Abstract
Background
Visual assessment of wall motion abnormalities (WMA) by 2-dimensional echocardiography (2DE) is the most semi-quantitative method used to detect coronary artery disease (CAD), but it carries many limitations. Speckle tracking echocardiography (STE) overcomes these limitations and allows an objective quantification of myocardial deformation. The aim of the study to examine the accuracy of global and segmental longitudinal strain (LS) for the detection of CAD compared with visual assessment of WMA using coronary angiography as a golden standard.
Methods
The study enrolled 25 patients (mean age 51.0 ± 8.7, 64% are male) referred to coronary angiography with clinical suspicion of CAD. 2DE assessment of WMA and evaluation of LS using STE were performed using left ventricular 17-segments models. Significant CAD was defined as ≥ 50% stenosis in one or more major coronary arteries by angiography.
Results
Patients were classified into 2 groups: group I included 15 patients with significant CAD and group II included 10 patients with insignificant and/or absence of CAD. WM score was strongly correlated with the global LS in group I and II (R = 0.80, p < 0.0001 and R = 0.88, p < 0.0001 respectively). In all patients, 425 segments were analyzed. WMA was detected in 163 segments of 425 (38.3%) while abnormal LS was detected in 214 segments (50.3%). Compared with coronary angiography, the total sensitivity, specificity and accuracy for visual analysis and STE were (56%, 88.2%, and 60% vs. 68.6%, 77%, and 81.8% respectively).
Conclusion
Segmental LS is more accurate for the detection of ischemic myocardial segment corresponding to functionally relevant coronary anatomy than visual assessment of WM.
Keywords: Speckle tracking, Longitudinal strain, Wall motion abnormalities
Introduction
Standard models of left ventricular (LV) segmentation have been used to facilitate a more detailed analysis of regional LV function. The use of the 17-myocardial segment model has been recommended by the American Society of Echocardiography and American Heart Association.1),2) Echocardiographic evaluation of segmental and global myocardial function plays a critical role in the diagnosis and management of coronary artery disease (CAD). Visual assessment of regional wall motion abnormalities (WMA) is commonly used in most laboratories. It relies mainly on myocardial radial performance which is limited by high inter and intra-observer variability.3) Speckle-tracking echocardiography (STE) is a new noninvasive imaging technique that quantitatively analyzes global and regional myocardial function. It presents an objective, semi-automatic, and angle-independent analysis of longitudinal peak systolic strain (LS) based on speckle tracking and provides a single bull's-eye summary of the LV segmental wall strain.4),5) Many published data supported the use of STE longitudinal strain to identify and risk-stratify CAD with good accuracy and reproducibility.6),7) The aim of this study was to assess the accuracy of global and segmental LS using STE to detect resting myocardial ischemia compared with visual assessment by conventional 2-dimensional echocardiography (2DE) using coronary angiography as gold standard.
Methods
A prospective study of 25 patients (51.0 ± 8.7, 64% are male) were referred for assessment of CAD by coronary angiography according to ACC/AHA guidelines.8) The reasons for referral to coronary angiography were [angina class III with multiple cardiovascular risk factors in 10 patients, positive stress electrocardiogram (ECG) in 5 patients, typical chest pain with resting ECG changes in 4 patients, atypical chest pain with impaired LV systolic function by conventional 2DE in 4 patients and typical chest pain after surgical revascularization in 2 patients]. The only exclusion criterion was evidence of previous attack of myocardial infarction by ECG and 2DE due to its ease identification by resting WMA. At the day of coronary angiography, conventional 2D echocardiography and STE were performed and inclusion of patients was based on adequate image quality and sinus rhythm.
Echocardiography and STE
Conventional 2DE was performed according to guidelines using a commercial ultrasound system (Vivid 7, GE Health Medical, Milwaukee, WI, USA) supported with a multi-frequency transducer (M3S 1.7/3.4 MHz). Visual analysis of the contractile function of LV was interpreted according to the American Society of Echocardiography criteria using the 17 segments module.1) A semiquantitative four-point scoring system (1, normal; 2, hypokinesia; 3, akinesia; 4, dyskinesia) was used to analyze each study. The sum of the WM scores, averaged over the number of segments with interpretive scores, gave the global WM score index.
