial agents aiming at these predisposing factors, therefore play, a significant role in prevention of these oral diseases and have a dramatic impact on improving the oral health of the individual.[7]
Among the plethora of oral hygiene products available, chlorhexidine has been the mouthwash of choice owing to its dramatic therapeutic effect, but its various side effects like taste alteration, supragingival calculus formation, and desquamation of oral mucosa have restricted its usage in pediatric age group.[4,8] Moreover, it also causes extrinsic staining by attaching to the polyphenolic and tannin group of beverages like tea and coffee. Alternative agents based on herbal extracts are therefore of particular interest.
Various herbal extracts like chamomile, ocimum, and echinacea are known to provide therapeutic benefits in the oral cavity when used topically. German chamomile according to Pourabbas et al.,[4] and Pujar and Makandar[9] retard biofilm formation and thereby prevent gingival inflammation. Agarwal et al.,[5] Prakash and Gupta,[10] and Ahonkhai et al.,[11] have found ocimum to have antimicrobial effect on various oral pathogens like S. mutans. Other beneficial herbs include echinacea which is immunostimulator, antimicrobial, and anti-inflammatory.[12,13,14]
Therefore, in this study, attempt has been made to clinically evaluate the synergistic effect of these herbal extracts in a commercially available herbal mouthwash Freshol as shown in Figure 1 (staphysagria, chamomilla, echinacea, plantago, ocimum, and cistus) on plaque accumulation, gingival health, and salivary S. mutans count.
Figure 1.
Test mouthwash
MATERIALS AND METHODS
A double-blind study was carried out on 55 healthy children between 8 and 14 years by the department of pedodontics and preventive dentistry after obtaining written consent and clearance from institutional ethical committee.
The entire sample size of 55 were randomly divided into Group A (35 subjects) who were given homeopathic mouthwash Freshol (Father Muller Charitable Institution, Mangalore, Karnataka, India) and Group B (20 subjects) who were given chlorhexidine and served as control.
Subjects with good general health, a minimum of 12 gradable teeth, agreement to delay any elective dental treatment including oral prophylaxis, and agreement to comply with the study visits were included in the study. Exclusion criteria involved subjects with relevant medical condition, history of early-onset periodontitis, acute necrotizing ulcerative gingivitis, gross oral pathology, history of steroid or antimicrobial therapy in last 3 months and those developing severe gingival inflammation during the study.[15]
The experimental mouthwash (Freshol) was prepared by mixing staphysagria 3×, chamomilla 3×, echinacea 3×, plantago 3×, ocimum 3×, and cistus 3× in distilled water.
The entire clinical trial was divided into three phases. Phase 1 and phase 3 were the clinical trial periods of 10 days each during which children were asked to rinse twice daily with 10 mL of the given mouthwash along with their routine mechanical plaque control measures. Phase 2 was the washout period of 2 weeks during which they were refrained from these mouthwashes but continued their other routine oral hygiene measures.
Plaque index given by Sillness and Loe and gingival index given by Loe was used to assess the plaque accumulation and gingivitis.[16,17] To assess the effect of mouthwashes on the caries susceptibility mutans streptococci in the saliva were counted and compared. For this 0.5 mL of the unstimulated saliva was collected in closed containers and incubated within 30 min to avoid use of any transportation media. Culture used was mitis salivarius bacitracin which is a selective media of S. mutans.[18] The inoculated culture plates were incubated at 37°C for 72 h and the microbial count was done. Baseline data were collected at the onset of phase 1 and the final value collected at the end of phase 3 were compared.
Statistical analysis
Intragroup comparison of both plaque and gingival indices were done using paired t-test, whereas intergroup comparison of these indices were done using Tukey's HSD test. Microbial evaluation of the salivary Streptococcus was done using Wilcoxon signed test for both intergroup and intragroup comparison.
RESULTS
Results of all the three parameters plaque status, gingival status, and salivary S. mutans count have been depicted in Table 1, 2, and 3, respectively.
Table 1.
