Abstract
Purpose
As part of the RICE study, we previously developed validated case definitions to identify interstitial cystitis/bladder pain syndrome (IC/BPS) in women and chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) in men. Using population-based screening methods, we applied these case definitions to determine the prevalence of these conditions in men.
Materials and Methods
A total of 6,072 households were contacted by phone to screen for men who had symptoms of IC/BPS or CP/CPPS. An initial 296 men screened positive, of which 149 met the inclusionary criteria and completed the telephone interview. For IC/BPS, two case definitions were applied (one with high sensitivity and one with high specificity), while for CP/CPPS, a single case definition (with both high sensitivity and specificity) was used. These case definitions were used to classify subjects into groups based on diagnosis.
Results
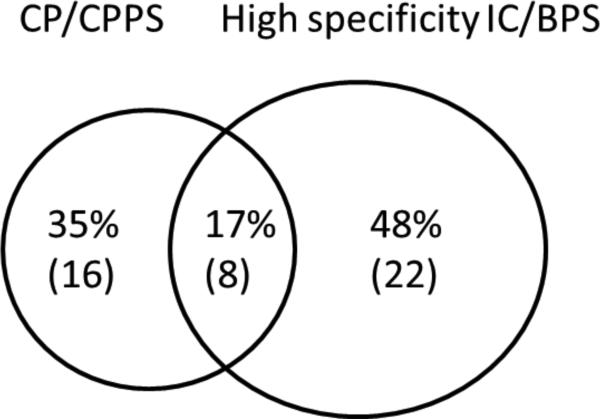
The IC/BPS weighted prevalence estimate for the high sensitivity and specificity definition was 4.2% (3.1-5.3%), and 1.9% (1.1-2.7%), respectively. The CP/CPPS weighted prevalence estimate was 1.8% (0.9-2.7%). These values equate to 1,986,972 (95% CI 966,042- 2,996,924) men with CP/CPPS and to 2,107,727 (95% CI 1,240,485 – 2,974,969) men with the high specificity definition of IC/BPS in the U.S.. The overlap between men who met either the high specificity IC/BPS case definition or the CP/CPPS case definition was 17%.
Conclusions
Symptoms of IC/BPS and CP/CPPS are widespread among men in the US.. The prevalence of IC/BPS symptoms in men approaches that in women, suggesting that this condition may be underdiagnosed and undertreated in the male population.
Keywords: interstitial cystitis, chronic prostatitis, epidemiology, men
Introduction
The prevalence of interstitial cystitis/bladder pain syndrome (IC/BPS) and chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) are poorly defined in men. These estimates are difficult to obtain because there are no good biomarkers or tests to diagnose these disorders. Instead, diagnosis of these chronic conditions is based on the presence of certain symptoms (e.g., pain, urinary frequency) and exclusion of other conditions which are recognized causes of these symptoms (e.g., urinary tract infection, cancer).
Previous studies have estimated the prevalence of these disorders in men using various methods. For instance, several studies administered surveys about prior diagnoses of IC/BPS or ‘prostatitis’,1-6 or about current symptoms of IC/BPS7, 8 or CP/CPPS.2-6 Others have abstracted data from medical records.8-10 All of these attempts, however, are limited by the lack of validated case definitions for these disorders, and/or their use of study samples from limited geographic regions.7 As a result, there are no comprehensive, national, weighted prevalence estimates of IC/BPS and CP/CPPS in men in the current literature.
In order to address this knowledge gap, we performed national population-based screening to identify men with symptoms or a diagnosis of IC/BPS or CP/CPPS. We then applied previously validated case definitions of IC/BPS and CP/CPPS to these conditions in men,11, 12 in order to obtain more comprehensive and accurate prevalence estimates.
