Abstract
This article provides information on the origin of tobacco and its subsequent spread throughout the world. In the era of the migration of communities, tobacco use gradually gained access and subsequently migrated along with the migrants, establishing in different locations. Probably at that time people were unaware of the health hazards and were using tobacco in treating certain ailments. Much has been known and written about tobacco in the context of oral and general health hazards but little has been explored and is known to many about where from and how this plant, which is now used in various forms, and speading widely. In what form, where, and how it had been served in religious rituals and considered for treatment or remedy of certain ailments in those days could not certainly be known. In the 21st century, people are considering hazardous tobacco as beneficial for their teeth, good for concentration of mind, and something which keeps them engaged. Even many professionals, though knowing the deleterious effects, are still using tobacco and gutkha in one or the other form. This article has been designed to revive the awareness for health hazards of tobacco and similar products. A pilot project questionnaire survey comprising this subject involving the educated mass has already been started and will be produced after analysis of data in part II of this paper.
Keywords: Bidee, gutkha, naswar, paan, shisha, tobacco
INTRODUCTION
For ages, tobacco has been popular and its use is significantly increasing in spite of alarming health hazards. However, so far a lot has been known about its disadvantages, but still tobacco is grown, developed, advertised, marketed, and sold to earn a big chunk of the financial cake. It is one of the great sources of revenue for the government as excise duty.
Many research works in different countries have emphasized potential detrimental effects of its use on almost all systems of living beings, in whatever form it is used. Many times articles are published in the newspapers, to develop awareness of its effects. Print and electronic media are playing a dual role by helping in promoting and popularizing tobacco / gutkha and similar products and contrarily printing and showing the health hazards.
The literature suggests that approximately 70% of alcoholics are heavy smokers compared with 10% of the general population. Likewise, smokers are 1.3 times more likely to consume alcohol compared with nonsmokers.
Where from, in what form, and how these leaves of the noxious plant gained popularity and made the mankind addictive is to be known. Although much has been known by now but knowing the history of tobacco is also necessary.
HISTORY
Tobacco is derived from the leaves of the genus Nicotiana, a plant from the night-shade family, indigenous to North and South America.
Archeological studies suggest the use of tobacco in around first century BC, when Maya people of Central America used tobacco leaves for smoking, in sacred and religious ceremonies. It then later started spreading as far as high up to the Mississippi Valley with the Maya community migrating from down south of America, between 470 and 630 AD. Gradually, it was then adopted by neighboring and native tribes.
Native American “Shamans” developed tobacco use for religious rites. Simultaneously, people practicing medicine also started using tobacco in different forms to cure certain illnesses such as asthma, earaches, bowel problems, fever, sore eyes, depression, insect bites, burns, etc.[1]
By the time Columbus and his successors documented tobacco in other countries, the natives started useing tobacco in pipes, cigars, and snuff. Subsequently, Portuguese and Spanish sailors helped to spread different forms of tobacco to be used, around the world.
Today, tobacco is used in various forms in different parts of the world. Tobacco in many countries is sometimes adopted as a cash crop by the farmers and government treasuries (excise, taxes, etc.), and is also grown for local consumption.
The major tobacco-growing and consuming countries are China, USA, the Former Soviet States, India, and Brazil. In South and Southeast Asia, it is incorporated into existing traditional customs, in the form of betel quid (paan) chewing.
The tobacco industry provides thousands of jobs, and is also a major source of income for the advertising industries, printed and electronic media, government (for revnew and as a source of foreign currency).
Modes of use
There is a wide range of use of tobacco in different countries.
The smoking form of tobacco, since its introduction in South Asian countries, has been used in several forms, like hukka (water pipe), chilam (clay pipe), cigarettes, rolled tobacco in the form of bidees, Chchuta (reverse smoking), etc., whereas the nonsmoking or chewable tobacco is in the form of snuff/naswar (roasted and finely powdered for inhalation), mawa, qiwam, gutkha, kheni (mixture of dry raw tobacco with lime), zarda, betel quid with tobacco, paan-masala, etc.. In Indonesia, tobacco is mixed with clove and dipped in the oral cavity.