Baseline and final scores of plaque status
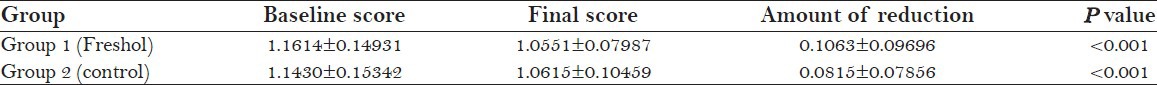
Table 2.
Baseline and final gingival scores of the test and control
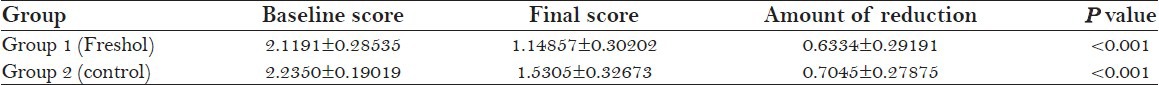
Table 3.
Baseline and final microbial count of the test and control
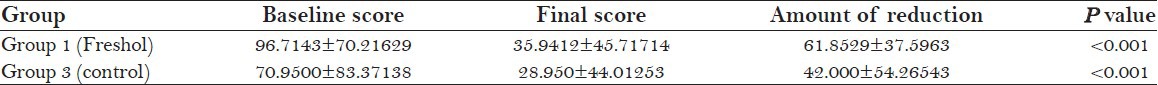
Table 1 shows statistically significant reduction in the plaque scores before and after the clinical trial in both the groups according to paired t-test (P < 0.001). Intergroup comparison, however, did not show any significant difference between the test mouthwash and control on plaque reduction according to Fisher's exact test (P = 0.639). Similarly, gingival inflammation was also significantly reduced by both the mouthwashes according to paired t-test (P < 0.001) and no statistically significant difference between the two according to Fisher's exact test (P = 0.019) as seen in Table 2.
On the contrary, the test mouthwash Freshol was found to be more effective in reducing salivary S. mutans count than the control mouthwash chlorhexidine according to Fisher's exact test (P < 0.001) as seen in Table 3. However, according to Wilcoxon signed rank sum test, intragroup comparison showed statistically significant improvement between baseline and final microbial count (P < 0.001).
DISCUSSION
The present study was designed to determine the efficacy of an herbal mouthrinse Freshol with chlorhexidine on plaque accumulation, gingival health, and mutans streptococci.
All the subjects taken for the study were residing in the same ashram, thereby eliminating the bias occurring due to different eating patterns. Each trial period was restricted to 10 days to prevent tooth staining associated with prolonged usage of chlorhexidine.
Results of this study have shown that the test mouthwash Freshol had better antimicrobial effect on salivary S. mutans than chlorhexidine and its effect on plaque control and gingival health was at par with the gold standard of chlorhexidine.
The superior antistreptococcal effect seen in the test mouthwash is due to the presence of potent antimicrobial herbs like echinacea and ocimum which accelerates granulation and regeneration of the tissue due to the presence of methyl ester of salicylic acid.[19,20] The active metabolites of these extracts like carvone and cineole impart antiplaque effect by stimulating immune response and retarding biofilm formation.[21,22] Chamomile and echinacea on the contrary inhibits hyaluronidase and interferes with the arachadonic acid pathway thereby imparting anti-inflammatory effect to the mouthwash which improves the gingival health.[23,24,25] Apart from these, Freshol is a nonalchoholic, with no-added sugar, no artificial preservatives and colors, and reported side effects.
The results of this study is in conjunction with that of Pourabbas et al.,[4] who also found significant reduction in plaque scores with the herbal mouthwash with chamomile extracts. Other supporting studies include those done by Mullaly et al.,[3] Pannuti et al.,[26] and George et al.,[27] also found the antiplaque effect of herbal-based dentifrice (with similar extracts) comparable to the standard ones. The antimicrobial effect of ocimum was also supported by the in vitro study done by Agarwal et al.,[5] who found significant inhibition zones associated with various concentration of ocimum.
Grossman et al.,[28] and Moran et al.,[29] on the contrary could not relate to this study as they found chlorhexidine to have better effect on plaque control than extracts of chamomile. Similarly, Dalirsani et al.,[19] could not relate to this study, as they found chlorhexidine to have better antimicrobial effect than chamomile when studied against.
