Abstract
In HIV vaccine trials, the collection and analysis of participant behavior data associated with risk of acquiring HIV-infection is important for a number of reasons. Although the rationale for behavioral risk assessment in HIV vaccine clinical trials is clear, consistent collection of behavioral data over time and across protocols has been challenging for the HIV Vaccine Trials Network (HVTN). Integrating biomedical and behavioral research within the same preventive vaccine clinical trial has proven difficult. The HVTN conducted an internal landscape analysis to: (1) evaluate the challenges of behavioral risk assessment in HIV vaccine trials and observational studies; (2) explore the impact of the Step Study on behavioral risk assessment measures; and (3) identify strategies to overcome existing challenges and improve the quality of data resulting from behavioral risk analysis. These analyses of behavioral risk within the HVTN revealed several challenges and recommendations for improved behavioral risk data collection in future protocols. The recommendations for improvement include: (1) establishment of protocol-specific behavioral risk working groups that include social and behavioral experts; (2) provision of behavioral rationale and objectives to the development team; (3) creation of a template for geographic- and population-specific assessment of low and high risk behaviors; and (4) pilot testing of behavioral risk assessments. Results also underscored the need for routinely conducted analyses of behavioral data.
Keywords: Biomedical interventions, HIV, Risk behavior, Vaccine clinical trials
1. Introduction
Collecting and analyzing participant behavior data associated with risk of acquiring HIV is important in HIV vaccine trials for several reasons. First, behavioral risk data assist in determining whether risk behavior profiles of participants in experimental and control study groups are comparable at baseline and provide a measure of whether they remain comparable over time. Second, behavioral risk data assist in determining patterns of behavior change during a trial and can indicate differential risk, which might impact exposure and violate blinding. Third, if the vaccine is efficacious, behavioral risk data help determine if behavior is an effect modifier, and can inform estimates of uptake of other biomedical interventions such as Pre-Exposure Prophylaxis (PrEP). Fourth, data can be utilized to assess statistically significant behavioral risks that would be used as covariates in models estimating vaccine efficacy and correlates of protection. Finally, data can inform behavioral eligibility criteria for future trials.
Although the rationale for behavioral risk assessment (BRA) is clear, consistent collection of behavioral data over time and across protocols has been a challenge for the HIV Vaccine Trials Network (HVTN). Integrating biomedical and behavioral research within a preventive vaccine clinical trial has proven difficult for several reasons. First, behavioral assessment time points are driven by study visit schedules, which are determined by protocol specific requirements, such as timing of doses, HIV testing, and primary safety and immunogenicity time points. Differences in protocol visit schedules and questionnaires make acquiring large sample sizes for behavioral data sets across protocols difficult.
Second, researchers endeavor to minimize time and effort required of participants in order to maximize retention and adherence to protocol procedures and to reduce missing data [1,2]. Efforts to reduce participant burden in the HVTN include limiting interview length and frequency of assessment timepoints.
Third, protocol development teams have historically had little or no social and behavioral science expertise and have relied on existing BRA templates from early phase I vaccine trials. Social and behavioral objectives and endpoints have largely been considered post hoc.
Results of the Step study and RV144 highlight the limitations of current methods of BRA [3,4]. Well-defined measures of behaviors that go beyond binary outcomes are needed so findings such as those in the Step Study and RV144 can be properly examined [4].
To improve the integration of behavioral and biomedical research within the Network, the HVTN Social Scientist and another HVTN staff member conducted formative research and an internal landscape analysis to: (1) explore existing perceptions of BRA and data amongst HVTN staff; (2) evaluate the challenges of BRA in HVTN protocols; (3) explore the impact of inconclusive findings in clinical trials on BRA measures; and (4) identify strategies to overcome existing challenges and improve the quality of behavioral risk data.
2. Methods
A mixed methods approach was utilized to conduct the landscape analysis from March 2011 to February 2012. First, key informant interviews were conducted. Key informants were selected based on involvement in BRA and to mirror HVTN core and site staff representation on protocol development teams. They were asked about the rationale for BRA in the HVTN, including assessment time points, question development, and analysis and dissemination of behavioral risk data. Due to the absence of social science expertise on protocol development teams and across the Network, Social Scientists were not available from the pool of key informants. Human Subjects approval was obtained at the Fred Hutchinson Cancer Research Center (FHCRC) (IR File #8034).
Twenty HVTN staff members who had worked on BRA in protocol development were identified and emailed a request to participate. Eleven respondents (9 protocol design staff, 1 operations staff and 1 community education staff) chose to participate. Because of the sensitive nature of the questions and the small staff at the HVTN we have not provided information regarding staff positions to ensure confidentiality.
