Abstract
In the past several decades some risk factors for cardiovascular disease have improved, while others have worsened. For example, smoking rates have dropped and treatment rates for cardiovascular disease have increased--factors that have made the disease less fatal. At the same time, Americans’ average body mass index and incidence of diabetes have increased as the population continues to live longer--factors that have made cardiovascular disease more prevalent. To assess the aggregate impact of these opposing trends, we used the nine National Health and Nutrition Examination Survey waves from 1973 to 2010 to forecast total cardiovascular disease risk and prevalence from 2015 to 2030. We found that continued improvements in cardiovascular disease treatment and declining smoking rates will not outweigh the influence of increasing population age and obesity on cardiovascular disease risk. Given an aging population, an obesity epidemic, and declining mortality from the disease, the United States should expect to see a sharp rise in the health care costs, disability, and reductions in quality of life associated with increased prevalence of cardiovascular disease. Policies that target the treatment of high blood pressure and cholesterol and the reduction of obesity will be necessary to curb the imminent spike in cardiovascular disease prevalence.
US trends in cardiovascular disease over the past several decades tell two stories. One is encouraging: Age-adjusted rates for cardiovascular disease mortality declined from 517 per 100,000 in 1981 to 244 per 100,000 in 2008.(1) The second story, however, is sobering: Cardiovascular disease remains the leading cause of death and of health care costs in the United States.(2) Over the past twenty years the incidence and prevalence of cardiovascular disease appear to be steady or rising, based on events observed in large cohort studies and estimates from nationally representative surveys.(3–5) These opposing trends in mortality and nonfatal burden of cardiovascular disease can be at least partially explained by the improvements in treatment that have made cardiovascular disease less fatal but more prevalent.(6)
To reduce the incidence and prevalence of cardiovascular disease, prevention efforts should be intensified.(7) Intervening before initial or subsequent cardiovascular disease events occur could avoid substantial mortality, morbidity, and health care costs attributable to cardiovascular disease.
With these prevention-related goals in mind, the use of lipid-lowering and antihypertensive medication has increased over the past forty years, and blood pressure and cholesterol levels have declined as a result.(8–10) Smoking has also steadily decreased over the past forty years, which has led—and will continue to lead—to a decrease in mortality from cardiovascular disease.(11,12) Other risk factors, such as a high body mass index (BMI), diabetes, and advanced age, have increased over the same time period and could offset the gains from increased treatment and decreased smoking.(11,13)
We sought to model the net effect of risk-factor and treatment trends on the incidence and prevalence of cardiovascular disease in future years. For the purposes of our projections, we classified variables affecting cardiovascular disease as either “upstream” policy-dependent variables that can be affected by policy or “downstream” risk factors that can be altered by upstream variables. For example, a high cholesterol level is a downstream risk factor that directly affects the risk of cardiovascular disease, but it can be predicted by upstream variables such as diet and exercise (which are approximated by BMI and saturated fat consumption) and medication use.
Previous studies have examined national trends and provided projections of cardiovascular disease risk factors and mortality.(11,13–16) However, less attention has been paid to how changes in multiple risk factors would affect the incidence and prevalence of cardiovascular disease in future years.(17)
How transparent a projection model is—in other words, how many calculations, data sources, and assumptions it involves—is key to determining how useful it can be to policy makers and researchers.(18) Therefore, in this study we used a limited number of calculations and data sources, primarily focusing on data from the National Health and Nutrition Examination Surveys (NHANES), to project the impact of age and five “upstream” variables (antihypertensive and lipid-lowering treatment, smoking, BMI, and saturated fat consumption) on “downstream” risk factors (total and high-density lipoprotein [HDL] cholesterol, systolic blood pressure, and diabetes) that were used to predict the risk and prevalence of cardiovascular disease.
Study Data And Methods
Data And Analyses
We used nine cross-sectional data sets from NHANES to analyze sex-specific trends and projections of cardiovascular disease risk factors, treatment uptake, ten-year “total” risk (as defined by the Framingham cardiovascular disease risk equation), and prevalence. The Framingham risk score is widely used to predict an individual’s ten-year risk of cardiovascular disease (myocardial infarction, angina, coronary insufficiency, coronary heart disease death, transient ischemic attack, congestive heart failure, peripheral artery disease, or death from cardiovascular disease) based on commonly obtained risk factors.(19)
Risk-factor, treatment, and total risk trends from 1973 to 2010 were produced from the following nine NHANES data sets: NHANES I (1971–75), NHANES II (1976–80), NHANES III (1988–94), and six two-year waves of NHANES data from 1999–2000 through 2009–10. These data were also used to derive regressions that, in turn, were used to project each of the variables five, ten, fifteen, and twenty years into the future (2015–30). In addition to NHANES data, we used large meta-analyses of cholesterol and blood pressure treatment to incorporate into our model the effects of medication use on cholesterol and systolic blood pressure in 2015–30.(9,10,20)
Our observed trend analyses consisted of weighted population averages for age, smoking, diabetes (self-reported or based on laboratory testing), BMI, systolic blood pressure, saturated fat consumption, total and HDL cholesterol, and blood pressure and cholesterol treatment. Physical activity was not included as a risk factor because a high proportion of relevant data was missing and definitions of physical activity changed across NHANES waves.(21) These population averages were reported separately for each sex, adjusted using sample weights specific to the data set, and age-adjusted to the standard 2000 US population.