CONCLUSION
This study, therefore, suggest that herbal alternatives like Freshol can prove to be an effective or better alternative to chlorhexidine in improving the oral health of the child with minimal side effects. Further scope lies in the long-term evaluation of the advantages and side effects off such herbal extracts.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Carounanidy U, Satyanarayan R, Velmurugan A. Use of an aqueous extract of Terminalia chebula as an anticaries agent: A clinical study. Indian J Dent Res. 2007;18:152–6. doi: 10.4103/0970-9290.35823. [DOI] [PubMed] [Google Scholar]
- 2.Rasooli I, Shayegh S, Astaneh S. The effects of Mentha spicata and Eucalyptus camaldulensis essential oils on dental biofilm. Int J Dent Hyg. 2009;7:196–203. doi: 10.1111/j.1601-5037.2009.00389.x. [DOI] [PubMed] [Google Scholar]
- 3.Mullaly BH, James JA, Coulter WA, Linden GJ. The efficacy of an herbal-based toothpaste on the control of plaque and gingivitis. J Clin Periodontol. 1995;22:686–9. doi: 10.1111/j.1600-051x.1995.tb00827.x. [DOI] [PubMed] [Google Scholar]
- 4.Pourabbas R, Delazar A, Chitsaz MT. The effect of german chamomile mouthwash on dental plaque and gingival inflammation. Int J Pharm Res. 2005;2:105–9. [Google Scholar]
- 5.Agarwal P, Nagesh L, Murlikrishnan Evaluation of the antibacterial activity of various concentrations of tulsi (Ocimum sanctum) extract against Streptococcus mutans: An in vitro study. Indian J Dent Res. 2010;21:357–9. doi: 10.4103/0970-9290.70800. [DOI] [PubMed] [Google Scholar]
- 6.Vyas YK, Bhatnagar M, Sharma K. In vitro evaluation of antibacterial activity of an herbal dentrifice against Streptococcus mutans and Lactobacillus acidophilus. Indian J Dent Res. 2008;19:26–8. doi: 10.4103/0970-9290.38928. [DOI] [PubMed] [Google Scholar]
- 7.Allaker RP, Douglas CW. Novel anti-microbial therapies for dental plaque-realted disease. Int J Antimicrob Agents. 2009;33:8–13. doi: 10.1016/j.ijantimicag.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 8.ELey BM. Antibacterial agents in the control of supragingival plaque :A review. Br Dent J. 1999;186:286–96. doi: 10.1038/sj.bdj.4800090. [DOI] [PubMed] [Google Scholar]
- 9.Pujar M, Makandar S. Herbal usage in endodontics-a review. Int J Contemp Dent. 2011;2:34–7. [Google Scholar]
- 10.Prakash P, Gupta N. Therapeutic uses of Ocimum sanctum Linn (Tulsi) with a note on eugenol and its pharmacological actions: A short review. Indian J Physiol Pharmacol. 2005;49:125–31. [PubMed] [Google Scholar]
- 11.Ahonkhai I, Ba A, Edogun O, Mu U. Antibacterial activities of the volatile oils of Ocimum bacilicum L. and Ocimum gratissimum L. (Lamiaceae) against some aerobic dental isolates. Pak J Pharm Sci. 2009;22:405–9. [PubMed] [Google Scholar]
- 12.Mistrikova I, Vaverkova S. Echinacea-chemical composition, immunostimulatory activities and uses. Thaiszia J Bot. 2006;16:11–26. [Google Scholar]
- 13.Melchart D, Linde K, Worku F, Bauer R, Wagner H. Immunomodulation with echinacea: A systematic review of controlled clinical trials. Phytomedicine. 1994;1:245–54. doi: 10.1016/S0944-7113(11)80072-3. [DOI] [PubMed] [Google Scholar]
- 14.Barnes J, Anderson LA, Philipson JD. 2nd ed. London: Pharmaceutical Press; 2000. Herbal Medicines. A Guide for Healthcare Professionals; p. 384. [Google Scholar]
