Abstract
Schwannomas are rarely located in the pelvis. A 54-year-old woman was found incidentally to have a tumor in the abdomen. Abdominal computed tomography and magnetic resonance imaging revealed a well-defined, heterogeneous tumor, 5 cm in diameter, in the pelvic cavity. With a diagnosis of a mesenteric tumor, a laparoscopic procedure was performed. Intra-operatively, an elastic tumor was identified in the pelvis adjacent to the right internal iliac vein and ureter. The tumor was dissected free from adjacent structures using Liga-Sure and blunt maneuvers. A complete laparoscopic excision was performed. Histopathological examination revealed a benign schwannoma. The patient had an uneventful post-operative course, and was discharged on the fourth post-operative day. Laparoscopic treatment is useful and feasible for retroperitoneal pelvic schwannoma, with minimal invasiveness and an early post-operative recovery. Thus, this procedure may be the first-choice surgical procedure for retroperitoneal pelvic schwannomas.
INTRODUCTION
Schwannomas are rare peripheral nerve tumors arising from Schwann cells of the nerve sheath, and they are usually located in the head and neck. Their pelvic occurrence is much rarer, accounting for 1–3% of all schwannomas [1]. Pelvic schwannomas arise mostly from the sacral nerve or the hypogastric plexus [2]. Computed tomography (CT) and other imaging modalities may help obtain information about tumor size, location and relationships with neighboring tissues, but they do not give a definitive diagnosis. A successful laparoscopic resection of a presacral schwannoma near the right internal iliac vessels and ureter is reported.
CASE REPORT
A 54-year-old woman was referred to our hospital with a mass in the pelvic cavity detected on chest-abdominal, CT done for investigation of breast cancer. She had no particular past and family history, and the physical examination was unremarkable. Ultrasonography of the pelvis revealed a 5 × 4.3 cm, solid mass separated from her right adnexa (Fig. 1). Contrast enhanced-CT showed a 5 × 4 cm, solid, well-defined, heterogeneous mass in the right side of the pelvic cavity (Fig. 2). MRI showed that the tumor demonstrated homogeneous hypointensity on T1-weighted images and heterogeneous slight hyperintensity on T2-weighted images (Fig. 3a and b). Sagittal sections of MRI demonstrated that the mass was intricately related to the anterior presacral fascia (Fig. 4). The preoperative diagnosis was a mesenteric gastrointestinal stromal tumor.
Figure 1:
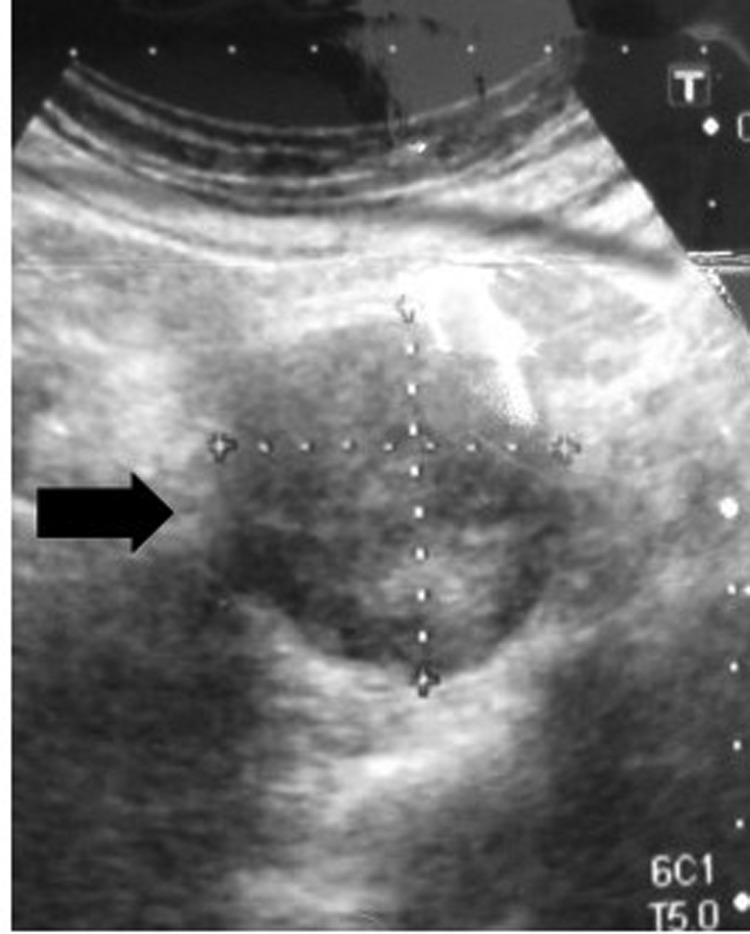
Ultrasonography of the pelvis shows a 5 × 4.3 cm solid and an iso-echoic mass.
