Abstract
Background
The impact of specialization on the practice of general surgery has not been characterized. Our goal was to assess general surgeons’ operative practices to inform surgical education and workforce planning.
Study Design
We examined the practices of general surgeons identified in the 2008 State Inpatient and Ambulatory Surgery Databases of the Healthcare Cost and Utilization Project (HCUP) for three US states. Operations were identified using ICD-9 and CPT codes linked to encrypted physician identifiers. For each surgeon, total operative volume and the percentage of practice comprised of their most common operation were calculated. Correlation was measured between general surgeons’ case volume and the number of other specialists in a health service area.
Results
There were 1,075 general surgeons who performed 240,510 operations in 2008. The mean operative volume for each surgeon was 224 annual procedures. General surgeons performed an average of 23 different types of operations. For the majority of general surgeons, their most common procedure comprised no more than 30% of total practice. The most common operations, ranked by the frequency that they appeared as general surgeons’ top procedure, included: cholecystectomy, colonoscopy, endoscopy, and skin excision. The proportion of general surgery practice comprised of endoscopic procedures inversely correlated with the number of gastroenterologists in the health service area (Rho = - 0.50, p = 0.005).
Conclusions
Despite trends toward specialization, the current practices of general surgeons remain heterogeneous. This indicates a continued demand for broad-based surgical education to allow future surgeons to tailor their practices to their environment.
Keywords: General Surgery, Workforce, Surgical Education, Specialization, Case-Mix
Introduction
The field of surgery is becoming increasingly specialized. As the majority of graduating general surgery residents pursues fellowship training 1-2, the traditional five-year general surgery residency needs to be re-evaluated. Disciplines that historically were part of the general surgical curriculum, including obstetrics and gynecology, orthopedics, otolaryngology, and urology, are no longer practiced by the majority of general surgeons and are therefore not emphasized or are often not included in current general surgical training. As more specialties emerge, the field of general surgery has become more ambiguous. Upon re-certification, 32% of board certified general surgeons reported having a subspecialty certificate in Surgical Critical Care, Pediatric Surgery, Vascular Surgery, Surgery of the Hand, Colorectal Surgery, Plastic Surgery, or Thoracic Surgery3. An untold number of other general surgeons have subspecialty practices in Surgical Oncology, Advanced Gastrointestinal and Laparo-endoscopic Surgery, Breast Surgery, Endocrine Surgery, Transplantation, or Acute Care Surgery.
This prevalence of specialization might suggest that many surgeons solely perform a defined subset of procedures and only use a portion of the general surgical education that they obtained in residency. This would favor a system with 3 years of general surgery and 3 years of specialty training, or 5 years of subspecialty integrated training, which has been proposed and implemented in some disciplines 4-7. However, preparing trainees for contemporary practice requires an understanding of what general surgeons actually do in practice. This study sought to determine whether general surgeons tend to specialize in a small number of procedures or maintain a broad, heterogeneous case-mix.
Understanding general surgeons’ case-mix will not only inform surgical education, but will also assist in workforce planning and allocation of health services. The Affordable Care Act has mandated that 75% of new residency positions be designated for either primary care or general surgery, in an effort to prevent projected physician shortages 8. A previous study by Stitzenberg and Sheldon projected that progressive sub-specialization within general surgery would lead surgeons to narrow their scope of practice, leading to a shortfall of surgical services 2. To cover the breadth of demand for surgical services, it was postulated that a larger number of surgeons would be required. As general surgical education is re-designed to meet current demands, it will be important to understand which procedures general surgeons perform and how varied their case-mix is.
Methods
Design
This was a retrospective observational study of a population-based cohort.
Data Sources
Data from the 2008 State Inpatient and State Ambulatory Databases of the Healthcare Cost and Utilization Project (HCUP) was obtained from Maine, South Carolina, and Wisconsin. These states were chosen because their datasets were among the few statewide datasets that included information on surgeon specialty. At the time of this study, 2008 data was the most current available in all states.