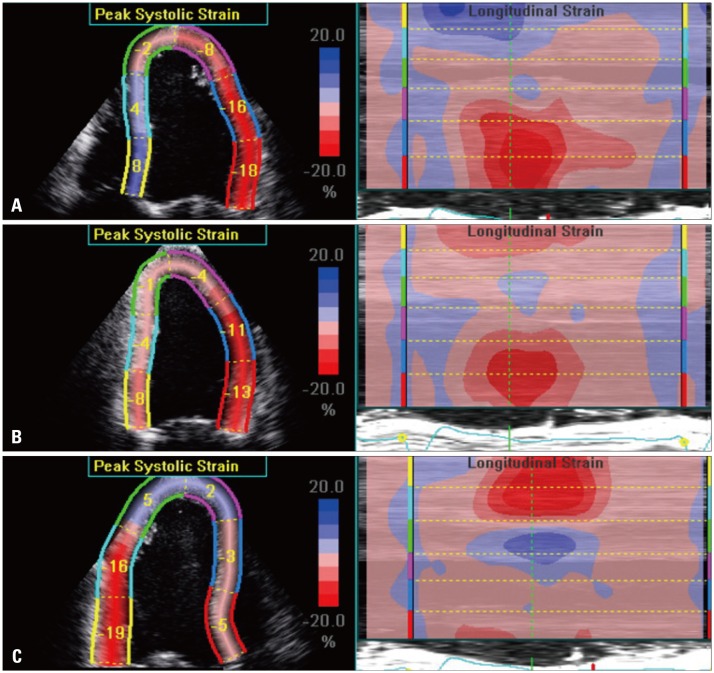
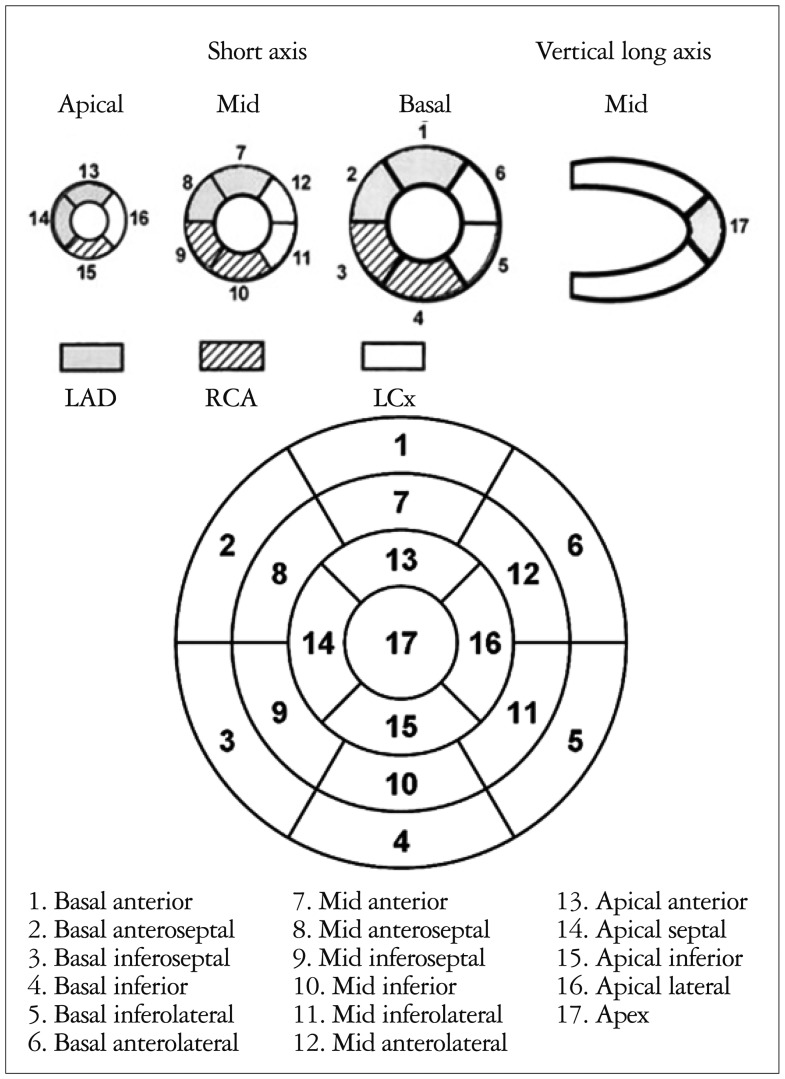
After the completion of the 2DE study, STE was performed using the automated function imaging algorithm to measure the peak systolic LS in a 17-segment LV model. It was performed through an off-line analysis of 3 digitally stored 2-D images (apical long-axis, 2- and 4-chamber) with high frame rates (> 60 frame/s) using commercial imaging analysis software (EchoPAC 6.1.0, GE Health Medical, Milwaukee, WI, USA).9) End-systole was defined as aortic valve closure in the apical long-axis view by continuous Doppler wave recording. Automated endocardial delineation was obtained through marking the mitral annulus level and at the apex on each digital loop. The region of interest was manually adjusted if automated delineation is not optimal. Segments with poor image acquisition or artifacts were excluded due to inability to measure LS. Segmental LS was calculated as the percentage of lengthening or shortening and the results for each plane were displayed (Fig. 1). The sum of LS, averaged over the number of segments with interpretive scores, gave the global longitudinal strain and can be