An analysis of HVTN BRA questionnaires was also conducted. Key informant interviews informed selection of protocols for analysis and revealed that modifications to the BRA template were largely absent prior to the Step Study results. As such, all included trials are those that were initiated post-Step (with the exception of the Step Study itself (HVTN 502)) (see Table 1). Studies were chosen to represent the breadth of HVTN protocols and the BRA included in these protocols was representative of other similar protocols (i.e., HVTN 069 and HVTN 903) or was revised based on Step results and/or geographic necessity (e.g., HVTN 505 and HVTN 906).
Table 1.
Analysis of Behavioral Risk Assessment Questionnaires in HVTN Trials.
| Protocol | Short title | Trial type |
|---|---|---|
| HVTN 069 | Evaluation of Different Routes of Vaccine Administration | Phase IB |
| HVTN 404 | Long-term Follow-up of HIV-1 Infected Participants from Early Phase HIV Vaccine Trials or HIV Vaccine Preparedness Cohorts | Roll-over/follow-up |
| HVTN 502 | Step Study: Efficacy (Test of Concept) Study of Merck Ad5 HIV-1 Vaccine, US | Phase IIB |
| HVTN 503 | Phambili: Efficacy Study of Merck Ad5 HIV-1 Vaccine, RSA | Phase IIB |
| HVTN 503a | Feasibility Study for Recruiting Partners of HIV Vaccine Trial Participants | Observational |
| HVTN 504 | Observational Follow-up of Adult Participants enrolled in the Step Study | Roll-over/follow-up |
| HVTN 505 | Efficacy Study of VRC DNA + rAd5 HIV-1 Vaccine | Phase IIB |
| HVTN 802 | Observational Study of HIV-Infected Participants from Phase 2b-3 HIV-1 Vaccine Trials | Roll-over/follow-up |
| HVTN 903 | HIV Vaccine Preparedness Study | Vaccine Preparedness |
| HVTN 906 | Longitudinal Study of Women at High Risk for HIV-1 in the US | Observational |
| HVTN 907 | Longitudinal Study of Female Sex Workers in the Caribbean | Observational |
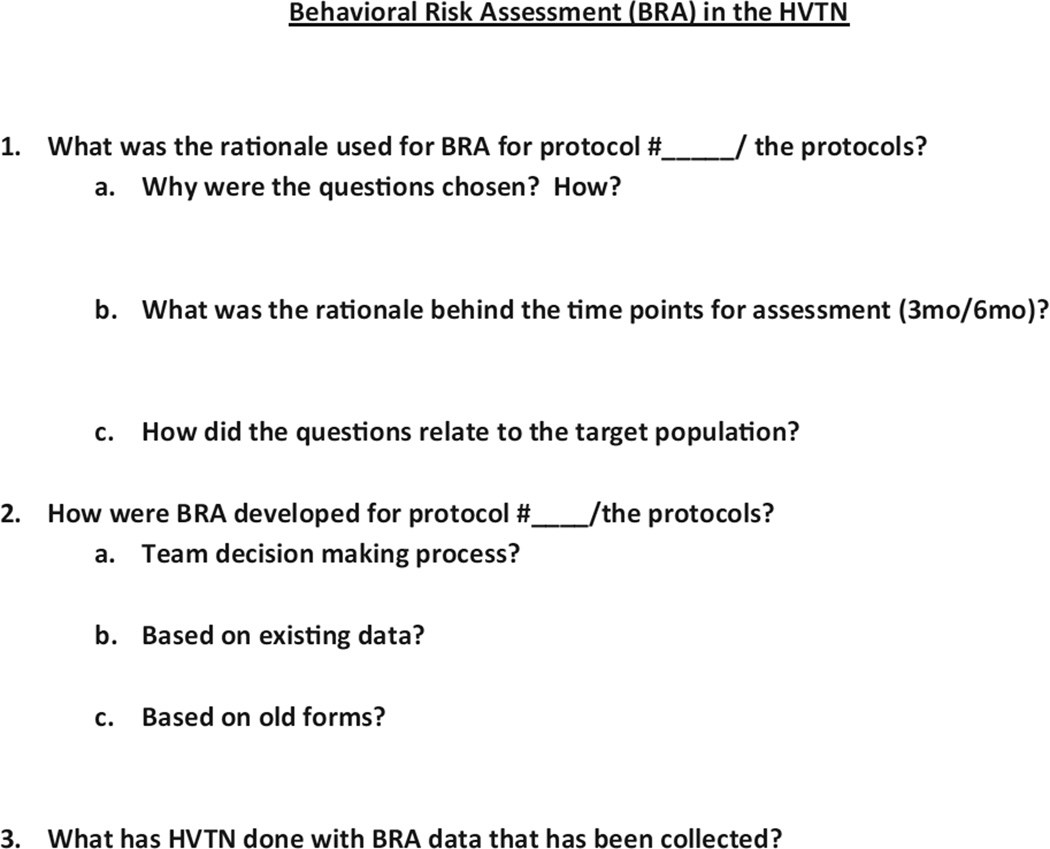
Two interviewers (MA and MN) independently conducted interviews (see Fig. 1). Thematic analysis was utilized to review and code interview transcripts, employing a constant comparative method [5]. First, two investigators independently coded the first 5 interviews and met to review codes – a summative or essence-capturing attribute assigned to a short portion of text (e.g., lack of social science expertise) [6] – and created a codebook. The codebook was used to reanalyze the transcripts and generate new codes in an iterative process. Differences in coding were resolved by consensus among three investigators. Subsequent interviews were coded independently using the codebook. To enhance validity of the findings, data source and investigator triangulation were employed [7].