Population-level Data
Hospital identifiers and hospital zip codes were used to link the HCUP data with the 2009 Area Resource File 9, a national county-level health resource information database of the Health Resources & Services Administration. The Area Resource File was used to identify health service areas (HSAs). HSAs were defined according to the National Center for Health Statistics, which designates them as a single county or cluster of contiguous counties that are relatively self-contained with respect to hospital care. Hospital identifiers and hospital zip codes were not available in the data for South Carolina. Therefore HCUP data from Maine and Wisconsin were used to analyze population-level practice patterns.
Individual Surgeon-Level Data
Encrypted physician identifiers were used to analyze practice patterns and case-mix at the level of each surgeon. General surgeons, surgical sub-specialists, and gastroenterologists were identified using HCUP physician specialty codes. The codes are based on attending physician specialty as provided by the data organizations, which included Maine Health Data Organization, the South Carolina Budget and Control Board Office of Research & Statistics, the Wisconsin Hospital Association and Wisconsin Department of Health Services. South Carolina reports physician specialty as the area in which the physician spends the most hours per week, as reported by the physician at license renewal. If the physician does not report hours, South Carolina assigns physician specialty as the first practice type reported by the physician.
Information from patient encounters was linked to individual general surgeons for analysis. Patient encounters included in the analysis involved a general surgeon as the admitting/primary provider, without a secondary provider; or a general surgeon as the consulting/secondary provider. All other encounters were excluded.
Procedure Variables
Surgical procedures were identified using ICD-9 and CPT codes, then classified into categories using modified HCUP Clinical Classification Software (CCS) 10-11. The HCUP-CCS categories were modified to capture all procedures that a general surgeon could potentially perform, and classify them into surgically meaningful categories. Three surgical research fellows independently reviewed the HCUP-CCS categorization of each procedure code. Redundant or indistinct HCUP-CCS-defined categories were eliminated, and their ICD-9 and CPT codes were re-assigned to modified categories. The final classifications were revised and reviewed by a board-certified general surgeon. Ultimately 210 types of procedures were designated as operations that a general surgeon could potentially perform. The primary procedure for each patient encounter was analyzed.
Analysis
The total number of general surgeons in each state and the number of general surgeons per 100,000 people in each state were calculated using 2008 US Census data 12. The total annual volume and number of different types of operations were calculated for each surgeon. General surgeons who performed fewer than 10 procedures annually were excluded from the analysis, as case-mix could not be reliably determined. Additionally, general surgeons with more than 1,000 procedures per year were excluded in order to achieve a representative sample for analysis and avoid skewing results toward those with the highest case-volumes. Hence, general surgeons at both extremes of the case volume spectrum were excluded in order to characterize the case-mix of the typical general surgeon and avoid skew toward the extremes.
The most common operation was then identified for each surgeon and the percentage of practice comprised of that operation was calculated. The volume of each surgeon’s most common operation was measured in proportion to the statewide total volume for that type of operation. The most common operations for all general surgeons were identified by ranking according to the frequency that they appeared as a general surgeon’s top procedure. To determine whether the top procedure was indicative of case-mix, surgeons were grouped by their top procedure and the second most common procedure for the majority of these surgeons was assessed for similarity. To assess the overall volume of procedures in the cohort, the procedures with the largest overall volume in the cohort were then identified.
Correlation between the number of procedures performed by general surgeons and the number of specialists in a health service area was measured using the Spearman correlation coefficient. A subgroup analysis was performed to analyze the practices of high volume surgeons who performed 25% or more of the statewide total for a given type of operation.
Results
Cohort
Of 1,540 general surgeons identified in HCUP data from 2008, 443 were found to have fewer than 10 annual procedures and were excluded from the cohort as described above. This excluded 18 of 188 (10%) general surgeons in Maine, 43 of 327 (13%) in South Carolina, and 382 of 1025 (37%) in Wisconsin. An additional 22 (2%) general surgeons had over 1,000 annual procedures and were excluded from the cohort to achieve a representative sample. The majority of these surgeons’ procedures included colonoscopies, upper endoscopies, and wound debridement. The final cohort included 1,075 general surgeons in the three states. There were 6 general surgeons per 100,000 people in South Carolina, 12 per 100,000 in Maine, and 11 per 100,000 in Wisconsin (Table 1).
