Abstract
Objective
This meta-analysis systematically examined the association of reported psychological trauma and posttraumatic stress disorder (PTSD) with functional somatic syndromes including fibromyalgia, chronic widespread pain, chronic fatigue syndrome, temporomandibular disorder, and irritable bowel syndrome. Our goals were to determine the overall effect size of the association and to examine moderators of the relationship.
Methods
Literature searches identified 71 studies with a control or comparison group and examined the association of the syndromes with traumatic events including abuse of a psychological, emotional, sexual, or physical nature sustained during childhood or adulthood, combat exposure, or PTSD. A random effects model was used to estimate the pooled odds ratio and 95% CI. Planned subgroup analyses and meta-regression examined potential moderators.
Results
Individuals who reported exposure to trauma were 2.7 (95% CI = 2.27 – 3.10) times more likely to have a functional somatic syndrome. This association was robust against both publication bias and the generally low quality of the literature. The magnitude of the association with PTSD was significantly larger than with sexual or physical abuse. Chronic fatigue syndrome had a larger association with reported trauma than either irritable bowel syndrome or fibromyalgia. Studies using non-validated questionnaires or self-report of trauma reported larger associations than those using validated questionnaires.
Conclusions
Findings highlight limitations of the existing literature and emphasize the importance of conducting prospective studies, further examining the potential similarities and differences of these conditions, and pursuing hypothesis-driven studies of the mechanisms underlying the link between trauma, PTSD, and functional somatic syndromes.
Keywords: functional somatic syndromes, trauma, PTSD, meta-analysis
INTRODUCTION
Somatic complaints that are medically unexplained are common in all areas of medicine. Approximately one-third of patients seen in primary care report experiencing symptoms for which no organic cause can be found [1–3]. Functional somatic syndromes (FSSs), including fibromyalgia (FM), chronic widespread pain (CWP), chronic fatigue syndrome (CFS), temporomandibular disorder (TMD), and irritable bowel syndrome (IBS), are a set of conditions defined by expert consensus or research diagnostic criteria, that lack currently understood physical or biological etiology or demonstrate inconsistent laboratory abnormalities [4]. Although these conditions are often characterized by symptoms such as pain, fatigue, sleep disturbances, and disability, they are typically complex conditions with a multiplicity of symptoms. Compared to other medical conditions, these unexplained conditions also are commonly associated with anxiety, depression, stressful life events, and psychological trauma in childhood or adulthood [5, 6]. Further, patients with FSSs are more likely to have an increased rate of current and lifetime psychiatric disorders [7].
The co-morbidity of specific FSSs often present challenges to differential diagnosis as they have high rates of overlap in symptoms, especially for FM, CWP, CFS, TMD, and IBS [8]. Due to the absence of distinct biomarkers that help define a syndrome, there is an ongoing debate as to whether FSSs should be defined as separate entities or as one syndrome [9]. While some emphasize the utility of separate diagnostic categories [10], others argue that all FSSs represent one underlying common basic syndrome [4, 11, 12]. However, examining FSSs in a way that focuses both on the similarities and differences between syndromes may provide a better understanding of their etiology and inform future treatment.
One area of potential similarity is the association of FSSs with psychological trauma. In addition to the psychological distress that frequently accompanies exposure to trauma [13], reported trauma is consistently associated with FSSs and other health outcomes [6, 14–17]. Significant links between reported trauma and FSSs are demonstrated for both trauma experienced in adulthood and childhood [5, 14, 18]. However, these studies have significant methodological weaknesses that limit interpretation [17]. Most of the studies that look at childhood trauma and FSSs are cross-sectional and use retrospective self-report accounts [19, 20]. The few existing prospective studies only show a low to modest association between childhood trauma and FSSs [17, 19, 20]. A recent review suggests that nearly all studies examining the association of abuse with FSSs are underpowered [17].
Two meta-analytic reviews have attempted to evaluate the strength of the association between both adult and childhood trauma with FSSs but limited their search to sexual abuse as the type of trauma [21] or FM as the specific FSS [22]. Neither of these meta-analyses examined the potential similarities or differences in how specific FSSs are related to trauma. Further, it is not clear if the association between trauma and FSSs is a result of exposure to trauma or driven by how a person responds to the traumatic event, for example with intense fear, numbing, re-experiencing, and/or avoidance. Posttraumatic stress disorder (PTSD) is a psychiatric condition that requires exposure to a traumatic event and captures an individual’s cognitive and behavioral response in relation to the trauma. While the exact mechanisms underlying the relationship between psychological trauma, PTSD, and FSSs still need to be elucidated [23–26], a recent meta-analytic review examined the association of PTSD with physical health outcomes including pain and gastrointestinal symptoms [27]. However, the study did not examine the strength of PTSD’s association with specific FSSs nor could it speak to the potential moderating effect of trauma exposure versus PTSD.
The goal of this meta-analysis was to provide a comprehensive review of the trauma and FSSs literature by encompassing multiple types of FSSs and reported psychological trauma, as well as PTSD. Given the diversity in the quality of the literature, we focused on FSSs that are defined by established diagnostic criteria based on a configuration of symptoms. Therefore, studies that examined only one symptom or key feature (e.g., chronic pelvic pain) and were not based on established diagnostic criteria for a condition were not included. Our primary aims were to determine the overall effect size of the association between reported trauma and PTSD with FSSs including FM, CWP, CFS, TMD, and IBS; and to examine the possible moderating effects of gender, type of trauma, type of FSS, type of trauma assessment, type of FSS assessment, age at time of trauma, and type of sample.
METHODS
Search and Screening Strategy
The review and meta-analysis was performed according to the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [28]. Articles were identified through searches of the electronic databases PubMed/MEDLINE (1948 – January 2012), PsyINFO (1860 – January 2012), and Google Scholar (up to January 2012). Our initial search included the following terms related to FSSs: fibromyalgia, chronic widespread pain, chronic fatigue syndrome, temporomandibular disorder, and irritable bowel syndrome, in combination with the following terms related to trauma: abuse, victimization, posttraumatic stress, and PTSD. The Medical Subject Headings (MeSH terms) were also included to obtain the maximum number of studies. All possible combinations of the keywords were entered into each database. Bibliographies of relevant articles were perused for other potentially relevant articles. The abstracts of all identified articles were screened to determine if they were consistent with the inclusion and exclusion criteria.
Inclusion Criteria
Traumatic events included abuse of a psychological, emotional, sexual, or physical nature sustained during childhood or adulthood; combat exposure; and undifferentiated abuse (i.e., type of abuse was unspecified). PTSD was also included since it requires exposure to a traumatic event. To be included, a study was required to include primary data, and to have a control or comparison group. No restrictions were placed on publication dates, participant age, or gender; however, results were limited to studies published in English and research conducted on human beings.
Exclusion Criteria
Articles were excluded for the following reasons: no control or comparison group; focus on symptoms only (e.g., chronic pelvic pain); comparison of two FSSs to each other; lack of data relevant to the meta-analysis; inadequate description of the FSS; inadequate description of trauma, even if undifferentiated; lack of response on missing data from author; or did not meet inclusion criteria listed above. For multiple articles published based on the same sample, only the study with the largest number of participants was included.
Study Coding
Each study was independently coded by 3 to 5 raters, with differences resolved via group consensus. Each article was coded for: sample size; number of participants broken down by gender, ethnicity, clinical condition(s) and control group(s); sample type (e.g., community-based, clinically-based, etc.); study design (retrospective, prospective); type of trauma; type of trauma assessment (e.g., structured interview, validated questionnaire); type of FSS; type of FSS assessment (clinician examination or interview, self-report); age at time of trauma (childhood, adulthood); and statistics reported for variables of interest. For type of FSS assessment, physician and tender point examinations and interviews were considered distinct from self-report questionnaires on medical history. When case-control data were reported, odd ratios (OR) were calculated; however, if adjusted ORs were reported in the article, those data were used for the meta-analysis.
For the overall analysis, independent and dependent groups were classified as follows: FSSs (i.e., FM, CWP, CFS, TMD, or IBS); no unexplained clinical condition (e.g., healthy, no-IBS); other clinical condition (e.g., Crohn’s, dyspepsia); trauma (i.e., PTSD, combat, or abuse); and no trauma. In order to avoid overlap between multiple types of abuse within studies, either the category of ‘any abuse’ was selected or, if this was not available, the subgroup of abuse type with the largest number of participants was selected for the overall analysis. In the rare instance that an article compared two FSSs of interest to a comparison group, we focused on the FSS most objectively assessed and/or with the largest sample size. If data for more than one comparison group were provided and the groups were similar to each other (e.g., rheumatoid arthritis and soft tissue rheumatic disorder) they were combined. If the comparison groups were not similar to each other, then the most relevant group was chosen based on group consensus (e.g., of somatoform disorder and medically explained chronic pain, the medically explained chronic pain group was chosen).