Averages not adjusted for age were also calculated to estimate the impact of population aging on risk trends for cardiovascular disease. For the period 2000–2010 only, because of questionnaire changes, the prevalence of cardiovascular disease was based on self-reported myocardial infarction, stroke, angina, congestive heart failure, or other coronary heart disease.
The aggregate study population across all NHANES waves consisted of 67,379 adults ages 25–85. Cholesterol treatment data were not collected in NHANES before the NHANES III population (1988–94). HDL cholesterol data were not available for people in the NHANES I cohort (1971–75) and were available for only 25 percent of the NHANES II population (1976–80). Because HDL cholesterol is an input for the Framingham cardiovascular risk score, we did not include these waves in any analyses of total cardiovascular disease risk.
For NHANES III and subsequent surveys, the information required to calculate risk of cardiovascular disease (age, smoking, diabetes, blood pressure treatment, systolic blood pressure, and total and HDL cholesterol) was available for 90.5 percent of the 42,755 adults in the study population.
Projections
Our projections for 2015–30 were informed by the NHANES data used in the observed trend analyses, US census data, and additional sources for treatment effects. Projections began with using census projections for age and sex distributions in 2015, 2020, 2025, and 2030 to generate representative populations of 100,000 hypothetical individuals at each point in time. These populations were treated as serial cross-sections—that is, the natural histories of these hypothetical individuals were not projected forward in time.
Once individuals in future years were assigned certain characteristics (starting with age and sex), they were sequentially given additional characteristics based on their existing profiles. For example, saturated fat consumption and smoking status were predicted based on a hypothetical individual’s age and sex. BMI was then predicted based on that individual’s age, sex, saturated fat consumption, and smoking status; diabetes was then predicted based on age, sex, and BMI; and so on. Cholesterol treatment, total and HDL cholesterol, blood pressure treatment, and systolic blood pressure estimates were sequentially projected for hypothetical individuals in all future cross-sections.
The functions used to predict these characteristics were based sex-specific regressions from the aggregate population of 67,379 adults in the observed NHANES data sets (1973–2010), with adjustment for sample weights. All continuous variables were transformed into their natural logarithms, and logistic regressions were used to generate probabilities for dichotomous variables (these probabilities were then used with random numbers to assign values of 1 or 0 to each individual). Prevalence projections for cardiovascular disease were based on total risk estimates and mortality trends for the disease. Online Appendixes A-1, A-2, and A-3 contain the details of the projection models based on sequential (weighted) regressions.(22)
Total risk and prevalence of cardiovascular disease were estimated for years in the trend (1973–2010) and projection (2015–30) analyses, which used published estimates to account for cholesterol and blood pressure treatment effects and compliance rates (as explained in Appendix A-1).(22) Projections were performed according to the base-case scenario, both with and without being adjusted for age, and the following alternative scenarios: one that held mortality from cardiovascular disease at 2010 levels (which affected only projections of cardiovascular disease prevalence); three scenarios that held upstream variables (smoking, BMI, and blood pressure and cholesterol treatment) at 2010 levels; one scenario that assumed a 50 percent reduction in treatment effectiveness because of noncompliance (the base-case scenario assumed a 25 percent reduction in effectiveness); and one scenario in which saturated fat consumption was reduced by 20 percent, the target set in Healthy People 2020.(23)
Projected risk estimates for cardiovascular disease in 2030 in these scenarios were compared to base-case projections using methods described in Appendix A-4.(22) Standard errors were not reported for absolute projections (as opposed to comparisons of risk projections of cardiovascular disease), which is consistent with other forecasting studies of cardiovascular disease.(11,24,25)
Limitations
Several limitations of our study should be noted. First, we limited our analysis to Framingham cardiovascular disease risk factors and BMI, saturated fat consumption, and treatment. We did not include other important lifestyle risk factors such as physical activity; broader social determinants such as education, stress, or poverty; or health outcomes such as morbidity or mortality from cancer or other conditions. Physical activity was not directly included in our analysis because of data limitations. The choice to limit our analysis to cardiovascular disease was driven partially by data availability (Framingham risk factors are routinely collected in all recent NHANES waves) and partially by our wish to use an established risk function (such as the Framingham risk factors) to estimate the aggregate impact of multiple risk factors.