Materials and Methods
IC/BPS case definitions
Our group previously developed and validated high sensitivity and high specificity case definitions for IC/BPS in women. Based on a comprehensive literature search and a structured expert panel, we developed a questionnaire to assess the presence of IC/BPS symptoms and administered these items to 599 adult women. Results from this questionnaire were used to develop two IC/BPS definitions, one with 81% sensitivity (RICE high sensitivity case definition) and another with 83% specificity (RICE high specificity case definition). Details of this definition are posted in an Appendix that is available online at the RAND website (http://www.rand.org/pubs/working_papers/WR959.html). For the present study, we modified these case definitions for use in men in two ways. First, we removed female-specific exclusion criteria (cervical cancer, uterine cancer, pregnancy), and replaced them with a male exclusion criterion (prostate cancer), while preserving all general exclusion criteria (bladder cancer, colon cancer, prior pelvic radiation, spinal cord injury, etc.). Second, we modified the RICE high sensitivity case definition by removing the criteria related to hormone injection therapy for endometriosis.
CP/CPPS case definition
We used a case definition for CP/CPPS that was initially proposed by Nickel and colleagues,2 which is derived from the pain subscale of the National Institute of Health Chronic Prostatitis Symptom Index (NIH-CPSI).13 This definition requires the presence of perineal or ejaculatory pain, plus a score of ≥4 on the NIH-CPSI pain subscale. The sensitivity and specificity of this case definition were 70% and 91% when compared to patients with benign prostatic hyperplasia, with a specificity of 99% when compared to controls.12
Population screening
Population-based screening was performed by the Opinion Research Corporation (ORC) between February and March of 2010. The ORC conducted an omnibus survey on a random sample of households across the United States, using random digit-dialing. Households were screened with the following two questions:
Is there a male age 18 or over in this household who has ever had problems with pain, pressure or discomfort in the pelvic or bladder area? The pain may or may not make him feel like he needs to urinate frequently.
Have you or another man age 18 or over currently living in this household ever been told by a doctor that you or they have CHRONIC PROSTATITIS or INTERSTITIAL CYSITITIS?
These items were asked to the household member who answered the phone. If this household member was male, he could either identify himself as the person with symptoms or a diagnosis of IC/BPS or CP/CPPS, or he could identify another man in the household who met these criteria. If the household member was female, she was asked to identify a man in the household who might fit the screening criteria. Once an eligible man in the household was identified, the household member was asked whether or not they would give permission for RAND to contact him about the study.
Next, RAND scheduled telephone interviews with the consenting men. In cases where the identified man was reached, the RAND interviewer rescreened them for eligibility. If more than one man in the household met the screening criteria, the man with the most recent birthday was selected. The screener then conducted a series of additional questions based on exclusionary and inclusionary criteria for both conditions. If the respondent screened positive based on these criteria, he was asked to complete a more in-depth interview lasting about one hour. The interview could either be started immediately or scheduled for a more convenient date and time.
The full interview contained questions about the respondent's current and past symptoms related to IC/BPS and CP/CPPS, medical history, experience with physicians, medications, impact on quality of life, physical and mental health status, insurance coverage, work status and history, and other demographic items. After the interview was completed, the respondent received a $50 check by mail. No monetary incentive was provided for completing only the screening portion of the interview.
Statistical Analysis
Non-response weights
Non-response weights are the inverse of predicted probabilities from a multivariate logistic regression model that predicted whether screening occurred among households with at least one male with bladder symptoms and/or a CP/CPPS or IC/BPS diagnosis. Predictors of screening were the respondent's gender, age, race/ethnicity, education level, employment status, marital status, total household income, head of household status, condition status (diagnosis only, symptoms only, or both), homeowner status, and indicators for the household having children under age 6, ages 6-11, and ages 12-17.
Within the logistic regression models, predictors were missing at low rates, and simple imputation was performed for missing values for household income (median) and the number of children (mean).
Overall weights
The final weight for each of the screened cases was calculated by multiplying the ORC weight by the non-response (screening) weight. Because there was no screening-based exclusion of households that did not screen positive, those observations received a non-response weight of 1.
Prevalence estimates
Current Population Survey (CPS) estimates from 2006 were used to estimate the number of males age 18 or older per household. Data were aggregated by household ID and the total number of males age 18 or older was calculated. Households without any males age 18 or older were dropped and the average number of males per household was calculated using the CPS weights.
