Abstract
Although eating disorders (EDs) and ED symptoms are common among individuals in recovery for substance abuse (SA), long-term SA treatment programmes rarely address these problems. The present study examined the prevalence of EDs among women residing in Oxford Houses—low-cost, self-governed recovery homes for SA. Further, among women both with and without an ED diagnosis, the association between duration of Oxford House residency and eating-related self-efficacy scores was examined as an indicator of potential treatment effects on ED symptoms. During a telephone assessment, participants were administered the Structured Clinical Interview for DSM-IV-TR Axis I Disorders and the Eating Disorder Recovery Self-Efficacy Questionnaire. Results indicated that 12 of the 31 women analysed met criteria for an ED (bulimia nervosa, 2; ED not otherwise specified, 10). Differential findings were evident for eating-related self-efficacy measures depending on ED diagnostic status and duration of residency. Potential interpretations, limitations and implications are discussed.
Keywords: eating disorder, substance abuse, Oxford House, self-efficacy, recovery home
Introduction
It is common for individuals recovering from a substance use disorder (SUD) to experience additional psychiatric symptoms (e.g. Grant et al., 2004; Kushner, Sher, & Beitman, 1990) and diagnoses (e.g. Tomlinson, Tate, Anderson, McCarthy, & Brown, 2006). If left untreated, mental health disorders precipitate substance use (Zimmermann et al., 2003). Individuals in recovery appear to be particularly vulnerable to symptoms of eating disorders; weight concerns (Cowan & Devine, 2008), maladaptive eating behaviours (Hatcher, 2004; Hodgkins, Jacobs, & Gold, 2003; Jackson & Grilo, 2002) and excessive weight gain (Cowan & Devine, 2008) have all been documented among individuals recovering from an SUD. ED symptoms manifested as clinically significant disorders—particularly bulimia nervosa and binge eating disorder—also occur commonly among this population (Mitchell, Pyle, Specker, & Hanson, 1992).
Despite the risk of poor body image and maladaptive eating patterns among those recovering from an SUD, long-term treatment programmes often fail to address these issues. However, one unique model of recovery for SUDs that holds potential to allay these ED symptoms is Oxford House, a network of over 1,300 non-profit communal-living homes for men and women in recovery for drug and/or alcohol use problems. Oxford Houses are unique in that they are self-governed and have no professional staff involved in the operations of the recovery homes, which makes Oxford House more affordable as a treatment option. The treatment model is one of total abstinence; if a resident uses a substance while residing in an Oxford House, he or she is evicted until having completed another inpatient programme or, at minimum, completing detoxification (Oxford House, 2006). Although the Oxford House model does not provide formal treatment for co-occurring psychiatric conditions such as EDs, outside treatment is often encouraged among residents because the sole focus of these recovery homes is to provide an abstinent living environment (Oxford House, 2006).
Research investigating the Oxford House model suggests that living in such a democratic environment provides unique contingencies for behaviour change imposed by the group living there, which differ from professionally led treatment settings (Ferrari, Jason, Davis, Olson, & Alvarez, 2004). Furthermore, residing in such a setting might augment beneficial outcomes among individuals with comorbid psychiatric conditions (Majer, Jason, Ferrari, & North, 2002; Majer et al., 2008) and contribute to greater reductions in anxiety-related symptoms (Aase et al., 2006–2007). Research suggests that these benefits emerge when at least 6 months have elapsed (Aase et al., 2006–2007) and may occur through social support and self-efficacy mechanisms (Jason, Davis, & Ferrari, 2007).
Through these same mechanisms, Oxford House may also foster the improvement in ED-related symptoms. For example, if it is true that exchanges of social support among members includes support for appearance-related matters and social support leads to increases in self-efficacy, then it can be hypothesised that living within the Oxford House environment could help residents improve their body image self-efficacy—one’s confidence in maintaining both a reasonable body image not strongly influenced by the desire to be thin, and a self-esteem not affected excessively by weight or shape (Pinto, Guarda, Heinberg, & DiClemente, 2006). To further support this hypothesis, it has been documented that support from peers is often found to be more credible than support from mental health professionals (Thoits, 1986).
