Abstract
Assessment of neck lymph nodes is essential in patients with head and neck cancers for predicting the patient’s prognosis and selecting the appropriate treatment. Ultrasonography is a useful imaging tool in the assessment of neck lymph nodes. Greyscale ultrasonography assesses the size, distribution, and internal architecture of lymph nodes. Doppler ultrasonography evaluates the intranodal vascular pattern and resistance of lymph nodes. Contrast-enhanced ultrasonography provides information on lymph node parenchymal perfusion. Elastography allows qualitative and quantitative assessment of lymph node stiffness. This article reviews the value of greyscale, Doppler and contrast-enhanced ultrasonography as well as elastography in the assessment of malignant nodes in the neck.
Keywords: Neck lymph nodes, ultrasonography, greyscale, Doppler, contrast enhancement, elastography
Introduction
Assessment of cervical lymph nodes is essential for patients with head and neck cancers for assessing the patient’s prognosis and selecting the appropriate treatment[1]. Regardless of the primary tumour, the presence of a unilateral metastatic cervical node reduces the 5-year survival rate by 50%, and the presence of bilateral metastatic cervical nodes further reduces the survival rate to 25%[2].
High-resolution ultrasonography has been used extensively in the assessment of cervical lymphadenopathy. Ultrasonography (97%) has higher sensitivity than palpation (73%) in the assessment of cervical lymph nodes, and has a high specificity (93%) when combined with ultrasound-guided fine-needle aspiration cytology (FNAC)[3]. Ultrasonography is particularly more sensitive than clinical examination in patients with previous head and neck cancer and post-radiotherapy neck fibrosis[4]. In addition, ultrasound-guided FNAC is more accurate than blind FNAC for distinguishing metastatic and benign cervical lymph nodes, with fewer false-negative (1% and 8%, respectively) and false-positive (1% and 5%, respectively) findings[5]. Greyscale ultrasonography can be used to assess the distribution and morphology of lymph nodes[6,7], whereas Doppler ultrasonography can be used to evaluate the distribution of intranodal vascularity and vascular resistance[8–12]. With the advent of elastography, the stiffness of cervical lymph nodes can now be estimated both qualitatively and quantitatively[13,14].
This article reviews the diagnostic value of different greyscale, Doppler and elastographic features of cervical lymph nodes in distinguishing metastatic and benign lymph nodes (Table 1).
Table 1.
Sonographic features of benign and malignant neck nodes
| Sonographic features | Benign nodes | Malignant nodes |
|---|---|---|
| Size | Persistent or slight changes in serial examinations | Increase in serial examinations |
| Shape | Elliptical (S/L <0.5) | Round (S/L >0.5) |
| Nodal border | Unsharp | Sharp. Proven malignant nodes with unsharp borders indicate extracapsular spread |
| Echogenic hilus | Present | Absent |
| Echogenicity | Hypoechoic | Hyperechoic in metastatic nodes from papillary thyroid carcinoma. Other malignant nodes tend to be hypoechoic |
| Intranodal reticulation | Absent | Common in lymphomatous nodes |
| Intranodal calcification | Absent | Punctate and peripherally located calcification is common in metastatic nodes from papillary thyroid carcinoma |
| Intranodal cystic necrosis | Common in tuberculous nodes | Common in metastatic nodes from papillary thyroid carcinoma and squamous cell carcinoma |
| Matting | Common in tuberculous nodes | May be found in patients with previous neck radiation therapy |
| Adjacent soft tissue oedema | Common in tuberculous nodes | May be found in patients with previous neck radiation therapy. May be found in malignant nodes with extracapsular spread |
| Intranodal vascular pattern | Hilar vascularity or apparently avascular | Peripheral or mixed vascularity |
| Stiffness | Soft | Hard |
Scanning techniques for cervical lymph nodes
There are over 300 lymph nodes in the neck. Therefore, a systematic scanning technique is needed to ensure ultrasound-detectable lymph nodes are not missed in the examination. For ultrasonographic examination of the neck, the patient lies supine with the neck hyperextended with a pillow or triangular soft pad under the patient’s shoulders and lower neck for support. The examination commences with a transverse scan of the submental region. The transducer is then swept laterally to either side of the neck with the patient’s head turned towards the contralateral side to ensure that the mandible does not hinder the free manipulation of the transducer. The submandibular region is examined with a transverse scan along the inferior border of the mandibular body. The transducer is angled cranially to examine submandibular nodes located in the submandibular niche behind the mandibular body. The transducer is then swept along the ramus of the mandible to assess the parotid nodes with longitudinal and transverse scans. The scanning is continued with examination of the internal jugular chain nodes, which are examined in transverse scans along the internal jugular vein and common carotid artery from the inferior end of the parotid gland to the junction between the internal jugular vein and the subclavian vein. The internal jugular chain nodes can be divided into upper cervical (above the level of the hyoid bone), middle cervical (between the level of the hyoid bone and cricoid cartilage) and lower cervical (below the level of cricoid cartilage) regions. From the lower cervical region, the transducer is then swept laterally to the supraclavicular fossa where the supraclavicular nodes are examined with transverse scans. The posterior triangle nodes are assessed with transverse scans from the mastoid tip and along the imaginary line of the spinal accessory nerve from the tip of the mastoid to the acromion process. The same scanning approach is used on the opposite side of the neck.
Sonographic features of cervical lymph nodes
Metastatic cervical lymph nodes from head and neck cancers are site specific. In patients with a known primary tumour, the specific distribution of metastatic nodes in the neck helps to identify metastases and aids tumour staging. When metastatic nodes are found at an unexpected site, the primary tumour is usually more biologically aggressive. Moreover, in patients with an unknown primary tumour, the distribution of metastatic cervical nodes may provide clues towards identifying the primary tumour[6,15,16]. The usual sites of nodal metastases for common head and neck cancers are[6,16–33]
tumours in the pharynx, larynx, oesophagus and papillary carcinoma of the thyroid: along the internal jugular chain
tumours in the oral cavity: submandibular and upper cervical regions (carcinoma of the tongue may show skip metastases to the lower neck)
infraclavicular carcinomas (breast and lung cancers): supraclavicular fossa and posterior triangle
nasopharyngeal carcinoma: upper cervical region and posterior triangle
Greyscale ultrasonography
Size
Nodal size used to be a criterion in distinguishing benign and malignant diseases[19,34–36]. Although malignant nodes tend to be larger, reactive lymph nodes can be as large as malignant nodes. In addition, lymph nodes with micrometastases may be small. Previous studies have reported different cut-off points for the maximum short axis axial diameter to differentiate malignant and benign lymph nodes (5, 8 and 10 mm)[36–40]. However, there is still no consensus on which cut-off point should be used in routine clinical practice. Van den Brekel et al.[41] noted that the optimal cut-off point of nodal size varies with the patient population, and they suggested that for any patient population the most acceptable size criterion is 9 mm for subdigastric nodes and 8 mm for other cervical lymph nodes.
In differentiating benign and metastatic lymph nodes, when a higher cut-off point of nodal size is used, the sensitivity of the size criterion decreases, whereas the specificity increases[42]. In our experience, nodal size is useful in routine clinical practice when lymph node size is monitored on serial ultrasonography examinations. In patients with a known primary tumour, an increase in nodal size on serial examinations is highly suspicious for metastases. In addition, a serial change in size of metastatic nodes is useful for monitoring patient response to treatment. For proven malignant nodes, a serial decrease in nodal size may indicate a positive treatment response[43].
Enlarged lymph nodes may compress the surrounding blood vessels and muscles in the neck. One should be cautious when assessing compressed vessels for vascular invasion.
Shape
Metastatic nodes tend to be round with a short axis to long axis ratio (S/L ratio) greater than 0.5 (Fig. 1), whereas reactive nodes are usually elliptical in shape with an S/L ratio smaller than 0.5[24,29,36,44–47]. Nevertheless, nodal shape should not be used as the sole criterion in the differential diagnosis because normal submandibular and parotid lymph nodes tend to be round[7].
Figure 1.
Transverse greyscale sonogram in a patient with carcinoma of the tongue shows a hypoechoic metastatic lymph node in the internal jugular chain. The lymph node is round in shape with well-defined borders and without an echogenic hilus (arrows).
Eccentric cortical hypertrophy of lymph nodes indicates focal intranodal tumour infiltration (Fig. 2), and is considered to be another useful feature to identify metastatic nodes[1]. In such cases, ultrasonography guides the needle towards the site within the node for biopsy.
Figure 2.
Longitudinal greyscale sonogram in a patient with carcinoma of the tongue shows a hypoechoic metastatic lymph node in the submandibular region. The lymph node is well defined and demonstrates eccentric cortical hypertrophy, which is related to focal tumour infiltration within the lymph node (arrows). Arrowheads indicate the intranodal echogenic hilus.
