Abstract
Hypokalemia is a frequent problem in patients on continuous ambulatory peritoneal dialysis (CAPD) and is affected by multiple factors. To evaluate factors associated with hypokalemia, we studied 68 patients on maintenance CAPD treatment for at least six months. In univariate analysis, patients with hypokalemia were associated with older age and the presence of diabetes mellitus. Serum albumin, calcium-phosphate product, triglyceride, body mass index, protein nitrogen appearance, and lean body mass assessed by creatinine kinetics were significantly lower as compared to those without hypokalemia. Serum C-reactive protein was significantly higher in the patients with hypokalemia. Multivariate stepwise linear regression analysis revealed that the serum albumin level and the ultrafiltration volume at the peritoneal equilibration test were independent factors associated with hypokalemia. This suggests that the serum potassium level may be an important nutritional marker in CAPD patients. Further longitudinal investigation is needed to clarify this relationship.
Keywords: Hypokalemia, Potassium, Continuous ambulatory peritoneal dialysis, Nutritional status
Introduction
Hypokalemia is a frequent problem in peritoneal dialysis (PD) and found in 10-36% of PD patients1). Cellular uptake and bowel loss probably play important roles in the pathogenesis of hypokalemia. However, ongoing losses of potassium into dialysate are also an important contributing factor to hypokalemia. This is compounded further by poor nutritional intake, particularly diets including potassium-rich foods like fruits and vegetables2). In most conditions, the plasma potassium concentration varies directly with body potassium stores; total body potassium is a strong predictor of skeletal muscle mass3). It was also reported that hypokalemia was associated with malnutrition or severe comorbidity in peritoneal dialysis patients2). We performed this cross-sectional study to investigate the clinical characteristics of the patients with hypokalemia and the relationship between serum potassium level and nutritional markers, peritoneal transport status, dialysis adequacy, biocompatibility of PD solution, and other clinical indices.
Materials and Methods
1. Patient selection
We studied 68 patients with end-stage renal disease (ESRD) who had received maintenance continuous ambulatory peritoneal dialysis (CAPD) treatment for at least six months. Since the peritoneal membrane transport characteristics can affect serum potassium level in PD patients, we only selected those subjects who underwent the standard measurements of the peritoneal equilibration test (PET) and dialysis adequacy indices on the same day as the blood was drawn for monthly biochemical analysis at Severance Hospital from July 2006 to July 2007. Demographic data including age, sex, duration of dialysis and the use of low glucose degradation products (GDP) solution was also recorded.
2. Detection of hypokalemia
In this study, serum electrolyte concentrations, including serum potassium, are represented as the mean values of three consecutive monthly measurements obtained one month before and one month after the date when the PET was performed. Hypokalemia is defined as an average serum potassium level of less than 3.5 mEq/L. Use of medication that might affect potassium balance, including diuretics, angiotensin-converting enzyme inhibitors (ACEI) and angiotensin receptor blockers (ARB) was also recorded.
3. Urea and creatinine kinetics and peritoneal equilibration test
Lean body mass was assessed by creatinine kinetics (LBMcr)4). Measurements of urea kinetic variables such as the protein equivalent of nitrogen appearance (PNA), urea nitrogen appearance (UNA), total Kt/V, and standardized creatinine clearance were also performed. The PNA was derived from the urea generation rate using the formula proposed by Bergstrom et al.5) and was normalized to the ideal body weight of the patients. The PET was performed to assess peritoneal transport characteristics as previously described6).
4. Statistical analysis
Statistical analysis was performed using SPSS for Window software, 12.0 (SPSS Inc, Chicago, IL). Results are expressed as mean±standard deviation (SD) unless otherwise specified. Comparisons between parameters were performed using the chi-square test, Fisher's exact test, and Mann-Whitney U test. For the analysis of the correlation between serum potassium level and other clinical parameters, we performed Pearson correlation analysis and partial correlation analysis. Subsequently, to determine the factors independently associated with serum potassium level, stepwise multiple linear regression analyses were performed, including factors that had significant association in univariate analysis and those generally accepted as contributing factors.
Results
1. Demographic features of subjects
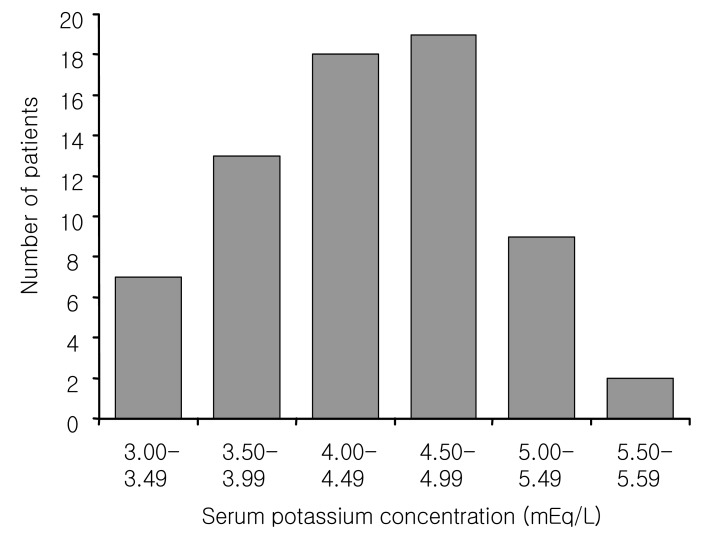
The demographic and clinical characteristics of 68 subjects are listed in Table 1. The mean age was 52.3±12.1 with a range of 25 to 78 years, the male to female ratio was 1.2:1. The mean CAPD duration was 46.5±47.0 months. The mean serum potassium level was 4.4±0.6 mmol/L with a distribution ranging from 3.23 mmol/L to 5.56 mmol/L (Fig. 1). Seven patients (10.3%) had an average serum potassium level less than 3.5 mmol/L. All of these patients required oral potassium supplementation. Forty-four patients (55.0 %) received ACEI/ARBs, and 23 (28.8%) received loop diuretics. These drugs were administered to the patients both with and without hypokalemia. However, the use of these medications did not make any differences between the two groups (Table 1, 2).
Table 1.