Figure 2:
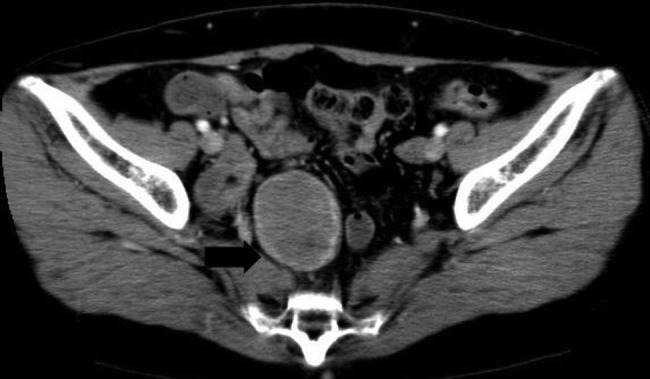
Contrast enhanced-CT shows a 5 × 4 cm solid, well-defined, heterogeneous mass in the right side of the pelvic cavity.
Figure 3:
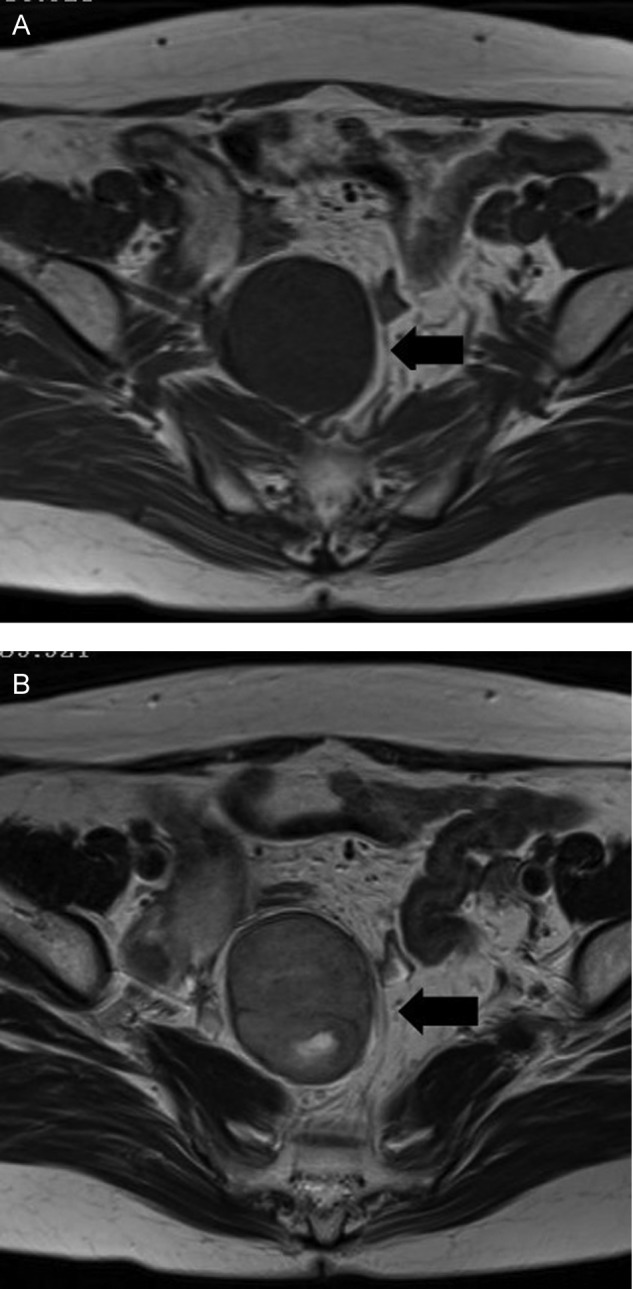
MRI shows that the tumor is a homogeneous hypointensity on T1-weighted images (A) and a heterogeneous slight hyperintensity on T2-weighted images (B) in a right side of the pelvic cavity.