Quality Assessment
Two independent raters assessed the quality of the studies using the Newcastle-Ottawa Scale (NOS) [29]. Disagreements were resolved by mediation between the raters and the first author. NOS provides separate quality assessment instructions for case-control studies and cohort studies. Each type of study can be awarded a maximum of 9 points distributed between 8 questions that address the selection of study groups; the comparability of the groups; and the ascertainment of either the exposure or outcome of interest for case-control or cohort studies, respectively.
Statistical Analysis
Data were analyzed using Comprehensive Meta-Analysis, version 2.0 software [30]. ORs were pooled for outcomes from each study with the DerSimonian-Laird random effects model. The 95% confidence interval (CI) for each outcome was estimated to reflect the uncertainty of point estimates. An OR of 1.0 indicates no association and an OR greater than 1.0 indicates increased risk for the outcome. The I2 statistic was used to estimate the extent of the heterogeneity in the pooled OR indexing the overall association of reported trauma with FSSs. The I2 index provides the percent of variability in the overall effect estimate that is due to true heterogeneity (e.g., differences in study design or participant characteristics) rather than sampling error within studies. I2 values of about 25%, 50%, and 75% represent low, moderate, and high heterogeneity, respectively [31]. Potential causes of heterogeneity in a meta-analysis can be explored by identifying study-level characteristics that may be associated with the variability in study results [32].
Planned subgroup analyses (for categorical variables) and meta-regression (for continuous variables) were used to examine possible sources of heterogeneity. The analytic software can separate studies into subgroups according to study-level variables and then use weighted ANOVA to run the meta-analysis within groups and compare the effect across groups. All relevant comparisons made by the studies were included in subgroup analyses; therefore the n for subgroup analyses may be larger than the total number of studies. To evaluate heterogeneity, the Q test was used. Under the null hypothesis of no heterogeneity, the Q test follows a X2 distribution with k−1 degrees of freedom (where k is the number of studies). A potential cause of heterogeneity is identified when there is considerable between-subgroup variation as indicated by a significant Q test. Locating sources of heterogeneity is analogous to identifying moderators associated with the results of studies. The predefined subgroup analyses included gender, type of trauma including PTSD, type of FSS, type of trauma assessment, type of FSS assessment, age at time of trauma, and sample type. Planned meta-regression evaluated whether study quality affected the overall effect size. P values < 0.05 were considered significant for all analyses.
To address the issue of publication bias (i.e., studies with non-significant findings are less likely to be published than studies with significant results), the classic Fail-Safe N (FSN) was calculated to determine how many null studies would need to be included in the meta-analysis to nullify the reported overall effect size for the association. A FSN that is greater than or equal to five times the number of studies in the analysis plus 10 (FSN ≥ 5k +10) is indicative of an effect size that is robust against publication bias [33].
RESULTS
Overview of Search
Literature searches resulted in 3,166 potentially eligible articles. Initial screening of abstracts found that 2,910 articles did not meet the inclusion criteria or were not relevant. Thus, 256 articles were closely examined by 3 to 5 raters, and 71 (28%) of these fulfilled all inclusion criteria; these articles are presented in the Appendix. Articles were excluded for various reasons: 80 did not present explicit data on any of the FSSs under review; 13 had no trauma variable; 39 had no control group or did not provide adequate information; 5 were not experiments (e.g., letters to the editor); 3 were used as reference papers to obtain demographic information for relevant articles; 19 were excluded for other reasons (e.g., both reported trauma and FSS were present but their relationship was not examined); and 26 were review articles or other resource materials that were used for background information only.
Study Characteristics
Of the 71 included studies, 70% used some form of abuse as the trauma variable while 23% used PTSD, and 6% used combat/deployment. Only one study presented separate analyses examining the relationship between the FSS and both PTSD and reported abuse. Trauma assessments included structured interviews (14%), semi-structured interviews (1%), unstructured interviews (3%), validated questionnaires (39%), non-validated questionnaires (27%), and self-report (15%). Twenty five studies focused on FM or CWP, 15 on CFS, 3 on TMD, and 28 on IBS. The majority of the studies used physician examination or interview (72%) to diagnose FSSs.
Twenty eight percent of the studies were published in the 1990s and 72% were published since 2000; all, except one, were retrospective. Thirty six publications (51%) reported on clinical samples, 19 (27%) used community-based samples, and the remaining 16 (22%) were classified as other (e.g., veterans, volunteers, etc.). The sample sizes ranged from 26 to 20,917 participants [34, 35]. With respect to gender, 49% of the articles presented data on a combination of male and female participants, 39% reported on female samples only, 6% reported on male samples only, and 6% reported separate analyses for some combination of these. Not enough studies presented data on age, race/ethnicity, or length of illness to report here.
Overall Meta-Analysis
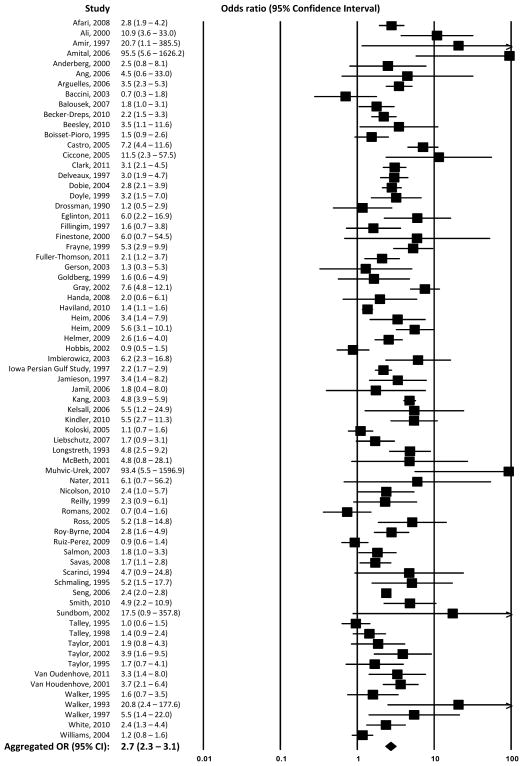
Figure 1 presents the independent and aggregated association(s) of reported trauma and FSSs for the 71 included studies. The aggregated random effects analysis revealed that individuals reporting exposure to trauma were 2.7 times more likely to have FSS (OR (95% CI) = 2.7 (2.27 – 3.10); n = 71). The FSN statistic indicated that another 1,537 null studies would need to be included to change the 2-tailed p-value from 0.00 to > 0.05; thus, the obtained OR can be considered robust against publication bias [33]. There was substantial heterogeneity in the studies (X2 = 325.86, df = 70, p < 0.001), confirming our a priori decision to use random effects models. The obtained I2 statistic indicated that 78.5% of the variability among the overall effect size was due to true heterogeneity between the studies rather than sampling error.
Figure 1.
Forest plot for the aggregated and independent associations of reported trauma and functional somatic syndromes
Subgroup Analyses for Gender
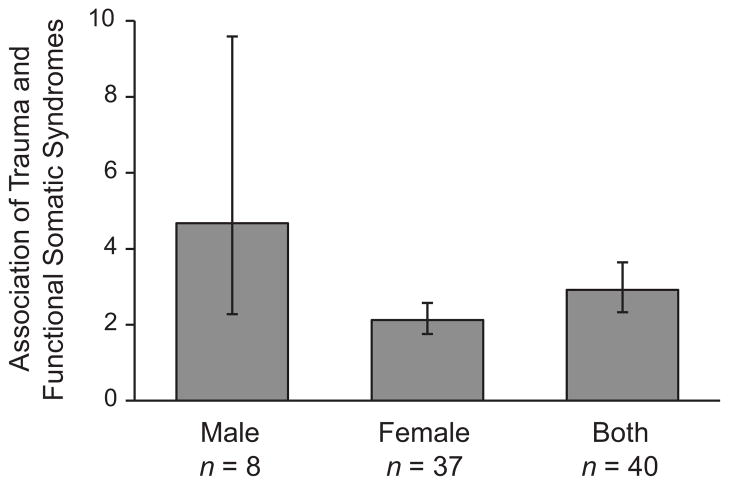
Figure 2 depicts gender effects in the relationship between reported trauma and FSSs. Initial comparisons revealed that the overall association between reported trauma and FSSs was more than twice as strong for males than females (male OR (95% CI) = 4.68 (2.28 – 9.59), n = 8; female OR (95% CI) = 2.13 (1.76 – 2.57), n = 37; X2 = 4.31, df = 1, p = 0.038). However, as a conservative effort, three studies with outlier results [34, 36, 37] were excluded and the gender difference, although still present was no longer significant as a moderating variable (male OR (95% CI) = 3.29 (1.89 – 5.71), n = 6; female OR (95% CI) = 2.11 (1.74 – 2.55), n = 36; X2 = 2.20, df = 1, p = 0.138).