Clinical Characteristics of the Patients
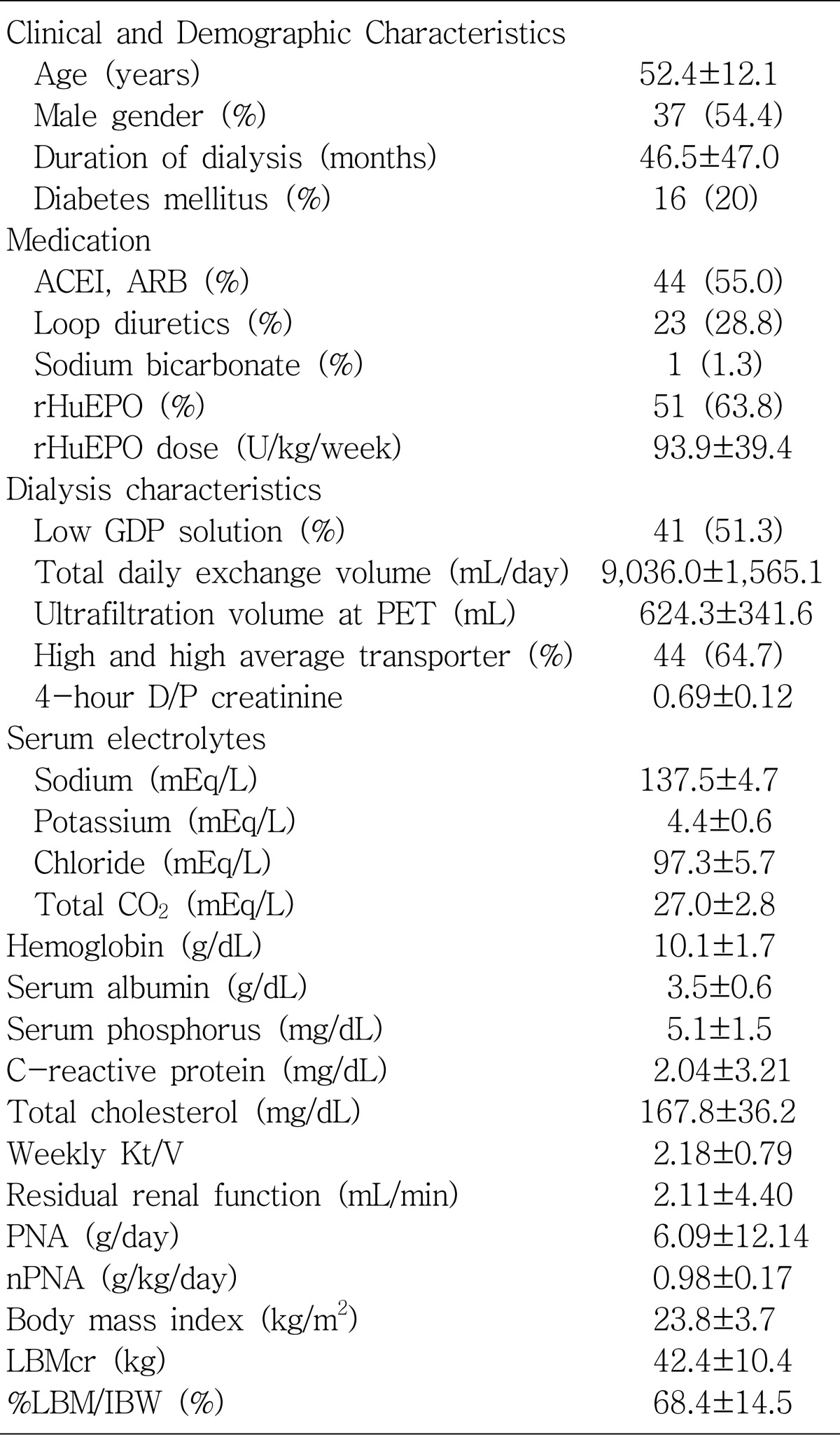
Values are expressed as mean±SD or number (%).
ACEI angiotensin-converting enzyme inhibitors; ARB, angiotensin receptor blockers; rHuEPO, recombinant human erythropoietin; GDP, glucose degradation product; PET, peritoneal equilibration test; D/P creatinine, dialysate to plasma creatinine; PNA, protein equivalent of nitrogen appearance; nPNA, normalized PNA; LBMCr, lean body mass assessed by creatinine kinetics, %LBM/IBW, %lean body mass/ideal body weight.
Fig. 1.
Distribution of patient serum potassium levels.
Table 2.
Clinical Characteristics of Patients with and without Hypokalemia
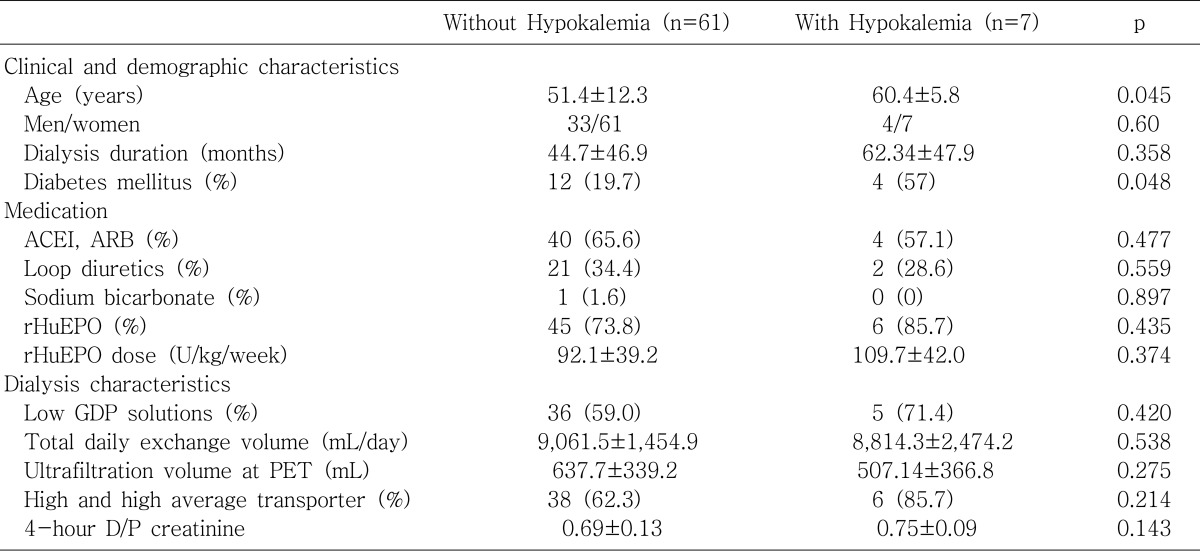
Values are expressed as mean±SD or number (%).
