Abstract
Cyclophosphamide is frequently used for the treatment of severe lupus nephritis, but is very rarely associated with dilutional hyponatremia. Recently we experienced a case of water intoxication following low-dose intravenous cyclophosphamide. Five hours after one dose of intravenous pulse cyclophosphamide 750 mg, the patient developed nausea, vomiting, and general weakness. Serum sodium concentration revealed 114 mEq/L and her hyponatremia was initially treated with hypertonic saline infusion. Then her serum sodium concentration rapidly recovered to normal with water restriction alone. During the course of intravenous pulse cyclophosphamide therapy, one must be aware of the possibility of significant water retention.
Keywords: Cyclophosphamide, Lupus nephritis, Water intoxication, Hyponatremia
Introduction
Cyclophophamide is an alkylating agent used extensively in the treatment of malignant and rheumatological diseases. Its side effects include bone marrow depression, infection, alopecia, sterility, bladder malignancy, and hemorrhagic cystitis1). However, it is less well known that intravenous cyclophosphamide reduces the kidney's ability to excrete water. Since forced hydration is used routinely to prevent hemorrhagic cystitis, treated patients may retain water, and rapidly develop severe hyponatremia2).
Severe hyponatremia was previously reported in patients treated with high-dose (30-40 mg/kg)3-6) and moderate-dose (20-30 mg/kg)7) intravenous cyclophosphamide. However, there have been only 5 cases in which severe hyponatremia was reported from low-dose intravenous pulse cyclophosphamide therapy1, 8, 9). Here we report another case of water intoxication following low-dose intravenous cyclophosphamide.
Case Report
A 27-year-old woman was diagnosed at a local hospital one year ago as systemic lupus erythematosus (SLE) presenting with arthritis of both hands and knees, serositis (pericarditis and pleuritis), and positive tests for anti-nuclear antibody and anti-double stranded DNA antibodies. At the same time, she was found to be hypertensive. Her SLE was initially treated with oral methylprednisone 48 mg per day, and anti-hypertensive drugs (propranolol, irbesartan and nifedipine) were given.
She visited us for further evaluation complaining of general weakness and lower extremities edema. At admission her blood pressure was well controlled (110/70 mmHg). Laboratory studies showed the followings: hemoglobin 6.9 g/dL, platelet 170,000/mm3, WBC count 5,600/mm3, blood urea nitrogen 47 mg/dL, serum creatinine 1.1 mg/dL, serum sodium concentration 136 mEq/L, serum potassium 4.6 mEq/L, serum chloride 104 mEq/L, serum total CO2 19.3 mEq/L, serum albumin 3.6 g/dL, serum protein 5.7 g/dL, and serum cholesterol 232 mg/dL. Positive antinuclear and anti-double stranded DNA antibodies were confirmed, and serum complement levels were lowered (C3 46.8 mg/dL, C4 9.2 mg/mL, CH50 6.4 Units/mL). Thyroid function test was normal (TSH 1.06 uIU/mL, free T4 1.05 ng/dL), and serum cortisol level was normal. Urinalysis showed that specific gravity 1.025; pH 6.0; protein 2+; occult blood 3+; WBC 0-1/HPF; and RBC 20-29/HPF. The amount of proteinuria collected from 24-h urine was 1.3 g.