Fig. 1.
Behavioral risk assessment (BRA) in the HVTN.
The landscape analysis consisted of a review of behavioral risk questions, time points, and assessment periods across the included protocols. Case report forms (CRFs) were reviewed to identify behavioral risk questions for each protocol. These questions were entered into Excel (see Table 2 for an example) and grouped according to risk behaviors. Within each risk behavior category, subgroups were created to capture recall period (e.g., last week) and assessment timepoint (e.g., baseline). Questions were analyzed for consistency across same-phase trials with respect to behaviors, recall periods, and assessment timepoints. The extent to which behavioral risk questions differed because of protocol population characteristics and geographic epidemiology was analyzed.
Table 2.
Male sex partner questions in select HVTN protocols.
| Phase I | Roll over | Phase II | Observational | VPa | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 69 | 404/802 | 504 | 502 | 503b | 505 | 503a | 906 | 907 | 903 | |
| LOCATION (RSA = Republic of South Africa; US = United States of America; Peru = Iquitos, Peru; C = Caribbean Islands, GB = Gaborone, Botswana; CA = Canada; SA = South America; A = Australia) | US and Peru | RSA, US, Peru, and C | US, CA, C, SA, and A | US, CA, C, SA, and A | RSA | US | RSA | US | US and C | GB, Peru, and C |
| SAMPLE SIZE | 90 | 193 | 2060 | 3000 | 801 | 2462 | 18 | 799 | 800 | 916 |
| PARTICIPANT RECRUITMENT YEARS | 06–07 | 08–13 | 2009 | 04–07 | 2007 | 09–13 | 10–11 | 09–10 | 09–10 | 03–06 |
| MALE SEX PARTNERS | ||||||||||
| Past week: # times vaginal sex w/out a condom w/male partners (HIV+/−/not sure) | X | |||||||||
| Past week: # times anal sex w/out condom with male sex partners (HIV+/−/unsure) | X | |||||||||
| 3 months – # male partners | X | X | X | |||||||
| 3 months – # new male partners | X | |||||||||
| 3 months – # male anal sex partners | X | |||||||||
| 3 months – any male anal sex partners HIV positive | X | |||||||||
| 3 months – # HIV infected male partners | X | X | X | X | ||||||
| 3 months – # non-HIV-infected male partners | X | X | X | X | ||||||
| 3 months – # HIV status unknown male partners | X | X | X | |||||||
| 3 months – # times insertive anal sex w/penis in partners rectum HIV +/−/unknown | X | |||||||||
| 3 months – # times insertive anal sex w/condom whole time – HIV +/−/unknown | X | |||||||||
| 3 months – #HIV+/−/unknown men had anal sex when you were a top (insertive) | X | |||||||||
| 3 months – # total times you were a top (insertive) w/HIV+/−/unknown men | X | |||||||||
| 3 months – # times you were a top and condom NOT used whole time HIV+/−/unknown | X | |||||||||
| 3 months – # different men where you were a top WITHOUT condom HIV+/−/unknown | X | |||||||||
| 3 months – # HIV+/−/unknown men had anal sex when you were a bottom (receptive) | X | |||||||||
| 3 months – # total times you were a bottom (receptive) HIV+/−/unknown | X | |||||||||
| 3 months – # times you were a bottom and condom NOT used whole time HIV+/−/unknown | X | |||||||||
| 3 months – # different men where you were a bottom WITHOUT condom HIV+/−/unknown | X | |||||||||
| 3 months – # HIV +/−/unknown men you had anal sex knew you were HIV+ | X | |||||||||
| 3 months – # HIV +/−/unknown men you had anal sex with you directly told you were HIV+ | X | |||||||||
| 3 months – # times receptive anal sex w/penis in your rectum HIV+/−/unknown | X | |||||||||
| 3 months – # times receptive anal sex condom used whole time HIV+/−/unknown | X | |||||||||
| 3 months – # times oral sex with ejaculation AND w/out condom | X | |||||||||
| 3 months – # times oral sex with ejaculation OR w/out condom | X | |||||||||
| 3 months – penis in partners rectum condom used whole time – HIV+/−/unknown | X | X | ||||||||
| 3 months – penis in partners rectum no condom or part time – HIV+/−/unknown | X | X | ||||||||