ACEI, angiotensin-converting enzyme inhibitors; ARB, angiotensin receptor blockers; rHuEPO, recombinant human erythropoietin; GDP, glucose degradation product; PET, peritoneal equilibration test; D/P creatinine, dialysate to plasma creatinine.
2.Univariate analysis of clinical and demographic data and correlation analysis
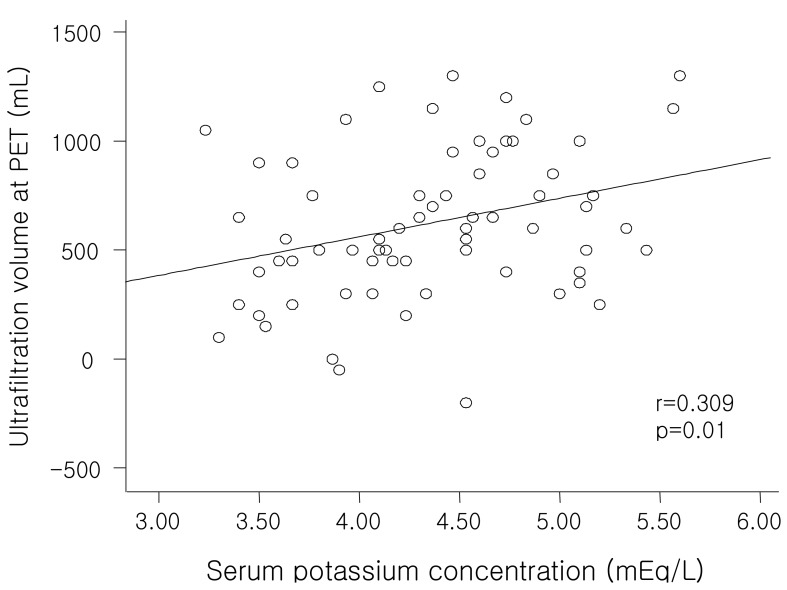
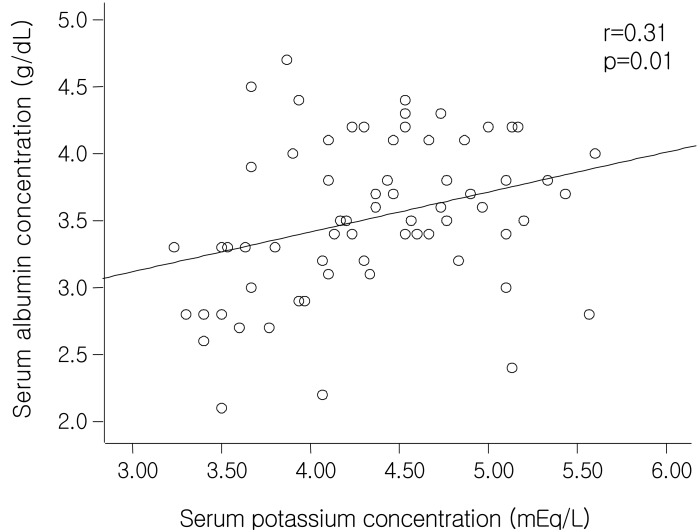
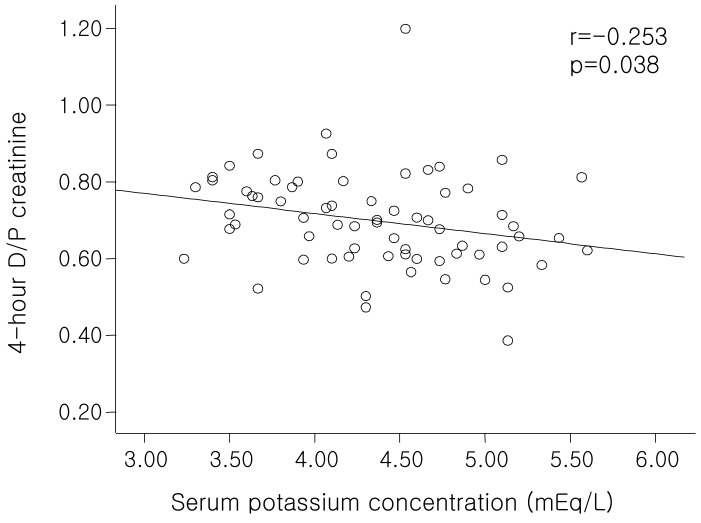
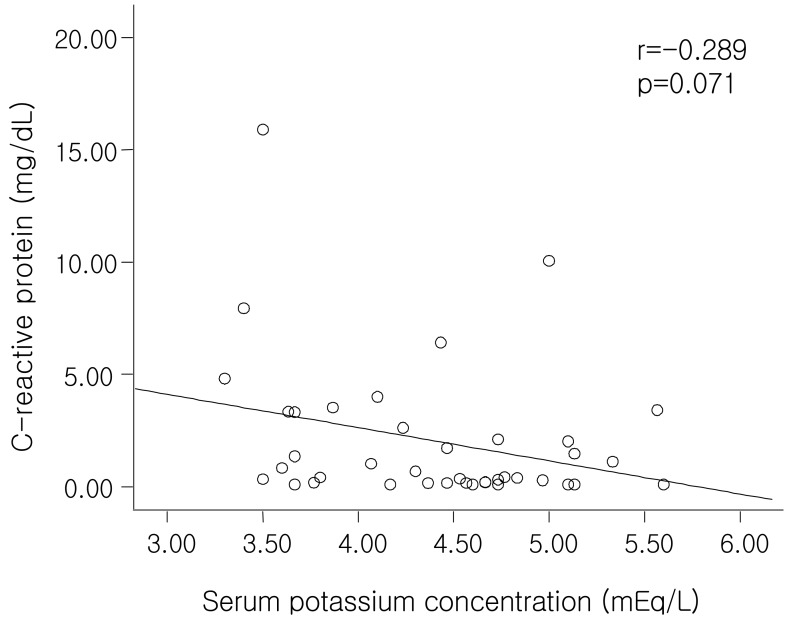
When patients were divided into two groups based on serum potassium level, patients with hypokalemia had significantly older mean ages (p=0.045) and a higher prevalence of diabetes mellitus (p=0.048). However, there was no difference in the frequency of low GDP solution use (p=0.420) and recombinant human erythropoietin (rHuEPO) use (p=0.435) (Table 2). In the patients with hypokalemia, the serum albumin level, calcium-phosphate product, serum triglyceride level, PNA (especially, in UNA component), body mass indices (BMI), and LBMcr (especially, in excretion component) were significantly lower than those without hypokalemia (Table 3-5). The serum C-reactive protein (CRP) level was significantly higher in the patients with hypokalemia compared to the patients without hypokalemia (p=0.028) (Table 3). Pearson correlation analysis showed that serum potassium correlates positively with ultrafiltration volume at the PET (r=0.309, p=0.01), sodium (r=0.301, p=0.013), serum albumin (r=0.31, p=0.01), serum BUN (r=0.354, p=0.03), serum creatinine (r=0.253, p=0.038), PNA (r=0.292, p=0.016), UNA (r=0.292, p=0.016), and dialysate urea nitrogen losses (r=0.263, p=0.03) (Fig. 2, 3). In contrast, serum potassium correlates negatively with 4-hour dialysate to plasma (D/P) creatinine (r=-0.253, p=0.038) (Fig. 4), total CO2 (r=-0.29, p=0.16), ferritin (r=-0.246, p=0.048), peritoneal creatinine clearance (r=-0.256, p=0.035), and serum CRP levels (r=-0.289, p=0.071) (Fig. 5).