Similarly, normative eating self-efficacy may improve for members who struggle to engage in healthy eating behaviours. Normative eating self-efficacy refers to one’s confidence in being able to refrain from engaging in maladaptive eating behaviours (e.g. binge eating, purging, restricting) and from experiencing inappropriate negative emotions when eating and engaging in related activities (Pinto et al., 2006). In addition to verbally conveyed social support encouraging healthy eating patterns, support delivered through modelling of healthy eating behaviours may help those who struggle to gain confidence in their ability to achieve the same. Because Oxford Houses have shared eating facilities and discourage members from isolating themselves within the homes, the demonstration and observation of healthy eating behaviours are likely to occur naturally and frequently within this recovery setting.
Because body image and normative eating self-efficacy have been found to increase during treatment for an ED and predict treatment outcomes (Pinto, Heinberg, Coughlin, Fava, & Guarda, 2008), identifying treatments that are effective at treating SUDs and at raising these two types of self-efficacy may be beneficial to those with a co-occurring ED and SUD. To explore the possibility that the Oxford House model fits this treatment description, the current study investigated the association between duration of Oxford House residency and levels of eating-related self-efficacy among female residents both with and without an ED diagnosis. Based on prior research suggesting that individuals with an ED have lower self-efficacy on eating-related self-efficacy measures, and that a longer duration of residence (6 months or longer) in an Oxford House is associated with lower psychological symptoms, it was hypothesised that among those with an ED, those who have lived in an Oxford House for at least 6 months would have greater body image self-efficacy and normative eating self-efficacy than those who have resided in an Oxford House for less than 6 months.
A secondary goal of this research was to gain perspective on the rates of each type of ED among women recovering from a SUD in self-governed treatment settings and to compare the presentation of ED symptoms among these women to standard symptoms of SUDs. In the current study, this was achieved by utilising a widely accepted diagnostic interview based on Diagnostic and Statistical Manual on Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) criteria. If our hypotheses are supported, and EDs are found to be both prevalent and manifested in ways similar to that of SUDs, these data can be used to provide further evidence for the need and rationale of identifying SUD treatments that are also effective for ED symptoms.
Methods
Participants
Thirty-one women residing in Oxford Houses located throughout the USA participated in the current study. On average, participants reported living at Oxford House for 9.2 months (SD = 10.4; ranging from 0.2 to 45.5months). The sample had an average age of 41.2 years (SD = 9.5) and reported last using drugs or alcohol an average of 21.9 months ago (SD = 26.5; ranging from 0.7 to 143.0 months). Descriptive statistics for the sample are presented in Table 1.
Table 1.
Descriptive statistics for the full sample (n = 31)
| Characteristic | Mean (SD) or percentage |
|---|---|
| Age (years) | 41.19 (9.46) |
| Duration of Oxford House residence (months) | 9.17 (10.42) |
| Duration of sobriety (months) | 21.91 (26.54) |
| Reported drug(s) of choice† | |
| Alcohol | 38.7% |
| Narcotics | 16.1% |
| Stimulants | 71.0% |
| Marijuana | 16.1% |
| Polysubstance use | 38.7% |
| Presence of ED | |
| Anorexia nervosa | 0.0% |
| Bulimia nervosa | 6.5% |
| Binge eating disorder | 16.1% |
| Eating disorder NOS‡ | 16.1% |
| Experiences ED as a psychological dependence§ | 75.0% |
| Body Mass Index | 28.79 (7.44) |
| Average no. of weekly 12-step meetings | 3.45 (1.67) |
Note:
Percentages do not add up to 100 as some participants reported polysubstance use.
Other than binge eating disorder that meets full DSM-IV-TR research criteria.
Percentage based on those with an ED.
SD, standard deviation; ED, eating disorder; NOS, not otherwise specified.