Figure 2.
Odd ratios and 95% confidence intervals for the association of reported trauma and functional somatic syndromes by articles using male-only, female-only, and both gender samples
n = Number of articles
Subgroup Analyses for Type of Trauma and FSS
Subgroup analyses identified type of trauma as a moderating variable (X2 = 12.76, df = 4, p = 0.013). Studies of PTSD showed significantly larger associations than studies of sexual abuse (X2 = 8.51, df = 1, p = 0.004) or physical abuse (X2 = 9.77, df = 1, p = 0.002). The top half of Table 1 presents the associations of reported trauma with FSSs separately for each type of trauma. Combat exposure had the largest association with FSSs but this was based on only 9 studies; physical abuse had the smallest association with 49 studies.
Table 1.
Associations of reported trauma and functional somatic syndromes presented separately by type of trauma and type of condition **
| OR | 95% CI | z-Value | p-Value | k | |
|---|---|---|---|---|---|
| Trauma† | |||||
| Emotional Abuse | 2.11 | 1.58 – 2.82 | 5.06 | <0.001 | 23 |
| Physical Abuse | 1.89 | 1.58 – 2.26 | 6.89 | <0.001 | 49 |
| Sexual Abuse | 2.01 | 1.74 – 2.32 | 9.41 | <0.001 | 69 |
| Combat/Deployment | 3.06 | 1.72 – 5.47 | 3.79 | <0.001 | 9 |
| PTSD* | 2.93 | 2.38 – 3.61 | 10.13 | <0.001 | 20 |
| Functional Somatic Syndrome‡ | |||||
| FM | 2.52 | 1.92 – 3.31 | 6.62 | <0.001 | 21 |
| CWP | 3.35 | 2.55 – 4.41 | 8.65 | <0.001 | 5 |
| CFS | 4.06 | 3.18 – 5.18 | 11.20 | <0.001 | 14 |
| TMD | 3.33 | 1.15 – 9.68 | 2.21 | 0.027 | 3 |
| IBS | 2.22 | 1.72 – 2.86 | 6.16 | <0.001 | 29 |
Subgroup analyses use weighted ANOVA to run the meta-analysis within groups and compare the effect across groups.
Associations compare those who were exposed to the trauma with those who were not.
Associations compare those who had the FSS with those who did not.
Muhvic-Urek 2007 and one of the comparisons made by Amital 2006 were considered outliers and thus were not used in this analysis.
OR = odds ratio; CI = confidence interval; k = number of relevant comparisons; PTSD = posttraumatic stress disorder; FM = fibromyalgia; CWP = chronic widespread pain; CFS = chronic fatigue syndrome; TMD = temporomandibular disorder; IBS = irritable bowel syndrome.
Subgroup analyses confirmed type of FSS as a moderator (X2 = 13.49, df = 4, p = 0.009) and identified significant differences between CFS and IBS (X2 = 11.24, df = 1, p = 0.001) and CFS and FM (X2 = 6.48, df = 1, p = 0.011). The bottom half of Table 1 presents the associations of reported trauma with FSSs for each type of FSS. CFS had the largest association with reported trauma with 14 studies and IBS was least likely to be associated with reported trauma in 29 studies.
Other Subgroup Analyses
The type of trauma assessment also was a moderating variable in the association of reported trauma and FSSs (X2 = 15.12, df = 3, p = 0.002). Studies using non-validated questionnaires reported larger associations than studies that used validated questionnaires (non-validated OR (95% CI) = 2.68 (2.26 – 3. 16), n = 70; validated OR (95% CI) = 1.80 (1.55 –2.09), n = 82; X2 = 12.08, df = 1, p = 0.001). Studies using self-report of trauma also reported larger associations than those using validated questionnaires (self-report OR (95% CI) = 2.75 (2.12 – 3.56), n = 35; X2 = 7.80, df = 1, p = 0.005). There were no differences between studies using validated questionnaires versus using interviews (interview OR (95% CI) = 2.31 (1.71 –3.11), n = 30; X2 = 2.15, df = 1, p = 0.143), nor were there significant differences between non-validated questionnaires, self-reports of trauma, and interviews. Type of FSS assessment (clinician assessment or interview OR (95% CI) = 2.69 (2.21 – 3.26), n = 50; self-report OR (95% CI) = 2.68 (2.03 – 3.54), n = 21; X2 = 0.00, df = 1, p = 0.987), age at the time of trauma (childhood abuse OR (95% CI) = 1.97 (1.72 – 2.25), n = 83; adulthood abuse OR (95% CI) = 1.91 (1.58 – 2.31), n = 52; X2 = 0.06, df = 1, p = 0.805), and sample type (clinical OR (95% CI) = 2.60 (2.10 – 3.23), n = 36; community OR (95% CI) = 2.32 (1.81 – 2.98), n = 19; other sample OR (95% CI) = 3.25 (2.24 – 4.70), n = 16; X2 = 2.19, df = 2, p = 0.335), were not significant moderators of the association between reported trauma and FSSs.
Quality Assessment
Of the 58 case-control studies, 21 (36%) received 0–3 points out of a possible 9 points, 32 (55%) were given 4–6 points, and only 5 (9%) were awarded 7 points. Of the 13 cohort studies, 3 (23%) received 0–3 points, 8 (62%) had 4–6 points, and 2 (15%) earned 7 points. No articles from either study design earned more than 7 points. Within the three subcategories of quality assessment, case-control studies needed the most improvement in their description of the exposure variable (i.e., 81% received only 1 of 3 possible points) while cohort studies needed to improve their selection of the study groups (69% received only 2 of 4 possible points). Meta-regression analyses indicated that the overall methodological quality was not a significant source of heterogeneity (Q = 81.18, df = 70, p = 0.170). Results were similar when the quality of case-control (case-control Q = 12.97, df = 12, p = 0.371) and cohort studies were examined separately (cohort Q = 68.57, df = 57, p = 0.140).
DISCUSSION
To our knowledge, this is the largest and most comprehensive review of the trauma and FSSs literature to date. We found 71 studies that met our stringent criteria for inclusion. The overall meta-analysis revealed that individuals who reported exposure to trauma were 2.7 times more likely to have FSS regardless of type of trauma or type of condition. This significant association was robust against both publication bias and the generally low quality of the literature. Type of trauma, type of FSS, and type of trauma assessment were moderators of the association between trauma and FSSs. The association between reported trauma and FSSs was more than twice as strong in men than women; however, our conservative effort of removing studies with outlier results rendered this difference non-significant. Type of FSS assessment, age at the time of trauma, and type of sample did not moderate the relationship between reported trauma and FSSs.
Combat exposure and PTSD had the strongest association with FSSs. Several studies have shown that military veterans with combat exposure and subsequent PTSD may be more likely to have experienced previous childhood or adulthood traumas as well [38, 39]. Thus, it is possible that the large association of combat exposure with FSSs may reflect the effect of multiple traumas or unreported PTSD. Since the meta-analysis only included a few studies that examined combat exposure and none had information on prior trauma exposure, this finding should be interpreted with caution. The effect size for PTSD was significantly larger than the effect size of sexual or physical abuse, possibly illustrating the nature of developing PTSD in response to trauma and its potential impact on health. While a person exposed to trauma may or may not have a maladaptive long-term response, an individual who develops PTSD will likely have several behavioral and psychological consequences as well as greater possible dysregulation of physiological systems that further limit one’s recovery and can potentially foster the development of FSSs.
We also found that studies using non-validated questionnaires and self-reports of trauma had larger associations between reported trauma and FSSs than studies using validated questionnaires. This finding is consistent with the previous meta-analysis that examined the association of PTSD with physical health symptoms [27]. It is possible that the format of the trauma assessment may influence how one responds to questions about trauma exposure. For example, using retrospective self-report is potentially problematic as it is often subject to recall and response bias. Previous studies have found variability in documenting abuse, specifically indicating that adults who are administered questionnaires or interviews often underreport childhood abuse [40].