Table 3.
Biochemical Characteristics of the Patients with and without Hypokalemia
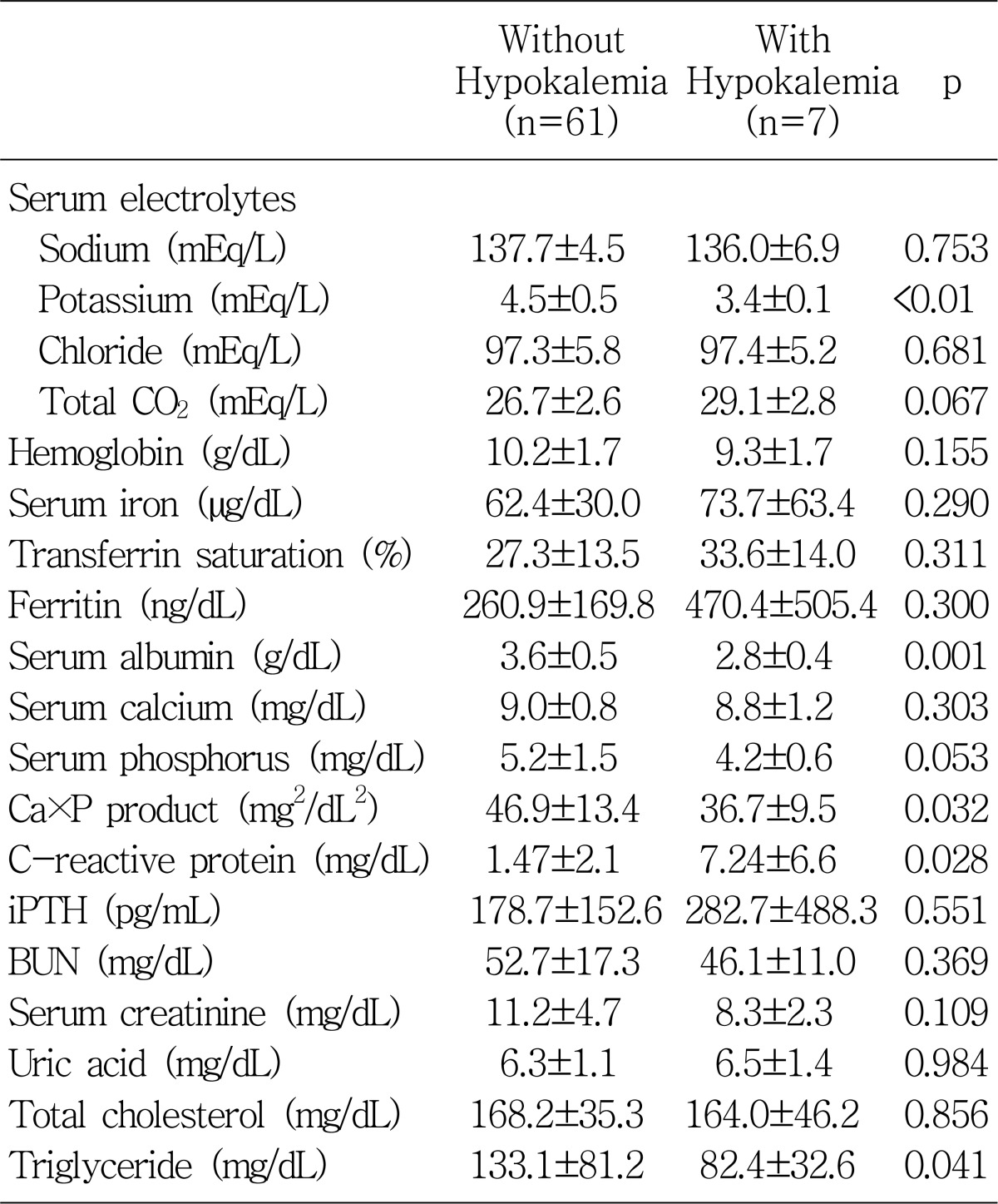
Values are expressed as mean±SD.
Ca×P, calcium-phosphate product; iPHT, intract parathyroid hormone; BUN, blood urea nitrogen.
Table 5.