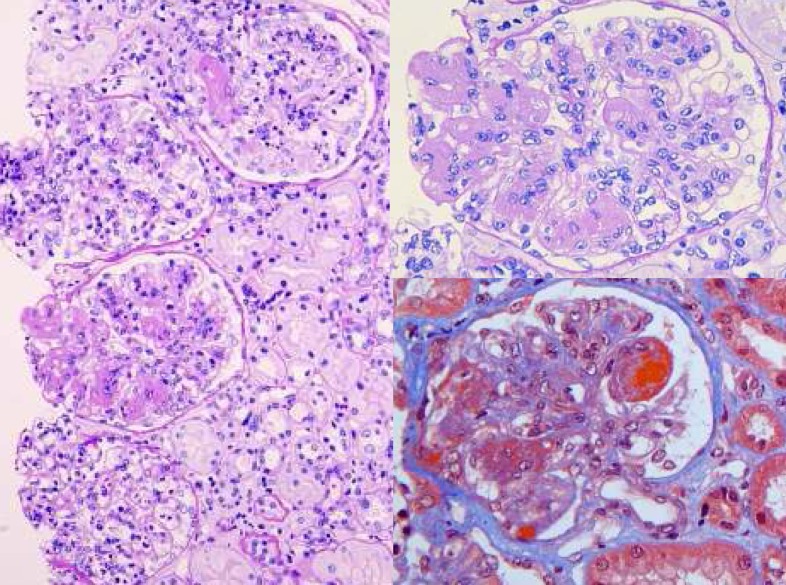
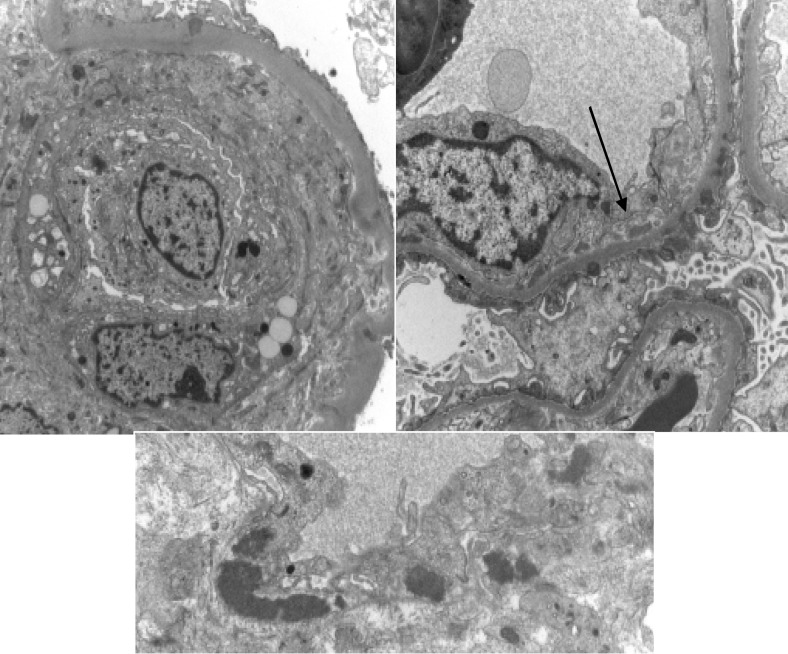
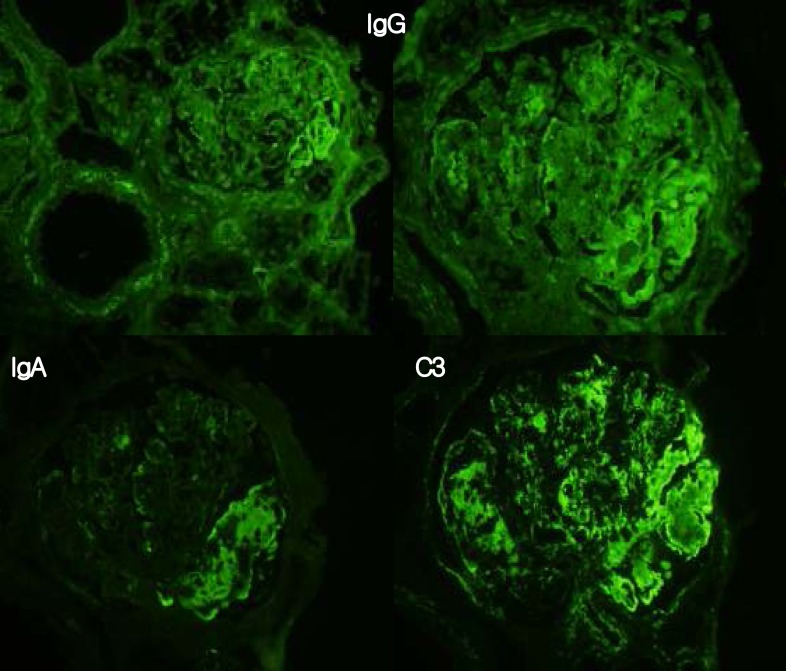
Percutaneous renal biopsy was carried out and revealed WHO class III focal segmental endocapillary proliferative lupus neprhitis with an associated subendothelial deposit (Fig. 1-3). NIH activity index was 9/24, and chronicity index was 3/12. Although she was treated with prednisolone 50 mg per day and hydroxychloroquine 200 mg per day for three weeks, proteinuria persistently increased to 2.5 g/day.