The magnitude of the association between reported trauma and CFS was significantly larger than that of FM or IBS. Given the uncertain etiology of these conditions, the reasons why CFS showed a stronger relationship with trauma is unclear. Any existing differences in the underlying etiology and pathophysiology of FSSs may contribute to variability in the physiological, emotional, and psychological responses that accompany each condition. Thus, these findings illustrate the importance of examining both the similarities of these conditions as well as their differences.
Proposed Explanations
It is widely recognized that a set of physiological and psychological processes become enacted when humans experience acute stress or trauma [16]. For many people, these physiological perturbations return to baseline once the stress or trauma has resolved. However, the initial state of hyperarousal can become chronic for some individuals [14, 15, 41]. The chronic hyperarousal then leads to dysregulation of the physiologic stress system and the ultimate development of stress-related conditions. Consistent with cognitive behavior theory, the experience of trauma also may impact one’s appraisals of potentially threatening stimuli including physical and physiological symptoms. This appraisal bias may then lead to increased avoidance, catastrophizing about symptoms, and amplification of the illness experience [42]. One’s expectation of further somatic symptoms also can play a role in perpetuating a cycle of further decline in functioning. For example, an individual with FM may experience significant anticipatory anxiety associated with the likelihood of future pain which may cause him to isolate or limit his activity level, potentially leading to higher pain susceptibility and poorer psychosocial functioning.
When trauma leads to the development of PTSD, the link between trauma exposure and FSS may be even more pronounced. Several theoretical models attempt to explain the link between trauma with resulting PTSD and pain. The mutual maintenance theory explicates that the high comorbidity between PTSD and pain including FSSs can be due to mechanisms that are common to both sets of conditions, including attentional bias toward threatening stimuli, anxiety sensitivity, reminders of the trauma that may be pain-related and trigger PTSD symptoms, behavioral avoidance, depression, and reduction of physical activity [23]. The shared vulnerability model proposes that shared individual difference factors, such as anxiety sensitivity and sympathetic dysregulation, influence the development of both PTSD and pain conditions, such as FSSs, in response to traumatic experiences [24]. The multiplex model of bodily experience, which has been mostly applied to traumatized refugees, explains how distress along four distinct fear networks may serve as significant mediators of the link between somatic symptoms and PTSD severity [25]. Finally, the perpetual avoidance model asserts that dysfunctional cognitive processing following trauma can lead to an increase in psychological and physiological arousal and therefore greater behavioral avoidance that maintains both PTSD and pain [26]. The relationship between trauma, PTSD, and pain conditions including FSSs is complex and likely involves many of the proposed mechanisms. However, there is a dearth of research to either support or refute any of these models. Therefore, future hypothesis-driven studies should systematically examine the mechanisms underlying the relationship between psychological trauma, PTSD, and FSSs to better inform treatment and prevention of these conditions.
Limitations of the Literature
Our findings are limited primarily based on the nature of the literature that was used. The most notable limitation is that nearly all the studies were cross-sectional. Thus, no assumptions about directionality of the effects can be made until more prospective studies are conducted. Further, the overall quality of the studies was generally low. Since a meta-analysis is based on a summation of studies, the results are only as good as the studies combined to make up the meta-analysis. The poor quality of the literature also may have played a role in the detection of an association between trauma and FSSs since we found that the magnitude of the association between trauma and FSSs was larger in studies using non-validated questionnaires and self-report rather than those using validated questionnaires for trauma assessment. Thus, inaccurate or false reports of trauma history are of primary concern in this and other studies [43–45].
The studies were also notable for what was not reported. None of the studies reported on the possible co-occurrence of psychological trauma with physical trauma, which may account for the link between trauma and FSSs. Additionally, only a handful of the studies examined the confounding effects of depression or other psychiatric conditions, precluding us from conducting a formal subgroup analysis to further examine this in the meta-analysis. Given the frequent comorbidity of both PTSD and FSSs with psychiatric conditions [7], examining the role of depression, for example, in the link between trauma and FSSs is worthy of consideration. Despite the known comorbidity among FSSs [8], practically none of the studies provided information on the presence or absence of more than one syndrome. Therefore, the effect sizes for conditions may have been inflated by existing but unmeasured high comorbidity between FSSs. Differential diagnosis is often problematic among FSSs, as several of these conditions share a common set of symptoms. Some even argue that differentiation of a specific FSS reflects the inclination of specialists to focus on only symptoms relevant to their specialty, rather than any real differences between patients [4]. For example, a researcher studying FM may choose to identify symptoms associated with that specific condition and not include measures to detect other conditions such as IBS or CFS. To further complicate the issue, small variations in the diagnostic criteria can produce wide variations in prevalence rates. For example, the ICD-10, diagnostic criteria for CFS requires persistent or relapsing fatigue of 6 or more consecutive months, chronic wide spread pain of at least 3 months for FM, and recurrent abdominal pain or discomfort of at least 3 days per month during the previous 3 months for IBS [46]. Such inconsistencies create several clinical, conceptual, and empirical challenges in examining the similarities and differences among FSSs.
Future Directions
Our findings can help to inform future research to address the complex nature of FSSs and how prior trauma experience may play a role in the etiology and maintenance of such conditions. It is fundamental that future studies address the inconsistent diagnostic issues within the FSSs literature in order to achieve a more comprehensive understanding of how to classify and study these conditions. More studies of comorbidities are needed to better understand similarities as well as the differences across these syndromes. There is also a need to systematically improve the methods used to assess for trauma exposure, perhaps through longitudinal studies, to refine our measurement of self-reported trauma.
Longitudinal and prospective studies that examine risk factors, temporal onset, and prognosis of FSSs are necessary to gain a better understanding of FSSs and how trauma may perpetuate such diagnoses. The findings related to gender also merit some consideration. Because the majority of the literature has focused on women, it was unexpected to see that the association between trauma and FSSs was initially stronger in men than women. Although the gender effect weakened once outlier results were controlled, this lends support for further exploration of the role of gender in the relationship between trauma and FSSs, particularly in the context of combat-related trauma.
Given that the magnitude of the association between reported trauma and FSSs differed depending on the type of trauma, type of FSS, and type of trauma assessment, future studies should attempt to identify the function of such variables on the trauma and FSS relationship. These types of studies can promote a better understanding of the pathophysiological mechanism that underlie these conditions, as well as inform assessment and treatment approaches. Moreover, studying individuals who have experienced trauma but do not have FSSs would provide a better understanding of protective factors, and thus would be particularly valuable to prevention work. Finally, to better address both the psychological consequences of trauma as well as overall functioning related to FSSs, more attention needs to be given to intervention research that is transdiagnostic in nature. This would require an understanding outside the conceptual structure of diagnosis by identifying common factors that affect the development and maintenance of cognitive, emotional, and behavioral features that characterize these conditions.
Conclusions
In summary, the current meta-analysis revealed a significant association between reported trauma and FSSs. We also found that the association between trauma and FSSs differed according to type of trauma, type of FSS, and type of trauma assessment. Our findings were robust against publication bias and were not significantly affected by the generally low-quality of the studies. Nonetheless, the findings should be interpreted with caution in light of the many limitations of the studies used. These findings also emphasize the importance of conducting prospective studies, further examining the potential similarities and differences of these conditions, and pursuing hypothesis-driven studies of the mechanisms underlying the link between trauma, PTSD, and FSSs. Finally, further research is necessary to develop and test the efficacy of treatments that can address the common factors in these conditions.
Supplementary Material
Acknowledgments
Source of Funding: This material is based upon work supported by the Department of Veterans Affairs Center of Excellence for Stress and Mental Health. This material also is the result of work supported with resources of the VA San Diego Healthcare System. Dr. Afari is also supported in part by NIH grants U01DK082325 and R03NR012841, and VA RR&D grant F7400R. Dr. Gundy is also supported in part by VA RR&D grant F7400R. This work was also supported in part by a predoctoral fellowship awarded to Sandra M. Ahumada by the NIMH (2T32MH15755-34). The views expressed in this paper are those of the authors and do not reflect the official policy or position of the Department of Veteran’s Affairs or any of the institutions with which the authors are affiliated.