displayed in single bull's-eye view (Fig. 2). Offline analysis of WMA and STE was performed by one ininvestigator at 2 separate sessions unaware of coronary angiographic results. The cut off values for normal and ischemic segments were considered (≤ -11% for normal and > -11% for abnormal) due to previous validation.10)
Fig. 1.
Segmental longitudinal strain displayed in 3 image planes: (A) apical 4-chamber, (B) apical 2-chamber and (C) apical long axis views
Fig. 2.
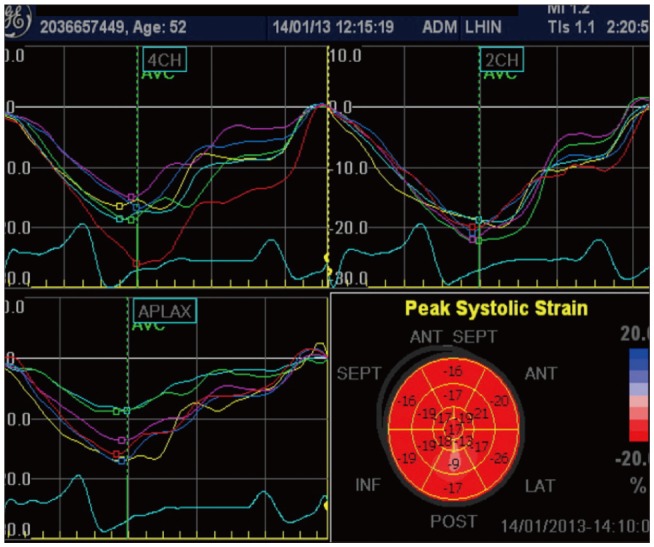
Example of display of all left ventricular segments in bulle's eye view with the corresponding curves in normal subject
Coronary angiography
Selective coronary angiography was performed using a biplane system with the standard technique from femoral approach. All views were acquired and reviewed by 2 experienced interventionists. Both were blinded with the echocardiographic findings. Diagnosis of significant CAD was considered when ≥ 50% reduction of vessel diameter by quantitative coronary angiography was observed in at least one major coronary artery.11) Distribution of each coronary artery territory on myocardial segments was displayed (Fig. 3).
Fig. 3.