Second, our observed trend analyses and projections were not stratified by socioeconomic status, race, or BMI. Previous studies have found that risk factors for cardiovascular disease progress or regress—that is, they change with age and over time periods—at different rates for certain subgroups.(8,24,26,27)
Third, our projection models that assigned cholesterol and blood pressure treatment were based on risk factors and variables included in our analyses (age, BMI, diabetes, smoking, and year) instead of on current and historical treatment guidelines.(28,29) Our rationale for doing this was because we wanted to project actual—not merely recommended—use of treatments for cardiovascular disease.(30,31)
Fourth, aspirin therapy was not included because of data limitations.(32) The use of aspirin treatment might increase in future years, as recommended by the Million Hearts Initiative.(33) Finally, our analyses were applied to people ages 25–85, although the Framingham risk equations were estimated based on people ages 30–74.(19)
Study Results
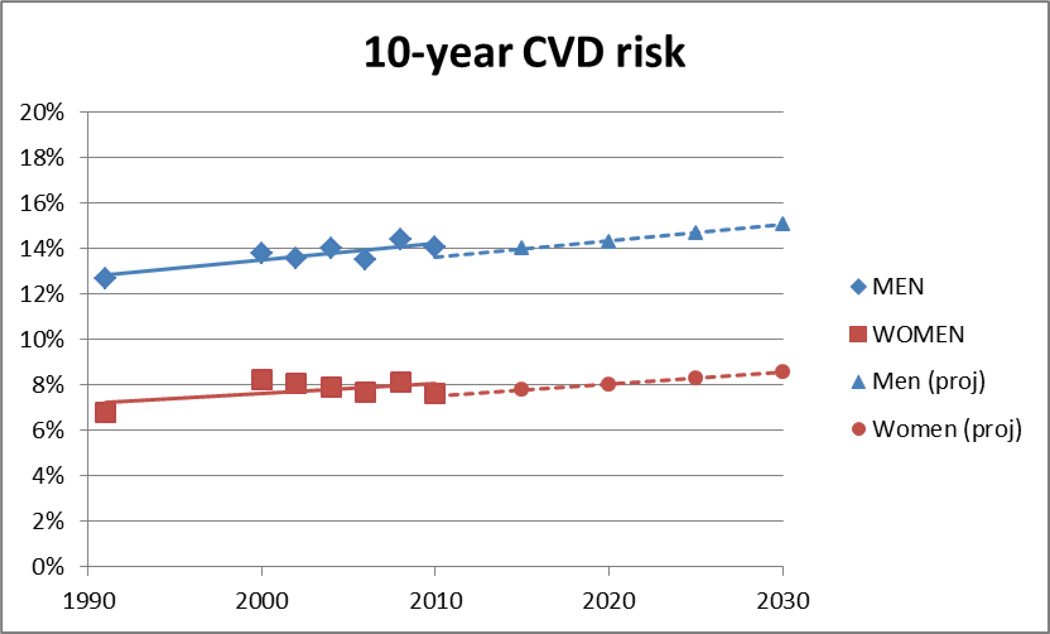
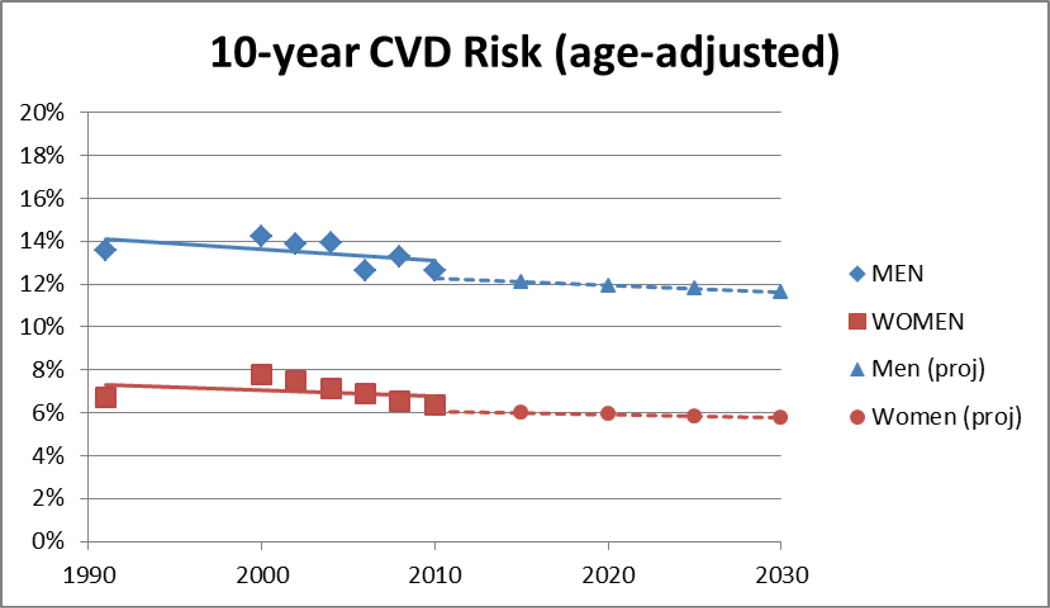
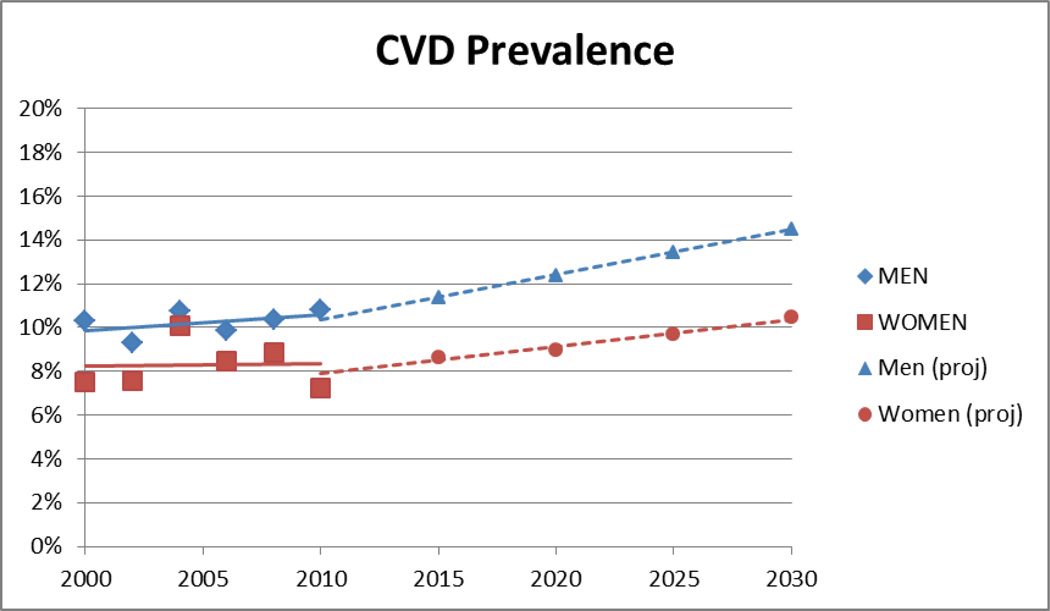
The average ten-year risk of cardiovascular disease in 1991 was 12.7 percent for men and 6.8 percent for women (Exhibit 1). By 2030 the risk is projected to rise to 15.1 percent and 8.6 percent, respectively. However, when we adjusted these averages for age (standardized to the 2000 US reference population), the risk declined from 1991 to 2030 for both men and women (Exhibit 2). The prevalence of cardiovascular disease (without adjusting for age) is projected to increase after 2010 in both men and women (Exhibit 3).
Exhibit 1.
Caption: Average Ten-Year Risk Of Cardiovascular Disease In The United States For Men And Women Ages 25–85, 1991–2010 And 2015–30