Prevalence estimates were calculated by dividing the household-level estimate by the CPS-based mean number of males per household. These estimates were based on the 2006 census data for men 18 years or older.14
Results
ORC screened 6,072 households, of which 29 refused to answer the screening question and 794 had no adult male residents. This left 5,249 households that were asked if any adult males in the household had bladder pain. Of these households, 788 screened positive with 421 having respondents with symptoms, 341 having someone else in the household with symptoms, and 26 households having both the respondent and someone else with symptoms. Of the remaining households, 3,995 screened negative, 362 were later determined to not have a male age 18 or older in the household, 91 refused to answer, and 53 did not know whether there was a man in the household with these symptoms.
After the households who did not contain males, refused to answerer, or did not know the answers to the questions were excluded, the remaining 4,796 households were asked if there were any males in the household with a diagnosis of IC/BPPS or CP/CPPS. Of these households, 70 respondents had a diagnosis, 73 responded that someone else in the household had a diagnosis, and 2 responded that both he and someone else in the household had diagnoses (, 90 respondents did not know if anyone had a diagnosis, and 13 refused to answer the question).
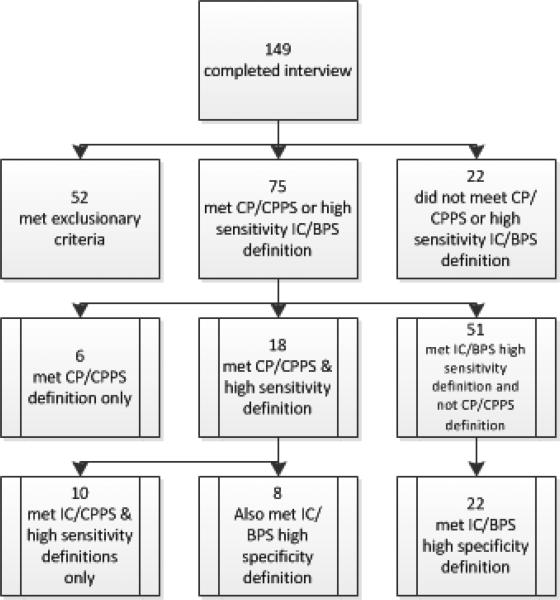
Households that screened positive (823) were asked to be contacted by RAND. Of these, 296 (36.0%) agreed and 223 (27.1%) completed the screening. Of those completing the screening, 74 did not meet the inclusion criteria, leaving 149 who were included and completed the interview, as shown in Figure 1. Ninety-seven men were included in the final analysis; their characteristics appear in Table 1. Of these men, 75 met the CP/CPPS or high sensitivity IC/BPS case definitions. Six out of these 75 men met only the CP/CPPS definition. Eighteen of the 75 men met the CP/CPPS case definition and the IC/BPS high sensitivity definition. Of these 18, 8 also met the IC high specificity definition. 51 of the 75 men did not meet the CP/CPPS case definition but met the IC/BPS high sensitivity definition. Of those men, 22 also met the IC/BPS high specificity definition.
Figure 1.
Flow diagram of the 149 patients who completed the full interview.
Table 1.
Subject characteristics and demographics. Percentages represent weighted values.
| N | Percent | |
|---|---|---|
| Age (in years) | ||
| 18−35 | 6 | 6.2 |
| 36−55 | 34 | 35.1 |
| 56−74 | 44 | 45.4 |
| 75 + | 13 | 13.4 |
| Race/Ethnicity | ||
| White | 83 | 85.6 |
| African American | 8 | 8.3 |
| Other | 6 | 6.2 |
| Educational attainment | ||
| No High School degree | 6 | 6.2 |
| High School degree, but no 4 year college degree | 54 | 55.7 |
| 4 year college degree, but no postgraduate degree | 19 | 19.6 |
| Any post graduate study | 18 | 18.5 |
| Employed in the past month | 37 | 38.1 |
| Total household income | ||
| Don't know | 4 | 4.1 |
| Refused | 8 | 8.2 |
| $21,000-$40,000 | 19 | 19.6 |
| $41,000-$60,000 | 15 | 15.5 |
| $60,000 + | 32 | 33.0 |
Finally, prevalence estimates were calculated. The prevalence estimate for CP/CPPS is 1.8% (95% CI 0.9-2.7%), which equates to 1,986,972 (95% CI 966,042 – 2,996,924) U.S. men. The prevalence of IC/BPS (high sensitivity case definition) is 4.2% (95% CI 3.1-5.3%), which corresponds to 4,610, 653 (95% CI 3,359,190 – 5,862,116) U.S. men, and the prevalence of IC/BPS (high specificity case definition) is 1.9% (95% CI 1.1-2.7%), which corresponds to 2,107,727 (95% CI 1,240,485 – 2,974,969) U.S. men.