Paan acquired significant popularity among the male population of the central and western India in contrast to female of these locations. Contrary are the findings in Bangladesh, with educated or uneducated females consuming more paan preferably with tobacco. According to a survey report, tobacco-consuming females in Bangladesh believe that this helps them in concentrating more on their work. The survey also states that a large population believes that paan strengthens their teeth and eliminates bad breath.
Influencing factors
Tobacco use has multifactor influences. Despite increasing public awareness of risks associated with tobacco use and education programs to discourage its use, cigarettes and alcohol are both considered as significant risk factors for a multitude of health consequences from the long-term use of either of these two.
There is a direct or an indirect influence of culture on tobacco use as some individuals having an inherited factor later become nicotine dependent. Boys see their grandfathers or fathers smoking, so they think it is part of being a man.[2] Smoking is seen as part of being a man and a sign of his male authority. In any society at large, it is not considered good for women to smoke but fine for men. The man is the boss and smoking is a symbol of that authority, and if a woman smokes,it is seen as a threat to the man and his manhood. Also, if a woman smokes, she is assumed to be indecent both morally and sexually.[3]
Smoking and paan chewing can be part of a social event, confirming hospitality and binding friendships.[4] Hookah, chilam (clay pipe with tobacco), and shisha are used in a social setting specifically in the rural culture. To attract youngsters, now a days some restaurants have started providing shisha clubs. Havana cigar is smoked in celebrations and is recognized as a status symbol.
Promotion and popularity
In India, gutkha users claim that it relieves tension, helps in concentration, combats bad breath, and keeps one engaged.[5,6] Before a decade, cinema and print media were the chief source of advertisement of and marketing cigarettes. An amendment in the law has imposed a ban on the advertisement of any smoking form of tobacco in the public places and through print media this message is published for the community to know. Still in Indian cinema, male stars are shown smoking in a stylish way, which leaves an imprint on the psychology of the younger generation who later try adopt and replicate that.
On satellite TV and cinema screen, the Indian cinema “heartthrobs” are shown advertising, propagating, promoting, and popularizing the different brands of gutkha products. Gutkha is a branded product of many companies, and sold in colorful, attractive sachets in India. Hence the younger generations consider and take it as modern, acceptable, and fashionable, and sussequently become addicted to it. In UK, the mothers of Asian origin blame the media of these countries for introducing children to gutkha.
It impacts on the vulnerable minds of the school children,as in a study many children were reported as spending their pocket money on gutkha.[7]
Some companies popularize tobacco as the dental care product by incorporating it in toothpastes or toothpowders. Although law has been amended barring the use of tobacco in dental care products, still some manufacturers use tobacco as an ingredient in the toothpowders without mentioning ingredients on the packaging.[8]
Chaudhury, in a questionnaire survey, has reported that among 13–15 year olds, 6–68% of respondents use tobacco products.[9]
In USA, split tobacco was popularized by sports icons. [10]
Health hazards
There are 2550 known compounds in tobacco and more than 4000 compounds in tobacco smoke.
Primary tobacco biohazardous compounds include at least 43 carcinogens, such as nicotine and nitrosamines, and alpha-emitting radionuclides such as polonium 210.
Tobacco smoke contains carbon monoxide, thiocyanate, herbicide, fungicide and pesticide residues, tars, and many other substances which promote diseases and impair the body's defense mechanism and functions. Toxic substances in the tobacco smoke affect virtually every viable cell type.
First and foremost, adverse effect of smoking is immunosuppressive effect on the host, and hence adversely affecting host-parasite interactions.
The consumption of tobacco, whether inhaled, sniffed, sucked, or chewed, has evident harmful effects on health, and is addictive too. Scientists unequivocally evidenced that tobacco consumers suffer from three Ds: death, disease, and disability.[11]
Different systems of our body are interrelated and they influence the use of any such product which is likely to cause health hazards affects many such body functions.