Thirty-nine percent (n = 12) of the participants met the criteria for an ED at the time of the interview. Of these 12 individuals, two met full criteria for bulimia nervosa, whereas the remaining 10 were given a diagnosis of ED not otherwise specified (EDNOS). It is important to note that all 10 of these participants were experiencing binge eating, and five fully met the research criteria specified by the DSM-IV-TR for binge eating disorder. Of the 15 participants that had a duration of residency of less than 6months, five had an ED diagnosis. Of the 16 participants that had been residing at Oxford House for at least 6 months, seven had an ED diagnosis.
Seventy-five percent (n = 9) of those with an ED also endorsed three or more symptoms from the modified Structured Clinical Interview for DSM-IV-TR Disorders (SCID-I) criteria for substance dependence, suggesting that for these individuals, the ED may function similar to a substance dependence.
Materials
Demographic information
A series of questions were developed and administered to assess demographic characteristics. Variables utilised in the current study include age, duration of sobriety, duration of Oxford House residency, frequency of attendance of 12-step meetings and self-reported height/weight.
Structured clinical interview for DSM-IV-TR axis I disorders
The ED module of the SCID-I (First, Spitzer, Gibbon, & Williams, 2002) was administered to assess the participants for a diagnosis of anorexia nervosa, bulimia nervosa, binge eating disorder and EDNOS. The ED module of the SCID-I has demonstrated good reliability (Zanarini et al., 2000) and is widely utilised as a diagnostic tool. SCID-I assessments were conducted by the first author, a trained interviewer, and diagnostic agreement was 80% based on a random sample of interview transcripts evaluated by the second author. Consensus diagnoses were achieved for the 20% of cases that were initially disagreed upon utilising the following described processes. First, each coder reviewed the case independently and then presented his or her rationale for the originally selected diagnosis. Supporting evidence was provided from the transcription when appropriate. A short discussion followed, concluded with each coder stating his or her post-review diagnosis.
If binge eating was present, a modified version of the substance dependence module of the SCID-I was administered to assess whether the participants experienced binge eating similar to substance dependence. References to a ‘substance’ in the SUD module of the SCID-I were replaced with ‘binge eating’, as others have done (Cassin & von Ranson, 2007).
Eating disorder recovery self-efficacy questionnaire
The Eating Disorder Recovery Self-Efficacy Questionnaire is a psychometrically sound instrument (Pinto et al., 2006). It has demonstrated good predictive validity for normative eating self-efficacy and body image self-efficacy among individuals with EDs (Pinto et al., 2008). The present study utilised this instrument to assess these self-efficacy constructs as an indicator of convergent validity as well as an outcome variable. In the present study, Cronbach’s alphas for each subscale were in the acceptable range at ≥.85.
Procedure
Telephone numbers of Oxford Houses for women were obtained from a publicly available listing on the Oxford House, Inc. website (www.oxfordhouse.org). Based on this listing, individual Oxford Houses were randomly selected to be contacted regarding the study. Each of the selected recovery homes were contacted by telephone or mail to inform the residents about an opportunity to participate in a study about drug and alcohol use, body image and eating behaviours. During recruitment, prospective participants were also informed of the compensation awarded for study participation—an entry into a drawing for a small cash prize. Telephone interviews were scheduled with those who expressed an interest in participating and conducted upon obtaining verbal consent.
Statistical analyses
Correlations were conducted among the following primary continuous variables: duration of Oxford House residency, duration of sobriety, average number of weekly 12-step meeting (primarily Alcoholics Anonymous and Narcotics Anonymous meetings) attended, body mass index (BMI), average body image self-efficacy score and average normative eating self-efficacy score. The participants were grouped by ED diagnostic status (present, absent) and duration of residency (less than 6 months, 6 months or more) for analyses. Comparisons were made using t-tests for continuous variables and χ2 analyses for categorical variables.