Nomenclature of left ventricular myocardial segments with their distribution according to coronary artery territories. LAD: left anterior descending, RCA: right coronary artery, LCx: left circumflex.
Statistical analysis
Statistical analysis was performed using the software package SPSS version 11.5 (SPSS Inc., Chicago, IL, USA). All data obtained were presented as mean ± standard deviation. To determine the accuracy of STE and visual assessment of WMA for the detection of hemodynamically significant CAD, > 50% stenosis was used as a cut point of significant CAD. The diagnostic accuracy of both techniques was carried out by using Decision Matrix tables in which sensitivities, specificities, predictive values were calculated and compared.12) The clustered nature of the myocardial territories per subject was accounted by estimating the observed distribution (95% confidence intervals) according to Zhou et al.13)
Results
Baseline criteria
The study included 25 consecutive patients (51.0 ± 8.7, 64% are male). Depending on coronary angiographic findings, the patients were classified into 2 groups: group I included 15 patients with significant CAD and group II included 10 patients with insignificant and/or absence of CAD. No significant differences were found between both groups in terms of age, sex, blood pressures, or clinical risk factors.
Visual analysis and STE
Global assessment of LV showed strong correlation between WM score and global LS in group I and II (R = 0.80, p < 0.0001 and R = 0.88, p < 0.0001 respectively). In the 25 patients, 425 segments were analyzed: 175 left anterior descending coronary artery (LAD), 125 right coronary artery (RCA), and 125 left circumflex artery (LCx). Visual assessment of WMA showed that, while by STE 214 segments (50.3%) were judged as abnormal.
Visual analysis and coronary angiography
In all patients, 163 segments of 425 (38.3%) were judged as abnormal by WMA (67 segments of LAD territory, 50 segments of LCx and 46 segments of RCA). In group I, of 105 LAD segments, 60 showed WMA. Similarly, of 75 RCA segments analyzed, 40 showed WMA. Of 75 LCx segments analyzed, 43 showed WMA. In group II, WMA was detected in 20 segments of 170 (7 segments of both LAD and LCx and 6 segment of RCA). The total sensitivity, specificity, accuracy, positive predictive value and negative predictive value of visual analysis of WMA to detect coronary artery stenosis are 56%, 88.2%, 60%, 89.3%, and 57.2%. The sensitivity rates for the diagnosis of LAD, LCx and RCA based on WMA are 57.1%, 53.3%, and 57.3%, respectively. The corresponding specificity rates were 90%, 86%, and 88%, respectively. The accuracy rate was higher for the diagnosis of RCA and LCx (69.6% and 66.4% respectively) than LAD (51.7%) (Table 1).
Table 1.
Sensitivity, specificity and accuracy for the detection of myocardial ischemia in each coronary artery separately by both modalities (WMA and STE)

WMA: wall motion abnormalities, STE: speckle tracking echocardiography, LAD: left anterior descending, LCx: left circumflex, RCA: right coronary artery
STE analysis and coronary angiography
Complete analysis was achieved in all patients within 3.7 ± 2.6 min. Manual modification of endocardial border was performed to get optimal delineation in 5 patients (20%). In all patients, 214 segments of 425 (50.3%) were judged as abnormal by STE (88 segments of LAD territory, 63 segments of LCx and 63 segments of RCA). In group I, of 105 LAD segments, 72 showed abnormal LS. Similarly, of 75 RCA segments analyzed, 52 showed abnormal LS. Of 75 LCx segments analyzed, 51 showed abnormal LS. In group II, abnormal LS was detected in 39 segments of 170 (16 segments of LAD, 12 segments of LCx and 11 segment of RCA). The total sensitivity, specificity, accuracy, positive predictive value and negative predictive value of STE to detect myocardial ischaemia are 68.6%, 77%, 72%, 81.8%, and 62.1%. The sensitivity rates for the diagnosis of LAD, LCx and RCA based on STE are 68.5%, 69.3%, and 68%, respectively. The corresponding specificity rates were 77.1%, 76%, and 78%, respectively. The accuracy rate was 72% for the diagnosis of the three vessels (Table 1).