Its active ingredients, tar, nicotine, and nitrosamine, are potentially associated with oral cancer worldwide.[12,13]
In the developed countries, smoking has been associated with over 85% deaths of all cancer deaths in men. It is estimated that 40–45% of all cancers and 90–95% of all lung cancers have an association with smoking. [14] Many other diseases, such as chronic pulmonary obstructive disease (COPD) are implicated to cause death in 75% of the people between the age of 35 and 70 years. Many clinical study have established that pipe smoking has been associated with lip cancer.
While smokeless tobacco habits are endemic, oral cancer can account for more than one-third of all cancers.[15] The prevalence of smoking in teenagers of India is increasing ranging from 19.7% to 34.5%.
ORAL AND SYSTEMIC EFFECTS OF SMOKING
Despite of increasing public awareness of risks associated with tobacco use and education programs to discourage its use, cigarettes and alcohol both are considered significant risk factors for a multitude of health consequences from the long-term and excessive use of either of these two.
It is ubiquitously accepted that smoking is a significant risk factor for cardiovascular diseases, COPD, and some forms of cancers. The use of any such product which is likely to cause health hazards, adversely affects functions of many systems.
Smokers have a characteristic change in color of exposed mucosal surfaces which is primarily due to melanin deposition on the basal cell layer of the mucosa. The relationship of a smoker's melanosis (dark-brown foci) and inflammatory changes that result from heat, smoke, and inhalation with the absorption of exogenous pigments has not been determined. Tobacco-associated white keratosis patches are commonly found in smokers [Figure 1]. Chronic smokers may also develop nicotine stomatitis (smoker's palate). Verrucous carcinoma of Ackerman is a variant of squamous cell carcinoma and has an association with smokeless tobacco.
Figure 1.

White keratosis of the buccal and tongue mucosa in a tobacco gutkha user
It has long been established that recurrent aphthous ulcer is a disease, almost exclusively, of nonsmokers. And this is one of the consistent findings. Recurrent aphthous ulcers may start if smoking is abandoned, although reasons are unclear.
Influence on periodontium
Arno et al. examined 1016 individuals for gingivitis and found a significant correlation between tobacco consumption and gingivitis when hygiene and age were kept constant.[16] Ismail et al. reviewed data from National Health and Nutrition Examination Survey and found that smokers had higher periodontal, debris, calculus, and oral hygiene index scores than non-smokers.[17]
Smokers have greater susceptibility to periodontitis, and paradoxically less to gingivitis; the explanation given for this paradoxical clinical behavior is that probably smoking interferes with the inflammatory and immune response by activating endothelial and inflammatory cells to induce cytokines’ secretion. The deleterious effects of smoking on the periodontium include alteration in periodontal tissue vasculature, direct alternative effect on bacterial microflora, and the inhibitory effect on immunoglobulin levels and antibody responses to plaque bacteria. Nicotine is a vasoconstrictor, although its effects on gingivae have been proven to be difficult to measure.
It has been documented that tobacco components can have deleterious effects on various neutrophil functions (impaired chemotaxis/phagocytosis or both). Polymorphonuclear leukocytes motility, chemotaxis, and phagocytosis are significantly reduced in smokers. Thus this important first line of defense against subgingival bacteria is compromised in smokers. Antibody production is altered, specially opsonizing IgG2 and immune-regulatory T-cell subset ratio.
In this manner, both innate and acquired immune mechanisms are compromised in current smokers, allowing periodontal bacteria to escape host clearance and establish themselves as subgingival inhabitants.
Cigarette smoking increases bacterial adhesion to epithelial cells and has a differential effect on bacterial colonization, favoring growth of Gram-negative bacteria.
Alternation in the subgingival environment, such as decreased oxygen tension, allows, in turn, the overgrowth of an essentially anaerobic flora and overgrowth of opportunistic pathogenic microbial species. Periodontal pocket oxygen tension partial oxygen pressure (PO2) was significantly less in smokers compared with nonsmokers and was not influenced by gingival oxygen sufficiency.