Fig. 1.
Lighg microscopy finding of the renal biopsy, compatible with lupus nephritis class III(A). Note moderately segmental endocapillary cell proliferation and infiltration of neutrophils and lymphocytes with some karyorrhetic bodies. The glomerular capillary walls are segmentally thickened and narrowed by large subendothelial fuchsinophilic deposits to form 'wire loop' lesion and hyaline thrombi in some lumina. There are moderate tubular atrophy, focal interstitial fibrosis and scattered lymphocytes.
Fig. 3.
Electron microscopy findings. Left : Endocapillary proliferation with double contour of glomerular basement membrane is shown along with mesangial electron dense deposits, Right: There are small subendothelial (arrow), and scattered subepithelial deposits. Below: Note large electron dense deposits in Intertubular capillary basement membranes.
On the twenty-second hospital day, she received a single intravenous cyclophosphamide 700 mg (14.8 mg/kg). Just before the low-dose intravenous pulse cyclophosphamide therapy, her blood pressure was 120/70 mmHg and laboratory findings were stable as follows: serum sodium concentration 135 mEq/L, serum potassium 5.1 mEq/L, serum chloride 96 mEq/L, blood urea nitrogen 28 mg/dL, and serum creatinine 0.8 mg/dL. To minimize the risk of hemorrhagic cystitis, half-saline was infused at a rate of 150 mL/h for 2 hours each before and after cyclophosphamide administration. Additionally she was advised to drink at least 2 L over the next 24 hours.
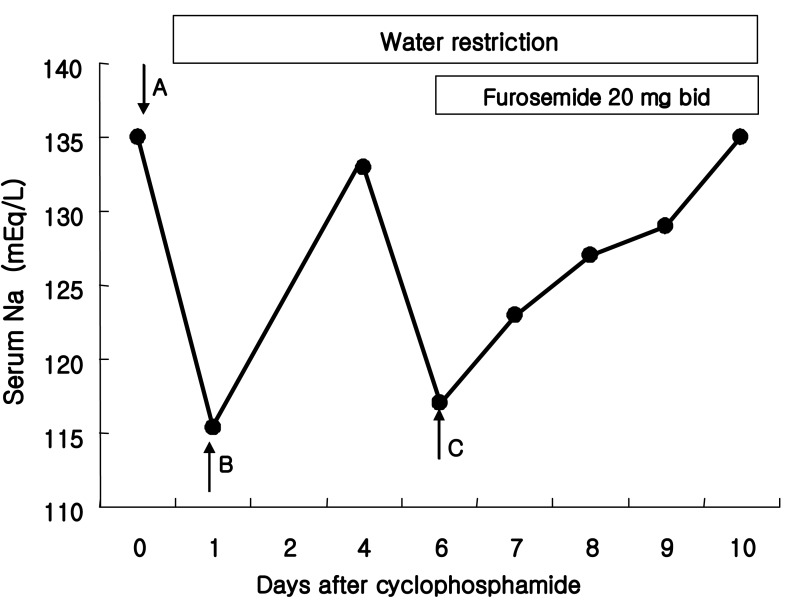
Five hours after the intravenous cyclophosphamide administration, nausea, vomiting and general weakness were suddenly developed. Her blood pressure was increased to 160/110 mmHg, and she was physically euvolemic and had no lateralizing sign. Emergency laboratory findings were serum sodium concentration 114 mEq/L, serum urea nitrogen 30 mg/dL, serum creatinine 0.8 mg/dL, serum osmolality 232 mOsm/kg H2O, urine osmolality 487 mOsm/kg H2O, urine sodium 121 mEq/L, urine potassium 44.4 mEq/L, and urine chloride 141 mEq/L. Because her hyponatremia was acute and symptomatic, she was treated with intravenous infusion of 3% NaCl solution at a rate of 30 mL/h for 11 hours. Then, with water restriction only, her serum sodium concentration gradually increased to 123 mEq/L and 128 mEq/L after 24 and 36 hours, respectively. It reached normal level in 5 days after the cyclophosphamide administration (Fig. 4).