| 3 months – partner’s penis in your rectum condom used whole time – HIV+/−/unknown | X | X | ||||||||
| 3 months – partner’s penis in your rectum no condom or part time HIV+/−/unknown | X | X | ||||||||
| 3 months – oral sex partner ejaculated in mouth w/out condom – HIV+/−/unknown | X | X | ||||||||
| 3 months – # times vaginal sex w/penis in your vagina HIV+/−/unknown | X | |||||||||
| 3 months – # times vaginal sex/penis in vagina/condom whole time HIV+/−/unknown | X | |||||||||
| 3 months – # times anal sex penis in your rectum HIV +/−/unknown | X | |||||||||
| 3 months – # times anal sex/penis in rectum/condom whole time HIV+/−/unknown | X | |||||||||
| 6 months – had any casual male partners | X | |||||||||
| 6 months – # casual male partners | X | |||||||||
| 6 months – have you had any male partners | X | |||||||||
| 6 months – # male partners | X | X | X | X m/f | X | |||||
| 6 months – # male vaginal sex partners (HIV+/−/not sure) | X | |||||||||
| 6 months – # male anal sex partners (HIV+/−/not sure) | X | |||||||||
| 6 months – unprotected vaginal/anal sex w/male partners | X | |||||||||
| 6 months – # male part NO condom receptive (bottom) | X | |||||||||
| 6 months – # male part NO condom insertive (top) | X | |||||||||
| 6 months – # male part always use condom/barrier oral | X | |||||||||
| 6 months – # male partners always use condom vaginal/anal | X | |||||||||
| 6 months – # HIV infected male partners | X | X | X m/fc | X | X | |||||
| 6 months – # non-HIV-infected male partners | X | X | X m/f | X | X | |||||
| 6 months – # HIV status unknown male partners | X | X | X m/f | X | X | |||||
| 6 months – protected insertive anal intercourse HIV+/−/unknown | X | X | X | |||||||
| 6 months – unprotected insertive anal intercourse HIV+/−/unknown | X | X | X | |||||||
| 6 months – protected receptive anal intercourse HIV+/−/unknown | X | X | X | |||||||
| 6 months – unprotected receptive anal intercourse HIV+/−/unknown | X | X | X | |||||||
| 6 months – receptive oral sex with ejaculation | X | X | ||||||||
| 6 months – protected vaginal intercourse HIV+/−/unknown | X | X | X | |||||||
| 6 months – unprotected vaginal intercourse HIV+/−/unknown | X | X | X | |||||||
| 6 months – protected anal intercourse | X | X | X | |||||||
| 6 months – unprotected anal intercourse | X | X | X | |||||||
| 6 months – oral sex – ejaculation w/partners penis in mouth w/or w/o condom | X | X | ||||||||
| 6 months – oral sex partner’s penis in mouth NO condom HIV+/−/unknown | X | |||||||||
| 6 months – # vaginal sex male partners NO condom (HIV+/−/not sure) | X | |||||||||
| 6 months – # anal male sex partners NO condom (HIV+/−/not sure) | X | |||||||||
| 6 months – # new (1st time sex) male partners HIV+/−/not sure | X | |||||||||
Vaccine preparedness.
Assessments were initially performed every 6 months.
m/f = asked of both male and female participants.
3. Results
Data indicated clear differences between early phase and later phase BRA rationale for the selected protocols, as was expected because phase I studies generally include only individuals who are at low risk for HIV infection while phase II trials are typically comprised of individuals at higher risk. For both phases of the selected vaccine trials, there was a clear shift in BRA rationale and data collection after the Step Study results [8] indicated that the vaccine was not efficacious in reducing HIV infection and that subgroups of men who received vaccine (uncircumcised and Ad5 seropositive at enrollment) had an increased risk of HIV acquisition. The increased relative risk of HIV acquisition among some sub-groups of male vaccine recipients compared to male placebo recipients observed in the Step Study [3] was not explained by differences in risk behaviors (see Table 3), but more robust behavioral risk data might have revealed differences [3,4].