Nodal border
Metastatic lymph nodes usually have sharp borders, whereas benign nodes tend to have unsharp borders[22,38,46]. The presence of sharp borders in metastatic nodes is supposedly related to infiltrating tumour cells, which replace the normal intranodal lymphoid tissues, causing an increased difference in acoustic impedance between the intranodal tissue and surrounding soft tissues. The reduced fatty infiltration in the lymph node may also result in a greater acoustic impedance difference between the lymph node and surrounding tissues leading to sharp nodal borders[38]. However, proven metastatic lymph nodes with unsharp borders indicate extracapsular spread (Fig. 3), suggesting poor patient prognosis. Inflammatory nodes also cause peri-adenitis thus blurring the border between the nodes and surrounding soft tissues resulting in unsharp nodal borders (Fig. 4)[29].
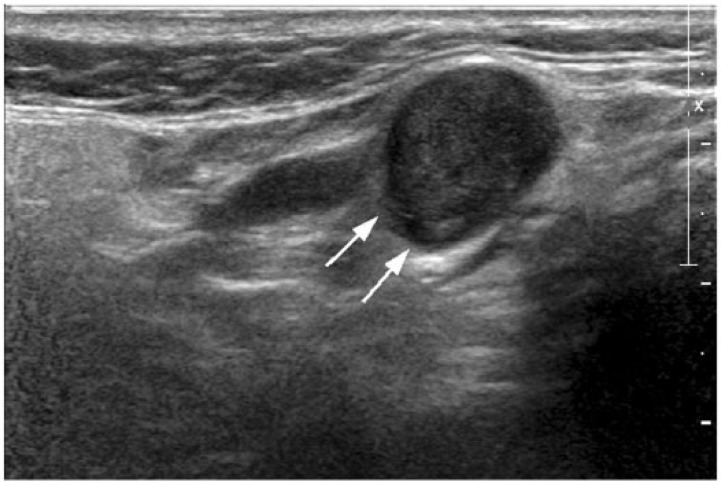
Figure 3.
Transverse greyscale sonogram in a patient with carcinoma of the larynx shows a hypoechoic metastatic lymph node in the internal jugular chain. The lymph node is round in shape with absence of echogenic hilus. The borders of the lymph node are ill defined indicating extracapsular spread (arrows). Note the tumour invasion into the adjacent soft tissues (arrowheads).
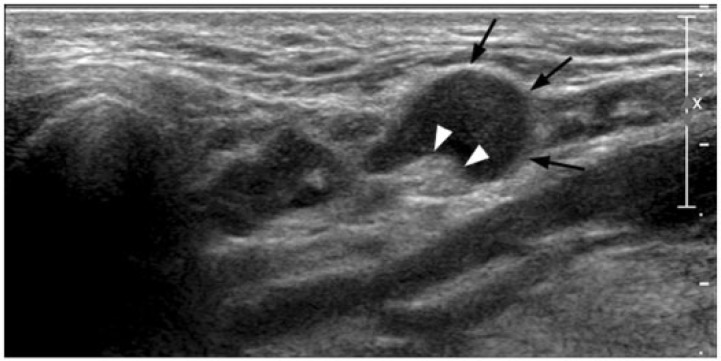
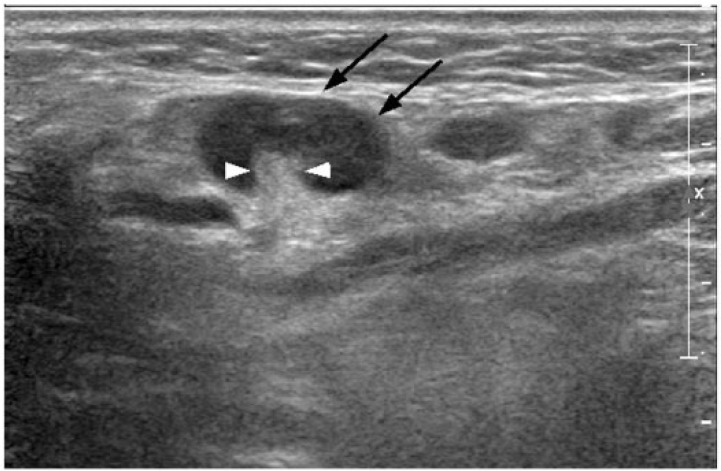
Figure 4.
Longitudinal greyscale sonogram in a patient with tuberculous lymphadenitis shows a hypoechoic necrotic tuberculous node with ill-defined borders and absence of echogenic hilus (arrows).
Echogenic hilus
The presence of an intranodal echogenic hilus was considered a sign of benignity[47–51]. Sonographically, the echogenic hilus appears as a hyperechoic linear structure continuous with the adjacent perinodal fat (Fig. 5). The multiple intranodal medullary sinuses act as acoustic interfaces and partially reflect the ultrasound waves to produce the echogenic appearance[45,48,49]. In the normal neck, using high-resolution ultrasonography, about 90% of lymph nodes with maximum transverse diameter greater than 5 mm show an echogenic hilus[52]. Previous studies have reported that 84–92% of benign nodes demonstrate an echogenic hilus[1,49]. However, 4–51.5% of metastatic nodes may also have an echogenic hilus[1,36,39,40,51]. Therefore, the presence/absence of an echogenic hilus within lymph nodes should not be the sole criterion in the evaluation of cervical nodes.
Figure 5.
Transverse greyscale sonogram in a patient with reactive lymphadenitis shows a reactive lymph node in the submandibular region (arrows). The lymph node is hypoechoic, oval shaped, with an echogenic hilus (arrowheads). Note the echogenic hilus is continuous with adjacent fat.
Echogenicity
Metastatic nodes tend to be hypoechoic compared with the adjacent muscles (Fig. 1)[24,53]. However, metastatic nodes from papillary carcinoma of the thyroid are usually hyperechoic (Fig. 6). The hyperechogenicity of the lymph nodes is believed to be due to the intranodal deposition of thyroglobulin originating from the thyroid primary tumour[30,54]. Therefore, in patients with an unknown primary, the presence of hyperechoic lymph nodes should direct the sonologist to evaluating the thyroid gland in closer detail.
Figure 6.
Transverse greyscale sonogram in a patient with papillary carcinoma of the thyroid shows a metastatic lymph node in the internal jugular chain (arrows). The lymph node is round, well defined and hyperechoic compared with the adjacent muscle. Note the intranodal calcification, which is echogenic and punctuate (white arrowhead). The black arrowheads indicate the common carotid artery.
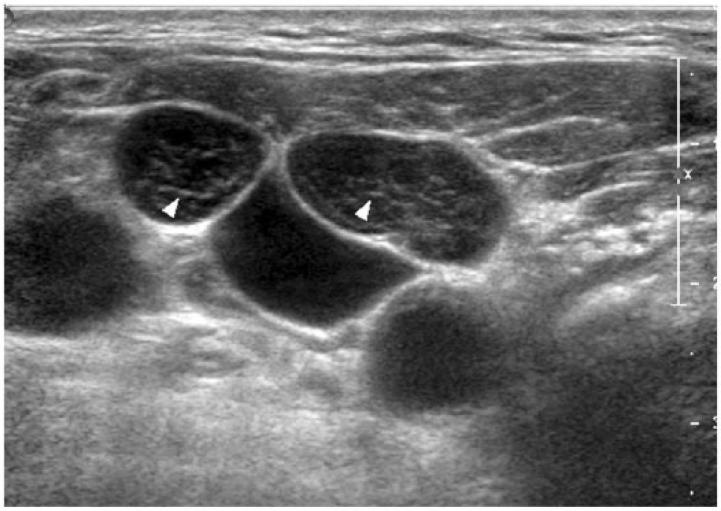
In the past, lymphomatous nodes were described as hypoechoic with posterior enhancement, i.e. the pseudocystic appearance[33,55,56]. However, the newer high-resolution transducers allow better interrogation of intranodal tissues and lymphomatous nodes demonstrate intranodal reticulation rather than the pseudocystic appearance (Fig. 7)[57].
Figure 7.
Transverse greyscale sonogram in a patient with non-Hodgkin lymphoma shows multiple lymphomatous nodes in the internal jugular chain. The lymph nodes are well defined, hypoechoic with intranodal reticulation (arrowheads).
Calcification
Intranodal calcification is generally rare in metastatic lymph nodes, but is a relatively common feature in metastatic nodes from papillary carcinoma and medullary carcinoma of the thyroid[2,6,15,30,58]. About 50–69% of metastatic nodes from papillary carcinoma of the thyroid have intranodal calcification (Fig. 6). The calcification in these lymph nodes is usually punctate and peripherally located with fine threads of acoustic shadow when a high-resolution transducer is used[6,30]. However, in our experience with modern multiple beam transducers, the posterior shadowing may be difficult to appreciate. Reverting back to the fundamental scan (easily done by using the greyscale feature in Doppler ultrasonography) better demonstrates the linear posterior shadowing. The high incidence of intranodal calcification in metastatic nodes from papillary carcinoma of the thyroid makes this feature useful in assessing the nature of the lymphadenopathy. Calcification may also be found in metastatic lymph nodes from medullary carcinoma of the thyroid but the incidence is relatively lower. It has been reported that when a medullary thyroid cancer is surgically removed, the recurrent cervical nodes usually have calcification[58]. The calcification in metastatic nodes from medullary carcinoma is relatively coarse and shows posterior shadowing (compared with the calcification in papillary carcinoma metastases). Intranodal calcification may also be found in irradiated metastatic lymph nodes and lymphomatous nodes after chemotherapy, and often in post-treatment tuberculous nodes in the neck.