Body image self-efficacy scores and normative eating self-efficacy scores were separately examined using a 2 × 2 [Residency (less than 6 months, 6months or more) × ED diagnosis (present, absent)] full factorial analysis of variance, and when interaction effects were significant, a simple main effects analysis controlled for number of comparisons using a Bonferroni adjustment. Duration of sobriety was employed as a covariate because of its potential influence on outcome variables.
Results
Descriptive statistics
Table 2 contains correlations among the primary continuous variables in the analysis. The primary outcome variables were average body image self-efficacy and average normative eating self-efficacy. There was a significant negative correlation between BMI and both the average number of 12-step meeting attended per week (p = .028) and body image self-efficacy (p = .011). There was a significant positive correlation between body image self-efficacy and both normative eating self-efficacy (p = .002) and duration of residence in Oxford House (p = .027).
Table 2.
Intercorrelations among primary continuous variables
| Measure | Residency | Sobriety | Attendance | BMI | BI-SE | NE-SE |
|---|---|---|---|---|---|---|
| Residency | – | – | – | – | – | – |
| Sobriety | .30 | – | – | – | – | – |
| Attendance | −.04 | −.21 | – | – | – | – |
| BMI | −.13 | .12 | −.39* | – | – | – |
| BI-SE | .40* | −.29 | .21 | −.45* | – | – |
| NE-SE | .21 | −.04 | .08 | −.03 | .55** | – |
Note:
Residency, duration of Oxford House residency; sobriety, duration of sobriety; attendance, average number of weekly 12-step meeting attended; BMI, body mass index; BI-SE, average body image self-efficacy score; NE-SE, average normative eating self-efficacy score.
p < .05.
p < .01.
Eating disorder diagnostic status
A comparison between the 12 participants with an ED and the 19 participants who did not have this diagnosis revealed no significant differences on the following variables: duration of sobriety, duration of residence in an Oxford House, polysubstance use status, average weekly 12-step attendance, BMI and age.
Self-efficacy
Body image self-efficacy
Eating disorder diagnostic status and duration of residency were tested as independent variables. Duration of sobriety was found to be a significant covariate, F(1, 26) = 11.46, p = .002, partial η2 = .31. There was a main effect of ED diagnostic status, such that women presenting with an ED (M = 2.29, standard error (SE) = .17) had significantly lower body image self-efficacy scores than women without this diagnosis (M = 3.17, SE = .14), F(1, 26) = 16.04, p < .001, partial η2 = .38. Women who lived in an Oxford House for at least 6 months (M = 3.03, SE = .15) had higher body image self-efficacy scores than women who had lived there for a shorter period (M = 2.42, SE = .16), F(1, 27) = 7.36, p = .012, partial η2 = .22. There was no significant interaction between the independent variables.