Glossary
- FSS
functional somatic syndrome
- FM
fibromyalgia
- CWP
chronic widespread pain
- CFS
chronic fatigue syndrome
- TMD
temporomandibular disorder
- IBS
irritable bowel syndrome
- PTSD
posttraumatic stress disorder
- OR
odds ratio
- CI
confidence interval
- NOS
Newcastle-Ottawa Scale
- FSN
Fail-Safe N
APPENDIX
Reviewed Articles
- 1.Afari N, Wen Y, Buchwald D, Goldberg J, Plesh O. Are post-traumatic stress disorder symptoms and temporomandibular pain associated? Findings from a community-based twin registry. J Orofac Pain. 2008;22:41–9. [PMC free article] [PubMed] [Google Scholar]
- 2.Ali A, Toner BB, Stuckless N, Gallop R, Diamant NE, Gould MI, Vidins EI. Emotional abuse, self-blame, and self-silencing in women with irritable bowel syndrome. Psychosom Med. 2000;62:76–82. doi: 10.1097/00006842-200001000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Amir M, Kaplan Z, Neumann L, Sharabani R, Shani N, Buskila D. Posttraumatic stress disorder, tenderness and fibromyalgia. J Psychosom Res. 1997;42:607–13. doi: 10.1016/s0022-3999(97)00009-3. [DOI] [PubMed] [Google Scholar]
- 4.Amital D, Fostick L, Polliack ML, Segev S, Zohar J, Rubinow A, Amital H. Posttraumatic stress disorder, tenderness, and fibromyalgia syndrome: are they different entities? J Psychosom Res. 2006;61:663–9. doi: 10.1016/j.jpsychores.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Anderberg UM, Marteinsdottir I, Theorell T, von Knorring L. The impact of life events in female patients with fibromyalgia and in female healthy controls. Eur Psychiatry. 2000;15:295–301. doi: 10.1016/s0924-9338(00)00397-7. [DOI] [PubMed] [Google Scholar]
- 6.Ang DC, Peloso PM, Woolson RF, Kroenke K, Doebbeling BN. Predictors of incident chronic widespread pain among veterans following the first Gulf War. Clin J Pain. 2006;22:554–63. doi: 10.1097/01.ajp.0000208907.42506.21. [DOI] [PubMed] [Google Scholar]
- 7.Arguelles LM, Afari N, Buchwald DS, Clauw DJ, Furner S, Goldberg J. A twin study of posttraumatic stress disorder symptoms and chronic widespread pain. Pain. 2006;124:150–7. doi: 10.1016/j.pain.2006.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baccini F, Pallotta N, Calabrese E, Pezzotti P, Corazziari E. Prevalence of sexual and physical abuse and its relationship with symptom manifestations in patients with chronic organic and functional gastrointestinal disorders. Digestive and Liver Disease. 2003;35:256–61. doi: 10.1016/s1590-8658(03)00075-6. [DOI] [PubMed] [Google Scholar]
- 9.Balousek S, Plane MB, Fleming M. Prevalence of interpersonal abuse in primary care patients prescribed opioids for chronic pain. J Gen Intern Med. 2007;22:1268–73. doi: 10.1007/s11606-007-0257-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Becker-Dreps S, Morgan D, Pena R, Cortes L, Martin CF, Valladares E. Association between intimate partner violence and irritable bowel syndrome: a population-based study in Nicaragua. Violence Against Women. 2010;16:832–45. doi: 10.1177/1077801210374816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beesley H, Rhodes J, Salmon P. Anger and childhood sexual abuse are independently associated with irritable bowel syndrome. Br J Health Psychol. 2010;15:389–99. doi: 10.1348/135910709X466496. [DOI] [PubMed] [Google Scholar]
- 12.Boisset-Pioro MH, Esdaile JM, Fitzcharles MA. Sexual and physical abuse in women with fibromyalgia syndrome. Arthritis Rheum. 1995;38:235–41. doi: 10.1002/art.1780380212. [DOI] [PubMed] [Google Scholar]
- 13.Castro I, Barrantes F, Tuna M, Cabrera G, Garcia C, Recinos M, Espinoza LR, Garcia-Kutzbach A. Prevalence of abuse in fibromyalgia and other rheumatic disorders at a specialized clinic in rheumatic diseases in Guatemala City. J Clin Rheumatol. 2005;11:140–5. doi: 10.1097/01.rhu.0000164823.78761.a2. [DOI] [PubMed] [Google Scholar]
- 14.Ciccone DS, Elliott DK, Chandler HK, Nayak S, Raphael KG. Sexual and Physical Abuse in Women With Fibromyalgia Syndrome: A Test of the Trauma Hypothesis. The Clinical Journal of Pain. 2005;21:378–86. doi: 10.1097/01.ajp.0000149796.08746.ea. [DOI] [PubMed] [Google Scholar]
- 15.Clark C, Goodwin L, Stansfeld SA, Hotopf M, White PD. Premorbid risk markers for chronic fatigue syndrome in the 1958 British birth cohort. Br J Psychiatry. 2011;199:323–9. doi: 10.1192/bjp.bp.110.083956. [DOI] [PubMed] [Google Scholar]
- 16.Delvaux M, Denis P, Allemand H. Sexual abuse is more frequently reported by IBS patients than by patients with organic digestive diseases or controls. Results of a multicentre inquiry. French Club of Digestive Motility. Eur J Gastroenterol Hepatol. 1997;9:345–52. doi: 10.1097/00042737-199704000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Dobie DJ, Kivlahan DR, Maynard C, Bush KR, Davis TM, Bradley KA. Posttraumatic stress disorder in female veterans: association with self-reported health problems and functional impairment. Arch Intern Med. 2004;164:394–400. doi: 10.1001/archinte.164.4.394. [DOI] [PubMed] [Google Scholar]
- 18.Doyle JP, Frank E, Saltzman LE, McMahon PM, Fielding BD. Domestic violence and sexual abuse in women physicians: associated medical, psychiatric, and professional difficulties. J Womens Health Gend Based Med. 1999;8:955–65. doi: 10.1089/jwh.1.1999.8.955. [DOI] [PubMed] [Google Scholar]
- 19.Drossman DA, Leserman J, Nachman G, Li ZM, Gluck H, Toomey TC, Mitchell CM. Sexual and physical abuse in women with functional or organic gastrointestinal disorders. Ann Intern Med. 1990;113:828–33. doi: 10.7326/0003-4819-113-11-828. [DOI] [PubMed] [Google Scholar]
- 20.Eglinton R, Chung MC. The relationship between posttraumatic stress disorder, illness cognitions, defence styles, fatigue severity and psychological well-being in chronic fatigue syndrome. Psychiatry Res. 2011;188:245–52. doi: 10.1016/j.psychres.2011.04.012. [DOI] [PubMed] [Google Scholar]
- 21.Fillingim RB, Maixner W, Sigurdsson A, Kincaid S. Sexual and physical abuse history in subjects with temporomandibular disorders: relationship to clinical variables, pain sensitivity, and psychologic factors. J Orofac Pain. 1997;11:48–57. [PubMed] [Google Scholar]
- 22.Finestone HM, Stenn P, Davies F, Stalker C, Fry R, Koumanis J. Chronic pain and health care utilization in women with a history of childhood sexual abuse. Child Abuse Negl. 2000;24:547–56. doi: 10.1016/s0145-2134(00)00112-5. [DOI] [PubMed] [Google Scholar]
- 23.Frayne SM, Skinner KM, Sullivan LM, Tripp TJ, Hankin CS, Kressin NR, Miller DR. Medical profile of women Veterans Administration outpatients who report a history of sexual assault occurring while in the military. J Womens Health Gend Based Med. 1999;8:835–45. doi: 10.1089/152460999319156. [DOI] [PubMed] [Google Scholar]
- 24.Fuller-Thomson E, Sulman J, Brennenstuhl S, Merchant M. Functional Somatic Syndromes and Childhood Physical Abuse in Women: Data From a Representative Community-Based Sample. Journal of Aggression, Maltreatment & Trauma. 2011;20:445–69. [Google Scholar]
- 25.Gerson A, Fox D. Fibromyalgia revisited: Axis II factors in MMPI and historial data in compensation claimants. American Journal of Forensic Psychology. 2003;21:21–5. [Google Scholar]
- 26.Goldberg RT, Pachas WN, Keith D. Relationship between traumatic events in childhood and chronic pain. Disabil Rehabil. 1999;21:23–30. doi: 10.1080/096382899298061. [DOI] [PubMed] [Google Scholar]