Source/Notes: SOURCES Authors’ calculations based on data from the National Health and Nutrition Examination Surveys for the trend analysis (1991–2010) and authors’ analysis for projections (2015–30). NOTE Linear trend lines added for trend analysis (solid lines) and projections (dotted lines).
Exhibit 2.
Caption: Age-Adjusted Average Ten-Year Risk Of Cardiovascular Disease In The United States For Men And Women Ages 25–85, 1991–2010 And 2015–30
Source/Notes: SOURCES Authors’ calculations based on data from the National Health and Nutrition Examination Surveys for trend analysis (1991–2010) and authors’ analysis for projections (2015–30). NOTE Linear trend lines added for trend analysis (solid lines) and projections (dotted lines).
Exhibit 3.
Caption: Prevalence Of Cardiovascular Disease In The United States For Men And Women Ages 25–85, 2000–10 And 2015–30
Source/Notes: SOURCES Authors’ calculations based on data from the National Health and Nutrition Examination Surveys for trend analysis (2000–10) and authors’ analysis for projections (2015–30). NOTE Linear trend lines added for trend analysis (solid lines) and projections (dotted lines).
Holding mortality from cardiovascular disease constant at the 2010 rate had a large impact on projected prevalence of cardiovascular disease for men and women (Exhibit 4). The scenario with constant mortality projected 26 percent and 16 percent lower mortality in 2030, respectively, than in the base-case scenario. In contrast, holding smoking or cholesterol treatment rates at 2010 levels increased risk and prevalence of cardiovascular disease compared to base-case assumptions, while holding BMI at 2010 levels decreased risk and prevalence of cardiovascular disease. Reducing treatment effectiveness because of reduced compliance increased risk of cardiovascular disease by 10 percent and 13 percent for men and women, respectively. Reducing saturated fat consumption did not significantly alter the risk or substantially affect the prevalence of cardiovascular disease.
Exhibit 4.