Discussion
This study demonstrated that analysis of global and segmental LS using STE was matched with coronary angiography and more accurate than visual assessment of WMA for the detection of myocardial ischemia at rest with an equal sensitivity rate for all coronary territories.
Assessment of regional myocardial function using echocardiography plays a critical role in the diagnosis and management of CAD. The visual interpretation of WMA with the conventional 2DE is widely used in most laboratories relies based on the assessment of myocardial thickening and endocardial excursion. However, this approach is subjective, operator dependent, demands complete visualization of the endocardium and is subject to the vicissitudes of cardiac loading and heart rate.3)
Previous studies described the reliability and feasibility of STE to evaluate global and segmental myocardial deformation throughout the cardiac cycle in both normal and abnormal subjects. It is able to investigate LV function (circumferential, radial and longitudinal) without angle dependency.14),15) The current study aimed to evaluate accuracy of STE to detect myocardial ischemia at rest compared with visual assessment of WMA. The cutoff value of LS used for abnormal myocardial segment was > -11 and ≥ 50% reduction of vessel diameter by quantitative coronary angiography was considered for the diagnosis of significant CAD. This percentage of coronary stenosis was considered for the assessment of functional rather than anatomical due to its crucial role in selection of therapeutic option and risk stratification. Previous reports showed that a stenosis of less than 50% is unlikely to be functionally significant, while stenosis of severity between 50% and 70% show a wide variability in their functional significance. There is a lack of correlation between anatomical severity and functional significance of CAD.11),16),17)
In patients without significant CAD (group II), global and segmental LS measurements were comparable to the HUNT study in Norway18) which presented the reference values in 1266 healthy individuals according to age and sex. Segmental analysis using STE showed a higher percentage of abnormal segments compared with visual analysis of WMA (50.3% vs. 38.3%). This can be explained by the limitation of visual analysis to detect WMA at rest even with coexisting severe CAD and thus the need for exercise imaging modalities.19),20) Previous reports described the ability of STE to detect subclinical LV dysfunction earlier before visual analysis of WMA in asymptomatic patients with apparently normal LV ejection fraction.21),22)
The study showed that the total sensitivity of STE was higher than visual analysis of WMA (68.6% vs. 56%) with nearly equal sensitivity rate for all coronary territories. In Choi et al.6) study, STE could discriminate severe 3-vessel or left main disease from lesser CAD with a higher sensitivity and specificity of 79% and 79%, respectively. The higher sensitivity and specificity in Choi et al. study can be explained by the cutoff value of LS they used (-17.9%) for the diagnosis of abnormal myocardial segment. They used a cutoff of percent diameter stenosis ≥ 70% for three epicardial vessels and ≥ 50% for LM coronary artery. Based on their findings, the higher sensitivity of STE has to be interpretated in the high risk subset of CAD. The novelty of the current study is that the patients were classified based on the presence of CAD or not using ≥ 50% reduction of vessel diameter as a cutoff for the diagnosis of significant CAD regardless of the number and nomenclature of the stenosed coronary artery. Also, the cutoff value of LS used for abnormal myocardial segment was > -11 which is higher than the value used by Choi et al.
There are some limitations in our study. First, the number of patients enrolled is relatively small. Second, only LS was evaluated and other parameters e.g., radial and circumferential strain were not.
In conclusion, measurement of global and segmental LS using STE is more sensitive and accurate tool in the identification of WMA at rest than visual analysis. This supports its use to identify and risk-stratify atherosclerotic CAD.
Acknowledgements
I am grateful for the help of Dr. Waqar A and Dr. Al-Asnag M in the interpretation of coronary angiography.