Table 1.
Summary of Number of Surgeons, Volume, and Case-Mix
| State | General surgeons with ≥10 and ≤1,000 procedures annually, n |
General surgeons per 100,000 people, % |
Mean no. of procedures per surgeon, n |
Mean no. of different types of procedures per surgeon, n (range) |
|---|---|---|---|---|
| Maine | 165 | 12.4 | 303 | 28 (2- 62) |
| Sout Carolina |
281 | 6.2 | 338 | 35 (2- 73) |
| Wisconsin | 629 | 11.2 | 152 | 16 (1- 51) |
| Combined | 1075 | - | 224 | 23 (1- 73) |
Volume
General surgeons performed 274,273 operations in Maine, South Carolina, and Wisconsin in 2008, with a mean total operative volume of 224 procedures (median 132) per surgeon that year. Most Common Operations Cholecystectomy was the most common procedure for the largest number of surgeons. When cholecystectomy was surgeons’ top procedure, it comprised 6 to 60% of those surgeons’ practices (Table 2). Bowel resection was the second most common procedure for the majority of those surgeons (Table 3). Colonoscopy and upper endoscopy played a significant role in many surgeons’ practices, as either their top procedure or second most common procedure (Table 2). Skin excision and wound debridement were the most common operations for a significant proportion of general surgeons as well, making up 11 to 100% of their practices. Breast lumpectomy was also among the top ten most common procedures. For surgeons whose most common procedure was breast lumpectomy, cholecystectomy was largely the second most common procedure (Table 3). These analyses were repeated with and without the exclusion of surgeons who had fewer than 10 or more than 1000 annual procedures. Ranking of the first and second most common operations remained in the same order. Procedures were also analyzed by state, and results identified the same top ten procedures with only slightly different rank order for each state.
Table 2.
Ten Most Common Operations - Ranked According To Frequency That They Appeared As General Surgeons’ Top Procedure
| Most common operations | General surgeons, n |
Individual practice comprised of top procedure, %, mean (range) |
|---|---|---|
| Cholecystectomy | 269 | 24 (6-60) |
| Colonoscopy | 216 | 38 (11-98) |
| Upper GI endoscopy | 121 | 33 (13-79) |
| Skin excision | 62 | 28 (12-100) |
| Inguinal or femoral hernia repair | 59 | 27 (10-71) |
| Debridement of wound, infection, or burn | 43 | 33 (11-98) |
| Breast lumpectomy | 32 | 41 (14-89) |
| Hemodialysis and peritoneal dialysis access | 22 | 36 (14-73) |
| Colorectal resection | 19 | 25 (10-47) |
| Therapeutic gastric procedures | 17 | 34 (15-83) |
Table 3.
First and Second Most Common Operations for General Surgeons
| Top procedures | Second most common operation for the majority of surgeons with the paired top procedure |
||
|---|---|---|---|
| Surgeons, most common procedure, n |
Procedure | Surgeons, second most common procedure, n |
|
| Cholecystectomy | 269 | Colorectal resection | 39 of 269 |
| Colonoscopy | 216 | Upper GI endoscopy | 109 of 216 |
| Upper GI endoscopy | 121 | Colonoscopy | 42 of 121 |
| Skin excision | 62 | Cholecystectomy | 14 of 62 |
| Inguinal or femoral hernia repair | 59 | Cholecystectomy | 27 of 59 |
| Debridement of wound, infection, or burn |
43 | Excision of skin/subcutaneous | 12 of 43 |
| Breast lumpectomy | 32 | Cholecystectomy | <12 of 32 |
| Hemodialysis and peritoneal dialysis access |
22 | Peripheral Vascular Bypass | <12 of 22 |
| Colorectal resection | 19 | Cholecystectomy | <12 of 19 |
| Therapeutic gastric procedures | 17 | Cholecystectomy | <12 of 17 |
Individual surgeons’ most common procedures (Table 3) were then compared to the largest volume procedures in the overall cohort (Table 4). Colonoscopy made up the largest proportion of the overall cohort case volume.
