Abstract
Background: Nasal tuberculosis (NTB) is rare, but it can be caused by either a pulmonary disease or a retrograde involvement of the nose by lupus vulgaris of the facial skin. In this study, we present a case of NTB with an ulcerative lesion in her left nasal cavity.
Case presentation: A 56 years old woman presented with an ulcerative lesion in her left nasal cavity. The patient exhibited no clinical evidence of any systemic diseases. Peripheral leucocyte count (CBC) was normal but erythrocyte sedimentation rate was elevated. Mantoux' test elicited 25 mm reaction after 72 hr. Chest x-ray was normal. Pathological evaluation of the lesion revealed the caseating granulomas, epithelioid cells, lymphocytes, and a few giant cells. These findings suggested a diagnosis of tuberculosis. The patient was cured after 6 months treatment with standard regimen of tuberculosis.
Conclusion: Although, nasal tuberculosis is rare, it should be considered in the differential diagnosis of patients with chronic nasal symptoms and ulcerative lesions of the nose.
Key Words: Tuberculosis, Nasal tuberculosis, Nasal cavity, Ulcerative lesion.
Tuberculosis is the most common infectious disease after HIV infection in the world (1). Although tuberculosis is more common in the developing nations, an increase has been noted even in developed countries. AIDS, which destroys the cellular immune system, is one of the primary factors responsible for the reemergence of tuberculosis (1). Nasal involvement is rare. Nasal tuberculosis (NTB) is usually secondary either to pulmonary TB or to facial TB (2). NTB was first described in 1761 by the Italian anatomist while reporting the autopsy findings of a young man with ulcerative lesion of the nose (3). Primary tuberculosis of the nose is also rare. The first case of primary NTB was presented in 1852 (3). Recently, in a case series study only eight cases of NTB was reported (4). Few cases were also reported previously (2, 5-8). In this article, we report a case of Nasal tuberculosis.
Case Peresentaion
A 56 year old woman referred by her primary practitioner to a dermatologist for evaluation of a 2 months history of her left nasal ulcerative lesion with obstruction and occasional epistaxis. Her doctors had prescribed courses of antibiotic, antihistamine and anti-leishmania therapy, but treatment did not relieve his symptoms. Because of continuation of her problems, she was referred to our center for further evaluation. Physical examination of her nose revealed the presence of a reddish ulcerative lesion on the lateral edge of the internal mucosal layer in the left nasal cavity (Figure 1).
Figure 1.
Reddish ulcerative lesion on the nose and in the internal mucosal layer
The mucosa over the turbinate and the mucosa over the septum were thick and bled when touched. The lesion was biopsied. A diagnosis of granulomatous disease of the nose was made. The patient exhibited no clinical evidence of any systemic diseases.
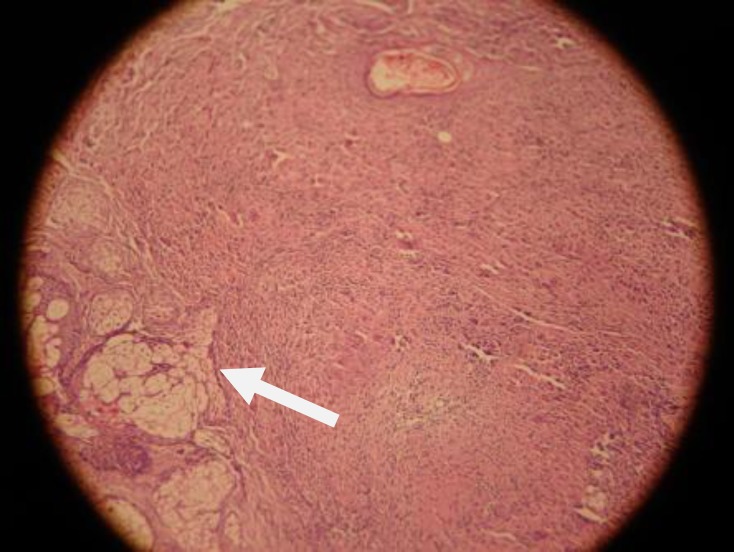
Complete blood cell count (CBC) was normal and erythreocyte sedimentation rate (ESR) was 20 mm/hr and she had no antibodies to HIV, results of renal and liver function tests were normal. Her Mantoux' test elicited 25 mm reaction after 72 hr. Three sputum smears were negative for acid-fast bacilli, as were subsequent cultures. Findings on CT scan of the Para nasal sinuses were normal except for hypertrophy of the turbinate on the left side. Findings of chest x-rays were normal. Histopathological evaluation revealed the caseating granulomatous reaction, epithelioid cells, lymphocytes, and a few giant cells (Figure 2). These findings suggested a diagnosis of tuberculosis.
Figure 2.