Projections Of Ten-Year Risk And Prevalence Of Cardiovascular Disease (CVD), According To Various Scenarios
| Men (%) | Women (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Scenario | 2015 | 2020 | 2025 | 2030 | 2015 | 2020 | 2025 | 2030 |
| Base case | ||||||||
| Risk | 14.0 | 14.3 | 14.7 | 15.1 | 7.8 | 8.0 | 8.3 | 8.6 |
| Prevalence | 11.4 | 12.4 | 13.4 | 14.5 | 8.6 | 9.0 | 9.7 | 10.4 |
| Base case, age adjusted | ||||||||
| Risk | 12.1 | 11.9 | 11.8 | 11.6 | 6.0 | 5.9 | 5.8 | 5.8 |
| Prevalence | 10.0 | 10.6 | 11.1 | 11.7 | 7.4 | 7.6 | 7.9 | 8.3 |
| Constant mortality ratea | ||||||||
| Prevalence | 10.0 | 10.4 | 10.5 | 10.7 | 7.9 | 7.9 | 8.2 | 8.7 |
| Constant smoking | ||||||||
| Risk | 14.2 | 14.7 | 15.2 | 15.7 | 7.9 | 8.2 | 8.5 | 8.7 |
| Prevalence | 11.5 | 12.7 | 13.8 | 15.0 | 8.6 | 9.0 | 9.8 | 10.7 |
| Constant BMI | ||||||||
| Risk | 13.4 | 13.5 | 13.7 | 13.9 | 7.7 | 7.7 | 8.0 | 8.1 |
| Prevalence | 11.0 | 11.9 | 12.5 | 13.5 | 8.3 | 8.7 | 9.4 | 10.1 |
| Constant cholesterol treatment | ||||||||
| Risk | 14.1 | 14.6 | 15.3 | 15.9 | 7.9 | 8.3 | 8.8 | 9.2 |
| Prevalence | 11.6 | 12.7 | 13.8 | 15.0 | 8.4 | 9.0 | 10.1 | 11.0 |
| Reduced treatment effectivenessb | ||||||||
| Risk | 14.9 | 15.4 | 16.0 | 16.6 | 8.4 | 8.8 | 9.2 | 9.7 |
| Prevalence | 12.2 | 13.3 | 14.5 | 15.8 | 9.0 | 9.5 | 10.5 | 11.6 |
| 20 percent reduced saturated fat consumption | ||||||||
| Risk | 13.9 | 14.2 | 14.6 | 15.0 | 7.8 | 8.0 | 8.3 | 8.6 |
| Prevalence | 11.3 | 12.4 | 13.2 | 14.4 | 8.5 | 8.9 | 9.7 | 10.4 |
SOURCE Authors’ projections based on census projections and nine waves of data from the National Health and Nutrition Examination Surveys, adjusted for cholesterol and blood pressure treatment. NOTES Men and women are ages 25–85. The scenarios are described in detail in the text. “Constant” means 2010 level was held constant. We tested for differences in ten-year CVD risk in 2030 for alternative scenarios compared to the base case for both men and women. The differences in all cases were significant (p < 0.001) except for the following: constant smoking for women (p = 0.147) and 20 percent reduced saturated fat consumption for men (p = 0.704) and women (p = 0.933). BMI is body mass index.
Constant mortality does not affect CVD risk.
Assumes 50 percent reduction in treatment effect (for cholesterol and blood pressure treatments) because of noncompliance (base-case scenario assumes only a 25 percent reduction).
Weighted regression results and observed weighted averages for each risk factor, treatment variable, and total risk estimate are displayed in Appendices A-1–A-5.(22) Appendix A-6 shows projections for risk factor and treatment variables.(34)
Discussion
In this study we used nine waves of NHANES data to analyze and project trends in risk factors, prevalence, and total (Framingham) risk of cardiovascular disease.(19) We chose to evaluate Framingham risk, which has not been the emphasis of previous studies, because it is a validated metric that can reflect the aggregate impact of various risk factors that change at different rates.
The net impact of the divergent trends in individual risk factors observed from 1973 to 2010 was that incidence of cardiovascular disease in the United States is likely to rise from 2015 to 2030. Age-adjusted risk projections of cardiovascular disease, however, are expected to decline over the same time period. The difference in these trends shows the overall impact that the aging population has had (and will continue to have, according to our projections) on total burden of cardiovascular disease. In other words, improvements in treatment of cardiovascular disease and smoking rates have not outweighed (and will not outweigh) the influence that rising age and obesity have had on increasing total risk of cardiovascular disease.
The prevalence of cardiovascular disease is affected by changes in incidence and mortality. We project that prevalence will rise because of increasing incidence of cardiovascular disease and longer duration of that disease, as a result of declining fatality rates. The prevalence projected for 2030 decreased by 27 percent in men and 16 percent in women when mortality was held at 2010 levels. Given an aging population, obesity epidemic, and declining mortality, the United States should expect to see a sharp rise in the health care costs, disability, and reductions in quality of life due to increases in the prevalence of cardiovascular disease.
The question of whether to make treatment or prevention of cardiovascular disease a higher priority has often been debated, and most researchers have suggested balanced approaches.(18) However, our findings suggest that substantial reductions in incidence are crucial: Otherwise, improvements in mortality from cardiovascular disease (along with aging and obesity trends) will lead to a troubling increase in prevalence.
Our projections for risk and prevalence of cardiovascular disease were most sensitive to the scenarios related to BMI and to blood pressure and cholesterol treatment. Holding BMI at its 2010 level would decrease prevalence of cardiovascular disease by 1.0 percentage point in men and 0.3 percentage point in women. Applying these increases to the total projected US population in 2030 (118 million men and 124 million women ages 25–85) implies that curbing obesity trends could mean that 1.6 million fewer people would have cardiovascular disease, compared to the base-case scenario.