Smokers are 2.6-6 times more likely to exhibit periodontal destruction than nonsmokers. Exposure to tobacco smoke is associated with an increased risk of adult periodontitis and increased disease severity in smokers compared to nonsmokers.[18] It has been suggested in many studies that smokers have greater clinical attachment loss (CAL).
Attachment loss severity was increased by 0.5% by smoking 1 cigarette / day, while smoking up to 10-20 cigarettes increased the clinical attachment loss by 5-10%. A positive correlation has been established between serum levels of the nicotine metabolite cotinine and severity of CAL, probing depth, and alveolar crest height, because of which cigarette smoking significantly increases the risk for tooth loss by 70%.
Smokers appear to have a depressed number of helper lymphocytes (Th) which are important for B-cell function and antibody production. This has been manifested by decreased levels of salivary antibodies IgA and serum IgG. In smokers, a diminished serum IgG2 level and an impaired IgG2 response have been hypothesized to increase the risk of periodontitis.
Serum IgG antibodies to Prevotella intermedia and Fusobacterium nucleatum have also been reported to be reduced in smokers.
Pindborg noted that 98% of acute necrotizing ulcerative gingivitis (ANUG) patients studied were smokers. The effect of smoking appears to be complex than a mere reflection of patient stress.[19] Clarke et al.. have demonstrated that the intra-arterial infusion of epinephrine and nicotine in rabbits resulted in reduced gingival blood flow rates in spite of increased systemic perfusion pressure.[20]
Smokers who underwent periodontal surgery with either modified Widman flap or mucoperiosteal flap reflection had significantly less reduction in the pocket depth and gain in clinical attachment levels compared with nonsmokers. Root coverage following free gingival graft procedures is reportedly diminished by heavy cigarette smoking. Following regenerative procedures, the clinical attachment gain was les in smokers. Miller has reported a 100% correlation between failure to obtain root coverage and heavy smoking (more than 10 cigarettes/day). Heavy smokers who refrained from smoking during the first 2 weeks of healing had results comparable to nonsmokers.[21]
Cigarette smokers have also been associated with a reduced healing response, after guided tissue regeneration (GTR) therapy in deep infrabony defects. Nicotine and carbon monoxide in tobacco smoke negatively influence wound healing.
An 80% failure rate in treatment of furcation defects using regenerative therapy has been seen in smokers. Nicotine may inhibit fibroblast-fibronectin and collagen production and increase the fibroblast collagenase activity.
Nicotine can also suppress the proliferation of cultured osteoblasts while stimulating the osteoblast alkaline phosphatase activity.
Tobacco components may also modify the production of cytokines or inflammatory mediators which play a role in periodontal tissue destruction.
Nicotine has been shown to increase the release of interleukin-6 by cultured murine osteoblasts. Smokers also have an increased crevicular fluid tumor necrosis factor-alpha (TNF- α) level.
Implant success rates are reduced in smokers. Smokers are 2.6 times more likely to have an implant failure between the time of implant uncovering and the time of restorative loading. A greater failure rate of implant in smokers has been seen in maxillary anterior teeth. Smoking may influence post-implant surgery healing and the long-term health of the peri-implant tissue. Many clinicians have reported smoking as an absolute risk factor in the selection of implant patients.
The risk of subgingival infection with Bacteroides forsythus in current smokers was 2.3 times that of former smokers or nonsmokers. The proportion of subjects positive for Actinobacillus actinomycetemcomitans, Porphyromonas gingivalis, and Bacteroid forsythss were higher among smokers. Observational studies also report a greater level of plaque, calculus, and oral debris in smokers. This conclusion dominated for nearly two decades of clinical practice.
Cigarette smoking was also associated with increased levels of TNF- α in the crevicular fluid compared with non-smokers. The neutrophil elastase activity and levels of prostaglandin E2 (PGE2) and Matrix meatalloproteinase-8 (MMP8) were raised in smokers.
Nicotine, in addition, up-regulates LPS-mediated monocyte secretion of PGE2 and IL-1B. Free oxygen radicals from neutrophils are increased in smokers. Levels of metallothionine, a free-radical scavenger, are increased in the gingival tissue of smokers. Therefore, smoking appears to favor a pathogenic subgingival flora.