Table 4.
List of 20 Procedures with the Largest Volume in the General Surgeon Cohort
| Procedure | Cohort no. of annual procedures, n=274,273 |
Cohort case volume, % |
|---|---|---|
| Colonoscopy | 51,649 | 19 |
| Cholecystectomy | 24,333 | 9 |
| Upper GI endoscopy | 22,987 | 8 |
| Inguinal or femoral hernia repair | 16,900 | 6 |
| Skin excision | 14,568 | 5 |
| Ventral and paraesophageal hernia repair | 11,791 | 4 |
| Breast lumpectomy | 10,541 | 4 |
| Wound debridement | 9,801 | 4 |
| Lower GI endoscopy | 9,705 | 4 |
| Central venous or arterial catheter | 8,322 | 3 |
| Appendectomy | 6,826 | 2 |
| Incision and drainage of soft tissue | 5,922 | 2 |
| Colorectal resection | 5,626 | 2 |
| Hemo- and peritoneal dialysis access | 4,581 | 2 |
| Therapeutic gastric procedure | 4,022 | 1 |
| Diagnostic lymphatic procedure | 4,152 | 2 |
| Breast biopsy | 3,642 | 1 |
| Hemorrhoid procedures | 3,177 | 1 |
| Thyroid and parathyroidectomy | 2,993 | 1 |
| Major anorectal procedure | 2,894 | 1 |
Individual Surgeon Case-mix
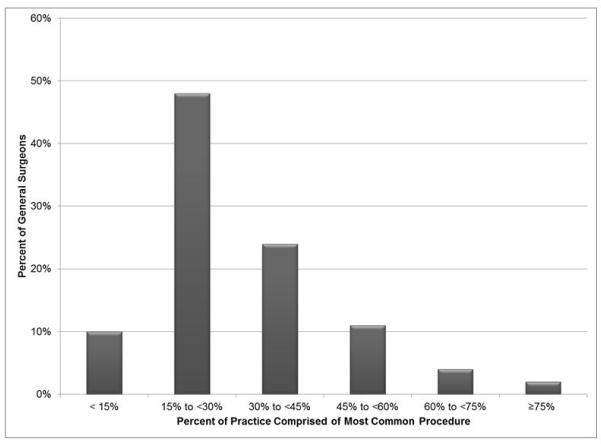
General surgeons performed a mean of 23 different types of operations (Table 1), with a range from 1 to 73 different types of operations. For the majority of surgeons, their most common procedure comprised no more than 30% of total practice (Figure 1). The remaining 70% of most surgeons’ practices were therefore made up of over 20 different kinds of operations. Only 2% of general surgeons devoted over 75% of their practice to their most common procedure.
Figure 1.
Distribution of general surgeons’ practice that is comprised of their most common procedure.
Practice environment
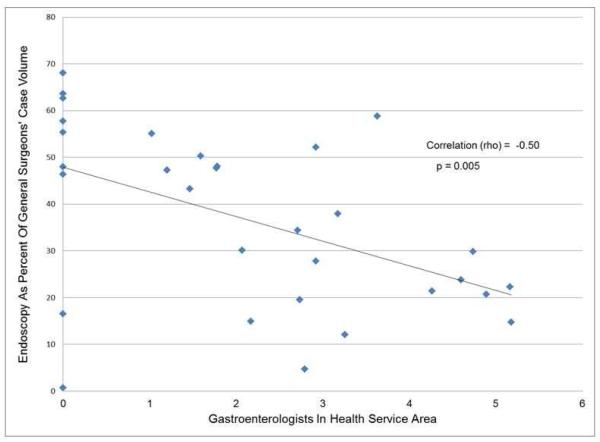
Given that colonoscopy and upper endoscopy were among the most common procedures, correlation was measured between general surgeons’ volume of endoscopic procedures relative to the number of local gastroenterologists. The endoscopic procedures included upper GI endoscopy, colonoscopy, proctoscopy, and endoscopic retrograde cholangiopancreatography. The total number of endoscopic procedures performed by general surgeons was inversely correlated with the number of gastroenterologists in a given health service area (Figure 2). The Spearman correlation coefficient was −0.50 and p = 0.005, indicating a small but statistically significant relationship between surgeons’ case-mix and the number of gastroenterologists nearby.