References
- 1.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ, Chamber Quantification Writing Group. American Society of Echocardiography's Guidelines and Standards Committee. European Association of Echocardiography Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T, Verani MS, American Heart Association Writing Group on Myocardial Segmentation and Registration for Cardiac Imaging Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Int J Cardiovasc Imaging. 2002;18:539–542. [PubMed] [Google Scholar]
- 3.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise J, Solomon S, Spencer KT, St John Sutton M, Stewart W, American Society of Echocardiography's Nomenclature and Standards Committee. Task Force on Chamber Quantification. American College of Cardiology Echocardiography Committee. American Heart Association. European Association of Echocardiography, European Society of Cardiology Recommendations for chamber quantification. Eur J Echocardiogr. 2006;7:79–108. doi: 10.1016/j.euje.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 4.Geyer H, Caracciolo G, Abe H, Wilansky S, Carerj S, Gentile F, Nesser HJ, Khandheria B, Narula J, Sengupta PP. Assessment of myocardial mechanics using speckle tracking echocardiography: fundamentals and clinical applications. J Am Soc Echocardiogr. 2010;23:351–369. doi: 10.1016/j.echo.2010.02.015. quiz 453-5. [DOI] [PubMed] [Google Scholar]
- 5.Belghitia H, Brette S, Lafitte S, Reant P, Picard F, Serri K, Lafitte M, Courregelongue M, Dos Santos P, Douard H, Roudaut R, DeMaria A. Automated function imaging: a new operator-independent strain method for assessing left ventricular function. Arch Cardiovasc Dis. 2008;101:163–169. doi: 10.1016/s1875-2136(08)71798-4. [DOI] [PubMed] [Google Scholar]
- 6.Choi JO, Cho SW, Song YB, Cho SJ, Song BG, Lee SC, Park SW. Longitudinal 2D strain at rest predicts the presence of left main and three vessel coronary artery disease in patients without regional wall motion abnormality. Eur J Echocardiogr. 2009;10:695–701. doi: 10.1093/ejechocard/jep041. [DOI] [PubMed] [Google Scholar]
- 7.Nucifora G, Schuijf JD, Delgado V, Bertini M, Scholte AJ, Ng AC, van Werkhoven JM, Jukema JW, Holman ER, van der Wall EE, Bax JJ. Incremental value of subclinical left ventricular systolic dysfunction for the identification of patients with obstructive coronary artery disease. Am Heart J. 2010;159:148–157. doi: 10.1016/j.ahj.2009.10.030. [DOI] [PubMed] [Google Scholar]
- 8.Scanlon PJ, Faxon DP, Audet AM, Carabello B, Dehmer GJ, Eagle KA, Legako RD, Leon DF, Murray JA, Nissen SE, Pepine CJ, Watson RM, Ritchie JL, Gibbons RJ, Cheitlin MD, Gardner TJ, Garson A, Jr, Russell RO, Jr, Ryan TJ, Smith SC., Jr ACC/AHA guidelines for coronary angiography: executive summary and recommendations. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Coronary Angiography) developed in collaboration with the Society for Cardiac Angiography and Interventions. Circulation. 1999;99:2345–2357. doi: 10.1161/01.cir.99.17.2345. [DOI] [PubMed] [Google Scholar]
- 9.Leitman M, Lysyansky P, Sidenko S, Shir V, Peleg E, Binenbaum M, Kaluski E, Krakover R, Vered Z. Two-dimensional strain-a novel software for real-time quantitative echocardiographic assessment of myocardial function. J Am Soc Echocardiogr. 2004;17:1021–1029. doi: 10.1016/j.echo.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 10.Kusunose K, Yamada H, Nishio S, Mizuguchi Y, Choraku M, Maeda Y, Hosokawa S, Yamazaki N, Tomita N, Niki T, Yamaguchi K, Koshiba K, Soeki T, Wakatsuki T, Akaike M, Sata M. Validation of longitudinal peak systolic strain by speckle tracking echocardiography with visual assessment and myocardial perfusion SPECT in patients with regional asynergy. Circ J. 2011;75:141–147. doi: 10.1253/circj.cj-10-0551. [DOI] [PubMed] [Google Scholar]