Intranodal necrosis
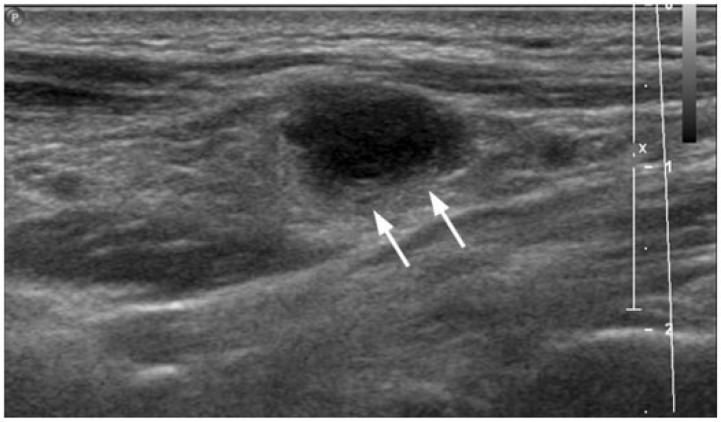
Intranodal necrosis is a late event in tumour infiltration of lymph nodes, and may appear as a cystic area (cystic or liquefaction necrosis) or an echogenic focus (coagulation necrosis) within the lymph node. Cystic necrosis appears as an echolucent area within the lymph node, and is common in metastatic nodes from papillary carcinoma of the thyroid, squamous cell carcinomas, as well as tuberculous nodes (Fig. 8)[6,24,29,30,46,47,59–63]. Coagulation necrosis is relatively less common and appears as an echogenic area within lymph nodes that is not continuous with the surrounding fat and does not produce an acoustic shadow[49,50]. Regardless of the nodal size, lymph nodes with intranodal necrosis are considered pathologic.
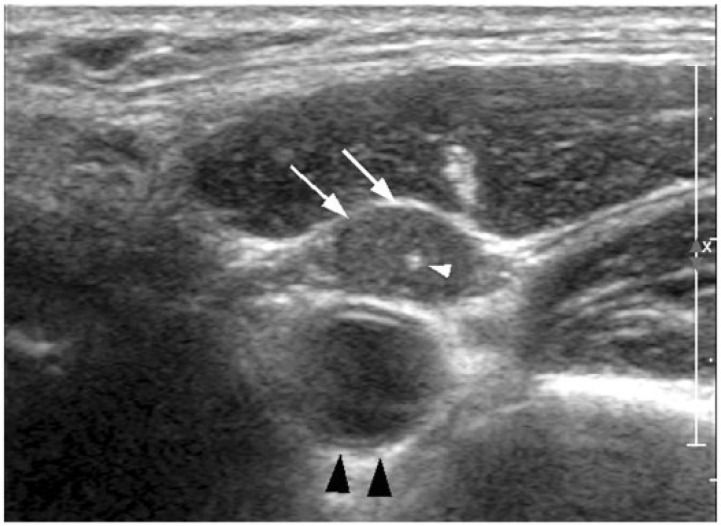
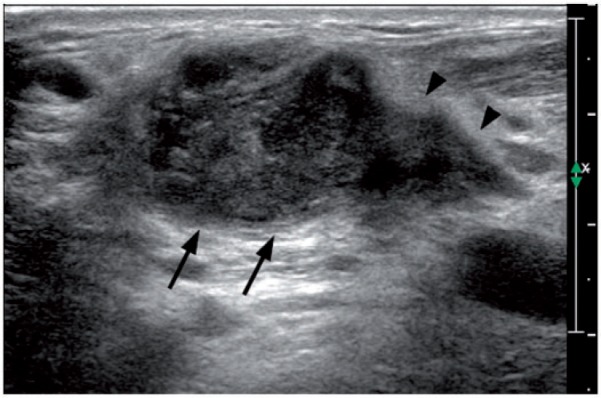
Figure 8.
Transverse greyscale sonogram in a patient with carcinoma of the larynx shows multiple hypoechoic metastatic lymph nodes in the internal jugular chain (arrows). The lymph nodes are round in shape with intranodal cystic necrosis (arrowheads), commonly seen in metastatic nodes from squamous cell carcinoma.
Ancillary features
Matting and adjacent soft tissue oedema are common in tuberculous lymph nodes because of the perinodal inflammatory reaction (periadenitis)[29,46]. However, metastatic nodes with extracapsular spread can invade adjacent soft tissues leading to tissue oedema. In addition, post-radiation soft tissue oedema and nodal matting may also be found in patients with previous radiation therapy of the neck[64].
Doppler ultrasonography
Intranodal vascular pattern
It has been reported that power Doppler ultrasonographic evaluation of the vascular pattern of cervical nodes is highly reliable with a repeatability of 85%[65]. In the normal neck, about 90% of lymph nodes with maximum transverse diameter greater than 5 mm show hilar vascularity[52]. Normal and reactive lymph nodes tend to demonstrate hilar vascularity or appear apparently avascular[10–12,36,66]. However, metastatic lymph nodes usually have a peripheral (Fig. 9) or mixed (hilar + peripheral) vascularity[9,10,12,46,47,66,67]. Unlike metastatic nodes, lymphomatous nodes tend to have mixed vascularity (Fig. 10) and isolated peripheral vascularity is uncommon[68]. The relatively high incidence of hilar vascularity in lymphomatous nodes is believed to be due to the fact that keratinization and intranodal necrosis are rare in lymphoma and thus the hilar vessels of the lymph nodes are preserved[69]. The presence of peripheral vascularity in malignant nodes is thought to be related to tumour angiogenesis and the associated recruitment of capsular vessels[10,12,66,67]. Because peripheral vascularity is common in malignant nodes, its presence, regardless of the presence or absence of hilar vascularity, is highly suggestive of malignancy.
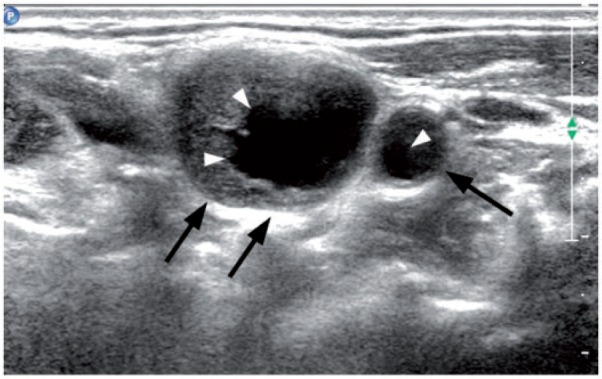
Figure 9.
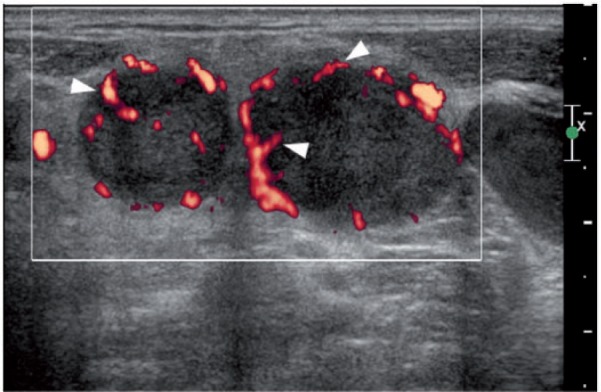
Transverse power Doppler sonogram in a patient with lung carcinoma shows multiple metastatic lymph nodes in the supraclavicular fossa. The lymph nodes are round in shape with peripheral vascularity (arrowheads).
Figure 10.
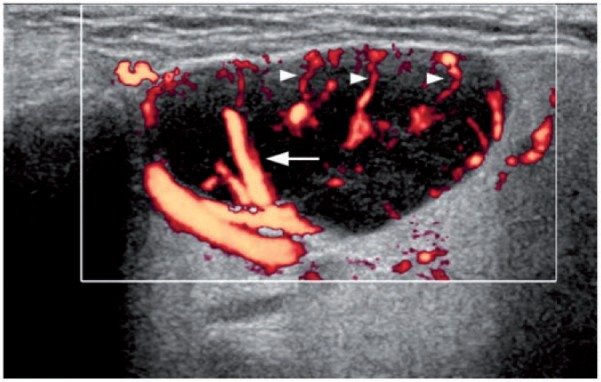
Longitudinal power Doppler sonogram in a patient with non-Hodgkin lymphoma shows a hypoechoic lymphomatous node in the submandibular region. The lymph node is oval in shape with both peripheral (arrowheads) and hilar (arrow) vascularity.