Figure 2.
Correlation between endoscopy as a percentage of surgeons’ case volume and number of gastroenterologists in the health service area.
Subgroup Analysis: High volume general surgeons
There were 31 high volume general surgeons (3% of cohort) whose most common procedure made up 25% or more of their state’s total volume for that particular type of procedure. High volume general surgeons’ most common procedures included skin graft, gastric bypass, pancreatic resection, pneumonectomy, thyroid and parathyroid surgeries, as well as other less common procedures. For these surgeons, their most common procedure comprised an average of 40% of their individual practice and they performed a mean of 20 different types of procedures annually (Range 1 to 58).
Discussion
Overall this study demonstrates that many general surgeons’ practices remain heterogeneous despite trends toward specialization; and there is a broad array of core general surgical procedures that a significant proportion of surgeons perform in addition to their most common procedure.
The number of general surgeons per 100,000 people in the three states was as expected, relative to the 6 per 100,000 people reported nationally 13. South Carolina had the national average, while Maine and Wisconsin had approximately twice the national average of general surgeons. It is also worth noting that 21% of South Carolina, 66% of Maine, and 79% of Wisconsin’s population reside in metropolitan areas while the remaining population lives in rural areas. These proportions can be compared to 90% of the US population that resides in metropolitan areas14. While the three states studied may comprise an oversampling of the rural US, their data represent the spectrum of both rural and major metropolitan practice settings.
About one tenth of general surgeons in Maine and South Carolina, and one third of the general surgeon workforce in Wisconsin performed fewer than 10 procedures annually. A potential explanation for this is the use of locum tenens surgeons who fill short-term service needs. A recent study found that locum tenens surgeons were hired in 15% of surveyed hospitals in small urban clusters of 2,500 to 9,999 people, small towns with high commuting to small urban clusters, small towns with low commuting, and isolated rural areas 15. The proportion of Rural Urban Commuting Areas that meet this description is three times higher in Wisconsin, compared to Maine and South Carolina 14.The use of locum tenens, the regionalization of healthcare across states 16,17 as well as the retirement of a large proportion of general surgeons 18,19 likely explain the proportions of surgeons with fewer than 10 procedures. In this study, general surgeons with fewer than 10 or greater than 1000 annual procedures were excluded to characterize the typical general surgery practice and avoid skew toward the extremes. However, in a post hoc analysis in which all general surgeons were included, we found that the first and second most common operations in Tables 2 & 3, as well as the results in Figure 2, remained the same. This supported the internal validity of our findings.
General surgeons’ mean annual operative volume of 224 operations in this study was similar to recently published data from American Board of Surgery certified surgeons in Florida who performed 228 to 456 procedures annually 20. The case-mix mean of 23 different types of surgery in our study is consistent with findings from a recent study showing that surgeons manage a wide variety of primary diagnoses, with 136 to 236 different primary diagnoses per full time equivalent (FTE) 21. The average surgeon in our study devoted less than 30% of their practice to their most common procedure, and their second most common procedure was often unrelated. This demonstrated that there is significant heterogeneity in the practice of general surgery. For example, one might expect that the majority of the surgeons whose most common procedure was lumpectomy would perform mastectomies or breast biopsies as their second most common procedure; but this was not the case, their second most common procedure was cholecystectomy. There were rare cases in which one type of procedure made up more than 75% of a surgeon’s practice. Colonoscopy, upper endoscopy, and therapeutic gastric procedures made up 11-98% of some surgeon’s practices. Previous studies of general surgeons’ practice patterns confirm this demand for endoscopies and colonoscopies, particularly in rural practices 3,22-24. We further explored the relationship between the practice environment and the number of endoscopic procedures performed by surgeons. We found a statistically significant inverse correlation between the number of gastroenterologists in the health service area and the number of endoscopic procedures performed by general surgeons. This suggests that general surgeons adapt their practices to the environment and needs of the community, broadening or narrowing their scope in relation to other providers.