- 11.Bamberg F, Becker A, Schwarz F, Marcus RP, Greif M, von Ziegler F, Blankstein R, Hoffmann U, Sommer WH, Hoffmann VS, Johnson TR, Becker HC, Wintersperger BJ, Reiser MF, Nikolaou K. Detection of hemodynamically significant coronary artery stenosis: incremental diagnostic value of dynamic CT-based myocardial perfusion imaging. Radiology. 2011;260:689–698. doi: 10.1148/radiol.11110638. [DOI] [PubMed] [Google Scholar]
- 12.Hawass NE. Comparing the sensitivities and specificities of two diagnostic procedures performed on the same group of patients. Br J Radiol. 1997;70:360–366. doi: 10.1259/bjr.70.832.9166071. [DOI] [PubMed] [Google Scholar]
- 13.Zhou XH, McClish DK, Obuchowski NA. Statistical methods in diagnostic medicine. New York: John Wiley and Sons; 2002. [Google Scholar]
- 14.Hoit BD. Strain and strain rate echocardiography and coronary artery disease. Circ Cardiovasc Imaging. 2011;4:179–179. doi: 10.1161/CIRCIMAGING.110.959817. [DOI] [PubMed] [Google Scholar]
- 15.Lorch SM, Ludomirsky A, Singh GK. Maturational and growth-related changes in left ventricular longitudinal strain and strain rate measured by two-dimensional speckle tracking echocardiography in healthy pediatric population. J Am Soc Echocardiogr. 2008;21:1207–1215. doi: 10.1016/j.echo.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 16.Pakkal M, Raj V, McCann GP. Non-invasive imaging in coronary artery disease including anatomical and functional evaluation of ischaemia and viability assessment. Br J Radiol. 2011;84(Spec No 3):S280–S295. doi: 10.1259/bjr/50903757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tonino PA, Fearon WF, De Bruyne B, Oldroyd KG, Leesar MA, Ver Lee PN, Maccarthy PA, Van't Veer M, Pijls NH. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol. 2010;55:2816–2821. doi: 10.1016/j.jacc.2009.11.096. [DOI] [PubMed] [Google Scholar]
- 18.Dalen H, Thorstensen A, Aase SA, Ingul CB, Torp H, Vatten LJ, Stoylen A. Segmental and global longitudinal strain and strain rate based on echocardiography of 1266 healthy individuals: the HUNT study in Norway. Eur J Echocardiogr. 2010;11:176–183. doi: 10.1093/ejechocard/jep194. [DOI] [PubMed] [Google Scholar]
- 19.Kumar SP, Movahed A. Importance of wall motion analysis in the diagnosis of left main disease using stress nuclear myocardial perfusion imaging. Int J Cardiovasc Imaging. 2003;19:219–224. doi: 10.1023/a:1023606223940. [DOI] [PubMed] [Google Scholar]
- 20.Huang WC, Chiou KR, Liu CP, Lee D, Mar GY, Hsiao SH, Chiou CW, Kung MH, Lin SL. Early assessment of left ventricular viability of dyskinesia and akinesia myocardium in patients with acute myocardial infarction: real-time contrast echocardiography versus low-dose dobutamine echocardiography. Acta Cardiol Sin. 2004;20:160–170. [Google Scholar]
- 21.Munk K, Andersen NH, Nielsen SS, Bibby BM, Bøtker HE, Nielsen TT, Poulsen SH. Global longitudinal strain by speckle tracking for infarct size estimation. Eur J Echocardiogr. 2011;12:156–165. doi: 10.1093/ejechocard/jeq168. [DOI] [PubMed] [Google Scholar]
- 22.Nakai H, Takeuchi M, Nishikage T, Lang RM, Otsuji Y. Subclinical left ventricular dysfunction in asymptomatic diabetic patients assessed by two-dimensional speckle tracking echocardiography: correlation with diabetic duration. Eur J Echocardiogr. 2009;10:926–932. doi: 10.1093/ejechocard/jep097. [DOI] [PubMed] [Google Scholar]