Power Doppler ultrasonography evaluation of nodal vascular pattern has been reported to have high sensitivity (83–89%) and specificity (87–100%) for differentiating metastatic and reactive nodes[10,12,68]. In distinguishing lymphomatous and reactive nodes, the sensitivity and specificity are 67% and 100%, respectively[68].
In our experience, power Doppler ultrasonography assessment of cervical nodes may not be necessary for every case in routine clinical practice because greyscale ultrasonography already has high sensitivity (95%) and specificity (83%) in differentiating metastatic and non-metastatic nodes[70]. However, power Doppler ultrasonography is useful in patients for whom greyscale ultrasonography is equivocal, and it improves diagnostic accuracy[70].
Intranodal vascularity has been used in the evaluation of treatment response. For patients with non-Hodgkin lymphoma on chemotherapy, reduced intranodal vascularity is a positive sign of good treatment response, whereas lymph nodes with persistent vascularity during the course of chemotherapy tend to have poor clinical outcome[43].
Intranodal vascular resistance
Using spectral Doppler ultrasonography, the vascular resistance (resistive index (RI) and pulsatility index (PI)) of the intranodal vessels can be estimated (Fig. 11). However, the role of vascular resistance in distinguishing malignant and benign nodes remains controversial and inconsistent. It has been reported that the RI and PI of metastatic nodes are higher than those of reactive nodes[12,46,66,67,71,72]. However, other studies suggest that metastatic nodes may have lower or similar vascular resistance compared with benign lymph nodes[73,74]. Previous studies recommended different cut-off of RI (0.6, 0.7 and 0.8) and PI (1.1, 1.5 and 1.6) for distinguishing metastatic and reactive nodes with different sensitivities (RI, 47–81%; PI, 55–94%) and specificities (RI, 81–100%; PI, 97–100%)[12,66,67,73]. In our experience, we found that the optimal cut-offs for RI and PI for differentiating metastatic and reactive nodes were 0.7 and 1.4 with a sensitivity of 86% and 80%, respectively, and a specificity of 70% and 86%, respectively[9]. Because of the inconsistent results in previous reports and poor repeatability, the value of spectral Doppler ultrasonographic evaluation of intranodal vascular resistance is limited in routine clinical practice.
Figure 11.
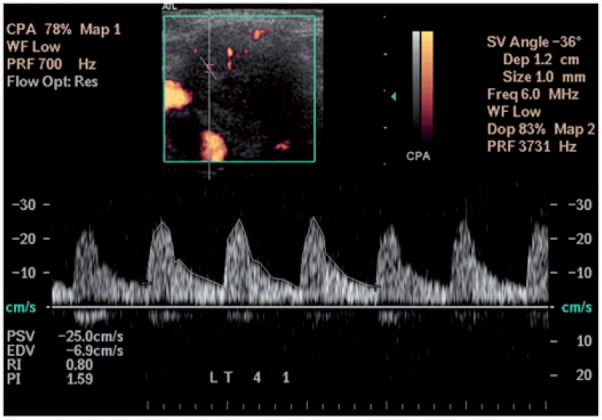
Spectral Doppler sonogram in a patient with carcinoma of the pharynx shows measurement of the resistive index (RI) and pulsatility index (PI) as well as the peak systolic velocity (PSV) and end diastolic velocity (EDV) of a metastatic lymph node in the internal jugular chain. The measurements are obtained from three consecutive waveforms.
Elastography
Basic principles
Elastography can generally be classified into qualitative and quantitative assessments. Using qualitative real-time ultrasound elastography, a compression force is applied to the region of interest (ROI) to measure its stiffness. The stiffness of the ROI is estimated by evaluating the degree of local tissue displacements before and after the compression force is applied. For quantitative assessment, the stiffness of the ROI can be quantified by conventional strain elastography using the strain index or by shear wave elastography (SWE). On conventional strain elastography, the strain of the soft tissues can be estimated by customized software. When examining neck lymph nodes, the strain index (also known as the strain ratio) is calculated as the ratio of the strain of neck muscle to the strain of lymph node[36,40,75]. SWE is a recent development in soft tissue elasticity imaging. Using a focused ultrasound beam, acoustic radiation force impulses are applied to the soft tissues and shear waves are generated. With the use of ultrafast ultrasound tracking techniques, the speed of the shear wave propagation is measured and the stiffness (elastic modulus) of the soft tissue is obtained. SWE allows absolute quantification of the soft tissue stiffness presented in kilopascals or measured as the shear wave in metres per second.
Qualitative assessment
On qualitative real-time ultrasound elastography, the lymph nodes and other soft tissues are colour coded and the colours represent different stiffness of the tissues. To evaluate the stiffness of the lymph nodes, elastograms are usually classified into 4 to 5 grades according to the proportion of hard area within the lymph node[14,40,51,75]. Previous studies suggest benign lymph nodes tend to be soft, whereas malignant lymph nodes are usually hard (Figs. 12 and 13)[14,40,51,75]. When distinguishing benign and malignant nodes, the reported sensitivity, specificity and accuracy of qualitative real-time ultrasound elastography are 62.2–88.4%, 35.3–100% and 66.3–89%, respectively[14,40,51]. When qualitative elastography is combined with greyscale ultrasonography, the sensitivity, specificity and accuracy are 92%, 94% and 93%, respectively[51]. However, a recent study reported that lymphomatous nodes (100% at score 2 in a 4-score classification method) tend to be softer than metastatic nodes (74.5% at score 3 or 4), and have a similar elastographic score to benign nodes (87.9% at score 1 or 2). Therefore, lymphomatous and benign nodes could not be distinguished according to the elastographic score alone[75].
Figure 12.
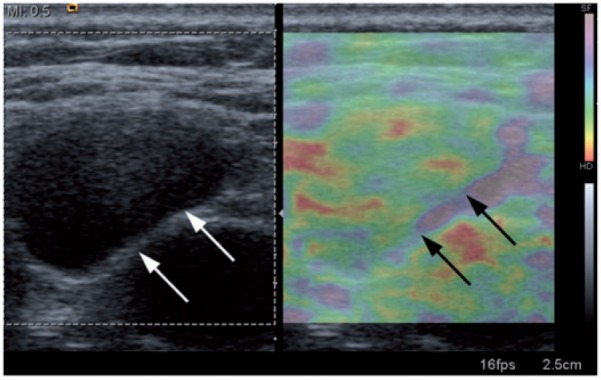
Longitudinal greyscale sonogram (left image) and strain elastogram (right image) in a patient with reactive lymphadenitis show a reactive lymph node in the internal jugular chain (arrows). In the elastogram, the lymph node is predominantly colour coded as green and blue, which indicates the lymph node is soft.
Figure 13.
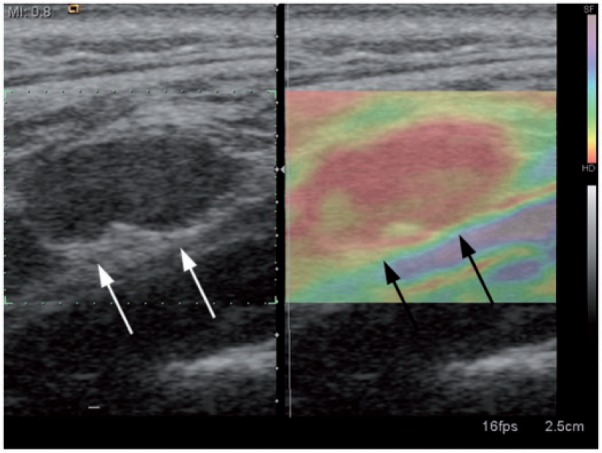
Longitudinal greyscale sonogram (left image) and strain elastogram (right image) in a patient with carcinoma of the pharynx shows a metastatic lymph node in the internal jugular chain (arrows). In the elastogram, the lymph node is predominantly colour coded as red, which indicates the lymph node is hard.
In view of the different elastography scoring systems and methodologies in the assessment of cervical lymphadenopathy, differing results are reported in the literature. In view of this inconsistency and non-repeatability, the value of qualitative real-time ultrasound elastography in routine clinical practice remains unclear and limited.
Quantitative assessment
On conventional strain elastography, benign lymph nodes tend to have a lower strain index, whereas malignant nodes usually have a higher strain index. Different cut-off values of strain index were suggested to distinguish benign and malignant nodes (1.5 and 1.78), and the sensitivity, specificity and accuracy of this technique in the differential diagnosis were 92.8–98.1%, 53.4–85% and 75–92%, respectively[36,40,75].