Wound debridement and skin excision were also among general surgeons’ most common procedures, making up 11 to 100% of a practice when it appeared as surgeons’ top procedure. Evidence of general surgeons devoting a bulk of their practice to wound debridement exists in a number of positions available nationwide for full and part-time general surgeons to join wound management practices, podiatry groups, and venous disease clinics 25. It is unclear whether this reflects healthcare consumer-driven demand for these subspecialists, need for subspecialists to manage increasingly complex disease, or other surgeons’ desire to exclude these types of cases from their practice. Nonetheless there is evidence that only a minority of surgeons have devoted the bulk of their practice to one type of procedure.
Given the increasing efforts by Medicare and healthcare quality agencies to reward high volume centers 26, one might expect that surgeons who draw a high volume of referrals for a given type of procedure would devote most of their practice to one procedure. However this study showed that high volume surgeons only devoted 40% of their practice to their most common procedure. These surgeons performed a mean of 20 different types of procedures annually, compared to the entire cohort mean of 23 different types of procedures.
The goal of this study was to assess the operative practice of the typical general surgeon in the United States, and this was achieved with some limitations. Statewide data from the Healthcare Cost & Utilization Project (HCUP) was used to approximate national trends. However, encrypted physician identifiers and linked physician specialty codes were only available for three states. Despite this limitation, our results consistently demonstrated that the majority of general surgeons’ most common procedure made up no more than 30% of individual practice when analyzed by state and in aggregate. Additionally the ten most common operations remained the same, with only slight changes in rank when analyzed by state. The fact that results remained consistent when analyzed both by state and in aggregate lends validity to our findings. It is unlikely that the three states studied represent one extreme in the US surgical case-mix spectrum, given the large geographic and demographic differences between the states 9,12, 14. Given that the data for this study was limited to three geographically dispersed states, our analysis was unable to capture the case-mix of surgeons who practice in more than one state within a region. This could be one explanation for the proportion of surgeons with fewer than 10 procedures. Another limitation to this assessment of general surgery practice was the availability of current data. At the time of this analysis, 2008 data was the most current data available. HCUP obtains data from state agencies or their designees that manage the original data. For this study, patient level data was merged with provider data from the National Provider Identifier (NPI) file, encrypted physician identifiers were then created by the agency before releasing the data for research. It is possible that trends towards sub-specialization have continued to increase since 2008, which would not be reflected in this study. However, trends toward sub-specialization far preceded this study, with 74% of residents entering fellowships in 1993 and 79% in 2005 1. Therefore we expected sub-specialization to impact the practices of general surgeons in 2008, but we did not find general surgeons’ scope of practice to be as narrow as expected.
It is possible that specialization within general surgery, when faced with continued demands for a wide breadth of surgical services, has led surgeons to narrow their scope less than what was projected by Stitzenberg and Sheldon 2. Our study shows that many general surgeons still have broad and heterogeneous practices. This conclusion is also supported by findings from previous studies which demonstrated that general surgeons perform a broad variety of procedures that span the sub-specialties 3, the clinical classification system 20, and various ICD-9 diagnoses 21. These results have significant implications for surgical education in an era of increasing healthcare specialization. A 2004 survey found that most general surgeons, with and without fellowship training, continued to practice broad-based general surgery and reported that such training was relevant to their current practice 27. It is likely that the 2008 cohort in this study would have reported the same.
Findings from our study suggest that surgical education should be broad-based to allow surgeons to tailor their practices to meet the needs of their communities and institutions. The American College of Surgeons has introduced the Transition to Practice Fellowship in General Surgery, 28 which may assist general surgeons entering practice in refining their skills while establishing themselves in a new environment. Other innovative approaches, such as surgical coaching,29 can help new attending surgeons transition into practices that will serve the growing need for surgical services in communities throughout the country.