A Venn diagram illustrating the amount of overlap of symptoms between respondents who met both the high specificity IC/BPS case definition and the CP/CPPS case definition is shown in Figure 2. Of the men who met the high specificity definition of IC/BPS or the case definition of CP/CPPS, 17% of the men met both.
Figure 2.
Venn diagram showing rela4onship between Chronic Prosta44s (case defini4on) and Inters44al Cys44s (high specificity defini4on) in men who screened posi4ve for symptoms (n=46). Percentages represent weighted values.
Discussion
Prevalence of IC/BPS
There is a great deal of discrepancy among population estimates for IC/BPS in the literature. Since there are no objective markers to establish disease diagnosis, studies have used different methods for estimating prevalence, and these estimates have varied accordingly. Studies that have used self-reported methods have estimated the prevalence of IC/BPS using the 1989 National Health Interview Survey (NHIS) and the National Health and Nutrition Examination Surveys (NHANES) between 1988 and 1994. Both surveys asked the patients, “have you ever had symptoms of a bladder infection (such as pain in your bladder and frequent urination) that lasted more than 3 months?”, and if “yes”, then patients were asked “when you had this condition, were you told that you had interstitial cystitis or painful bladder syndrome?” Only respondents answering “yes” to both questions met the study criteria. The NHIS study estimated that the prevalence of IC/BPS was 500 per 100,000 population, with 60 per 100,000 men, for a total of 82,832 men. 1, 15 This is a much lower estimate than reported in this study. The difference could be due to the particular questions that were asked in this survey, and the need for an actual diagnosis of IC/BPS, rather than simply symptoms of these conditions.
Other studies have used physician diagnosis to estimate IC/BPS prevalence. One such study used electronic health records from the Kaiser Permanente Northwest health maintenance organization database and found that the prevalence of a coded diagnosis of IC (ICD-9 code 595.1) was 197/100,000 women and 41/100,000 men.16 The estimate for men is potentially low because it only represents patients who have sought medical care and who have been assigned a diagnosis, not necessarily representative of the greater population.
A symptoms-based approach to estimating the prevalence of IC/BPS was implemented by ICD-9 based queries of the Kaiser Permanente Northwest database for patients with bladder symptoms. Patients were sent a questionnaire with questions about the presence of IC symptoms and the O'Leary-Sant interstitial cystitis questionnaire. Prevalence estimates ranged from 2.3 to 4.6% in men.8 These estimates are higher than those reported based on physician diagnosis of the same population,16 indicating that IC/BPS might be underdiagnosed. Another study took an epidemiological approach in the Boston area to estimate prevalence of IC/BPS based on patient-reported symptoms. This study found that 1.3% of men reported having symptoms of IC/BPS, as defined as “pain increasing as the bladder fills and/or pain relieved by urination (fairly often, usually, or almost always, considering the last month) present for at least 3 months.”17
Collectively, our IC/BPS prevalence estimates are higher than those reported by the self-reported and physician diagnosis-based methods, but are lower than those based on patient-reported symptoms. We believe that our estimates have the strength of combining the use of validated case definitions and a representative random national sample, making them more accurate than the prevalence estimates using other methods.
Additionally, these prevalence estimates in men are similar in magnitude to those that the RICE study found in females of 6.53%, based on the high sensitivity definition, and 2.70% based on the high specificity definition,18 suggesting that prevalence of IC/BPS differs little by gender.
Prevalence of CP/CPPS
Similarly to IC/BPS, prevalence estimates for CP/CPPS vary based on definitional and methodological parameters. Studies that used the same NIH-CPSI definition of CP/CPPS used in this study obtained prevalence rates that ranged widely from 2.3% to 10.5%.2, 3, 19-24 While many of these studies were performed on populations in different countries,2, 20-24 the range of prevalence rates for CP/CPPS in the United States still varied from 2.3% to 6.3%.3, 5, 19 All of these estimates are higher than what was found in this study.