Anthropometric Parameters of the Patients with and without Hypokalemia
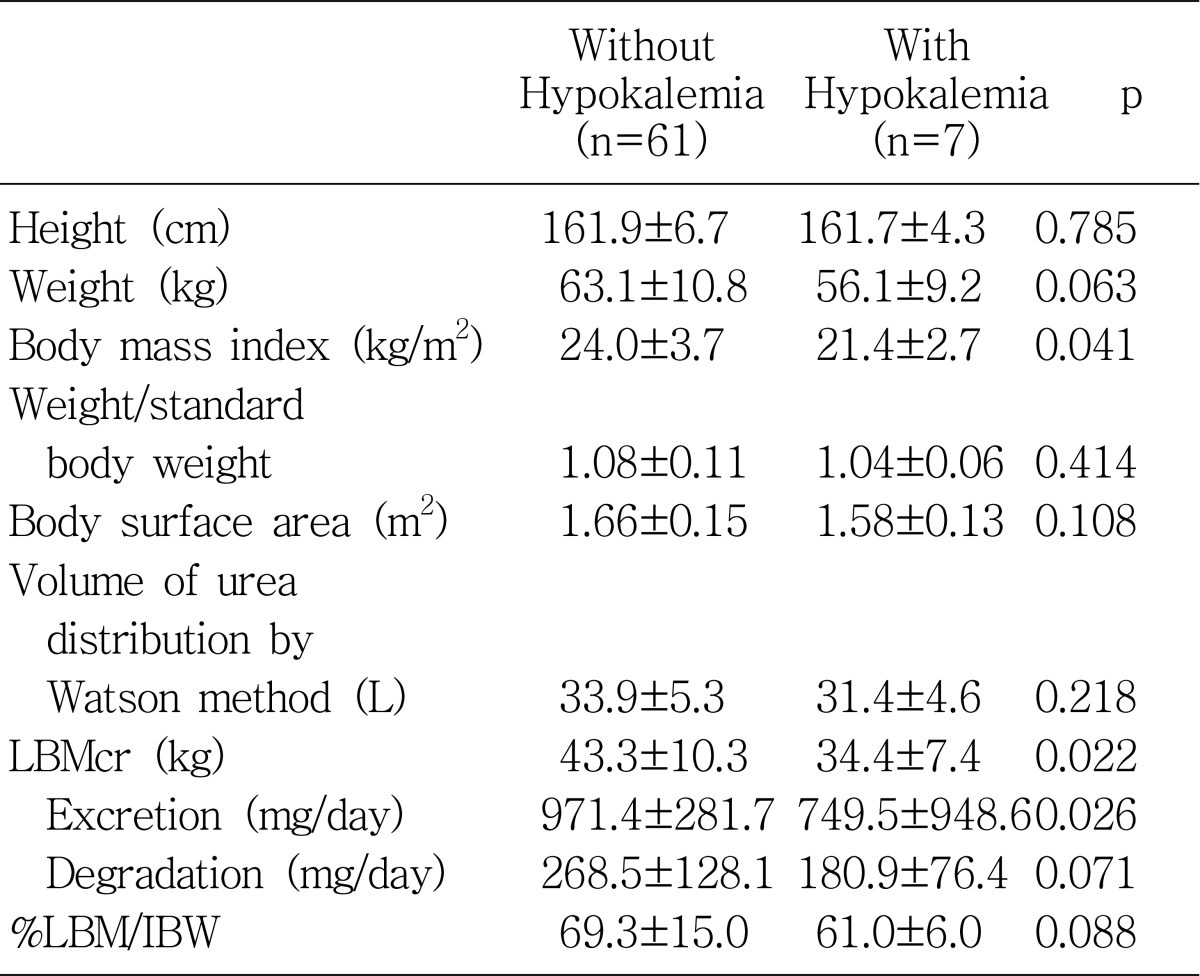
Values are expressed as mean±SD.
LBMCr, lean body mass assessed by creatinine kinetics, %LBM/IBW, %lean body mass/ideal body weight.
Fig. 2.
Correlation between serum potassium levels and ultrafiltration volumes at peritoneal equilibration test (PET).
Fig. 3.
Correlation between serum potassium levels and serum albumin levels.
Fig. 4.
Correlation between serum potassium levels and 4-hour dialysate to plasma (D/P) creatinines.
Fig. 5.
Correlation between serum potassium levels and C-reactive protein levels.
3. Multivariate analysis of the factors associated with serum potassium levels
Multivariate stepwise linear regression analysis revealed that the serum potassium level was positively-correlated with the ultrafiltration volume at the PET (p=0.017) and serum albumin (p=0.029) after adjusted for factors accepted to be significant; 4-hour D/P creatinine, dialysate urea nitrogen losses, total CO2 level, dialysate creatinine clearance, dialysate protein losses, and LBMcr (Table 6).
Table 6.
Stepwise Multivariate Linear Regression Analysis of Factors Significantly Associated with Serum Potassium Levels in Patients
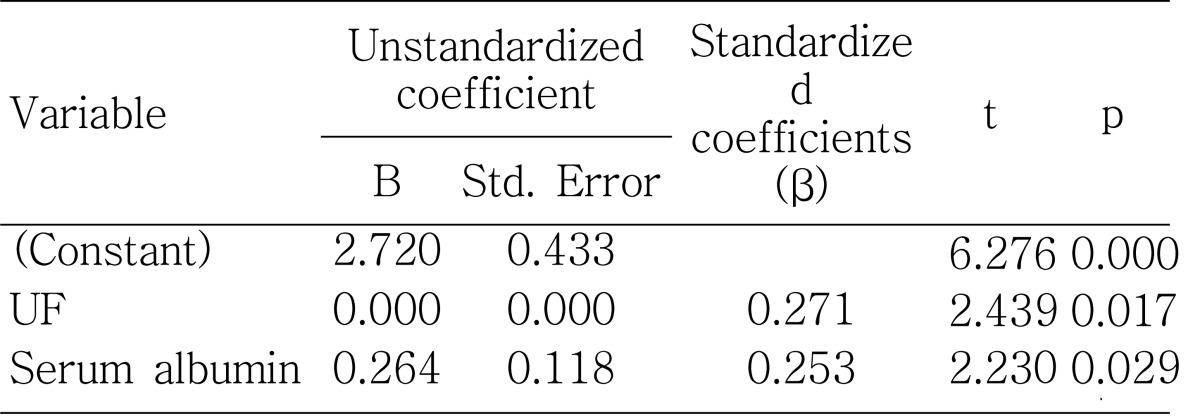
UF, ultrafiltration volume at the peritoneal equilibration test.
Discussion
The occurrence of hypokalemia is strongly dependent on the patient population. In otherwise healthy adults not receiving any medication, less than 1% will develop hypokalemia7). In CAPD patients, the prevalence of hypokalemia has been found to vary from the 10% to 36%8). It was reported that 10-15% of PD patients required potassium supplementation for hypokalemia9). In our study, the prevalence of hypokalemia in our center was about 10%, similar to previous studies9).