Table 3.
Step study behavioral risk questions.
| 39 Behavioral risk questions |
| 6 month assessment timepoints and recall period |
Questions:
|
3.1. Behavioral risk assessment analysis
3.1.1. Phase I protocols
Immediately prior to Step, phase I trials administered BRAs at screening and baseline (e.g., day of first vaccination) with no follow-up assessment time points. The phase I BRA template was viewed as providing limited data, particularly because it did not allow for identification of same sex vs. heterosexual sexual activity. The general consensus among key informants was that phase I BRA was used to document behavior at the beginning of the trial, and remained virtually “untouched” prior to the Step Study results.
Following Step, the HVTN developed new guidelines defining low risk behavior for purposes of determining eligibility for phase I trials. These guidelines, which continue to evolve, led to corresponding revisions in the standard phase I BRA, including soliciting more information about participants’ risk behaviors, particularly to track changes in behaviors assessed at baseline for eligibility (see Table 4).
Table 4.
Phase one behavioral risk assessment revisions post-step study results.
| Assessment time point | Prior to step study Screening and baseline only | Post step study results Screening, baseline and every 6 months |
|---|---|---|
| Behavioral risk questions (n) | ||
| Allowance for distinction between same sex vs. heterosexual sexual activity | No | Yes |
| Sexual partners | 4 | 7 |
| Exchange sex | 1 | 2 |
| STI history | 0 | 3 |
| Partner concurrency | 0 | 1 |
| Alcohol and other drug use | Drug use (n = 4) | Alcohol and other drug use (n = 4) |
3.1.2. Phase II protocols
For phase II studies, BRA design is largely driven by protocol objectives, study population, and products tested, and a team approach has been used for question development. The team generally consists of one Statistical Center for HIV/AIDS Research & Prevention (SCHARP) staff member, an HVTN Clinical Research Site (CRS) staff member, principal investigator(s), members of the HVTN Social and Behavioral Working Group, and (for protocols since 2010) the HVTN Social Scientist. Recent BRAs have utilized computer assisted self-interviewing (CASI) and audio computer assisted self-interviewing (ACASI). The assessment also allows for tailored, protocol-specific questions (e.g., heterosexual risk in South Africa).
Following Step, visit frequency was increased in Ad5 vaccine-specific phase II trials to closely monitor new HIV infections and possible relationship to vaccine. Additional risk factors were measured including sexual victimization, living situation, and quality of social relationships. Questions regarding sex partners were more detailed. In prior risk assessments participants were asked to report number of partners or number of episodes they had unprotected/ protected sex with a partner. Beginning with the HVTN’s first phase II trial post-Step, HVTN 505, participants were asked to report both number of partners and episodes to determine the better predictor of HIV acquisition outcome. Questions specific to sero-status were added to determine the number of HIV-positive, HIV-negative, and sero-status unknown partners. Finally, respondents were asked about condom use, breakage, and slipping and about sexual risk behaviors with different types of partners, including primary, single occasion, multiple casual, and sex clients.
3.2. Key informant interview analysis
Formative data collection revealed several key challenges (see Table 5). First, staff felt that the BRA rationale and goals were unclear. Several staff members perceived that the inclusion of behavioral risk questions was done out of investigator personal interest and was not based on a need for protocol-specific data.
Table 5.
Formative Data Themes and Quotes.