Caseating granulomatous reaction, epithelioid cells, lymphocytes, and a few giant cells
The patient was received isoniazid, rifampin, ethambutol and pyrazinamide for 2 months, followed by isoniazid and rifampin for 4 months. Treatment resulted in a rapid resolution of symptoms and a regression of the nasal lesion. Nine months follow-up, including comprehensive clinical and nasal examination was performed and he remained disease-free at this period.
Discussion
In this paper we present a case of nasal tuberculosis in an endemic region. Reported cases of nasal tuberculosis have occurred in patients between the ages of 20 and 84 years. The NTB occurs more often in women than men. The presenting symptoms were nasal obstruction, nasal discharge, epistaxis, crusting, recurrent nasal polyps and ulceration. Lesions may be ulcerative, infiltrative, or proliferative, and most cases were unilateral (5). The most commonly involved site is the nasal septum. Perforation of the nasal septum occurs in some cases (4).
The diagnosis is difficult because NTB sign and symptoms are nonspecific (9). A definitive diagnosis is made by identifying or isolating tuberculosis bacilli from tissue removed during biopsy or surgery. Nasal secretions and swab specimens have a very low yield and should not be used to rule out this condition. On histology, both caseation and non-caseation granulomas have been described. Biopsies of noncaseating granulomas are confusing histologically, and these cases are often misdiagnosed as Wegener's granuloma (1, 3). Acid-fast bacilli may be demonstrated on Ziehl-Neelsen staining cultures of involved tissues are more often positive than are smears. A portion of any biopsy specimen should be sent for culture, along with a notification of the types of organisms that are suspected (10). Standard 6 months anti TB treatment should be established for the treatment of NTB. Accordance of current TB incidence trends, it would be kept in mind of infectious disease specialist as well as ENT specialist to consider of TB as a potential entity when encountering an unusual lesion in the nasal cavity (10, 11). The nasal lesion in our patient was diagnosed as nasal tuberculosis on the basis of histology and the clinical response to antituberculous drugs.
Acknowledgments
The authors thank the chief and personnel of Behbahan Health Center for kindly cooperation in treatment and post treatment following the case.
Conflict of interest: There is no conflict of interest.
References
- 1.Fitzgerald DW, Sterling TR, Haas DW. Mycobacterium tuberculosis. In: Mandell GL, Bennett JE, Dolin R, editors. Principle and Practice of infectious diseases. 7th ed. USA, Philadelphia: Churchill Livingstone; 2010. pp. 3129–63. [Google Scholar]
- 2.Choi YC, Park YS, Jeon EJ, Song SH. The disappeared disease: Tuberculosis of the nasal septum. Rhinology. 2000;38:90–2. [PubMed] [Google Scholar]
- 3.Waldman SR, Levine HL, Sebek BA, Parker W, Tucker HM. Nasal tuberculosis: A forgotten entity. Laryngoscope. 1981;91:11–6. doi: 10.1288/00005537-198101000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Kim YM, Kim AY, Park YH, Kim DH, Rha KS. Eight cases of nasal tuberculosis. Otolaryngol Head Neck Surg. 2007;137:500–4. doi: 10.1016/j.otohns.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 5.Blanco Aparicio M, Verea Hernando H, Pombo F. Tuberculosis of the nasal fossa manifested by a polypoid mass. J Otolaryngol. 1995;24:317–18. [PubMed] [Google Scholar]
- 6.Singhal SK, Dass A, Mohan H, Venkataramana Y. Primary nasal tuberculosis. J Otolaryngol. 2002;31:60–2. doi: 10.2310/7070.2002.19258. [DOI] [PubMed] [Google Scholar]
- 7.Hup AK, Haitjema T, de Kuijper G. Primary nasal tuberculosis. Rhinology. 2001;39:47–8. [PubMed] [Google Scholar]
- 8.Batra K, Chaudhary N, Motwani G, Rai AK. An unusual case of primary nasal tuberculosis with epistaxis and epilepsy. Ear Nose Throat J. 2002;81:842–4. [PubMed] [Google Scholar]
- 9.Hughes RG, Drake Lee A. Nasal manifestations of granulomatous disease. Hosp Med. 2001;2:417–21. doi: 10.12968/hosp.2001.62.7.1612. [DOI] [PubMed] [Google Scholar]
- 10.Goguen LA, Karmody CS. Nasal tuberculosis. Otolaryngol Head Neck Surg. 1995;113:131–5. doi: 10.1016/S0194-59989570156-7. [DOI] [PubMed] [Google Scholar]
- 11.Johnson IJ, Soames JV, Marshall HF. Nasal tuberculosis: an increasing problem? J Laryngeal Tool. 1995;109:326–7. doi: 10.1017/s002221510013004x. [DOI] [PubMed] [Google Scholar]