Our scenarios also predict that if blood pressure and cholesterol treatment levels did not increase as predicted by current trends, 1.3 million additional people would have cardiovascular disease in 2030. Pessimistic assumptions of 50 percent compliance with treatment resulted in 3.0 million additional cases of cardiovascular disease in 2030, compared to the base-case assumption of 75 percent compliance.
Scenarios that involved optimistic (decreased) saturated fat consumption or pessimistic (constant) smoking levels in 2015–30 also affected risk and prevalence estimates of cardiovascular disease, but not to the same extent as the scenarios related to BMI and treatment described above. In a modeling study, Earl Ford and coauthors also found that the decline in mortality from coronary heart disease in 1980–2000 could be attributed primarily to improvements in cholesterol (which accounted for 24 percent of the decline), systolic blood pressure (20 percent), smoking prevalence (12 percent), and physical activity (5 percent).(35)
Previous studies have examined the trends and projections of cardiovascular disease risk factors, incidence, and mortality. However, none of these studies analyzed the relationship of these factors to projected prevalence of cardiovascular disease. Mark Huffman and colleagues used NHANES-based regressions to forecast a larger set of risk factors for cardiovascular disease (including diet and physical activity) in future years, but they did not project incidence or prevalence of cardiovascular disease as outcomes.(14) Richard Kahn and coauthors used the large-scale Archimedes microsimulation model to evaluate the impact of hypothetical prevention activities (including factors not considered in our analysis, such as aspirin use and diabetes management), but their forecasts did not account for continuing trends in BMI, smoking, or use of medication for cardiovascular disease.(15)
Paul Heidenrich and colleagues forecast the prevalence of the disease in 2010–30 based on observed and self-reported NHANES data with adjustments made for age, sex, and race.(25) In contrast, our projection methodology was based on forecasting changes in individual risk factors, which allowed us to evaluate scenarios that reflect targeted health policies or assumptions about specific risk factors.
Kirsten Bibbins-Domingo and coauthors used the Coronary Heart Disease Policy Model to forecast the impact of various obesity trajectories on future incidence, prevalence, and mortality of coronary heart disease, but these projections did not include trends in smoking or use of medication for cardiovascular disease.(17) Appendix A-9(22) contains descriptions of additional projection studies of cardiovascular disease (most of which focused on mortality), with comparisons to our analysis.
If mortality rates from cardiovascular disease continue to improve and people with the disease live longer, the United States will likely experience substantial increases in the cost and morbidity burdens from the additional people living with the disease. In addition, the incidence of cardiovascular disease is expected to increase in future years because of an aging population and increasing obesity rates.
These factors will speed up the increase in prevalence of cardiovascular disease, in spite of projected declines in age-adjusted incidence rates. The health policy and planning problems associated with this increased prevalence will be exacerbated by the expected shortage of primary care physicians.(36) The effect of this shortage could be mitigated by shifting cardiovascular disease screening and management tasks to mid-level providers, increasing coordination among primary care physicians to increase their capacity to see patients with cardiovascular disease, or providing financial incentives for specialists in cardiovascular disease to practice in rural and other underserved areas.(37,38)
Conclusion
Our analyses show the importance of curbing obesity and improving cholesterol and blood pressure treatment to reduce projected risk and prevalence of cardiovascular disease. Our base-case BMI projections were based on long-term trends (1973–2010), but adult obesity has been relatively stable in recent years—that is, in 2003–08 compared to 2009–10.(39) If BMI remained at 2010 levels, our analysis suggested that this could prevent more than a million cases of cardiovascular disease in 2030 and could significantly reduce the risk of cardiovascular disease.
To understand how best to address the epidemic of obesity, it is critical to study the possible explanations for the apparent stabilization of obesity in recent years. For example, is it a result of the cumulative effect of anti-obesity interventions? Or is it simply an artifact of recent data—that is, a temporary lull that is not indicative of a long-term trend of slowing obesity rates?(40)
Not enough of the population is receiving warranted treatment for high blood pressure or high cholesterol, according to clinically optimal or cost-effective treatment thresholds.(31,41–43) Medication compliance is also suboptimal, which is associated with substantial health and cost burdens.(44,45)
The Million Hearts Initiative,(33) a joint undertaking of the Department of Health and Human Services and other public and private partners, aims to increase access to blood pressure and cholesterol medications. The initiative also has projects to improve treatment compliance, such as the consistent reporting of simple blood pressure and cholesterol management quality measures. Additionally, the initiative stresses the use of health information technology to improve medication compliance via patient reminders.(33)
Furthermore, through incentivizing care coordination and quality and expanding access to health care services, the Affordable Care Act can facilitate the implementation of these and other prevention and treatment policies. The effectiveness of such polices will be instrumental in determining the ultimate prevalence and incidence of cardiovascular disease in the future, and their effects.(33)
We project that the prevalence of cardiovascular disease will increase as a result of the following three factors: the aging of the US population, continued declines in mortality from cardiovascular disease, and increasing rates of obesity and diabetes. In addition to planning how to meet anticipated provider workforce needs, policies targeted toward treatment of high blood pressure and cholesterol and reductions in obesity will be necessary to curb the imminent spike in prevalence of cardiovascular disease.