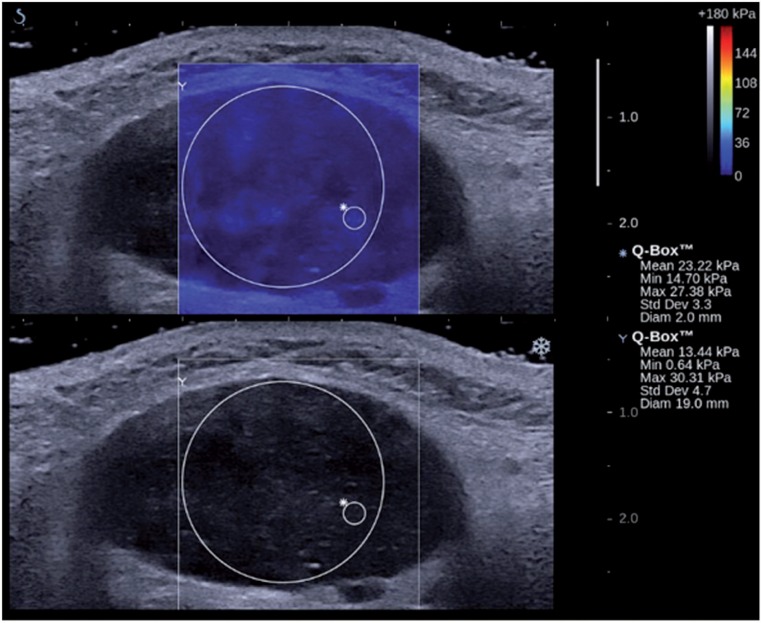
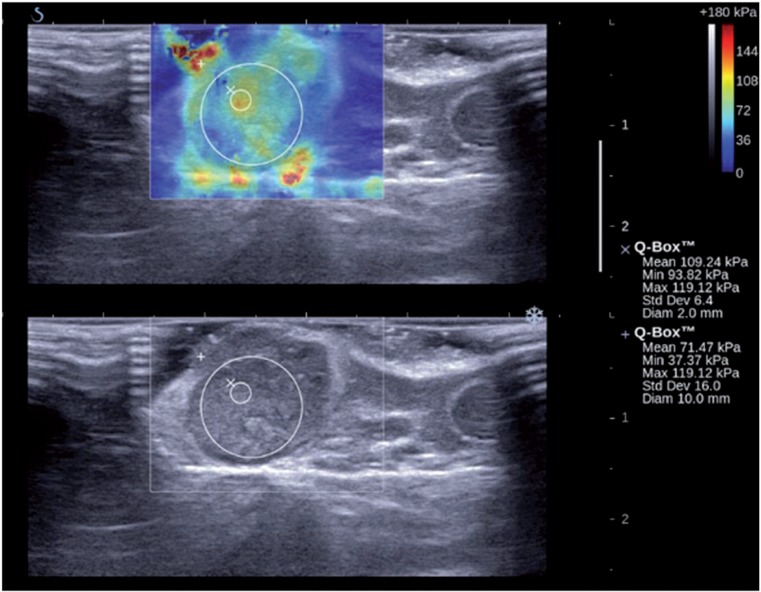
SWE has been used in the assessment of the neck. It has been reported that SWE has variable reliability in assessing the stiffness of neck lesions[76]. A recent study using SWE to evaluate the stiffness of malignant and benign cervical nodes found that malignant nodes were stiffer than benign nodes (Figs. 14 and 15)[13]. Using SWE to distinguish malignant and benign cervical nodes, the optimal cut-off of tissue stiffness was 30.2 kPa with sensitivity, specificity and accuracy of 41.9%, 100% and 61.8%, respectively[13].
Figure 14.
Transverse shear wave elastogram in a patient with reactive lymphadenitis shows a reactive lymph node in the submandibular region. The lymph node has relatively lower stiffness values compared with the metastatic lymph node in Fig. 15. The large circle measures the overall stiffness of the lymph node, and the small circle measures a focal area within the node.
Figure 15.
Transverse shear wave elastogram in a patient with carcinoma of the larynx shows a metastatic lymph node in the internal jugular chain. The lymph node has relatively higher stiffness values compared with the reactive lymph node in Fig. 14. The large circle measures the overall stiffness of the lymph node, and the small circle measures the relatively harder area within the node.
Strain index and SWE allow quantification of lymph node stiffness, which provides additional information for the assessment of cervical lymphadenopathy. However, the results remain inconsistent limiting its use in routine clinical practice.
Contrast enhancement
Contrast-enhanced ultrasonography allows more accurate evaluation of nodal vascularity and provides information on lymph node parenchymal perfusion[77]. However, the value of this technique in differentiating benign and malignant lymph nodes is controversial. Previous studies reported that contrast-enhanced ultrasonography improves the accuracy in differentiating benign and malignant nodes because it increases the sensitivity in detecting intranodal vascularity[77–79]. However, others have reported that contrast-enhanced ultrasonography does not improve the accuracy of greyscale and Doppler ultrasonography for identifying malignant n nodes[80].
Although contrast enhancement may provide additional information in the evaluation of cervical lymph nodes, the value of this technique in routine clinical practice is limited, in particular because it is expensive, time consuming and does not obviate the need for FNAC.
Ultrasound-guided FNAC
Ultrasound-guided FNAC is an accurate method for the evaluation of neck nodes with a sensitivity of 89–98%, specificity of 95–98% and overall accuracy of 95–97%[5,81]. It has been reported that ultrasound-guided FNAC correctly stages the neck nodes in 93% of patients with head and neck malignancy[81], and influences the indications for therapeutic and elective treatment[82].
Thyroglobulin measurement in the washout of the fine-needle aspirates in neck nodes is another accurate method for identifying nodal metastases from papillary carcinoma of the thyroid. It has been suggested that a cut-off value of 10 ng/ml in thyroglobulin measurement has a sensitivity and specificity of 100% for detecting nodal metastases[83].
In our experience, ultrasound-guided FNAC is performed to confirm the diagnosis whenever the ultrasonographic findings are equivocal. The technique not only aids in tumour staging and treatment planning[81,82,84,85], but is also useful in post-operative neck node surveillance[86].
Limitations and pitfalls of ultrasonography in the evaluation of malignant neck nodes
Ultrasonography cannot assess the retropharyngeal lymph nodes, which lie behind the air-filled pharynx. Retropharyngeal lymph nodes are common sites of metastases in some head and neck cancers such as nasopharyngeal carcinoma, and these lymph nodes are evaluated with computed tomography or magnetic resonance imaging. Similar to other imaging modalities, ultrasonography cannot detect micrometastasis in lymph nodes and may lead to false-negative findings[87]. On greyscale ultrasonography, both coagulation necrosis and the hilus appear echogenic within the lymph node. The two can be distinguished by noting that the hilus is a linear echogenic structure continuous with the surrounding fat, whereas coagulation necrosis appears as an echogenic focus and is not continuous with the surrounding fat.
Conclusion
Ultrasonography is a useful and reliable imaging method in the assessment of malignant cervical nodes in patients with head and neck cancer. It helps to identify abnormal nodes and evaluates treatment response.
Conflict of interest
The authors have no conflicts of interest to declare.
Footnotes
This paper is available online at http://www.cancerimaging.org. In the event of a change in the URL address, please use the DOI provided to locate the paper.