| THEMES | QUOTES |
|---|---|
| Rationale and Goals for conducting Behavioral Risk Assessment Unclear | There was clear rationale but whether everyone bought into it or knew it beats me. For me there is always a concern about is this the best way to look at the question and is the question going to be used in analysis or just “interesting”. At [name] we are always asking the question, Is this data that is going to be used? We can create questions but we often wonder what expertise goes into what questions will be asked. |
| Unaware of behavioral risk assessment methods and measurement | We as a Network need to distinguish what kind of questions to ask and how to ask them for specific populations. Most of the members of the protocol team do not know what behavioral measures are available and what’s been validated. We often have to look at multiple resources regarding behavioral risk assessment. We look at what we wish we would have collected in previous trials, the Step data, and several other resources and pull them all together. There is a fair amount of borrowing with the idea of trying to get the best of everything. |
| Lack of Epidemiological data for specific populations | It would be helpful if we had specific population risk factors that we could pull from when developing the protocol. We were working mainly with sex workers and high drug use women so in the absence of epidemiological data, lots of the risk assessments and many of the questions came from the experience of the sites. Additional behavioral risk questions were added that were based on feedback from our colleagues regarding the local population. |
| Time restrictions and limitations | One of weaknesses is that we don’t pilot test things. People are always fussing over wording and it is hard to get consensus because multiple people have different views so we are right up against the deadline of when the protocol will open without any time for pilot testing. I have also experienced issues with translating. It would be nice if it was someone’s job to read through the final version to make sure it matches back to English. Taking the back translated version and having someone look through the final copy. What has really helped from [name] perspective is when the behavioral risk planning could start early and we could vet out all of the questions prior to when [name] officially takes off with it. |
| Need for face-to-face meetings | Meeting in person helped with 505 and having a clear decision making plan for the Behavioral risk assessment was good with conference calls later. What really helped is that we spent lots of hours and went to work with the team on risk assessment questions in person. It is always best when the behavioral risk assessment process begins well in advance and team meetings begin early and include face-to-face meetings. |
Second, some staff did not know the type of behavioral risk questions that should be asked or how those questions should be asked for specific populations. The majority were also unaware of current BRA measurement standards or validated measures. The BRA analysis revealed differences in wording of questions and definition of terms (e.g., main partner) indicating lack of discussion about and consistent measurement of behavioral risk across protocols. This may have resulted from the general lack of awareness of BRA rationale and existing standards.
Third, interview respondents noted the lack of readily available current epidemiological data for specific populations, and risk factor information specific to study geographic regions and sub-populations. This was not supported by the BRA analysis, which revealed that protocol development teams were successful in obtaining information about local HIV epidemiology and incorporating this information into the design of protocol-specific BRAs. This was particularly true in HVTN 906 and HVTN 907 where local stakeholders were consulted and information was gathered about local HIV prevalence and incidence, sex practices, and risk behavior and was utilized to develop appropriate behavioral risk questions.
Fourth, in most protocols behavioral risk questions were developed in parallel with the trial opening deadline, which leaves no time for pilot testing or translation. Though behavioral risk questions are often translated from English into another language, there is often no time for back translation and review of the final versions.
Finally, due to geographic distribution of protocol team members, many team meetings occur via conference call. Key informants voiced frustration with this process, noting the challenges of developing a clear decision making plan and a timeline for development of BRA in the absence of a face-to-face meeting.
4. Discussion
The conduct of this BRA landscape analysis and the resulting organizational awareness of the limitations inherent in the existing protocol development process have led to changes in both the composition and processes of protocol development teams.
Within the HVTN, behavioral risk data collection has improved greatly with the implementation of a streamlined team approach, which includes protocol-specific working groups comprised of members with social and behavioral science expertise. Within the Network there are only a few scientists with social and behavioral science training so there are usually two (and at minimum one) social and behavioral science experts in these groups of ten to fifteen members. Membership is open to community representatives, site staff, and biomedical, epidemiologic, and clinical scientists. The groups develop behavioral risk questions specific to the populations of interest, study products, and injection schedule of each protocol. With this approach social and behavioral science questions are considered a priori, an important step in moving the Network toward better integration of biomedical and social and behavioral science [9,10]. The team consolidates behavioral risk questions from previous trials with similar characteristics (e.g., similar phase, population, products) and utilizes this as a template when generating questions for new protocols in development. Behavioral risk questions are also informed by the literature and new developments in the field.
In addition, the HVTN hired a Social Scientist whose work supplements the team approach. The Social Scientist provides expertise and consistency across protocols, and is a liaison between the protocol development team and the protocol-specific behavioral working group. The Social Scientist is also co-chair for the Network-wide HVTN Social and Behavioral Science Working Group (SBWG). The SBWG addresses social and behavioral science questions that have an impact on the design, implementation, and interpretation of the HVTN’s preventive HIV vaccine trials. In addition, the SBWG has identified social and behavioral science research priorities within the HVTN, and works to incorporate behavioral and social science questions into HVTN studies. The addition of a Social Scientist is a necessary first step in achieving optimal integration of biomedical and social and behavioral science. Yet, as is true in biomedicine, it is impossible for one individual to hold all social and behavioral science expertise, and any true advancement in social and behavioral science within the Network will require additional expertise in these areas.
5. Limitations
The results of this study should be viewed in light of its limitations. First, the interviews were conducted during regular work hours by HVTN staff obtaining information from HVTN core and site staff conducting HVTN trials. The content and focus is inclusive of BRAs in HVTN trials enrolling participants from November 2008 (post Step results) to May 2011 and may not generalize to other HVTN trials or to other organizations conducting vaccine or clinical trials. Second, to increase comfort and honest disclosure among staff volunteering to be participants, interviews were not recorded. The absence of this more rigorous data collection method may have resulted in the omission of important data. Finally, all key informant interviews were conducted by the HVTN Social Scientist and an HVTN Clinical Trials Manager who knew and worked together in the same organization with the key informants. Thus, results may have been influenced by social desirability and some key informants may have answered based on their desire to be perceived as good employees. Furthermore, this may have led to an avoidance of being critical of the organization in both questions and responses.