Supplementary Material
Acknowledgment
The authors gratefully acknowledge insightful feedback from four anonymous reviewers and journal editors.
Notes
- 1.National Center for Health Statistics. National Vital Statistics System data. Hyattsville (MD): NCHS; 2012. [Google Scholar]
- 2.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feinleib M, Kannel WB, Garrison RJ, McNamara PM, Castelli WP. The Framingham Offspring Study. Design and preliminary data. Prev Med. 1975;4(4):518–525. doi: 10.1016/0091-7435(75)90037-7. [DOI] [PubMed] [Google Scholar]
- 4.White AD, Folsom AR, Chambless LE, Sharret AR, Yang K, Conwill D, et al. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study: methods and initial two years’ experience. J Clin Epidemiol. 1996;49(2):223–233. doi: 10.1016/0895-4356(95)00041-0. [DOI] [PubMed] [Google Scholar]
- 5.National Center for Health Statistics. National Health and Nutrition Examination Survey data. Hyattsville (MD): NCHS; 2012. [Google Scholar]
- 6.Rosamond WD, Chambless LE, Folsom AR, Cooper LS, Conwill DE, Clegg L, et al. Trends in the incidence of myocardial infarction and in mortality due to coronary heart disease, 1987 to 1994. N Engl J Med. 1998;339(13):861–867. doi: 10.1056/NEJM199809243391301. [DOI] [PubMed] [Google Scholar]
- 7.Pearson TA. The prevention of cardiovascular disease: have we really made progress? Health Aff (Millwood) 2007;26(1):49–60. doi: 10.1377/hlthaff.26.1.49. [DOI] [PubMed] [Google Scholar]
- 8.Gregg EW, Cheng YJ, Cadwell BL, Imperatore G, Williams DE, Flegal KM, et al. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA. 2005;293(15):1868–1874. doi: 10.1001/jama.293.15.1868. [DOI] [PubMed] [Google Scholar]
- 9.Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366(9493):1267–1278. doi: 10.1016/S0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]
- 10.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. doi: 10.1136/bmj.b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stewart ST, Cutler DM, Rosen AB. Forecasting the effects of obesity and smoking on U.S. life expectancy. N Engl J Med. 2009;361(23):2252–2260. doi: 10.1056/NEJMsa0900459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Silverstein MD, Nietert PJ, Zoller JS, Silvestri GA. Predicted impact of attaining smoking reduction goals on mortality. South Med J. 2001;94(2):176–183. [PubMed] [Google Scholar]
- 13.Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352(11):1138–1145. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- 14.Huffman MD, Capewell S, Ning H, Shay CM, Ford ES, Lloyd-Jones DM. Cardiovascular health behavior and health factor changes (1988–2008) and projections to 2020: results from the National Health and Nutrition Examination Surveys. Circulation. 2012;125(21):2595–2602. doi: 10.1161/CIRCULATIONAHA.111.070722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kahn R, Robertson RM, Smith R, Eddy D. The impact of prevention on reducing the burden of cardiovascular disease. Circulation. 2008;118(5):576–585. doi: 10.1161/CIRCULATIONAHA.108.190186. [DOI] [PubMed] [Google Scholar]
- 16.Capewell S, Ford ES, Croft JB, Critchley JA, Greenlund KJ, Labarthe DR. Cardiovascular risk factor trends and potential for reducing coronary heart disease mortality in the United States of America. Bull World Health Organ. 2010;88(2):120–130. doi: 10.2471/BLT.08.057885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bibbins-Domingo K, Coxson P, Pletcher MJ, Lightwood J, Goldman L. Adolescent overweight and future adult coronary heart disease. N Engl J Med. 2007;357(23):2371–2379. doi: 10.1056/NEJMsa073166. [DOI] [PubMed] [Google Scholar]
- 18.Jones DS, Greene JA. The contributions of prevention and treatment to the decline in cardiovascular mortality: lessons from a forty-year debate. Health Aff (Millwood) 2012;31(10):2250–2258. doi: 10.1377/hlthaff.2011.0639. [DOI] [PubMed] [Google Scholar]
- 19.D’Agostino RB, Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117(6):743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 20.Wierzbicki AS, Mikhailidis DP. Beyond LDL-C—the importance of raising HDL-C. Curr Med Res Opin. 2002;18(1):36–44. doi: 10.1185/030079902125000165. [DOI] [PubMed] [Google Scholar]
- 21.Yang Q, Cogswell ME, Flanders WD, Hong Y, Zhang Z, Loustalot F, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307(12):1273–1283. doi: 10.1001/jama.2012.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 23.Washington (DC): Department of Health and Human Services; [cited 2012 Sep 12]. HealthyPeople.gov. 2020 topics and objectives: nutrition and weight status. [Internet] [last updated 2013 Aug 28; Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=29. [Google Scholar]
- 24.Wang YC, Colditz GA, Kuntz KM. Forecasting the obesity epidemic in the aging, US population. Obesity. 2007;15(11):2855–2865. doi: 10.1038/oby.2007.339. [DOI] [PubMed] [Google Scholar]