In patients on chronic dialysis, hypokalemia is induced by factors affecting internal and external potassium balance. The internal potassium balance includes reduced potassium uptake by cells because of uremia, acidosis, drugs, and alterations of the profile of hormones influencing potassium movement and it represents the potassium redistribution between the intracellular and the extracellular compartments. Compared to hemodialysis, peritoneal dialysis patients have a normal or even higher intracellular potassium content, especially those on CAPD. This phenomenon is probably related to continuous glucose absorption from the dialysis solutions and the subsequent stimulation of intracellular uptake of potassium, mediated by insulin release10). The external balance includes diminished or absent renal excretion, diminished dietary intake, and increased fractional excretion of potassium in the feces. The mode and frequency of dialysis also affected both internal and external potassium balance11). Considered from a standpoint of internal potassium redistribution, the trend of a higher frequency of hypokalemia in diabetic patients in our study is explained by the hypothesis that the insulin hormone stimulated by hyperglycemia together with the continuous peritoneal glucose absorption, could promote an excess of potassium redistribution into the intracellular compartment by activating N+ ,K+-ATPase, which results in active potassium uptake7). From the view of external balance, generally dialysis itself is the main source of external loss.
In CAPD, most dialysate solutions contain no potassium and patients dialyzed with such solutions lose 25-30 mEq of potassium per day via CAPD. Because this amount is relatively small when compared to the normal daily uptake (70-80 mEq)9), hypokalemia secondary to low potassium ingestion usually occurs only after an extended period of low oral potassium intake. It was reported that serum potassium levels in PD patients were not only associated with nutritional status or severity of coexisting comorbid conditions, but were also an independent prognostic indicator in PD patients2). In accordance with this report, we also found that hypokalemia levels were associated with poor nutritional indicators such as lower PNA, body mass index, LBMcr, and serum albumin level.
Protein equivalent of nitrogen appearance computed by urea kinetic modeling is known to reflect the dietary protein intake5), which is closely related to dietary potassium intake since dietary protein contains about 1 mEq of potassium per gram12). This study also revealed that dialysate urea nitrogen losses were significantly higher in the patients without hypokalemia. This can be probably explained by the nutritional aspect, because dialysate urea nitrogen loss is the main component of PNA. Some high potassium foods are also high in phosphorus; examples include corn, yogurt, milk, and beans13). Although not reaching statistical significance, the serum potassium level was associated with the serum phosphate level and also significantly associated with calcium-phosphate, indirectly suggesting that hypokalemic patients had an overall reduction in general oral intake.
Serum CRP is an acute-phase protein that is a marker for underlying systemic inflammation. The prevalence of an increased CRP and other pro-inflammatory cytokines (interleukin-1, interleukin-6 and tumor necrosis factor-α) was reported to be high in dialysis and pre-dialysis patients14). It is well documented that high levels of pro-inflammatory cytokines may cause muscle wasting by stimulating protein catabolism via the ubiquitin-proteosome pathway 15) and by inhibiting appetite16); they are also associated with a higher cardiovascular mortality in ESRD patients17). Qureshi et al. showed a close relationship between CRP and nutritional status as assessed by SGA (subjective global assessment)18). Noh et al. reported that serum CRP is an independent predictor of two-year patient survival in CAPD patients19). Recently, it was reported that malnutrition-inflammation scores including serum albumin level, total iron binding capacity level, BMI, etc. correlated significantly with clinical, nutritional, inflammatory, and anthropometric parameters in PD patients, even more strongly than SGA20). In our study, we also found that the patients with hypokalemia had a significantly higher CRP level; that level was negatively related to the serum albumin level (r=-0.29, p=0.07) (Fig. 3) and serum potassium level (r=-0.289, p=0.071) (Fig. 5), but these two correlations were not statistically significant. In addition, the higher levels of ferritin in the patients with hypokalemia in our study might also be explained in terms of an inflammatory marker.
The creatinine kinetic approach to lean body mass (LBM) estimation was reported to correlate well with other techniques for lean body mass, such as bioimpedance, infrared, and anthropometric measurements4). We found that the patients with hypokalemia had significantly lower LBM levels than those without hypokalemia and that serum potassium levels correlated significantly with LBM levels (r=0.31, p=0.01). The total amount of potassium in the plasma did correlate with total body potassium in normal subjects21), and was expected to bear close relationship to plasma potassium especially when maintained for sufficient time at steady levels 22). A decrease in total body potassium could either reflect a diminishing cellular mass, which is likely to be present in malnutrition, or a change in membrane function that is common in uremia23).
The ultrafiltration volume at the PET was significantly lower in patients with hypokalemia than those without hypokalemia (Table 2) and showed a positive correlation with serum potassium levels both significantly and independently (Fig. 2; Table 6), consistent with the significant negative correlation between serum potassium level and 4-hour D/P creatinine (Fig. 4). This is explained by both the higher rate of diffusive removal of potassium through the peritoneal membrane as a solute with a low molecular weight and the volume overload induced by the lower rate of fluid removal resulting from early loss of osmolar gradients. Cheng et al. also showed that there was a strong association between fluid status and nutritional status, and that volume overload is associated with the development of malnutrition with inflammation. Furthermore, improved fluid status was associated with improvement in nutritional status24). This can be interpreted by the hypothesis that volume overload might lead to gastrointestinal edema with poor nutritional status which results in bacterial and endotoxin translocation. This phenomena can elevate serum TNF-α and other inflammatory cytokines which induce anorexia by inhibiting the normal feeding response to energy deficits25). We also showed in our study that lower ultrafiltration volume at a PET with higher 4-hour D/P creatinine is associated with hypokalemia, probably reflecting volume overload with poor nutritional status. We did not find any correlation between serum potassium level and daily exchange volume or the dialysis adequacy index Kt/V, as with a previous study done by Szeto et al.2).