References
- 1.Vassallo P, Wernecke K, Roos N, Peters PE. Differentiation of benign from malignant superficial lymphadenopathy: the role of high-resolution US. Radiology. 1992;183:215. doi: 10.1148/radiology.183.1.1549675. PMid:1549675. [DOI] [PubMed] [Google Scholar]
- 2.Som PM. Detection of metastasis in cervical lymph nodes: CT and MR criteria and differential diagnosis. Am J Roentgenol. 1992;158:961. doi: 10.2214/ajr.158.5.1566697. [DOI] [PubMed] [Google Scholar]
- 3.Baatenburg de Jong RJ, Rongen RJ, Lameris JS, Harthoorn M, Verwoerd CD, Knegt P. Metastatic neck disease. Palpation vs ultrasound examination. Arch Otolaryngol Head Neck Surg. 1989;115:689. doi: 10.1001/archotol.1989.01860300043013. PMid:2655666. [DOI] [PubMed] [Google Scholar]
- 4.Bruneton JN, Normand F. Cervical lymph nodes. In: Bruneton JN, editor. Ultrasonography of the neck. Berlin: Springer-Verlag; 1987. p. 81. [Google Scholar]
- 5.Baatenburg de Jong RJ, Rongen RJ, Verwoerd CD, van Overhagen H, Lameris JS, Knegt P. Ultrasound-guided fine-needle aspiration biopsy of neck nodes. Arch Otolaryngol Head Neck Surg. 1991;117:402. doi: 10.1001/archotol.1991.01870160056008. PMid:2007009. [DOI] [PubMed] [Google Scholar]
- 6.Ahuja A, Ying M, King W, Metreweli C. A practical approach to ultrasound of cervical lymph nodes. J Laryngol Otol. 1997;111:245. doi: 10.1017/s0022215100137004. PMid:9156061. [DOI] [PubMed] [Google Scholar]
- 7.Ying M, Ahuja A, Brook F, Brown B, Metreweli C. Sonographic appearance and distribution of normal cervical lymph nodes in a Chinese population. J Ultrasound Med. 1996;15:431. doi: 10.7863/jum.1996.15.6.431. PMid:8738986. [DOI] [PubMed] [Google Scholar]
- 8.Ahuja A, Ying M, Yuen HY, Metreweli C. Power Doppler sonography of cervical lymphadenopathy. Clin Radiol. 2001;56:965. doi: 10.1053/crad.2001.0717. PMid:11795924. [DOI] [PubMed] [Google Scholar]
- 9.Ahuja AT, Ying M, Ho SS, Metreweli C. Distribution of intranodal vessels in differentiating benign from metastatic neck nodes. Clin Radiol. 2001;56:197. doi: 10.1053/crad.2000.0574. PMid:11247696. [DOI] [PubMed] [Google Scholar]
- 10.Ariji Y, Kimura Y, Hayashi N, et al. Power Doppler sonography of cervical lymph nodes in patients with head and neck cancer. Am J Neuroradiol. 1998;19:303. PMid:9504483. [PMC free article] [PubMed] [Google Scholar]
- 11.Ying M, Ahuja A, Brook F, Metreweli C. Power Doppler sonography of normal cervical lymph nodes. J Ultrasound Med. 2000;19:511. doi: 10.7863/jum.2000.19.8.511. PMid:10944036. [DOI] [PubMed] [Google Scholar]
- 12.Wu CH, Chang YL, Hsu WC, Ko JY, Sheen TS, Hsieh FJ. Usefulness of Doppler spectral analysis and power Doppler sonography in the differentiation of cervical lymphadenopathies. Am J Roentgenol. 1998;171:503. doi: 10.2214/ajr.171.2.9694484. [DOI] [PubMed] [Google Scholar]
- 13.Bhatia KS, Cho CC, Tong CS, Yuen EH, Ahuja AT. Shear wave elasticity imaging of cervical lymph nodes. Ultrasound Med Biol. 2012;38:195. doi: 10.1016/j.ultrasmedbio.2011.10.024. PMid:22178167. [DOI] [PubMed] [Google Scholar]
- 14.Bhatia KS, Cho CC, Yuen YH, Rasalkar DD, King AD, Ahuja AT. Real-time qualitative ultrasound elastography of cervical lymph nodes in routine clinical practice: interobserver agreement and correlation with malignancy. Ultrasound Med Biol. 2010;36:1990. doi: 10.1016/j.ultrasmedbio.2010.08.016. PMid:20950927. [DOI] [PubMed] [Google Scholar]
- 15.Som PM. Lymph nodes of the neck. Radiology. 1987;165:593. doi: 10.1148/radiology.165.3.3317494. PMid:3317494. [DOI] [PubMed] [Google Scholar]
- 16.Swartz JD, Yussen PS, Popky GL. Imaging of the neck: nodal disease. Crit Rev Diagn Imaging. 1991;31:413. PMid:2036177. [PubMed] [Google Scholar]
- 17.Lindberg R. Distribution of cervical lymph node metastases from squamous cell carcinoma of the upper respiratory and digestive tracts. Cancer. 1972;29:1446. doi: 10.1002/1097-0142(197206)29:6<1446::aid-cncr2820290604>3.0.co;2-c. PMid:5031238. [DOI] [PubMed] [Google Scholar]
- 18.Komisar A. Treatment of the node negative neck. In: Vogl SE, editor. Head and neck cancer. New York: Churchill Livingstone; 1988. p. p. 19. [Google Scholar]
- 19.van Overhagen H, Lameris JS, Berger MY, et al. Supraclavicular lymph node metastases in carcinoma of the esophagus and gastroesophageal junction: assessment with CT, US, and US-guided fine- needle aspiration biopsy. Radiology. 1991;179:155. doi: 10.1148/radiology.179.1.2006268. PMid:2006268. [DOI] [PubMed] [Google Scholar]
- 20.van Overhagen H, Lameris JS, Zonderland HM, Tilanus HW, van Pel R, Schutte HE. Ultrasound and ultrasound-guided fine needle aspiration biopsy of supraclavicular lymph nodes in patients with esophageal carcinoma. Cancer. 1991;67:585. doi: 10.1002/1097-0142(19910201)67:3<585::aid-cncr2820670310>3.0.co;2-q. PMid:1985752. [DOI] [PubMed] [Google Scholar]
- 21.Van Overhagen H, Lameris JS, Berger MY, et al. Improved assessment of supraclavicular and abdominal metastases in oesophageal and gastro-oesophageal junction carcinoma with the combination of ultrasound and computed tomography. Br J Radiol. 1993;66:203. doi: 10.1259/0007-1285-66-783-203. PMid:8472112. [DOI] [PubMed] [Google Scholar]
- 22.Ahuja A, Ying M. Grey-scale sonography in assessment of cervical lymphadenopathy: review of sonographic appearances and features that may help a beginner. Br J Oral Maxillofac Surg. 2000;38:451. doi: 10.1054/bjom.2000.0446. PMid:11010773. [DOI] [PubMed] [Google Scholar]
- 23.Ishii JI, Amagasa T, Tachibana T, Shinozuka K, Shioda S. US and CT evaluation of cervical lymph node metastasis from oral cancer. J Craniomaxillofac Surg. 1991;19:123. doi: 10.1016/s1010-5182(05)80575-x. PMid:2071694. [DOI] [PubMed] [Google Scholar]
- 24.Ying M, Ahuja AT, Evans R, King W, Metreweli C. Cervical lymphadenopathy: sonographic differentiation between tuberculous nodes and nodal metastases from non-head and neck carcinomas. J Clin Ultrasound. 1998;26:383. doi: 10.1002/(sici)1097-0096(199810)26:8<383::aid-jcu2>3.0.co;2-e. PMid:9783244. [DOI] [PubMed] [Google Scholar]
- 25.Sugama Y, Kitamura S. Ultrasonographic evaluation of neck and supraclavicular lymph nodes metastasized from lung cancer. Intern Med. 1992;31:160. doi: 10.2169/internalmedicine.31.160. PMid:1600260. [DOI] [PubMed] [Google Scholar]
- 26.Yao ZH, Wu AR. Supraclavicular lymph node metastasis from carcinoma of the uterine cervix after radiotherapy–analysis of 219 patients. Chung Hua Chung Liu Tsa Chih. 1988;10:230. PMid:3219986. [PubMed] [Google Scholar]
- 27.Kiricuta IC, Willner J, Kolbl O, Bohndorf W. The prognostic significance of the supraclavicular lymph node metastases in breast cancer patients. Int J Radiat Oncol Biol Phys. 1994;28:387. doi: 10.1016/0360-3016(94)90062-0. PMid:8276654. [DOI] [PubMed] [Google Scholar]
- 28.Cervin JR, Silverman JF, Loggie BW, Geisinger KR. Virchow's node revisited. Analysis with clinicopathologic correlation of 152 fine-needle aspiration biopsies of supraclavicular lymph nodes. Arch Pathol Lab Med. 1995;119:727. PMid:7646330. [PubMed] [Google Scholar]
- 29.Ahuja A, Ying M, Evans R, King W, Metreweli C. The application of ultrasound criteria for malignancy in differentiating tuberculous cervical adenitis from metastatic nasopharyngeal carcinoma. Clin Radiol. 1995;50:391. doi: 10.1016/s0009-9260(05)83136-8. PMid:7789023. [DOI] [PubMed] [Google Scholar]