Our results showed that 17% of patients with symptoms of either IC/BPS (high specificity definition) or CP/CPPS have symptoms of both. These data represent the first systematic evaluation of the co-occurrence of these chronic conditions in men. This is not surprising, given other studies showing a high amount of overlap among men with voiding symptoms and pain.10 The substantial overlap between these two chronic conditions in these data supports the idea that IC/BPS and CP/CPPS may share a common pathophysiological abnormality in men. The considerable overlap between IC/BPS and CP/CPPS also suggests that when treating patients with one of these conditions that there should be heightened suspicion of the presence of the other condition.
The main limitation of this study is that it relies on patient self-reported symptoms and diagnoses. The nature of patient self-reporting introduces an element of recall bias to the study. Additionally, the case definitions used for IC/BPS were based on definitions that our group validated in females. These definitions have not been validated in males; instead, they were modified from our female definitions. We assume that the sensitivity and specificity values will be similar between men and women, with perhaps improved specificity in men due to fewer competing exclusionary diagnoses. Another limitation to our study is that we had a response rate of 36%. Of note, this response rate was similar to that of 39.3% in females in the RICE study.18 For these reasons, we weighted our data for non-responders based on weighting criteria used by our group for females with IC/BPS. We believe that these methods should offset the lower response rate and ensure the validity of our results.
Conclusions
The prevalence of and the degree of overlap between IC/BPS and CP/CPPS in United States men are higher than previously thought. These estimates suggest that these conditions are widespread and that they might be underdiagnosed and undertreated by physicians. Patients who have one disorder should also be evaluated for symptoms of the other disorder.
Acknowledgments
Supported by National Institute of Diabetes and Digestive Kidney Diseases Grant U10DK070234-01
References
- 1.Payne CK, Joyce GF, Wise M, et al. Interstitial cystitis and painful bladder syndrome. J Urol. 2007;177:2042. doi: 10.1016/j.juro.2007.01.124. [DOI] [PubMed] [Google Scholar]
- 2.Nickel JC, Downey J, Hunter D, et al. Prevalence of prostatitis-like symptoms in a population based study using the National Institutes of Health chronic prostatitis symptom index. J Urol. 2001;165:842. [PubMed] [Google Scholar]
- 3.Roberts RO, Jacobson DJ, Girman CJ, et al. Prevalence of prostatitis-like symptoms in a community based cohort of older men. J Urol. 2002;168:2467. doi: 10.1016/S0022-5347(05)64170-5. [DOI] [PubMed] [Google Scholar]
- 4.Clemens JQ, Brown SO, Kozloff L, et al. Predictors of symptom severity in patients with chronic prostatitis and interstitial cystitis. J Urol. 2006;175:963. doi: 10.1016/S0022-5347(05)00351-4. [DOI] [PubMed] [Google Scholar]
- 5.Daniels NA, Link CL, Barry MJ, et al. Association between past urinary tract infections and current symptoms suggestive of chronic prostatitis/chronic pelvic pain syndrome. J Natl Med Assoc. 2007;99:509. [PMC free article] [PubMed] [Google Scholar]
- 6.Cheah PY, Liong ML, Yuen KH, et al. Chronic prostatitis: symptom survey with follow-up clinical evaluation. Urology. 2003;61:60. doi: 10.1016/s0090-4295(02)02081-2. [DOI] [PubMed] [Google Scholar]
- 7.Link CL, Pulliam SJ, Hanno PM, et al. Prevalence and psychosocial correlates of symptoms suggestive of painful bladder syndrome: results from the Boston area community health survey. J Urol. 2008;180:599. doi: 10.1016/j.juro.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clemens JQ, Meenan RT, O'Keeffe Rosetti MC, et al. Prevalence of interstitial cystitis symptoms in a managed care population. J Urol. 2005;174:576. doi: 10.1097/01.ju.0000165170.43617.be. [DOI] [PubMed] [Google Scholar]