Nicotine has divergent effects on IL-1 and PGE2 secretion, depending upon the cell type and whether or not the bacterial components are present. Such alterations in the host response may affect the reparative and regenerative potential of the periodontium in tobacco users.
From the contemporary studies, a general pattern has emerged:
Smokers have greater clinical attachment and alveolar bone loss.
Increased number of deep pockets and calculus formation.
Variable levels of plaque and inflammation.
A previous history of smoking does not appear to be deleterious to the response to periodontal therapy. It has been observed that occasionally, aphthae start when smoking is given up
Although bias is toward decreased signs of clinical inflammation [Figure 2].
Figure 2.
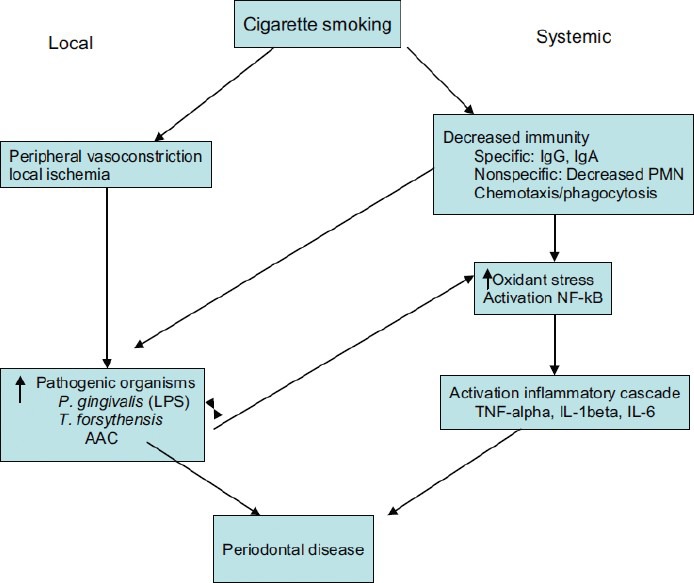
Cigarette smoking - Local and Systemic
CONCLUSION AND COMMENTS
The association of tobacco and its products with several reversible and irreversible oral and systemic diseases and its manifestations have been ubiquitously established.
The adaptation of tobacco by either sex certainly has a familial or cultural impact.
Much has been done to produce, publicize, and popularize tobacco. In contrast negligible efforts are seen to discourage the practice of tobacco use, by the government, and NGOs.
In many countries,the health departments, trusts, and NGOs run voluntary services for smoking cessation at centers with various hospital services. Counseling to give up smoking is done by demonstrating the potential health hazards due to tobacco. Alcohol and tobacco are frequently used together and scientific research supports the popular observation that at large “smokers drink and drinkers smoke.”
Smoking has been identified as one of the major predictive variables for response in periodontal therapy. Studies on non-surgical therapy have shown less probing depth reduction and less attachment gain in smokers as compared to non-smokers. Similar results with less gain in bone height were found in patients’ undergone surgery.
Smoking has been considered as a significant risk factor in implant patients.
Wound healing is delayed in smokers as compared to nonsmokers.