Normative eating self-efficacy
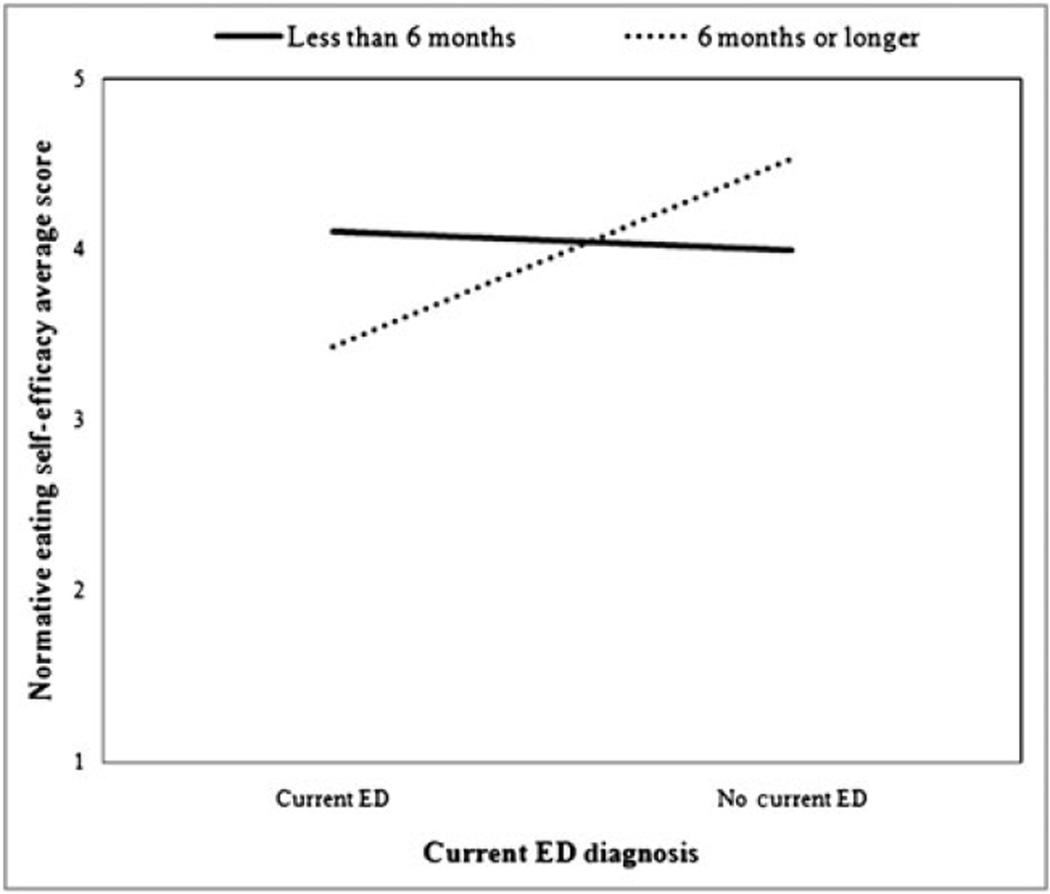
Results indicated that duration of sobriety was not a significant covariate. No main effect of duration of Oxford House residency or ED diagnostic status was found. However, women with an ED (M = 3.77, SE = .19) had directionally lower normative eating self-efficacy than women without this diagnosis (M = 4.25, SE = .15), F(1, 26) = 3.80, p = .062, partial η2 = .13. Further, there was a significant interaction between the independent variables. Among women who had lived in Oxford House for less than 6 months, individuals with an ED (M = 4.16, SE = .30) had similar levels of normative eating self-efficacy to individuals who did not (M = 3.84, SE = .22). However, among the women who lived in an Oxford House for at least 6 months, individuals without an ED had significantly higher levels of normative eating self-efficacy (M = 4.67, SE = .23) than individuals given this diagnosis (M = 3.38, SE = .35), F(1, 26) = 8.96, p < .01, partial η2 = .26 (Figure 1).
Figure 1.
The interaction between length of Oxford House residency and current eating disorder (ED) diagnosis on normative eating self-efficacy
Discussion
The primary purpose of the current study was to explore if there is evidence to suggest that residing in an Oxford House is beneficial in the reduction of ED symptoms among those with a co-occurring ED and SUD. This was accomplished by examining the association between duration of Oxford House residency and eating-related self-efficacy scores among women both with and without an ED diagnosis. The present study found that among a sample of women residing in self-governed recovery homes for SA, 39% met the criteria for an ED or EDNOS. Participants who both had an ED diagnosis and who had been living in an Oxford House for at least 6months reported the lowest levels of normative eating self-efficacy. Still, among all groups, normative eating self-efficacy was higher than observed in previous research, which has found comparatively lower levels among those with an ED (Pinto et al., 2006). Further, longer duration of residency in an Oxford House was associated with higher body image self-efficacy scores.