- 27.Gray GC, Reed RJ, Kaiser KS, Smith TC, Gastanaga VM. Self-reported symptoms and medical conditions among 11,868 Gulf War-era veterans: the Seabee Health Study. Am J Epidemiol. 2002;155:1033–44. doi: 10.1093/aje/155.11.1033. [DOI] [PubMed] [Google Scholar]
- 28.Handa M, Nukina H, Hosoi M, Kubo C. Childhood physical abuse in outpatients with psychosomatic symptoms. Biopsychosoc Med. 2008;2:8. doi: 10.1186/1751-0759-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haviland MG, Morton KR, Oda K, Fraser GE. Traumatic experiences, major life stressors, and self-reporting a physician-given fibromyalgia diagnosis. Psychiatry Res. 2010;177:335–41. doi: 10.1016/j.psychres.2009.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Heim C, Nater UM, Maloney E, Boneva R, Jones JF, Reeves WC. Childhood trauma and risk for chronic fatigue syndrome: association with neuroendocrine dysfunction. Arch Gen Psychiatry. 2009;66:72–80. doi: 10.1001/archgenpsychiatry.2008.508. [DOI] [PubMed] [Google Scholar]
- 31.Heim C, Wagner D, Maloney E, Papanicolaou DA, Solomon L, Jones JF, Unger ER, Reeves WC. Early adverse experience and risk for chronic fatigue syndrome: results from a population-based study. Arch Gen Psychiatry. 2006;63:1258–66. doi: 10.1001/archpsyc.63.11.1258. [DOI] [PubMed] [Google Scholar]
- 32.Helmer DA, Chandler HK, Quigley KS, Blatt M, Teichman R, Lange G. Chronic widespread pain, mental health, and physical role function in OEF/OIF veterans. Pain Med. 2009;10:1174–82. doi: 10.1111/j.1526-4637.2009.00723.x. [DOI] [PubMed] [Google Scholar]
- 33.Hobbis IC, Turpin G, Read NW. A re-examination of the relationship between abuse experience and functional bowel disorders. Scand J Gastroenterol. 2002;37:423–30. doi: 10.1080/003655202317316051. [DOI] [PubMed] [Google Scholar]
- 34.Imbierowicz K, Egle UT. Childhood adversities in patients with fibromyalgia and somatoform pain disorder. Eur J Pain. 2003;7:113–9. doi: 10.1016/S1090-3801(02)00072-1. [DOI] [PubMed] [Google Scholar]
- 35.Iowa_Persian_Gulf_Study_Group. Self-reported illness and health status among Gulf War veterans. A population-based study. The Iowa Persian Gulf Study Group. JAMA. 1997;277:238–45. [PubMed] [Google Scholar]
- 36.Jamieson DJ, Steege JF. The association of sexual abuse with pelvic pain complaints in a primary care population. Am J Obstet Gynecol. 1997;177:1408–12. doi: 10.1016/s0002-9378(97)70083-8. [DOI] [PubMed] [Google Scholar]
- 37.Jamil H, Nassar-McMillan SC, Salman WA, Tahar M, Jamil LH. Iraqi Gulf War veteran refugees in the U.S.: PTSD and physical symptoms. Soc Work Health Care. 2006;43:85–98. doi: 10.1300/J010v43n04_06. [DOI] [PubMed] [Google Scholar]
- 38.Kang HK, Natelson BH, Mahan CM, Lee KY, Murphy FM. Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: a population-based survey of 30,000 veterans. Am J Epidemiol. 2003;157:141–8. doi: 10.1093/aje/kwf187. [DOI] [PubMed] [Google Scholar]
- 39.Kelsall H, Sim M, McKenzie D, Forbes A, Leder K, Glass D, Ikin J, McFarlane A. Medically evaluated psychological and physical health of Australian Gulf War veterans with chronic fatigue. J Psychosom Res. 2006;60:575–84. doi: 10.1016/j.jpsychores.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 40.Kindler LL, Jones KD, Perrin N, Bennett RM. Risk factors predicting the development of widespread pain from chronic back or neck pain. J Pain. 2010;11:1320–8. doi: 10.1016/j.jpain.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Koloski NA, Talley NJ, Boyce PM. A history of abuse in community subjects with irritable bowel syndrome and functional dyspepsia: the role of other psychosocial variables. Digestion. 2005;72:86–96. doi: 10.1159/000087722. [DOI] [PubMed] [Google Scholar]
- 42.Liebschutz J, Saitz R, Brower V, Keane TM, Lloyd-Travaglini C, Averbuch T, Samet JH. PTSD in urban primary care: high prevalence and low physician recognition. J Gen Intern Med. 2007;22:719–26. doi: 10.1007/s11606-007-0161-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Longstreth GF, Wolde-Tsadik G. Irritable bowel-type symptoms in HMO examinees. Prevalence, demographics, and clinical correlates. Dig Dis Sci. 1993;38:1581–9. doi: 10.1007/BF01303163. [DOI] [PubMed] [Google Scholar]
- 44.McBeth J, Morris S, Benjamin S, Silman AJ, Macfarlane GJ. Associations between adverse events in childhood and chronic widespread pain in adulthood: are they explained by differential recall? J Rheumatol. 2001;28:2305–9. [PubMed] [Google Scholar]
- 45.Muhvić-Urek M, Uhac I, Vuksić-Mihaljević Z, Leović D, Blecić N, Kovac Z. Oral health status in war veterans with post-traumatic stress disorder. J Oral Rehabil. 2007;34:1–8. doi: 10.1111/j.1365-2842.2006.01674.x. [DOI] [PubMed] [Google Scholar]
- 46.Nater UM, Maloney E, Heim C, Reeves WC. Cumulative life stress in chronic fatigue syndrome. Psychiatry Res. 2011;189:318–20. doi: 10.1016/j.psychres.2011.07.015. [DOI] [PubMed] [Google Scholar]
- 47.Nicolson NA, Davis MC, Kruszewski D, Zautra AJ. Childhood maltreatment and diurnal cortisol patterns in women with chronic pain. Psychosom Med. 2010;72:471–80. doi: 10.1097/PSY.0b013e3181d9a104. [DOI] [PubMed] [Google Scholar]
- 48.Reilly J, Baker GA, Rhodes J, Salmon P. The association of sexual and physical abuse with somatization: characteristics of patients presenting with irritable bowel syndrome and non-epileptic attack disorder. Psychol Med. 1999;29:399–406. doi: 10.1017/s0033291798007892. [DOI] [PubMed] [Google Scholar]
- 49.Romans S, Belaise C, Martin J, Morris E, Raffi A. Childhood abuse and later medical disorders in women. An epidemiological study. Psychother Psychosom. 2002;71:141–50. doi: 10.1159/000056281. [DOI] [PubMed] [Google Scholar]
- 50.Ross CA. Long Term Effects of Child Sexual Abuse: Childhood Sexual Abuse and Psychosomatic Symptoms in Irritable Bowel Syndrome. Journal of Child Sexual Abuse. 2005;14:27–38. doi: 10.1300/J070v14n01_02. [DOI] [PubMed] [Google Scholar]
- 51.Roy-Byrne P, Smith WR, Goldberg J, Afari N, Buchwald D. Post-traumatic stress disorder among patients with chronic pain and chronic fatigue. Psychol Med. 2004;34:363–8. doi: 10.1017/s0033291703008894. [DOI] [PubMed] [Google Scholar]
- 52.Ruiz-Perez I, Plazaola-Castano J, Caliz-Caliz R, Rodriguez-Calvo I, Garcia-Sanchez A, Ferrer-Gonzalez MA, Guzman-Ubeda M, del Rio-Lozano M, Lopez-Chicheri Garcia I. Risk factors for fibromyalgia: the role of violence against women. Clin Rheumatol. 2009;28:777–86. doi: 10.1007/s10067-009-1147-6. [DOI] [PubMed] [Google Scholar]
- 53.Salmon P, Skaife K, Rhodes J. Abuse, dissociation, and somatization in irritable bowel syndrome: towards an explanatory model. J Behav Med. 2003;26:1–18. doi: 10.1023/a:1021718304633. [DOI] [PubMed] [Google Scholar]
- 54.Savas LS, White DL, Wieman M, Daci K, Fitzgerald S, Laday Smith S, Tan G, Graham DP, Cully JA, El-Serag HB. Irritable bowel syndrome and dyspepsia among women veterans: prevalence and association with psychological distress. Aliment Pharmacol Ther. 2008 doi: 10.1111/j.1365-2036.2008.03847.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Scarinci IC, McDonald-Haile J, Bradley LA, Richter JE. Altered pain perception and psychosocial features among women with gastrointestinal disorders and history of abuse: a preliminary model. Am J Med. 1994;97:108–18. doi: 10.1016/0002-9343(94)90020-5. [DOI] [PubMed] [Google Scholar]
- 56.Schmaling KB, DiClementi JD. Interpersonal stressors in chronic fatigue syndrome: A pilot study. Journal of Chronic Fatigue Syndrome. 1995;1:153–7. [Google Scholar]