- 9.Roberts RO, Lieber MM, Rhodes T, et al. Prevalence of a physician-assigned diagnosis of prostatitis: the Olmsted County Study of Urinary Symptoms and Health Status Among Men. Urology. 1998;51:578. doi: 10.1016/s0090-4295(98)00034-x. [DOI] [PubMed] [Google Scholar]
- 10.Clemens JQ, Markossian TW, Meenan RT, et al. Overlap of voiding symptoms, storage symptoms and pain in men and women. J Urol. 2007;178:1354. doi: 10.1016/j.juro.2007.05.157. [DOI] [PubMed] [Google Scholar]
- 11.Berry SH, Bogart LM, Pham C, et al. Development, validation and testing of an epidemiological case definition of interstitial cystitis/painful bladder syndrome. J Urol. 2010;183:1848. doi: 10.1016/j.juro.2009.12.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clemens JQ, Hilton L, Suttorp M, et al. Identifying chronic prostatitis/chronic pelvic pain syndrom for epidemiologic studies. American Urological Association; San Francisco: 2010. [Google Scholar]
- 13.Litwin MS, McNaughton-Collins M, Fowler FJ, Jr., et al. The National Institutes of Health chronic prostatitis symptom index: development and validation of a new outcome measure. Chronic Prostatitis Collaborative Research Network. J Urol. 1999;162:369. doi: 10.1016/s0022-5347(05)68562-x. [DOI] [PubMed] [Google Scholar]
- 14.Bureau USC. General demographic characteristics. 2006;2011 [Google Scholar]
- 15.Jones CA, Nyberg L. Epidemiology of interstitial cystitis. Urology. 1997;49:2. doi: 10.1016/s0090-4295(99)80327-6. [DOI] [PubMed] [Google Scholar]
- 16.Clemens JQ, Meenan RT, Rosetti MC, et al. Prevalence and incidence of interstitial cystitis in a managed care population. J Urol. 2005;173:98. doi: 10.1097/01.ju.0000146114.53828.82. [DOI] [PubMed] [Google Scholar]
- 17.Hall SA, Link CL, Pulliam SJ, et al. The relationship of common medical conditions and medication use with symptoms of painful bladder syndrome: results from the Boston area community health survey. J Urol. 2008;180:593. doi: 10.1016/j.juro.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 18.Berry SH, Elliott MN, Suttorp M, et al. Prevalence of symptoms of bladder pain syndrome/interstitial cystitis among adult females in the United States. J Urol. 2011;186:540. doi: 10.1016/j.juro.2011.03.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clemens JQ, Meenan RT, O'Keeffe-Rosetti MC, et al. Prevalence of prostatitis-like symptoms in a managed care population. J Urol. 2006;176:593. doi: 10.1016/j.juro.2006.03.089. [DOI] [PubMed] [Google Scholar]
- 20.Walz J, Perrotte P, Hutterer G, et al. Impact of chronic prostatitis-like symptoms on the quality of life in a large group of men. BJU Int. 2007;100:1307. doi: 10.1111/j.1464-410X.2007.07250.x. [DOI] [PubMed] [Google Scholar]
- 21.Tripp DA, Nickel JC, Ross S, et al. Prevalence, symptom impact and predictors of chronic prostatitis-like symptoms in Canadian males aged 16-19 years. BJU Int. 2009;103:1080. doi: 10.1111/j.1464-410X.2008.08157.x. [DOI] [PubMed] [Google Scholar]
- 22.Liang CZ, Li HJ, Wang ZP, et al. The prevalence of prostatitis-like symptoms in China. J Urol. 2009;182:558. doi: 10.1016/j.juro.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 23.Kunishima Y, Mori M, Kitamura H, et al. Prevalence of prostatitis-like symptoms in Japanese men: Population-based study in a town in Hokkaido. Int J Urol. 2006;13:1286. doi: 10.1111/j.1442-2042.2004.01556.x. [DOI] [PubMed] [Google Scholar]
- 24.Marszalek M, Wehrberger C, Temml C, et al. Chronic pelvic pain and lower urinary tract symptoms in both sexes: analysis of 2749 participants of an urban health screening project. Eur Urol. 2009;55:499. doi: 10.1016/j.eururo.2008.03.073. [DOI] [PubMed] [Google Scholar]