With regard to normative eating self-efficacy findings, over time, women with EDs residing in Oxford Houses may gain awareness that their eating behaviours are not normal but rather are maladaptive, and therefore may be more likely to report a lower self-efficacy for normative eating. Indeed, a significant minority of people with symptoms of disordered eating do not recognise their behaviours as problematic (Becker, Franko, Nussbaum, & Herzog, 2004). Further, comments by friends and others about one’s appearance and eating behaviours are important in the recognition of problematic eating behaviours (Hepworth & Paxton, 2007), paradoxically deleterious for normative eating self-efficacy. Residents who have been living in an Oxford House for at least 6months may have developed more and closer relationships with other Oxford House members than those living in an Oxford House for less than 6months. Therefore, it is possible that the women who have been living in these recovery homes longer might have not only received more of such comments overall, but might be receiving them at a higher rate compared with the women who have been living in an Oxford House for a shorter period. Considering the findings from Hepworth and Paxton (2007) discussed previously, these more numerous and frequent comments to women that have been residing in an Oxford House for longer duration may explain why, among residents with EDs, individuals who have lived in Oxford House for 6months or longer have, on average, a lower normative eating self-efficacy than their counterparts who have spent less time at these recovery homes. Alternatively, it is also possible that women with EDs identify more strongly with other Oxford House members who have EDs, and it is the lengthened exposure to the maladaptive eating behaviours engaged in by these women that diminishes their own confidence in abstaining from those behaviours.
The higher than expected levels of normative eating self-efficacy among those with EDs overall may be explained by the fact that binge eating disorder and subthreshold binge eating disorder were the most common ED in the current sample whereas approximately one-fifth of the items on the scale used to measure normative eating self-efficacy were more pertinent to anorexia nervosa and bulimia nervosa (e.g. ‘I can eat a cheeseburger without compensating by restricting, exercising excessively, or purging.’). These items may have inflated the scores of those with binge eating disorder and subthreshold binge eating disorder, which would explain why the mean normative eating self-efficacy among the sample of those with EDs was relatively high. This same effect may not have been replicated with the body image self-efficacy data because each item generally transcended disorders (e.g. ‘I can feel proud of how I look.’). A second possible explanation is that some of the individuals in the sample may not have been familiar with the terminology used in the measure to describe problematic eating behaviour. If residents with EDs become familiar with the terminology over time living at the Oxford House, this could also account for the unexpected nature of the interaction between length of residency and ED status on normative eating self-efficacy. Similarly, the higher than expected normative eating self-efficacy scores could also be explained by the participants’ lack of recognition of their own eating behaviours as problematic.
Unlike normative eating self-efficacy scores, body image self-efficacy levels were significantly higher for those living in an Oxford House for 6 months or longer, as predicted. This may suggest that the Oxford House environment promotes a healthy body image among its residents. One mechanism through which this change may occur is through increases in self-esteem. This hypothesis is based on research demonstrating Oxford House residents’ feelings that this recovery environment facilitates increases in their self-esteem (Alvarez, Jason, Davis, Ferrari, & Olson, 2004) along with findings that suggest, at least among adolescents, interventions that target self-esteem lead to improvements in body image (O’Dea & Abraham, 2000). An alternative explanation that may account for the current finding is that individuals who have resided in Oxford House for longer periods may be receiving more frequent positive comments regarding their appearance than their counterparts because of having more developed social support networks. Indeed, research has demonstrated that, among women, positive feedback regarding one’s appearance has a positive impact on body image (McLaren, Kuh, Hardy, & Gauvin, 2004), and there is some evidence to suggest that longer lengths of stay at Oxford House are associated with greater social support (Groh, Jason, Davis, Olson, & Ferrari, 2007).
The findings of the current study suggest that symptoms of EDs—particularly those related to having poor body image—may be quite prevalent among those recovering from SUDs, as indicative of the low average body image self-efficacy scores among both those with and without EDs. Furthermore, the high percentage (38.7%) of participants who met the criteria for an ED at the time of the interview suggests that this is a major issue for women in recovery from SUDs. Consistent with these findings, prior research suggests that rates of EDs among women seeking treatment for SUDs are high. Thus, it appears that these self-governed treatment settings have similar rates of EDs as women in more traditional treatment settings.