- 57.Seng JS, Clark MK, McCarthy AM, Ronis DL. PTSD and physical comorbidity among women receiving Medicaid: results from service-use data. J Trauma Stress. 2006;19:45–56. doi: 10.1002/jts.20097. [DOI] [PubMed] [Google Scholar]
- 58.Smith BW, Papp ZZ, Tooley EM, Montague EQ, Robinson AE, Cosper CJ. Traumatic events, perceived stress and health in women with fibromyalgia and healthy controls. Stress and Health. 2010;26:83–93. [Google Scholar]
- 59.Sundbom E, Henningsson M, Holm U, Söderbergh S, Evengård B. Possible influence of defenses and negative life events on patients with chronic fatigue syndrome: a pilot study. Psychol Rep. 2002;91:963–78. doi: 10.2466/pr0.2002.91.3.963. [DOI] [PubMed] [Google Scholar]
- 60.Talley NJ, Boyce PM, Jones M. Is the association between irritable bowel syndrome and abuse explained by neuroticism? A population based study. Gut. 1998;42:47–53. doi: 10.1136/gut.42.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Talley NJ, LFS, RZA Self-reported abuse and gastrointestinal disease in outpatients: association with irritable bowel-type symptoms. Am J Gastroenterol. 1995;90:366–71. [PubMed] [Google Scholar]
- 62.Taylor ML, Trotter DR, Csuka ME. The prevalence of sexual abuse in women with fibromyalgia. Arthritis Rheum. 1995;38:229–34. doi: 10.1002/art.1780380211. [DOI] [PubMed] [Google Scholar]
- 63.Taylor RR, Jason LA. Sexual abuse, physical abuse, chronic fatigue, and chronic fatigue stndrome: a community-based study. The Journal of Nervous and Mental Disease. 2001;189:709–15. doi: 10.1097/00005053-200110000-00008. [DOI] [PubMed] [Google Scholar]
- 64.Taylor RR, Jason LA. Chronic fatigue, abuse-related traumatization, and psychiatric disorders in a community-based sample. Soc Sci Med. 2002;55:247–56. doi: 10.1016/s0277-9536(01)00168-x. [DOI] [PubMed] [Google Scholar]
- 65.Van Houdenhove B, Neerinckx E, Lysens R, Vertommen H, Van Houdenhove L, Onghena P, Westhovens R, D’Hooghe MB. Victimization in chronic fatigue syndrome and fibromyalgia in tertiary care: a controlled study on prevalence and characteristics. Psychosomatics. 2001;42:21–8. doi: 10.1176/appi.psy.42.1.21. [DOI] [PubMed] [Google Scholar]
- 66.Van Oudenhove L, Vandenberghe J, Vos R, Holvoet L, Tack J. Factors associated with co-morbid irritable bowel syndrome and chronic fatigue-like symptoms in functional dyspepsia. Neurogastroenterol Motil. 2011;23:524–e202. doi: 10.1111/j.1365-2982.2010.01667.x. [DOI] [PubMed] [Google Scholar]
- 67.Walker EA, Gelfand AN, Gelfand MD, Katon WJ. Psychiatric diagnoses, sexual and physical victimization, and disability in patients with irritable bowel syndrome or inflammatory bowel disease. Psychol Med. 1995;25:1259–67. doi: 10.1017/s0033291700033225. [DOI] [PubMed] [Google Scholar]
- 68.Walker EA, Katon WJ, Roy-Byrne PP, Jemelka RP, Russo J. Histories of sexual victimization in patients with irritable bowel syndrome or inflammatory bowel disease. Am J Psychiatry. 1993;150:1502–6. doi: 10.1176/ajp.150.10.1502. [DOI] [PubMed] [Google Scholar]
- 69.Walker EA, Keegan D, Gardner G, Sullivan M, Bernstein D, Katon WJ. Psychosocial factors in fibromyalgia compared with rheumatoid arthritis: II. Sexual, physical, and emotional abuse and neglect. Psychosom Med. 1997;59:572–7. doi: 10.1097/00006842-199711000-00003. [DOI] [PubMed] [Google Scholar]
- 70.White DL, Savas LS, Daci K, Elserag R, Graham DP, Fitzgerald SJ, Smith SL, Tan G, El-Serag HB. Trauma history and risk of the irritable bowel syndrome in women veterans. Aliment Pharmacol Ther. 2010;32:551–61. doi: 10.1111/j.1365-2036.2010.04387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Williams RE, Hartmann KE, Sandler RS, Miller WC, Steege JF. Prevalence and characteristics of irritable bowel syndrome among women with chronic pelvic pain. Obstet Gynecol. 2004;104:452–8. doi: 10.1097/01.AOG.0000135275.63494.3d. [DOI] [PubMed] [Google Scholar]
Footnotes
Conflicts of Interest: None of the authors have any conflicts of interest to declare.
References
- 1.Barsky AJ, Borus JF. Functional somatic syndromes. Ann Intern Med. 1999;130:910–21. doi: 10.7326/0003-4819-130-11-199906010-00016. [DOI] [PubMed] [Google Scholar]
- 2.Burton C. Beyond somatisation: a review of the understanding and treatment of medically unexplained physical symptoms (MUPS) Br J Gen Pract. 2003;53:231–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Escobar JI, Hoyos-Nervi C, Gara M. Medically unexplained physical symptoms in medical practice: a psychiatric perspective. Environ Health Perspect. 2002;110 (Suppl 4):631–6. doi: 10.1289/ehp.02110s4631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wessely S, Nimnuan C, Sharpe M. Functional somatic syndromes: one or many? Lancet. 1999;354:936–9. doi: 10.1016/S0140-6736(98)08320-2. [DOI] [PubMed] [Google Scholar]
- 5.Katon W, Sullivan M, Walker E. Medical symptoms without identified pathology: relationship to psychiatric disorders, childhood and adult trauma, and personality traits. Ann Intern Med. 2001;134:917–25. doi: 10.7326/0003-4819-134-9_part_2-200105011-00017. [DOI] [PubMed] [Google Scholar]
- 6.Roelofs K, Spinhoven P. Trauma and medically unexplained symptoms towards an integration of cognitive and neuro-biological accounts. Clin Psychol Rev. 2007;27:798–820. doi: 10.1016/j.cpr.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 7.Russo J, Katon W, Sullivan M, Clark M, Buchwald D. Severity of somatization and its relationship to psychiatric disorders and personality. Psychosomatics. 1994;35:546–56. doi: 10.1016/S0033-3182(94)71723-0. [DOI] [PubMed] [Google Scholar]
- 8.Aaron LA, Buchwald D. Chronic diffuse musculoskeletal pain, fibromyalgia and co-morbid unexplained clinical conditions. Best Pract Res Clin Rheumatol. 2003;17:563–74. doi: 10.1016/s1521-6942(03)00033-0. [DOI] [PubMed] [Google Scholar]
- 9.White PD. Chronic fatigue syndrome: Is it one discrete syndrome or many? Implications for the “one vs. many” functional somatic syndromes debate. J Psychosom Res. 2010;68:455–9. doi: 10.1016/j.jpsychores.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 10.Moss-Morris R, Spence M. To “lump” or to “split” the functional somatic syndromes: can infectious and emotional risk factors differentiate between the onset of chronic fatigue syndrome and irritable bowel syndrome? Psychosom Med. 2006;68:463–9. doi: 10.1097/01.psy.0000221384.07521.05. [DOI] [PubMed] [Google Scholar]
- 11.Wessely S, White PD. There is only one functional somatic syndrome. Br J Psychiatry. 2004;185:95–6. doi: 10.1192/bjp.185.2.95. [DOI] [PubMed] [Google Scholar]
- 12.Aggarwal VR, McBeth J, Zakrzewska JM, Lunt M, Macfarlane GJ. The epidemiology of chronic syndromes that are frequently unexplained: do they have common associated factors? Int J Epidemiol. 2006;35:468–76. doi: 10.1093/ije/dyi265. [DOI] [PubMed] [Google Scholar]
- 13.Gershuny BS, Thayer JF. Relations among psychological trauma, dissociative phenomena, and trauma-related distress: a review and integration. Clin Psychol Rev. 1999;19:631–57. doi: 10.1016/s0272-7358(98)00103-2. [DOI] [PubMed] [Google Scholar]
- 14.Leserman J, Drossman DA. Relationship of abuse history to functional gastrointestinal disorders and symptoms: some possible mediating mechanisms. Trauma Violence Abuse. 2007;8:331–43. doi: 10.1177/1524838007303240. [DOI] [PubMed] [Google Scholar]