It has been well established that serum albumin level is a strong predictor of increased risk of morbidity and mortality in peritoneal dialysis patients26). The amount of albumin in the body and serum albumin concentration are determined by multiple factors including hepatic albumin synthesis (which is influenced by dietary protein intake), protein catabolism, and extravascular albumin distribution27). In addition to these factors, CAPD patients are uniquely susceptible to the adverse effects on levels of serum albumin because of protein losses into the peritoneal effluent. Our study showed that the patients with hypokalemia had significantly lower serum albumin levels than those without hypokalemia and that the serum albumin levels correlated significantly with serum potassium levels (r=0.31, p=0.01), even after adjustment by 4-hour D/P creatinine, total body water by the Watson method and dialysate albumin losses by partial correlation analysis (r=0.255, p=0.041). This suggests that none of the factors-potassium loss via the peritoneum as a small molecule or hypoalbuminemia caused by overhydration or excessive peritoneal loss of albumin can explain the relationship between serum albumin and potassium levels sufficiently. Stepwise multiple linear regression analysis also showed that serum albumin levels reveal independently-significant correlation with serum potassium levels (β=0.253, p=0.029), together with ultrafiltration volume at the PET (β=0.271, p=0.017) (Table 6). Higher levels of triglyceride, blood urea nitrogen, and serum creatinine in the patients without hypokalemia can also be explained by the common association with nutritional status.
In summary, we have shown that the patients with hypokalemia were associated with older age, higher CRP levels, and the presence of diabetes mellitus. Serum albumin, calcium-phosphate product, triglyceride, BMI, PNA, and LBMcr were significantly lower as compared to those without hypokalemia. The serum potassium level revealed significant positive correlation independently with ultrafiltration volume at the PET and serum albumin level. These results emphasize the importance of serum potassium level as a valid nutritional marker as well as a potential predictor of outcome. Further long-term follow up of a larger number of patients would be needed to clarify this relationship.
Table 4.
Urea Kinetic Parameters of the Patients with and without Hypokalemia
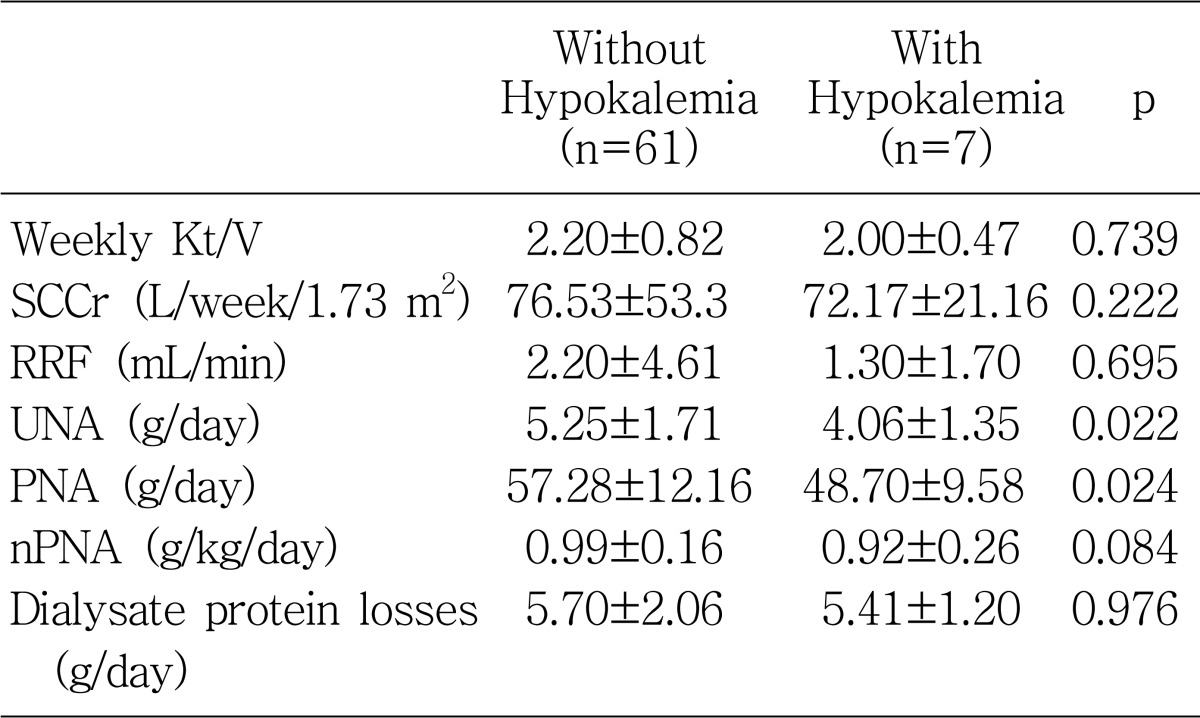
Values are expressed as mean±SD.
SCCr, standardized creatinine clearance; RRF, residual renal function; UNA, urea nitrogen appearance; PNA, protein equivalent of nitrogen appearance; nPNA, normalized PNA.
Acknowledgements
We would like to thank the nursing staff of the PD unit for inspiration and helpful discussions.