Fig. 4.
Time course of serum sodium concentration following intravenous cyclophosphamide. A) Intravenous pulse cyclophosphamide, B) The first episode of hyponatremia, C) The second episode of hyponatremia.
Two days later, another episode of severe hyponatremia occurred when she temporarily went out of the hospital for a day. At home she happened to have a lot of water, and then nausea was developed again. When she was back to the hospital, her serum sodium concentration was 117 mEq/L. She was treated with water restriction and oral furosemide 20 mg twice a day. Her hyponatremia was gradually recovered to the normal level (136 mEq/L) over the next 4 days. She was discharged with oral medications of prednisolone 50 mg per day, azathioprine 25 mg per day and hydroxychloroquine 200 mg per day but without any further plans of intravenous cyclophosphamide.
Discussion
It has been clearly demonstrated that cyclophosphamide transiently impairs the kidney's ability to dilute the urine3, 5-7). In this case we suspected intravenous cyclophosphamide as the cause of severe hyponatremia since no other causes could be found. Disease predisposing to water retention such as renal failure, hypothyroidism and adrenal insufficiency were not present. Besides, our patient had no evidence of congestive heart failure, liver cirrhosis, pulmonary disease or neurologic abnormalities. Prior to treatment with cyclophosphamide, she had normal serum electrolytes and no symptoms of nausea and vomiting.
Our case has common features with other reports in which hyponatremia was induced by intravenous cyclophosphamide. In all reports of cyclophosphamide-induced water intoxication, the drug was given intravenously. Hyponatremia usually occurs 4-12 hours after the administration of cyclophosphamide, although sometimes not until 48 hours afterwards, and returns to normal in around 24 hours. The antidiuretic effect seems to be related to the appearance of an active alkylating metabolite of cyclophosphamide9).
Interestingly, our patient had another episode of severe hyponatremia in 7 days after the administration of cyclophosphamide. It is not very clear whether this was caused by the initial dose of the drug because the half-life of cyclophosphamide in the blood has been estimated to be 6-7 hours10, 11). However, the maximum antidiuretic effect occurs later, 10-14 hours after the drug administration, and the pharmacodynamic profile might be prolonged with the pulse therapy. The general advice to patients to drink 2-3 L of water following intravenous cyclophosphamide to reduce the risk of hemorrhagic cystitis should contribute to water intoxication.
The mechanism by which the active form of cyclophosphamide exerts an effect on urine concentrating ability has not been determined. Harlow et al.4) suggested a syndrome of inappropiate antidiuretic hormone secretion (SIADH). This hypothesis is corroborated by the postmortem examination performed on one patient who had received high-dose cyclophosphamide, demonstrating loss of Herring's bodies and degranulation of various hypothalamic neurosecretory organelles. This metabolite could act indirectly by causing ADH release and this has been demonstrated with ifosfamide, a close structural analogue to cyclophosphamide12). However, other studies have shown that monitored serum ADH levels have not altered significantly during treatment with cyclophosphamide 13). Therefore, although the clinical picture of cyclophosphamide-induced hyponatremia is typical of SIADH, this term is a misnomer. De Fronzo et al.6) believed that the occurrence of antidiuresis without altered glomerular filtration rate or urine sodium excretion is best explained by a direct effect of an alkylating metabolite of cyclophosphamide on the kidney resulting in enhanced permeability of the distal tubules to water. Further evidence of the possible site of interaction between cyclophosphamide and ADH comes from hypopituitary patients treated with cyclophosphamide who still develop water intoxication14).
In brief, we need to be aware of the potentially life-threatening complication of water intoxication when even low-dose intravenous pulse cyclophosphamide is applied to the treatment of lupus nephritis. It is recommended to check renal function, electrolytes, serum albumin and full blood count on the day of intravenous cyclophosphamide and to advise patients to drink just 1L of fluid over and above their usual fluid intake in the following 24 hours9). Care is taken to explain that rapid consumption of large fluid volumes should be avoided. In patients with significant renal impairment, severe hypoalbuminemia or tubulo-interstitial damage on renal biopsy, furosemide at the time of intravenous cyclophosphamide therapy may be considered15).
Fig. 2.