- 15.Kendall-Tackett KA. Physiological correlates of childhood abuse: chronic hyperarousal in PTSD, depression, and irritable bowel syndrome. Child Abuse Negl. 2000;24:799–810. doi: 10.1016/s0145-2134(00)00136-8. [DOI] [PubMed] [Google Scholar]
- 16.Bracha HS. Freeze, flight, fight, fright, faint: adaptationist perspectives on the acute stress response spectrum. CNS Spectr. 2004;9:679–85. doi: 10.1017/s1092852900001954. [DOI] [PubMed] [Google Scholar]
- 17.Romans S, Cohen M. Unexplained and underpowered: the relationship between psychosomatic disorders and interpersonal abuse -- a critical review. Harv Rev Psychiatry. 2008;16:35–54. doi: 10.1080/10673220801933788. [DOI] [PubMed] [Google Scholar]
- 18.Chitkara DK, van Tilburg MA, Blois-Martin N, Whitehead WE. Early life risk factors that contribute to irritable bowel syndrome in adults: a systematic review. Am J Gastroenterol. 2008;103:765–74. doi: 10.1111/j.1572-0241.2007.01722.x. quiz 775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Raphael KG, Janal MN, Nayak S, Schwartz JE, Gallagher RM. Familial aggregation of depression in fibromyalgia: a community-based test of alternate hypotheses. Pain. 2004;110:449–60. doi: 10.1016/j.pain.2004.04.039. [DOI] [PubMed] [Google Scholar]
- 20.Raphael KG. Childhood abuse and pain in adulthood: more than a modest relationship? Clin J Pain. 2005;21:371–3. doi: 10.1097/01.ajp.0000149794.70627.18. [DOI] [PubMed] [Google Scholar]
- 21.Paras ML, Murad MH, Chen LP, Goranson EN, Sattler AL, Colbenson KM, Elamin MB, Seime RJ, Prokop LJ, Zirakzadeh A. Sexual abuse and lifetime diagnosis of somatic disorders: a systematic review and meta-analysis. Jama. 2009;302:550–61. doi: 10.1001/jama.2009.1091. [DOI] [PubMed] [Google Scholar]
- 22.Hauser W, Kosseva M, Uceyler N, Klose P, Sommer C. Emotional, physical, and sexual abuse in fibromyalgia syndrome: a systematic review with meta-analysis. Arthritis Care Res (Hoboken) 2011;63:808–20. doi: 10.1002/acr.20328. [DOI] [PubMed] [Google Scholar]
- 23.Sharp TJ, Harvey AG. Chronic pain and posttraumatic stress disorder: mutual maintenance? Clin Psychol Rev. 2001;21:857–77. doi: 10.1016/s0272-7358(00)00071-4. [DOI] [PubMed] [Google Scholar]
- 24.Asmundson GJ, Coons MJ, Taylor S, Katz J. PTSD and the experience of pain: research and clinical implications of shared vulnerability and mutual maintenance models. Can J Psychiatry. 2002;47:930–7. doi: 10.1177/070674370204701004. [DOI] [PubMed] [Google Scholar]
- 25.Hinton DE, Hinton SD, Loeum RJ, Pich V, Pollack MH. The ‘multiplex model’ of somatic symptoms: application to tinnitus among traumatized Cambodian refugees. Transcult Psychiatry. 2008;45:287–317. doi: 10.1177/1363461508089768. [DOI] [PubMed] [Google Scholar]
- 26.Liedl A, Knaevelsrud C. Chronic pain and PTSD: the Perpetual Avoidance Model and its treatment implications. Torture. 2008;18:69–76. [PubMed] [Google Scholar]
- 27.Pacella ML, Hruska B, Delahanty DL. The physical health consequences of PTSD and PTSD symptoms: A meta-analytic review. J Anxiety Disord. 2012;27:33–46. doi: 10.1016/j.janxdis.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 28.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9. W64. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 29.Wells G, Shea B, O’Connell D, Petersen J, Welch V, Losos M, Tugwell P. The Newcastle Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Department of Epidemiology and Community Medicine, University of Ottawa; Canada: 2009. [Google Scholar]
- 30.Borenstein MHL, Higgins J, Rothstein H. Comprehensive Meta-analysis Version 2. Englewood NJ: Biostat; 2005. [Google Scholar]
- 31.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 32.Song F, Sheldon TA, Sutton AJ, Abrams KR, Jones DR. Methods for exploring heterogeneity in meta-analysis. Eval Health Prof. 2001;24:126–51. doi: 10.1177/016327870102400203. [DOI] [PubMed] [Google Scholar]
- 33.Rosenthal R. Meta-analysis: A review. Psychosom Med. 1991;53:247–271. doi: 10.1097/00006842-199105000-00001. [DOI] [PubMed] [Google Scholar]
- 34.Sundbom E, Henningsson M, Holm U, Soderbergh S, Evengard B. Possible influence of defenses and negative life events on patients with chronic fatigue syndrome: a pilot study. Psychol Rep. 2002;91:963–78. doi: 10.2466/pr0.2002.91.3.963. [DOI] [PubMed] [Google Scholar]
- 35.Kang HK, Natelson BH, Mahan CM, Lee KY, Murphy FM. Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: a population-based survey of 30,000 veterans. Am J Epidemiol. 2003;157:141–8. doi: 10.1093/aje/kwf187. [DOI] [PubMed] [Google Scholar]
- 36.Amital D, Fostick L, Polliack ML, Segev S, Zohar J, Rubinow A, Amital H. Posttraumatic stress disorder, tenderness, and fibromyalgia syndrome: are they different entities? J Psychosom Res. 2006;61:663–9. doi: 10.1016/j.jpsychores.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 37.Muhvic-Urek M, Uhac I, Vuksic-Mihaljevic Z, Leovic D, Blecic N, Kovac Z. Oral health status in war veterans with post-traumatic stress disorder. J Oral Rehabil. 2007;34:1–8. doi: 10.1111/j.1365-2842.2006.01674.x. [DOI] [PubMed] [Google Scholar]
- 38.Clancy CP, Graybeal A, Tompson WP, Badgett KS, Feldman ME, Calhoun PS, Erkanli A, Hertzberg MA, Beckham JC. Lifetime trauma exposure in veterans with military-related posttraumatic stress disorder: association with current symptomatology. J Clin Psychiatry. 2006;67:1346–53. doi: 10.4088/jcp.v67n0904. [DOI] [PubMed] [Google Scholar]
- 39.Dedert EA, Green KT, Calhoun PS, Yoash-Gantz R, Taber KH, Mumford MM, Tupler LA, Morey RA, Marx CE, Weiner RD, Beckham JC. Association of trauma exposure with psychiatric morbidity in military veterans who have served since September 11, 2001. J Psychiatr Res. 2009;43:830–6. doi: 10.1016/j.jpsychires.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Goodman GS, Ghetti S, Quas JA, Edelstein RS, Alexander KW, Redlich AD, Cordon IM, Jones DP. A prospective study of memory for child sexual abuse: new findings relevant to the repressed-memory controversy. Psychol Sci. 2003;14:113–8. doi: 10.1111/1467-9280.01428. [DOI] [PubMed] [Google Scholar]
- 41.Raphael KG, Janal MN, Nayak S, Schwartz JE, Gallagher RM. Psychiatric comorbidities in a community sample of women with fibromyalgia. Pain. 2006;124:117–25. doi: 10.1016/j.pain.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 42.Bryant RA, Sackville T, Dang ST, Moulds M, Guthrie R. Treating acute stress disorder: an evaluation of cognitive behavior therapy and supportive counseling techniques. Am J Psychiatry. 1999;156:1780–6. doi: 10.1176/ajp.156.11.1780. [DOI] [PubMed] [Google Scholar]
- 43.Williams LM. Recall of childhood trauma: a prospective study of women’s memories of child sexual abuse. J Consult Clin Psychol. 1994;62:1167–76. doi: 10.1037//0022-006x.62.6.1167. [DOI] [PubMed] [Google Scholar]
- 44.Raphael KG, Cloitre M, Dohrenwend BP. Problems of recall and misclassification with checklist methods of measuring stressful life events. Health Psychol. 1991;10:62–74. doi: 10.1037//0278-6133.10.1.62. [DOI] [PubMed] [Google Scholar]
- 45.Widom CS, Kuhns JB. Childhood victimization and subsequent risk for promiscuity, prostitution, and teenage pregnancy: a prospective study. Am J Public Health. 1996;86:1607–12. doi: 10.2105/ajph.86.11.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.WHO. The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. World Health Organization; 1993. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.