6. Implications
This analysis has identified several steps to improve the collection of behavioral risk data in the HVTN. To improve education regarding the rationale and goals of BRA, the protocol team should receive detailed information about the behavioral and biomedical rationale, objectives, and schema early in protocol development. This may assist in improved integration of behavioral and biomedical data collection, analysis, and dissemination.
In addition, protocol teams would benefit from information regarding population-specific behavioral risk questions. An overview of factors influencing the accuracy of self-reported risk behavior assessment methods would facilitate the development of strategies to increase validity and reliability of behavioral risk data collection. This overview could include information on recall periods and the use of CASI and ACASI. For example, information on recall periods could explain that shorter recall periods are more likely to result in the use of more reliable recall strategies [11–19]. In addition, information could be provided about ACASI and its utility in high-risk populations [20,21].
Key informants suggested creating templates for geographicand population-specific assessment of both low- and high-risk behaviors. Similar templates exist for biomedical data collection, and are used to facilitate protocol development and data analysis. Developing cross-protocol behavioral risk assessment templates (specific to phase, product, population, etc.) may facilitate cross-protocol comparisons, enhance behavioral data analysis through increased power with larger data sets, and facilitate efficient protocol development by providing a foundation for BRA within same-phase trials.
The team approach to BRA outlined above addresses several challenges identified by key informants. Identifying a behavioral team early in protocol development is critical to ensure adequate BRA preparation time and facilitate better integration of biomedical and behavioral objectives.
A more deliberate approach to BRA early in protocol development will ensure that it is not considered post hoc and will allow time for discussion and also for translation and pilot testing. Furthermore, staff with social and behavioral expertise (i.e., HVTN Social Scientist) can ensure the reliability and validity of behavioral risk data, for example, by facilitating activities like translation and pilot testing.
Key informants suggested that BRA development would be improved if the protocol-specific behavioral team met face-to-face to establish study objectives and a decision-making plan for behavioral risk assessment. In the one case where the behavioral risk team met face-to-face (HVTN 505), team members perceived the meeting as extremely beneficial since the team established a decision-making plan and timeline that aided progress during sub-sequent conference calls.
7. Future directions
The analysis revealed a need for routinely conducted analyses of behavioral data in the HVTN. Suggestions for future analyses included: examining low risk participants among phase I and some phase II studies, focusing on behavior changes over time in low risk MSM; exploring alcohol and other drug use across phase I and II trials; obtaining data from key informants with direct experience performing BRAs in the context of HIV vaccine clinical trials; and examining adverse events (e.g., pregnancy, STIs) across protocols. Results of these inquiries have potential to inform both biomedical and behavioral aspects of future protocols, facilitating the enrollment of appropriate trial participants for phase I and II trials and contributing to the preservation of participant safety and the achievement of both biomedical and behavioral scientific endpoints in trials. Efforts to apply the best BRA methods and measures will continue to be critical for preventive HIV vaccine studies as non-vaccine prevention modalities (e.g., PrEP) expand in scope and as novel risk assessment methods (e.g., mobile phone technologies) become available.
Acknowledgements
This research was supported by the National Institutes of Mental Health (NIMH) grant number 3U01AI068614-04S1 (to Dr. Larry Corey). This publication resulted (in part) from research for the Leadership Group for a Global HIV Vaccine Clinical Trials Network supported by the National Institute of Allergies and Infectious Diseases (NIAID) grant number 5UM1AI068614.