There are a number of limitations to the present study that warrant consideration. First, the small sample size presents restrictions for the external validity of the study and in the interpretations of statistical differences (and non-differences) because of a lack of sufficient power. As such, although significant findings and trends are interesting, further research is required to validate their quality. Furthermore, this exploratory study did not include a control or comparison group, which limits generalizability and internal validity. There also may have been a self-selection bias for participating given the nature of the interviews, although attempts were made to minimise this by describing the study without mentioning any specific problem or disorder. Finally, the study lacked information about past ED treatment and also utilised a diagnostic tool to evaluate binge eating disorder, which is not yet a formally recognised diagnosis.
However, despite these limitations, the results may hold clinical utility. The present findings suggest that young adult and middle-aged women in recovery from an SUD appear to be at a high risk for binge eating disorder. Thus, although additional research is needed, the current research may serve to demonstrate to clinicians treating this demographic the need to be aware of the risk and occurrence of such eating-related problems. In addition, the results of the current study may also serve to prompt future research to explore if group recovery settings help women with symptoms of EDs to recognise their unhealthy eating behaviour and what individual and environmental factors contribute to improve body image in such a setting.
Acknowledgements
Support for this research was provided by funding from DePaul University’s Undergraduate Research Assistant Program to Jennifer A. Czarlinski, NIDA grants DA13231 and DA19935, NIAAA grant AA16973 and the National Center on Minority Health and Health Disparities grant MD002748 to Leonard A. Jason. The authors would like to acknowledge Jesse Chavvaria, Melissa Halik and Alex LaMantia for their assistance with data collection and entry.
REFERENCES
- Aase DM, Jason LA, Ferrari JR, Groh DR, Alvarez J, Olson BD, et al. Anxiety symptoms and alcohol use: A longitudinal analysis of length of time in mutual help recovery homes. International Journal of Self Help and Self Care. 2006–2007;4:21–35. [Google Scholar]
- Alvarez J, Jason LA, Davis MI, Ferrari JR, Olson BD. Latinos and latinas in Oxford House: Perceptions of barriers and opportunities. Journal of Ethnicity in Substance Abuse. 2004;3:17–32. [Google Scholar]
- Becker A, Franko D, Nussbaum K, Herzog D. Secondary prevention for eating disorders: The impact of education, screening, and referral in a college-based screening program. International Journal of Eating Disorders. 2004;36:157–162. doi: 10.1002/eat.20023. [DOI] [PubMed] [Google Scholar]
- Cassin S, von Ranson K. Is binge eating experienced as an addiction? Appetite. 2007;49:687–690. doi: 10.1016/j.appet.2007.06.012. [DOI] [PubMed] [Google Scholar]
- Cowan J, Devine C. Food, eating, and weight concerns of men in recovery from substance addiction. Appetite. 2008;50:33–42. doi: 10.1016/j.appet.2007.05.006. [DOI] [PubMed] [Google Scholar]
- Ferrari JR, Jason LA, Olson BD, Davis MI, Alvarez J. Assessing similarities and differences in governance among residential recovery programs: Self versus staff rules and regulations. Therapeutic Communities: The International Journal for Therapeutic and Supportive Organizations. 2004;25:185–198. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition With Psychotic Screen (SCID-I/P W/PSY SCREEN) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiological Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Groh DR, Jason LA, Davis MI, Olson BD, Ferrari JR. Friends, family, and alcohol abuse: An examination of general and alcohol-specific social support. American Journal on Addictions. 2007;16:49–55. doi: 10.1080/10550490601080084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher AS. Weighty matters during recovery: Unhealthy eating behaviors can impede client progress. Addiction Professional. 2004;2:23–26. [Google Scholar]