Several studies suggest that smokers show a low response to maintenance therapy compared with non-smokers.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Goodman J. Abingdon: Routledge; 1994. Tobacco in history: The Cultures of dependence. [Google Scholar]
- 2.Bush J, White M, Kai J, Rankin J, Bhopal R. Understanding influences on smoking in Bangladesh and Pakistani adults: Community based, qualitative study. Br Med J. 2003;326:962–8. doi: 10.1136/bmj.326.7396.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Doyal N, Farren C, Naidoo J, Tilson J. London: HEA Helios Project; 1992. Smoking prevention for minority ethnic groups: A resource pack. [Google Scholar]
- 4.Qureshi B. Dordrecht: Kluwer: Academic Publishers; 1989. Transcultural Medicine. [Google Scholar]
- 5.Chadda R, Sengupta S. Tobacco use by Indian adolescents. Tob Induc Dis. 2002;1:111–9. doi: 10.1186/1617-9625-1-2-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anwar S, Williams SA, Scott-Smith J, Sage H, Baweja S, Singal M, et al. A comparison of attitudes and practices of gutkha users and non users in Chitrakoot, India. A Pilot. Prim Dent Care. 2005;12:5–10. doi: 10.1308/1355761052894176. [DOI] [PubMed] [Google Scholar]
- 7.Williams S, Malik A, Chowdhury S, Chauhan S. Socio-cultural aspects of areca nut use. Addict Biol. 2002;7:147–54. doi: 10.1080/135562101200100147. [DOI] [PubMed] [Google Scholar]
- 8.Sinha DN, Gupta PC, Pednekar MS. Use of tobacco products as dentifrice among adolescents in India: Questionnaire study. Br Med J. 2004;328:323–4. doi: 10.1136/bmj.328.7435.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chaudhury K. Tobacco control in India. In: Agrawal SP, Rao YN, Gupta S, editors. Fifty years of cancer control in India. India: New-Delhi cancer control programme; 2002. pp. 204–19. [Google Scholar]
- 10.Connolly GN, Orleans CT, Blum A. Snuffling tobacco out of sport. Am J Public Health. 1992;82:351–3. doi: 10.2105/ajph.82.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta P. Chewing and Smoking: The Underestimated 53 [Google Scholar]
- 12.Seventh World Conference on Tobacco and Health, Perth; 1990. The WHO Framwork Convention on Tobacco Control, World Health Assembly Resolution No. 56. 1, May 21, 2003. Epidemic. [Google Scholar]
- 13.Ashley DL, Beeson MD, Johnson DR, McCraw JM, Richter P, Pirkle JL, et al. Tobacco-specific nitrosamines in tobacco from U.S. brand and non-U.S. brand cigarettes. Nicotine Tob Res. 2003;5:323–31. doi: 10.1080/1462220031000095311. [DOI] [PubMed] [Google Scholar]
- 14.London: Smoking Kills: The Stationary office; 1998. A White Paper on Tobacco. [Google Scholar]
- 15.Balaram P, Sridhar H, Rajkumar T, Vaccarella S, Herrero R, Nandakumar A, et al. Oral cancer in southern India: The influence of smoking, drinking, pan chewing and oral hygiene. Int J Cancer. 2002;98:440–5. doi: 10.1002/ijc.10200. [DOI] [PubMed] [Google Scholar]
- 16.Arno A, Waerhaug J, Lovdal A, Schei O. Incidence of gingivitis as related to sex, occupation, tobacco consumption, tooth brushing and age. Oral Surg Oral Med Oral Pathol. 1958;11:587–95. doi: 10.1016/0030-4220(58)90004-5. [DOI] [PubMed] [Google Scholar]
- 17.Ismail AZ, Burt BA, Eklund SA. Epideological pattern of smoking and periodontal disease in United States. J Am Dent Assoc. 1983;106:617–21. doi: 10.14219/jada.archive.1983.0137. [DOI] [PubMed] [Google Scholar]
- 18.Genco RJ. Assessment of risk of periodontal disease. Compend Suppl. 1994;18:S678–83. [PubMed] [Google Scholar]
- 19.Pindborg JJ. Influence of service in armed forces on incidence of gingivitis. J Am Dent Assoc. 1951;42:517–22. doi: 10.14219/jada.archive.1951.0083. [DOI] [PubMed] [Google Scholar]
- 20.Clarke NG, Shepherd BC, Hirsch RS. The effect of intra-arterial epinephrine and nicotine on gingival circulation. Oral Surg Oral Med Oral Pathol. 1981;52:577–82. doi: 10.1016/0030-4220(81)90071-2. [DOI] [PubMed] [Google Scholar]
- 21.Miller PD., Jr Root coverage with free gingival graft. Factors associated with incomplete coverage. J Periodontol. 1987;58:674–81. doi: 10.1902/jop.1987.58.10.674. [DOI] [PubMed] [Google Scholar]