References
- 1.Ulrich CM, Wallen GR, Feister A, Grady C. Respondent burden in clinical research: when are we asking too much of subjects? IRB. 2005;27(4):17–20. [PubMed] [Google Scholar]
- 2.Bradburn N. Respondent burden. Health survey research methods: second biennial conference; Williamsburg, VA. Washington, DC: U.S. Government Printing Office; 1977. [Google Scholar]
- 3.Buchbinder SP, Mehotra DV, Duerr A, Fitzgerald DW, Mogg R, Li D, et al. Efficacy assessment of cell-mediated immunity HIV-1 vaccine (the Step Study): a double-blind, randomized, placebo-controlled, test-of-concept trial. Lancet. 2008;372(9653):1881–1893. doi: 10.1016/S0140-6736(08)61591-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koblin BA, Mayer KH, Noonan E, Wang CY, Marmor M, Sanchez J, et al. Sexual risk behaviors, circumcision status, and preexisting immunity to adenovirus type 5 among Men Who Have Sex with Men participating in a randomized HIV-1 efficacy trial: Step Study. J Acquir Immune Defic Syndr. 2012;60(4):405–413. doi: 10.1097/QAI.0b013e31825325aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Strauss A, Corbin J. Basics of qualitative research: grounded theory procedures and techniques. Newbury Park, CA: Sage; 1990. [Google Scholar]
- 6.Saldana J. The coding manual for qualitative researchers. Thousand Oaks, CA: Sage; 2009. [Google Scholar]
- 7.Miles MB, Huberman AM. Qualitative data analysis: a sourcebook of new methods. 2nd ed. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 8.Gray G, Buchbinder S, Duerr A. Overview of Step and Phambili trial results: two phase IIb test-of-concept studies investigating the efficacy of MRK adenovirus type 5 gag/pol/neg subtype B HIV vaccine. Curr Opin HIV AIDS. 2010;5(5):357–361. doi: 10.1097/COH.0b013e32833d2d2b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Newman PA. Integrating social and biomedical science in HIV vaccine research: obstacles, opportunities and ways forward. Expert Rev Vaccines. 2012;11(1):1–3. doi: 10.1586/erv.11.162. [DOI] [PubMed] [Google Scholar]
- 10.Lau CY, Stansbury JP, Gust DA, Kafaar Z. Social and behavioral science in HIV vaccine trials: a gap assessment of the literature. Expert Rev Vaccines. 2009;8(2):179–190. doi: 10.1586/14760584.8.2.179. [DOI] [PubMed] [Google Scholar]
- 11.Bogart LM, Walt LC, Pavlovic JD, Ober AJ, Brown N, Kalichman SC. Cognitive strategies affecting recall of sexual behavior among high-risk men and women. Health Psychol. 2007;26:787–793. doi: 10.1037/0278-6133.26.6.787. [DOI] [PubMed] [Google Scholar]
- 12.Jaccard J, McDonald R, Wan CK, Dittus PJ, Quinlan S. The accuracy of self-reports of condom use and sexual behavior. J Appl Soc Psychol. 2002;32:1863–1905. [Google Scholar]
- 13.Fals-Stewart W, O’Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patients: psychometric properties. J Consult Clin Psychol. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- 14.Levy S, Sherritt L, Harris SK, Gates EC, Holder DW, Kulig JW, et al. Test–retest reliability of adolescents’ self-report of substance use. Alcohol Clin Exp Res. 2004;28(8):1236–1241. doi: 10.1097/01.alc.0000134216.22162.a5. [DOI] [PubMed] [Google Scholar]
- 15.Scheurich A, Muller MJ, Anghelescu I, Lorch B, Dreher M, Hautzinger M, et al. Reliability and validity of the form 90 interview. Eur Addict Res. 2005;11(1):50–56. doi: 10.1159/000081417. [DOI] [PubMed] [Google Scholar]
- 16.Slesnick N, Tonigan JS. Assessment of alcohol and other drug use by runaway youths: a test–retest study of the form 90. Alcohol Treat Q. 2004;22(2):21–34. doi: 10.1300/J020v22n02_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carey MP, Carey KB, Maisto SA, Gordon CM, Weinhardt LS. Assessing sexual risk behavior with the Timeline Followback (TLFB) approach: continued development and psychometric evaluation with psychiatric outpatients. Int J STD AIDs. 2001;12:365–375. doi: 10.1258/0956462011923309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sieving R, Hellerstedt W, McNeely C, Fee R, Snyder J, Resnick M. Reliability of self-reported contraceptive use and sexual behaviors among adolescent girls. J Sex Res. 2005;42(2):159–166. doi: 10.1080/00224490509552269. [DOI] [PubMed] [Google Scholar]
- 19.Sneed CD, Chin D, Rotheram-Borus MJ, Milburn NG, Murphy DA, Corby N, et al. Test–retest reliability for self-reports of sexual behavior among Thai and Korean respondents. AIDS Educ Prev. 2001;13(4):302–310. doi: 10.1521/aeap.13.4.302.21429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boekeloo BO, Schiavo L, Rabin DL, Conion RT, Jordan CS, Mundt DJ. Self-reports of HIV risk factors by patients at a sexually transmitted disease clinic: audio vs. written questionnaires. Am J Public Health. 1994;84(5):754–760. doi: 10.2105/ajph.84.5.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, violence: increased reporting with computer survey technology. Science. 1998;5365;208:867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]