- 15.Jayaprakash K, Veeresha KL, Hiremath SS. A comparative study of two mouthrinses on plaque and gingivitis in school children in the age group of 13 - 16 years in Bangalore city. J Indian Soc Pedod Prev Dent. 2007;25:126–9. doi: 10.4103/0970-4388.36562. [DOI] [PubMed] [Google Scholar]
- 16.Sillness J, Loe H. Periodontal disease in pregnancy ii. correlation between oral hygine and periodontal condition. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 17.Loe H. The Gingival Index, the Plaque Index and the Retention Index System. J Periodontol. 1967;38:610–6. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 18.Mourughan K, Suryakanth MP. Evaluation of an alum-containing mouthrinse for inhibition of salivary streptococcus mutans levels in children: A controlled clinical trial. J Indian Soc Pedod Prev Dent. 2004;22:100–5. [PubMed] [Google Scholar]
- 19.Dalirsani Z, Aghazadeh, Adibpour M, Amirchaghmaghi, Pakfetrat A. In vitro comparison of the antibacterial activity of ten herbal extracts against Streptococcus mutans with chlorhexidine. J Appl Sci. 2011;11:878–82. [Google Scholar]
- 20.Blumenthal M, Hall T, Goldberg A, Kunz T, Dinda K, Brinkman J, et al. Austin: American Botanical Council; 2003. The ABC clinical guide to herbs; pp. 51–60. [Google Scholar]
- 21.Cowan MM. Plant products as antimicrobial agents. Clin Microbiol Rev. 1999;12:564–82. doi: 10.1128/cmr.12.4.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McKay DL, Blumberg JB. A Review of the bioactivity and potential health benefits of peppermint tea (Mentha piperita L) Phytother Res. 2006;20:619–33. doi: 10.1002/ptr.1936. [DOI] [PubMed] [Google Scholar]
- 23.Pistorius A, Willerhausen B, Steinmeier EM, Kriesler M. Efficacy of subgingival irrigation using herbal extracts on gingival inflammation. J Periodontol. 2003;74:616–22. doi: 10.1902/jop.2003.74.5.616. [DOI] [PubMed] [Google Scholar]
- 24.Groppo FC, Ramacciato JC, Simoes RP, Florio FM, Sartoratto A. Antibacterial activity of garlic, tea tree oil, and chlorhexidine against oral microorganisms. Int Dent J. 2002;52:433–7. doi: 10.1111/j.1875-595x.2002.tb00638.x. [DOI] [PubMed] [Google Scholar]
- 25.Lee SS, Zhang W, Li Y. The antimicrobial potential of 14 natural herbal dentifrices: Results of an in vitro diffusion method study. J Am Dent Assoc. 2004;135:1133–41. doi: 10.14219/jada.archive.2004.0372. [DOI] [PubMed] [Google Scholar]
- 26.Pannuti CM, Mattos JP, Ranoya PN, Jesus AM, Lotufo RF, Romito GA. Clinical effect of a herbal dentifrice on the control of plaque and gingivitis: A double-blind study. Pesqui Odontol Bras. 2003;17:314–8. doi: 10.1590/s1517-74912003000400004. [DOI] [PubMed] [Google Scholar]
- 27.George J, Hegde S, Rajesh KS, Kumar A. The efficacy of a herbal-based toothpaste in the control of plaque and gingivitis: A clinic-biochemical study. Indian J Dent Res. 2009;20:480–2. doi: 10.4103/0970-9290.59460. [DOI] [PubMed] [Google Scholar]
- 28.Grossman E, Meckel AH, Isaacs RL, Ferretti GA, Sturzenberger OP, Bollmer BW, et al. A clinical comparison of antibacterial mouthrinses: Effects of chlorhexidine, phenolics, and sanguinarine on dental plaque and gingivitis. J Periodontol. 1989;60:435–40. doi: 10.1902/jop.1989.60.8.435. [DOI] [PubMed] [Google Scholar]
- 29.Moran J, Addy M, Roberts S. A comparison of natural product, triclosan and chlorhexidine mouthrinses on 4-day plaque regrowth. J Clin Periodontol. 1992;19:578–82. doi: 10.1111/j.1600-051x.1992.tb00686.x. [DOI] [PubMed] [Google Scholar]