Immumofluorescence microscopy finding. Segementally positive stainings for IgG and C3 are conspicuous, and staining for IgA in the mesangium and along the glomerular capillary wall is weak, compatible with lupus nephritis class III.
References
- 1.Webberley MJ, Murray JA. Life-threatening acute hyponatremia induced by low-dose cyclophosphamide and indomethacin. Postgrad Med J. 1989;65:950–952. doi: 10.1136/pgmj.65.770.950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spital A, Ristow S. Cyclophospahmide induced water intoxication in a woman with Sjogren's syndrome. J Rheumatol. 1997;24:2473–2475. [PubMed] [Google Scholar]
- 3.DeFronzo RA, Braine H, Colvin M, Davis PJ. Water intoxication in man after cyclophosphamide therapy. Time course and relation to drug activation. Ann Intern Med. 1973;78:861–869. doi: 10.7326/0003-4819-78-6-861. [DOI] [PubMed] [Google Scholar]
- 4.Harlow PJ, DeClerck YA, Shore NA, Ortega JA, Carranza A, Heuser E. A fatal case of inappropriate ADH secretion induced by cyclophosphamide therapy. Cancer. 1979;44:896–898. doi: 10.1002/1097-0142(197909)44:3<896::aid-cncr2820440316>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 5.Steele TH, Serpick AA, Block JB. Antidiuretic response to cyclophosphamide in man. J Pharmacol Exp Ther. 1973;185:245–253. [PubMed] [Google Scholar]
- 6.DeFronzo RA, Colvin OM, Braine H, Roberson GL, Davis PJ. Proceedings: Cyclophosphamide and the kidney. Cancer. 1974;33:483–491. doi: 10.1002/1097-0142(197402)33:2<483::aid-cncr2820330224>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 7.Bressler RB, Huston DP. Water intoxication following moderate-dose intravenous cyclophosphamide. Arch Intern Med. 1985;145:548–549. [PubMed] [Google Scholar]
- 8.McCarron M, Wright GD, Robert SD. Water intoxication after low dose cyclophosphamide. BMJ. 1995;311:292. doi: 10.1136/bmj.311.7000.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salido M, Macarron P, Hernandez-Garcia C, D'Cruz DP, Khamashta MA, Hughes GR. Water intoxication induced by low-dose cyclophosphamide in two patients with systemic lupus erythematosus. Lupus. 2003;12:636–639. doi: 10.1191/0961203303lu421cr. [DOI] [PubMed] [Google Scholar]
- 10.Buckner CD, Rudolph RH, Fefer A, Clift RA, Epstein RB, Funk DD, Neiman PE, Slichter SJ, Storb R, Thomas ED. High-dose cyclophosphamide therapy for malignant disease. Toxicity, tumor response, and the effects of stored autologous marrow. Cancer. 1972;29:357–365. [Google Scholar]
- 11.Cohen JL, Jao JY, Jusko WJ. Pharmacokinetics of cyclophosphamide in man. Br J Pharmacol. 1971;43:677–680. doi: 10.1111/j.1476-5381.1971.tb07199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kirch C, Garchot B, German N, Blot F, Nitenberg G. Recurrent ifosfamide-induced hyponatremia. Eur J Cancer. 1997;33:2438–2439. doi: 10.1016/s0959-8049(97)00329-8. [DOI] [PubMed] [Google Scholar]
- 13.Pratt CB, Douglass EC, Kovnar EH, Heideman R, Kun L, Avery L, Kellie SJ. A phase I study of ifosfamide given on alternate days to treat children with brain tumors. Cancer. 1993;71:3666–3669. doi: 10.1002/1097-0142(19930601)71:11<3666::aid-cncr2820711132>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 14.Campbell DM, Atkinson A, Gillis D, Sochett EB. Cyclophosphamide and water retention: mechanism revisited. J Pediatr Endocrinol Metab. 2000;13:673–675. doi: 10.1515/jpem.2000.13.6.673. [DOI] [PubMed] [Google Scholar]
- 15.Green TP, Mirrkin BL. Prevention of cyclophosphamide-induced antidiuresis by furosemide infusion. Clin Pharmacol Ther. 1981;29:634–642. doi: 10.1038/clpt.1981.88. [DOI] [PubMed] [Google Scholar]