- Hepworth N, Paxton S. Pathways to help-seeking in bulimia nervosa and binge eating problems: A concept mapping approach. International Journal of Eating Disorders. 2007;40:493–504. doi: 10.1002/eat.20402. [DOI] [PubMed] [Google Scholar]
- Hodgkins CC, Jacobs WS, Gold MS. Weight gain after adolescent drug addiction treatment and supervised abstinence. Psychiatric Annals. 2003;33:112–117. [Google Scholar]
- Jackson TD, Grilo CM. Weight and eating concerns in outpatient men and women being treated for substance abuse. Eating and Weight Disorder. 2002;7:276–283. doi: 10.1007/BF03324973. [DOI] [PubMed] [Google Scholar]
- Jason LA, Davis MI, Ferrari JR. The need for substance abuse after-care: Longitudinal analysis of Oxford House. Addictive Behaviors. 2007;32:803–818. doi: 10.1016/j.addbeh.2006.06.014. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Beitman BD. The relation between alcohol problems and the anxiety disorders. The American Journal of Psychiatry. 1990;147:685–695. doi: 10.1176/ajp.147.6.685. [DOI] [PubMed] [Google Scholar]
- Majer JM, Jason LA, Ferrari JR, North CS. Comorbidity among Oxford House residents: A preliminary outcome study. Addictive Behaviors. 2002;27:837–845. doi: 10.1016/s0306-4603(01)00214-3. [DOI] [PubMed] [Google Scholar]
- Majer JM, Jason LA, North CS, Ferrari JR, Porter NS, Olson B, et al. A longitudinal analysis of psychiatric severity upon outcomes among substance abusers residing in self-help settings. American Journal of Community Psychology. 2008;42:145–153. doi: 10.1007/s10464-008-9190-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaren L, Kuh D, Hardy R, Gauvin L. Positive and negative body-related comments and their relationship with body dissatisfaction in middle-aged women. Psychology & Health. 2004;19:261–272. [Google Scholar]
- Mitchell JE, Pyle RL, Specker S, Hanson K. Eating disorders and chemical dependency. In: Yager J, Gwirtsman HE, Edelstein CK, editors. Special problems in managing eating disorders. Washington, DC: American Psychiatric Press; 1992. pp. 1–14. [Google Scholar]
- O’Dea JA, Abraham S. Improving the body image, eating attitudes, and behaviors of young male and female adolescents: A new educational approach that focuses on self-esteem. International Journal of Eating Disorders. 2000;28:43–57. doi: 10.1002/(sici)1098-108x(200007)28:1<43::aid-eat6>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Oxford House, Inc. Oxford House Manual. Silver Spring, MD: Oxford House, Inc; 2006. (Commemorative Edition). [Google Scholar]
- Pinto AM, Guarda AS, Heinberg LJ, DiClemente CC. Development of the Eating Disorder Recovery Self-Efficacy Questionnaire. International Journal of Eating Disorders. 2006;39:376–384. doi: 10.1002/eat.20256. [DOI] [PubMed] [Google Scholar]
- Pinto AM, Heinberg LJ, Coughlin JW, Fava JL, Guarda AS. The Eating Disorder Recovery Self-Efficacy Questionnaire (EDRSQ): Change with treatment and prediction of outcome. Eating Behaviors. 2008;9:143–153. doi: 10.1016/j.eatbeh.2007.07.001. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Social support as coping assistance. Journal of Consulting and Clinical Psychology. 1986;54:416–423. doi: 10.1037//0022-006x.54.4.416. [DOI] [PubMed] [Google Scholar]
- Tomlinson KL, Tate SR, Anderson KG, McCarthy DM, Brown SA. An examination of self-medication and rebound effects: Psychiatric symptomatology before and after alcohol or drug relapse. Addictive Behaviors. 2006;31:461–474. doi: 10.1016/j.addbeh.2005.05.028. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, et al. The Collaborative Longitudinal Personality Disorders Study: Reliability of axis I and II diagnoses. Journal of Personality Disorders. 2000;14:291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]
- Zimmermann P, Wittchen HU, Höfler M, Pfister H, Kessler RC, Lieb R. Primary anxiety disorders and the development of subsequent alcohol use disorders: A 4-year community study of adolescents and young adults. Psychological Medicine. 2003;33:1211–1222. doi: 10.1017/s0033291703008158. [DOI] [PubMed] [Google Scholar]