- 25.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123(8):933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 26.Harper S, Lynch J, Smith GD. Social determinants and the decline of cardiovascular diseases: understanding the links. Annu Rev Public Health. 2011;32:39–69. doi: 10.1146/annurev-publhealth-031210-101234. [DOI] [PubMed] [Google Scholar]
- 27.Dray-Spira R, Gary TL, Brancati FL. Socioeconomic position and cardiovascular disease in adults with and without diabetes: United States trends, 1997–2005. J Gen Intern Med. 2008;23(10):1634–1641. doi: 10.1007/s11606-008-0727-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Cholesterol Education Program (NCEP) Expert Panel on Detection Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–3421. [PubMed] [Google Scholar]
- 29.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 30.Gaziano JM, Gaziano TA. Simplifying the approach to the management of dyslipidemia. JAMA. 2009;302(19):2148–2149. doi: 10.1001/jama.2009.1685. [DOI] [PubMed] [Google Scholar]
- 31.Kuklina EV, Yoon PW, Keenan NL. Trends in high levels of low-density lipoprotein cholesterol in the United States, 1999–2006. JAMA. 2009;302(19):2104–2110. doi: 10.1001/jama.2009.1672. [DOI] [PubMed] [Google Scholar]
- 32.Slattery ML, Murtaugh MA, Quesenberry C, Caan BJ, Edwards S, Sweeney C. Changing population characteristics, effect-measure modification, and cancer risk factor identification. Epidemiol Perspect Innov. 2007;4:10. doi: 10.1186/1742-5573-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Frieden TR, Berwick DM. The “Million Hearts” initiative—preventing heart attacks and strokes. N Engl J Med. 2011;365(13):e27. doi: 10.1056/NEJMp1110421. [DOI] [PubMed] [Google Scholar]
- 34.Regressions that predicted saturated fat consumption, diabetes, cholesterol treatment, total cholesterol, and blood pressure treatment (women only) required calibrated regression intercepts (so that the predicted levels for these averages in 2010 match observed trends). Appendices A-7 and A-8 (see Note 22) show that results were robust to the following changes in modeling assumptions: performing projections without calibration adjustments limiting regressions to recent data (2000–10) using relative risks for cholesterol and blood pressure treatments instead of improvement in clinical values.
- 35.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356(23):2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 36.Foot DK, Lewis RP, Pearson TA, Beller GA. Demographics and cardiology, 1950–2050. J Am Coll Cardiol. 2000;35(4):1067–1081. doi: 10.1016/s0735-1097(00)00561-1. [DOI] [PubMed] [Google Scholar]
- 37.Green LV, Savin S, Lu Y. Primary care physician shortages could be eliminated through use of teams, nonphysicians, and electronic communication. Health Aff (Millwood) 2013;32(1):11–19. doi: 10.1377/hlthaff.2012.1086. [DOI] [PubMed] [Google Scholar]
- 38.Aneja S, Ross JS, Wang Y, Matsumoto M, Rodgers GP, Bernheim SM, et al. US cardiologist workforce from 1995 to 2007: modest growth, lasting geographic maldistribution especially in rural areas. Health Aff (Millwood) 2011;30(12):2301–2309. doi: 10.1377/hlthaff.2011.0255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 40.Olds T, Maher C, Zumin S, Péneau S, Lioret S, Castetbon K, et al. Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. Int J Pediatr Obes. 2011;6(5–6):342–360. doi: 10.3109/17477166.2011.605895. [DOI] [PubMed] [Google Scholar]
- 41.Pletcher MJ, Lazar L, Bibbins-Domingo K, Moran A, Rodondi N, Coxson P, et al. Comparing impact and cost-effectiveness of primary prevention strategies for lipid-lowering. Ann Intern Med. 2009;150(4):243–254. doi: 10.7326/0003-4819-150-4-200902170-00005. [DOI] [PubMed] [Google Scholar]
- 42.Lazar LD, Pletcher MJ, Coxson PG, Bibbins-Domingo K, Goldman L. Cost-effectiveness of statin therapy for primary prevention in a low-cost statin era. Circulation. 2011;124(2):146–153. doi: 10.1161/CIRCULATIONAHA.110.986349. [DOI] [PubMed] [Google Scholar]
- 43.Thorpe KE. The rise in health care spending and what to do about it. Health Aff (Millwood) 2005;24(6):1436–1445. doi: 10.1377/hlthaff.24.6.1436. [DOI] [PubMed] [Google Scholar]
- 44.Mazzaglia G, Ambrosioni E, Alacqua M, Filippi A, Sessa E, Immordino V, et al. Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation. 2009;120(16):1598–1605. doi: 10.1161/CIRCULATIONAHA.108.830299. [DOI] [PubMed] [Google Scholar]
- 45.Dragomir A, Côté R, White M, Lalonde L, Blais L, Bérard A, et al. Relationship between adherence level to statins, clinical issues and health-care costs in real-life clinical setting. Value Health. 2010;13(1):87–94. doi: 10.1111/j.1524-4733.2009.00583.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.