References
- 1.Khan AN, Bernardini J, Johnston JR, Piraino B. Hypokalemia in peritoneal dialysis patients. Perit Dial Int. 1996;16:652. [PubMed] [Google Scholar]
- 2.Szeto CC, Chow KM, Kwan BC, Leung CB, Chung KY, Law MC, Li PK. Hypokalemia in Chinese peritoneal dialysis patients: prevalence and prognostic implication. Am J Kidney Dis. 2005;46:128–135. doi: 10.1053/j.ajkd.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 3.Wang Z, Zhu S, Wang J, Pierson RN, Jr, Heymsfield SB. Whole-body skeletal muscle mass: development and validation of total-body potassium prediction models. Am J Clin Nutr. 2003;77:76–82. doi: 10.1093/ajcn/77.1.76. [DOI] [PubMed] [Google Scholar]
- 4.Keshaviah PR, Nolph KD, Moore HL, Prowant B, Emerson PF, Meyer M, Twardowski ZJ, Khanna R, Ponferrada L, Collins A. Lean body mass estimation by creatinine kinetics. J Am Soc Nephrol. 1994;4:1475–1485. doi: 10.1681/ASN.V471475. [DOI] [PubMed] [Google Scholar]
- 5.Bergstrom J, Furst P, Alvestrand A, Lindholm B. Protein and energy intake, nitrogen balance and nitrogen losses in patients treated with continuous ambulatory peritoneal dialysis. Kidney Int. 1993;44:1048–1057. doi: 10.1038/ki.1993.347. [DOI] [PubMed] [Google Scholar]
- 6.Twardowski ZJ, Nolph KD, Khanna R, Prowant BF, Ryan LP, Moore HL, Nielsen MP. Peritoneal Equilibration Test. Perit Dial Bull. 1987;7:138–147. [Google Scholar]
- 7.Weiner ID, Wingo CS. Hypokalemia-consequences, causes, and correction. J Am Soc Nephrol. 1997;8:1179–1188. doi: 10.1681/ASN.V871179. [DOI] [PubMed] [Google Scholar]
- 8.Tziviskou E, Musso C, Bellizzi V, Khandelwal M, Wang T, Savaj S, Oreopoulos DG. Prevalence and pathogenesis of hypokalemia in patients on chronic peritoneal dialysis: one center's experience and review of the literature. Int Urol Nephrol. 2003;35:429–434. doi: 10.1023/b:urol.0000022867.93739.03. [DOI] [PubMed] [Google Scholar]
- 9.Oreopoulos DG, Khanna R, Williams P, Vas SI. Continuous ambulatory peritoneal dialysis-1981. Nephron. 1982;30:293–303. doi: 10.1159/000182504. [DOI] [PubMed] [Google Scholar]
- 10.Musso CG. Potassium metabolism in patients with chronic kidney disease. Part II: patients on dialysis (stage 5) Int Urol Nephrol. 2004;36:469–472. doi: 10.1007/s11255-004-6194-y. [DOI] [PubMed] [Google Scholar]
- 11.Tzamaloukas AH, Avasthi PS. Temporal profile of serum potassium concentration in nondiabetic and diabetic outpatients on chronic dialysis. Am J Nephrol. 1987;7:101–109. doi: 10.1159/000167443. [DOI] [PubMed] [Google Scholar]
- 12.Rostand SG. Profound hypokalemia in continuous ambulatory peritoneal dialysis. Arch Intern Med. 1983;143:377–378. [PubMed] [Google Scholar]
- 13.Factor KF. Potassium management in pediatric peritoneal dialysis patients: can a diet with increased potassium maintain a normal serum potassium without a potassium supplement? Adv Perit Dial. 2007;23:167–169. [PubMed] [Google Scholar]
- 14.Stenvinkel P, Heimburger O, Lindholm B, Kaysen GA, Bergstrom J. Are there two types of malnutrition in chronic renal failure? Evidence for relationships between malnutrition, inflammation and atherosclerosis (MIA syndrome) Nephrol Dial Transplant. 2000;15:953–960. doi: 10.1093/ndt/15.7.953. [DOI] [PubMed] [Google Scholar]
- 15.Bistrian BR, Schwartz J, Istfan NW. Cytokines, muscle proteolysis, and the catabolic response to infection and inflammation. Proc Soc Exp Biol Med. 1992;200:220–223. doi: 10.3181/00379727-200-43423. [DOI] [PubMed] [Google Scholar]
- 16.Plata-Salaman CR, Peloso E, Satinoff E. Cytokine-induced fever in obese (fa/fa) and lean (Fa/Fa) Zucker rats. Am J Physiol. 1998;275:R1353–R1357. doi: 10.1152/ajpregu.1998.275.4.R1353. [DOI] [PubMed] [Google Scholar]
- 17.Zimmermann J, Herrlinger S, Pruy A, Metzger T, Wanner C. Inflammation enhances cardiovascular risk and mortality in hemodialysis patients. Kidney Int. 1999;55:648–658. doi: 10.1046/j.1523-1755.1999.00273.x. [DOI] [PubMed] [Google Scholar]
- 18.Qureshi AR, Alvestrand A, Danielsson A, Divino-Filho JC, Gutierrez A, Lindholm B, Bergstrom J. Factors predicting malnutrition in hemodialysis patients: a cross-sectional study. Kidney Int. 1998;53:773–782. doi: 10.1046/j.1523-1755.1998.00812.x. [DOI] [PubMed] [Google Scholar]
- 19.Noh H, Lee SW, Kang SW, Shin SK, Choi KH, Lee HY, Han DS. Serum C-reactive protein: a predictor of mortality in continuous ambulatory peritoneal dialysis patients. Perit Dial Int. 1998;18:387–394. [PubMed] [Google Scholar]
- 20.Afsar B, Sezer S, Ozdemir FN, Celik H, Elsurer R, Haberal M. Malnutrition-inflammation score is a useful tool in peritoneal dialysis patients. Perit Dial Int. 2006;26:705–711. [PubMed] [Google Scholar]
- 21.Boddy K, Hume R, White C, Pack A, King PC, Weyers E, Rowan T, Mills E. The relation between potassium in body fluids and total body potassium in healthy and diabetic subjects. Clin Sci Mol Med. 1976;50:455–461. doi: 10.1042/cs0500455. [DOI] [PubMed] [Google Scholar]
- 22.Patrick J. Assessment of body potassium stores. Kidney Int. 1977;11:476–490. doi: 10.1038/ki.1977.65. [DOI] [PubMed] [Google Scholar]
- 23.Cotton JR, Woodard T, Carter NW, Knochel JP. Resting skeletal muscle membrane potential as an index of uremic toxicity. A proposed new method to assess adequacy of hemodialysis. J Clin Invest. 1979;63:501–506. doi: 10.1172/JCI109328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cheng LT, Tang W, Wang T. Strong association between volume status and nutritional status in peritoneal dialysis patients. Am J Kidney Dis. 2005;45:891–902. doi: 10.1053/j.ajkd.2005.01.037. [DOI] [PubMed] [Google Scholar]
- 25.Aguilera A, Codoceo R, Selgas R, Garcia P, Picornell M, Diaz C, Sanchez C, Bajo MA. Anorexigen (TNF-alpha, cholecystokinin) and orexigen (neuropeptide Y) plasma levels in peritoneal dialysis (PD) patients: their relationship with nutritional parameters. Nephrol Dial Transplant. 1998;13:1476–1483. doi: 10.1093/ndt/13.6.1476. [DOI] [PubMed] [Google Scholar]
- 26.Kaysen GA. Biological basis of hypoalbuminemia in ESRD. J Am Soc Nephrol. 1998;9:2368–2376. doi: 10.1681/ASN.V9122368. [DOI] [PubMed] [Google Scholar]
- 27.Kaysen GA, Schoenfeld PY. Albumin homeostasis in patients undergoing continuous ambulatory peritoneal dialysis. Kidney Int. 1984;25:107–114. doi: 10.1038/ki.1984.15. [DOI] [PubMed] [Google Scholar]