- 30.Ahuja AT, Chow L, Chick W, King W, Metreweli C. Metastatic cervical nodes in papillary carcinoma of the thyroid: ultrasound and histological correlation. Clin Radiol. 1995;50:229. doi: 10.1016/s0009-9260(05)83475-0. PMid:7729119. [DOI] [PubMed] [Google Scholar]
- 31.Attie JN, Setzin M, Klein I. Thyroid carcinoma presenting as an enlarged cervical lymph node. Am J Surg. 1993;166:428. doi: 10.1016/s0002-9610(05)80348-4. PMid:8214308. [DOI] [PubMed] [Google Scholar]
- 32.De Jong SA, Demeter JG, Jarosz H, Lawrence AM, Paloyan E. Primary papillary thyroid carcinoma presenting as cervical lymphadenopathy: the operative approach to the “lateral aberrant thyroid”. Am Surg. 1993;59:172. PMid:8476156. [PubMed] [Google Scholar]
- 33.Ahuja A, Ying M, Yang WT, Evans R, King W, Metreweli C. The use of sonography in differentiating cervical lymphomatous lymph nodes from cervical metastatic lymph nodes. Clin Radiol. 1996;51:186. doi: 10.1016/s0009-9260(96)80321-7. PMid:8605749. [DOI] [PubMed] [Google Scholar]
- 34.Hohlweg-Majert B, Metzger MC, Voss PJ, Holzle F, Wolff KD, Schulze D. Preoperative cervical lymph node size evaluation in patients with malignant head/neck tumors: comparison between ultrasound and computer tomography. J Cancer Res Clin Oncol. 2009;135:753. doi: 10.1007/s00432-008-0487-y. PMid:18830710. [DOI] [PubMed] [Google Scholar]
- 35.Furukawa MK, Furukawa M. Diagnosis of lymph node metastases of head and neck cancer and evaluation of effects of chemoradiotherapy using ultrasonography. Int J Clin Oncol. 2010;15:23. doi: 10.1007/s10147-009-0017-1. PMid:20111883. [DOI] [PubMed] [Google Scholar]
- 36.Lyshchik A, Higashi T, Asato R, et al. Cervical lymph node metastases: diagnosis at sonoelastography–initial experience. Radiology. 2007;243:258. doi: 10.1148/radiol.2431052032. PMid:17293571. [DOI] [PubMed] [Google Scholar]
- 37.Hajek PC, Salomonowitz E, Turk R, Tscholakoff D, Kumpan W, Czembirek H. Lymph nodes of the neck: evaluation with US. Radiology. 1986;158:739. doi: 10.1148/radiology.158.3.3511503. PMid:3511503. [DOI] [PubMed] [Google Scholar]
- 38.Shozushima M, Suzuki M, Nakasima T, Yanagisawa Y, Sakamaki K, Takeda Y. Ultrasound diagnosis of lymph node metastasis in head and neck cancer. Dentomaxillofac Radiol. 1990;19:165. doi: 10.1259/dmfr.19.4.2097226. PMid:2097226. [DOI] [PubMed] [Google Scholar]
- 39.Solbiati L, Rizzatto G, Bellotti E, Montali G, Cioffi V, Croce F. High-resolution sonography of cervical lymph nodes in head and neck cancer: criteria for differentiation of reactive versus malignant nodes. Radiology. 1988;169:113. [Google Scholar]
- 40.Teng DK, Wang H, Lin YQ, Sui GQ, Guo F, Sun LN. Value of ultrasound elastography in assessment of enlarged cervical lymph nodes. Asian Pac J Cancer Prev. 2012;13:2081. doi: 10.7314/apjcp.2012.13.5.2081. PMid:22901174. [DOI] [PubMed] [Google Scholar]
- 41.van den Brekel MW, Castelijns JA, Stel HV, Golding RP, Meyer CJ, Snow GB. Modern imaging techniques and ultrasound-guided aspiration cytology for the assessment of neck node metastases: a prospective comparative study. Eur Arch Otorhinolaryngol. 1993;250:11. doi: 10.1007/BF00176941. PMid:8466744. [DOI] [PubMed] [Google Scholar]
- 42.Ying M, Ahuja A, Metreweli C. Diagnostic accuracy of sonographic criteria for evaluation of cervical lymphadenopathy. J Ultrasound Med. 1998;17:437. doi: 10.7863/jum.1998.17.7.437. PMid:9669302. [DOI] [PubMed] [Google Scholar]
- 43.Ho SS, Ahuja AT, Yeo W, Chan TC, Kew J, Metreweli C. Longitudinal colour Doppler study of superficial lymph nodes in non-Hodgkin's lymphoma patients on chemotherapy. Clin Radiol. 2000;55:110. doi: 10.1053/crad.1999.0229. PMid:10657155. [DOI] [PubMed] [Google Scholar]
- 44.Tohnosu N, Onoda S, Isono K. Ultrasonographic evaluation of cervical lymph node metastases in esophageal cancer with special reference to the relationship between the short to long axis ratio (S/L) and the cancer content. J Clin Ultrasound. 1989;17:101. doi: 10.1002/jcu.1870170206. PMid:2492556. [DOI] [PubMed] [Google Scholar]
- 45.Vassallo P, Edel G, Roos N, Naguib A, Peters PE. In-vitro high-resolution ultrasonography of benign and malignant lymph nodes. A sonographic-pathologic correlation. Invest Radiol. 1993;28:698. doi: 10.1097/00004424-199308000-00009. PMid:8376001. [DOI] [PubMed] [Google Scholar]
- 46.Gupta A, Rahman K, Shahid M, et al. Sonographic assessment of cervical lymphadenopathy: role of high-resolution and color Doppler imaging. Head Neck. 2011;33:297. doi: 10.1002/hed.21448. PMid:20652889. [DOI] [PubMed] [Google Scholar]
- 47.Imani Moghaddam M, Davachi B, Mostaan LV, et al. Evaluation of the sonographic features of metastatic cervical lymph nodes in patients with head and neck malignancy. J Craniofac Surg. 2011;22:2179. doi: 10.1097/SCS.0b013e3182324166. PMid:22075819. [DOI] [PubMed] [Google Scholar]
- 48.Evans RM, Ahuja A, Metreweli C. The linear echogenic hilus in cervical lymphadenopathy–a sign of benignity or malignancy? Clin Radiol. 1993;47:262. doi: 10.1016/s0009-9260(05)81135-3. PMid:8495573. [DOI] [PubMed] [Google Scholar]
- 49.Rubaltelli L, Proto E, Salmaso R, Bortoletto P, Candiani F, Cagol P. Sonography of abnormal lymph nodes in vitro: correlation of sonographic and histologic findings. Am J Roentgenol. 1990;155:1241. doi: 10.2214/ajr.155.6.2122673. [DOI] [PubMed] [Google Scholar]
- 50.Sakai F, Kiyono K, Sone S, et al. Ultrasonic evaluation of cervical metastatic lymphadenopathy. J Ultrasound Med. 1988;7:305. doi: 10.7863/jum.1988.7.6.305. PMid:3294431. [DOI] [PubMed] [Google Scholar]
- 51.Alam F, Naito K, Horiguchi J, Fukuda H, Tachikake T, Ito K. Accuracy of sonographic elastography in the differential diagnosis of enlarged cervical lymph nodes: comparison with conventional B-mode sonography. AJR Am J Roentgenol. 2008;191:604. doi: 10.2214/AJR.07.3401. PMid:18647939. [DOI] [PubMed] [Google Scholar]
- 52.Ying M, Ahuja A, Brook F, Metreweli C. Vascularity and grey-scale sonographic features of normal cervical lymph nodes: variations with nodal size. Clin Radiol. 2001;56:416. doi: 10.1053/crad.2000.0680. PMid:11384142. [DOI] [PubMed] [Google Scholar]
- 53.Ahuja A, Ying M. An overview of neck node sonography. Invest Radiol. 2002;37:333. doi: 10.1097/00004424-200206000-00005. PMid:12021590. [DOI] [PubMed] [Google Scholar]
- 54.Som PM, Brandwein M, Lidov M, Lawson W, Biller HF. The varied presentations of papillary thyroid carcinoma cervical nodal disease: CT and MR findings. Am J Neuroradiol. 1994;15:1123. PMid:8073982. [PMC free article] [PubMed] [Google Scholar]
- 55.Bruneton JN, Normand F, Balu-Maestro C, et al. Lymphomatous superficial lymph nodes: US detection. Radiology. 1987;165:233. doi: 10.1148/radiology.165.1.3306785. PMid:3306785. [DOI] [PubMed] [Google Scholar]
- 56.Ishii J, Fujii E, Suzuki H, Shinozuka K, Kawase N, Amagasa T. Ultrasonic diagnosis of oral and neck malignant lymphoma. Bull Tokyo Med Dent Univ. 1992;39:63. PMid:1458552. [PubMed] [Google Scholar]
- 57.Ahuja AT, Ying M, Yuen HY, Metreweli C. ‘Pseudocystic’ appearance of non-Hodgkin's lymphomatous nodes: an infrequent finding with high-resolution transducers. Clin Radiol. 2001;56:111. doi: 10.1053/crad.2000.0642. PMid:11222067. [DOI] [PubMed] [Google Scholar]
- 58.Gooding GA. Malignant carotid invasion: sonographic diagnosis. ORL J Otorhinolaryngol Relat Spec. 1993;55:263. doi: 10.1159/000276437. PMid:8378064. [DOI] [PubMed] [Google Scholar]
- 59.DePena CA, Van Tassel P, Lee YY. Lymphoma of the head and neck. Radiol Clin North Am. 1990;28:723. PMid:2190267. [PubMed] [Google Scholar]