Acknowledgment
The authors appreciate the assistance of Qianqian Zhao for supplemental statistical programming support.
Funding support: Dr Decker is supported by a NIH T32 Surgical Oncology Research Training Grant T32CA090217; Dr Dodgion was supported by the Brigham and Women’s Hospital, Center for Surgery and Public Health, Arthur Tracy Cabot Fellowship and a NIH Surgical Oncology Research Training Grant (T32 CA009535-23); Dr Hu was supported by a NIH Alimentary Tract Surgery Research Training Grant (2T32DK00754-12).
Abbreviations/ Acronyms
- (HCUP)
Healthcare Cost and Utilization Project
- (CCS)
Clinical classification Software
- (ICD-9)
International Classification of Diseases
- (CPT)
Current Procedural Terminology
- (FTE)
Full Time Equivalent
- (ME)
Maine
- (SC)
South Carolina
- (WI)
Wisconsin
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Information: Nothing to disclose.
Presented at the American College of Surgeons 97th Annual Clinical Congress, San Francisco, CA, October 2011.
References
- 1.Borman KR, Vick LR, Biester TW, Mitchell ME. Changing demographics of residents choosing fellowships: long-term data from the American Board of Surgery. J Am Coll Surg. 2008;206:782–788. doi: 10.1016/j.jamcollsurg.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 2.Stritzenberg KB, Sheldon GF. Progressive specialization within general surgery: adding complexity of workforce planning. J Am Coll Surg. 2005;201:925–93. doi: 10.1016/j.jamcollsurg.2005.06.253. [DOI] [PubMed] [Google Scholar]
- 3.Valentine JR, Jones AT, Biester TW, et al. General surgery workloads and practice patterns in the United States, 2007-2009: a 10-year update from the American Board of Surgery. Ann Surg. 2011;254:520–526. doi: 10.1097/SLA.0b013e31822cd175. [DOI] [PubMed] [Google Scholar]
- 4.Bass BL. Early specialization in surgical training: an old concept whose time has come? Sem Vasc Surg. 2006;19:214–217. doi: 10.1053/j.semvascsurg.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 5.Grosfield JL. General surgery fellowship training: mutually beneficial or competing entities? Surgery. 2002;132:526–528. doi: 10.1067/msy.2002.127696. [DOI] [PubMed] [Google Scholar]
- 6.Sachdeva AK, Bell RH, Britt LD, et al. National efforts to reform residency education in surgery. Acad Med. 2007;82:1200–1210. doi: 10.1097/ACM.0b013e318159e052. [DOI] [PubMed] [Google Scholar]
- 7.Stain SC, Biester TW, Hanks JB, et al. Early tracking would improve the operative experience of general surgery residents. Ann Surg. 2010;252:445–449. doi: 10.1097/SLA.0b013e3181f0d105. [DOI] [PubMed] [Google Scholar]
- 8.U.S. Government Printing Office [Accessed September 9, 2012];Public Law 111-148 The Patient Protection and Affordable Care. 2010 Mar 23; http://www.gpo.gov/fdsys/pkg/PLAW-111publ148/content-detail.html.
- 9.US Department of Health and Human Services [Accessed September 9, 2012];Area Resource File (ARF) 2008. http://www.arf.hrsa.gov/
- 10.HCUP Clinical Classifications Software for Services and Procedures . Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality; Rockville, MD: [Accessed September 9, 2012]. 2004. http://www.hcup-us.ahrq.gov/toolssoftware/ccs_svcsproc/ccssvcproc.jsp. [Google Scholar]
- 11.Duffy SQ, Elixhauser A, Sommers JP. Healthcare Cost and Utilization Project (HCUP 3) Research Note 5. Agency for Health Care Policy and Research; Rockville, MD: 1996. Diagnosis and procedure combinations in hospital inpatient data. AHCPR Pub. No. 96-0047. [Google Scholar]
- 12.U.S. Census Bureau [Accessed September 9, 2012]; http://www.census.gov/
- 13.Lynge DC, Larson EH, Thompson MJ, et al. A longitudinal analysis of the general surgery workforce in the United States, 1981-2005. Arch Surg. 2008;143:345–350. doi: 10.1001/archsurg.143.4.345. [DOI] [PubMed] [Google Scholar]
- 14.US Department of Agriculture, Economic Research Service [Accessed April 22, 2013];Rural Urban Commuting Area Codes. Available at http://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx.