- 60.Mancuso AA, Harnsberger HR, Muraki AS, Stevens MH. Computed tomography of cervical and retropharyngeal lymph nodes: normal anatomy, variants of normal, and applications in staging head and neck cancer. Part II: pathology. Radiology. 1983;148:715. doi: 10.1148/radiology.148.3.6878692. PMid:6878692. [DOI] [PubMed] [Google Scholar]
- 61.Olsen WL, Jeffrey RB, Jr, Sooy CD, Lynch MA, Dillon WP. Lesions of the head and neck in patients with AIDS: CT and MR findings. Am J Roentgenol. 1988;151:785. doi: 10.2214/ajr.151.4.785. [DOI] [PubMed] [Google Scholar]
- 62.Miseikyte-Kaubriene E, Trakymas M, Ulys A. Cystic lymph node metastasis in papillary thyroid carcinoma. Medicina (Kaunas) 2008;44:455. [PubMed] [Google Scholar]
- 63.Landry CS, Grubbs EG, Busaidy NL, Staerkel GA, Perrier ND, Edeiken-Monroe BS. Cystic lymph nodes in the lateral neck are an indicator of metastatic papillary thyroid cancer. Endocr Pract. 2010;16:1. doi: 10.4158/EP10134.OR. [DOI] [PubMed] [Google Scholar]
- 64.Ahuja A, Ying M, Leung SF, Metreweli C. The sonographic appearance and significance of cervical metastatic nodes following radiotherapy for nasopharyngeal carcinoma. Clin Radiol. 1996;51:698. doi: 10.1016/s0009-9260(96)80241-8. PMid:8893638. [DOI] [PubMed] [Google Scholar]
- 65.Ying M, Ahuja A, Brook F. Repeatability of power Doppler sonography of cervical lymph nodes. Ultrasound Med Biol. 2002;28:737. doi: 10.1016/s0301-5629(02)00523-9. PMid:12113786. [DOI] [PubMed] [Google Scholar]
- 66.Na DG, Lim HK, Byun HS, Kim HD, Ko YH, Baek JH. Differential diagnosis of cervical lymphadenopathy: usefulness of color Doppler sonography. Am J Roentgenol. 1997;168:1311. doi: 10.2214/ajr.168.5.9129432. [DOI] [PubMed] [Google Scholar]
- 67.Steinkamp HJ, Maurer J, Cornehl M, Knobber D, Hettwer H, Felix R. Recurrent cervical lymphadenopathy: differential diagnosis with color- duplex sonography. Eur Arch Otorhinolaryngol. 1994;251:404. doi: 10.1007/BF00181966. PMid:7857628. [DOI] [PubMed] [Google Scholar]
- 68.Ying M, Ahuja A, Brook F. Accuracy of sonographic vascular features in differentiating different causes of cervical lymphadenopathy. Ultrasound Med Biol. 2004;30:441. doi: 10.1016/j.ultrasmedbio.2003.12.009. PMid:15121245. [DOI] [PubMed] [Google Scholar]
- 69.Steinkamp HJ, Mueffelmann M, Bock JC, Thiel T, Kenzel P, Felix R. Differential diagnosis of lymph node lesions: a semiquantitative approach with colour Doppler ultrasound. Br J Radiol. 1998;71:828. doi: 10.1259/bjr.71.848.9828794. PMid:9828794. [DOI] [PubMed] [Google Scholar]
- 70.Ahuja A, Ying M. Sonographic evaluation of cervical lymphadenopathy: is power Doppler sonography routinely indicated? Ultrasound Med Biol. 2003;29:353. doi: 10.1016/s0301-5629(02)00759-7. PMid:12706185. [DOI] [PubMed] [Google Scholar]
- 71.Maurer J, Willam C, Schroeder R, et al. Evaluation of metastases and reactive lymph nodes in Doppler sonography using an ultrasound contrast enhancer. Invest Radiol. 1997;32:441. doi: 10.1097/00004424-199708000-00002. PMid:9258731. [DOI] [PubMed] [Google Scholar]
- 72.Dragoni F, Cartoni C, Pescarmona E, et al. The role of high resolution pulsed and color Doppler ultrasound in the differential diagnosis of benign and malignant lymphadenopathy: results of multivariate analysis. Cancer. 1999;85:2485. doi: 10.1002/(sici)1097-0142(19990601)85:11<2485::aid-cncr26>3.0.co;2-y. PMid:10357422. [DOI] [PubMed] [Google Scholar]
- 73.Chang DB, Yuan A, Yu CJ, Luh KT, Kuo SH, Yang PC. Differentiation of benign and malignant cervical lymph nodes with color Doppler sonography. Am J Roentgenol. 1994;162:965. doi: 10.2214/ajr.162.4.8141027. [DOI] [PubMed] [Google Scholar]
- 74.Adibelli ZH, Unal G, Gul E, Uslu F, Kocak U, Abali Y. Differentiation of benign and malignant cervical lymph nodes: value of B-mode and color Doppler sonography. Eur J Radiol. 1998;28:230. doi: 10.1016/s0720-048x(97)00174-5. PMid:9881258. [DOI] [PubMed] [Google Scholar]
- 75.Tan R, Xiao Y, He Q. Ultrasound elastography: its potential role in assessment of cervical lymphadenopathy. Acad Radiol. 2010;17:849. doi: 10.1016/j.acra.2010.03.014. PMid:20540909. [DOI] [PubMed] [Google Scholar]
- 76.Bhatia K, Tong CS, Cho CC, Yuen EH, Lee J, Ahuja AT. Reliability of shear wave ultrasound elastography for neck lesions identified in routine clinical practice. Ultraschall Med. 2012;33:463. doi: 10.1055/s-0032-1325330. PMid:23070932. [DOI] [PubMed] [Google Scholar]
- 77.Rubaltelli L, Khadivi Y, Tregnaghi A, et al. Evaluation of lymph node perfusion using continuous mode harmonic ultrasonography with a second-generation contrast agent. J Ultrasound Med. 2004;23:829. doi: 10.7863/jum.2004.23.6.829. PMid:15244307. [DOI] [PubMed] [Google Scholar]
- 78.Moritz JD, Ludwig A, Oestmann JW. Contrast-enhanced color Doppler sonography for evaluation of enlarged cervical lymph nodes in head and neck tumors. Am J Roentgenol. 2000;174:1279. doi: 10.2214/ajr.174.5.1741279. [DOI] [PubMed] [Google Scholar]
- 79.Rickert D, Jecker P, Metzler V, Lehmann T, Ernst E, Westhofen M. Color-coded duplex sonography of the cervical lymph nodes: improved differential diagnostic assessment after administration of the signal enhancer SH U 508A (Levovist) Eur Arch Otorhinolaryngol. 2000;257:453. doi: 10.1007/s004059900210. PMid:11073198. [DOI] [PubMed] [Google Scholar]
- 80.Zenk J, Bozzato A, Hornung J, et al. Neck lymph nodes: prediction by computer-assisted contrast medium analysis? Ultrasound Med Biol. 2007;33:246. doi: 10.1016/j.ultrasmedbio.2006.08.005. PMid:17306695. [DOI] [PubMed] [Google Scholar]
- 81.Knappe M, Louw M, Gregor RT. Ultrasonography-guided fine-needle aspiration for the assessment of cervical metastases. Arch Otolaryngol Head Neck Surg. 2000;126:1091. doi: 10.1001/archotol.126.9.1091. PMid:10979122. [DOI] [PubMed] [Google Scholar]
- 82.Robinson IA, Cozens NJ. Does a joint ultrasound guided cytology clinic optimize the cytological evaluation of head and neck masses? Clin Radiol. 1999;54:312. doi: 10.1016/s0009-9260(99)90561-5. PMid:10362238. [DOI] [PubMed] [Google Scholar]
- 83.Zanella AB, Meyer EL, Balzan L, et al. Thyroglobulin measurements in washout of fine needle aspirates in cervical lymph nodes for detection of papillary thyroid cancer metastases. Arq Bras Endocrinol Metabol. 2010;54:550. doi: 10.1590/s0004-27302010000600007. PMid:20857060. [DOI] [PubMed] [Google Scholar]
- 84.Hodder SC, Evans RM, Patton DW, Silvester KC. Ultrasound and fine needle aspiration cytology in the staging of neck lymph nodes in oral squamous cell carcinoma. Br J Oral Maxillofac Surg. 2000;38:430. doi: 10.1054/bjom.2000.0332. PMid:11010769. [DOI] [PubMed] [Google Scholar]
- 85.Lo CP, Chen CY, Chin SC, et al. Detection of suspicious malignant cervical lymph nodes of unknown origin: diagnostic accuracy of ultrasound-guided fine-needle aspiration biopsy with nodal size and central necrosis correlate. Can Assoc Radiol J. 2007;58:286. PMid:18286904. [PubMed] [Google Scholar]
- 86.van den Brekel MW, Reitsma LC, Quak JJ, et al. Sonographically guided aspiration cytology of neck nodes for selection of treatment and follow-up in patients with N0 head and neck cancer. Am J Neuroradiol. 1999;20:1727. PMid:10543649. [PMC free article] [PubMed] [Google Scholar]
- 87.Lee N, Inoue K, Yamamoto R, Kinoshita H. Patterns of internal echoes in lymph nodes in the diagnosis of lung cancer metastasis. World J Surg. 1992;16:986. doi: 10.1007/BF02067013. PMid:1334300. [DOI] [PubMed] [Google Scholar]