- 15.Doty B, Andres M, Zuckerman R, Borgstrom D. Use of locum tenens surgeons to provide surgical care in small rural hospitals. World J Surg. 2009;33:228–232. doi: 10.1007/s00268-008-9820-5. [DOI] [PubMed] [Google Scholar]
- 16.Birkmeyer JD, Siewers AE, Marth NJ, Goodman DC. Regionalization of high-risk surgery and implications for patient travel times. JAMA. 2003;290:2703–2708. doi: 10.1001/jama.290.20.2703. [DOI] [PubMed] [Google Scholar]
- 17.Peterson OL, Bloom BS. Regionalization of surgical services. Am J Public Health. 1983;73:179–183. doi: 10.2105/ajph.73.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jonasson O, Kwakawa F. Retirement age and the work force in general surgery. Ann Surg. 1996;224:574–579. doi: 10.1097/00000658-199610000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams TE, Ellison EC. Population analysis predicts a future critical shortage of general surgeons. Surgery. 2008;144:548–554. doi: 10.1016/j.surg.2008.05.019. [DOI] [PubMed] [Google Scholar]
- 20.Studnicki J, Fisher JW, Tsulukidze MM, et al. Career phase of board-certified general surgeons: workload composition and outcomes. Arch Surg. 2011;146:1307–1313. doi: 10.1001/archsurg.2011.265. [DOI] [PubMed] [Google Scholar]
- 21.Semel ME, Bader AM, Marston A, et al. Measuring the range of services clinicians are responsible for in ambulatory practice. J Eval Clin Pract. 2012;18:404–408. doi: 10.1111/j.1365-2753.2010.01598.x. [DOI] [PubMed] [Google Scholar]
- 22.Ritchie WP, Rhodes RS, Biester TW. Work loads and practice patterns of general surgeons in the United States, 1995-1997: A report from the American Board of Surgery. Ann Surg. 1999;230:533–542. doi: 10.1097/00000658-199910000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sariego J. The role of the rural surgeon as endoscopist. Am Surg. 2000;66:1176–1178. [PubMed] [Google Scholar]
- 24.Zuckerman R, Doty B, Bark K, Heneghan S. Rural versus non-rural differences in surgeon performed endoscopy: results of a national survey. Am Surg. 2007;73:903–905. [PubMed] [Google Scholar]
- 25.ACS Career Opportunities [Accessed April 22, 2013];American College of Surgeons. http://www.healthecareers.com/acs.
- 26.Centers for Medicare & Medicaid Services [Accessed April 22, 2013];Medicare Approved Facilities/Trials/Registries. Available at http://www.cms.gov/Medicare/Medicare-General-Information/MedicareApprovedFacilitie/index.html?redirect=/medicareapprovedfacilitie/nopr/list.asp.
- 27.Cheadle WG, Franklin GA, Richardson D, Polk HC. Broad-based general surgery training is a model of continued utility for the future. Ann Surg. 2004;239:627. doi: 10.1097/01.sla.0000124384.08410.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hoyt DB. Executive Director’s Report: Looking Forward—February 2013. Bull of the ACS. 2013 http://bulletin.facs.org/2013/02/looking-forward-february-2013. [Google Scholar]
- 29.Hu YY, et al. Postgame analysis: using video-based coaching for continuous professional development. J Am Coll Surg. 2012;214:115–124. doi: 10.1016/j.jamcollsurg.2011.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]