Figure 4:

Sagittal MRI sections show the mass to be intricately related to the anterior presacral fascia.
Under general anesthesia, the patient was placed in the supine position, and a 4-port technique was used. A 12-mm port was inserted through an umbilical incision for the placement of a flexible laparoscope. Three other ports (one 12-mm and two 5-mm ports for retraction or the working port) were placed. The left-sided port was mainly used for retraction. An initial incision was made in the retroperitoneum, and mainly sharp dissection by Liga-Sure was used to isolate the mass from the surrounding tissues. With careful dissection using sharp and blunt maneuvers, the mass was dissected from the neighboring vessels, such as the right internal iliac vessels and ureter (Fig. 5). Although the ureter was easily identified and dissected free, the mass strongly adhered to the right internal iliac vessels, making its dissection difficult. Sponge dissection was very useful in that situation. Once free from the surrounding tissues, the mass was placed into a plastic bag to avoid spillage into the abdomen. It was then received through the enlarged incision of the umbilicus. A suction drainage tube was placed into the pouch of Douglas through a 12-mm port in the right side of the abdomen.
Figure 5:
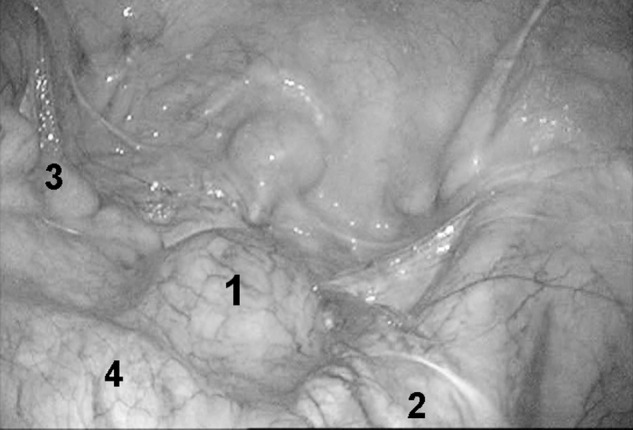
Laparoscopic findings of schwannoma in the pelvis. 1, schwannoma 2, right ureter 3, rectum 4, right iliac vessel.
The intra-operative blood loss was minimal, and the operation time was 150 min. The specimen was an elastic hard, 5 × 4 cm mass with an integral envelope. On sectioning, it was yellow and white in color, predominantly solid with cystic change (Fig. 6). Pathologic examination showed whorls and interlacing fascicles of schwannoma spindle cells, along with alternating Antoni-A and -B patterns with areas of hyalinization and fibrinoid degeneration (Fig. 7a and b). The cells stained positive for S-100 protein and negative for desmin and muscle-specific actin, consistent with a benign schwannoma. The patient had an uneventful post-operative course and was discharged on the fourth post-operative day. The patient has had no evidence of recurrence so far, 20 months after surgery.
Figure 6:
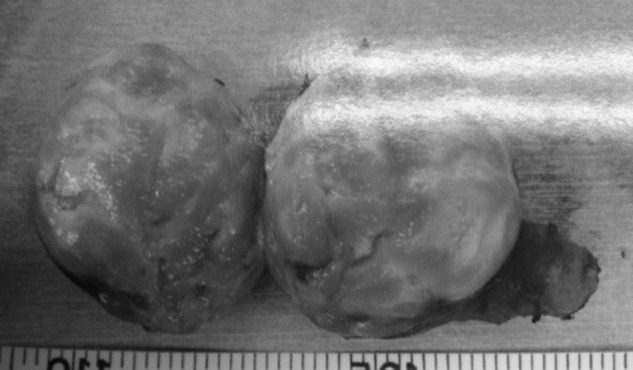
The specimen is an elastic hard, 5 × 4 cm mass with an integral envelope. On sectioning, it is yellow and white in color, predominantly solid with cystic change.
Figure 7:
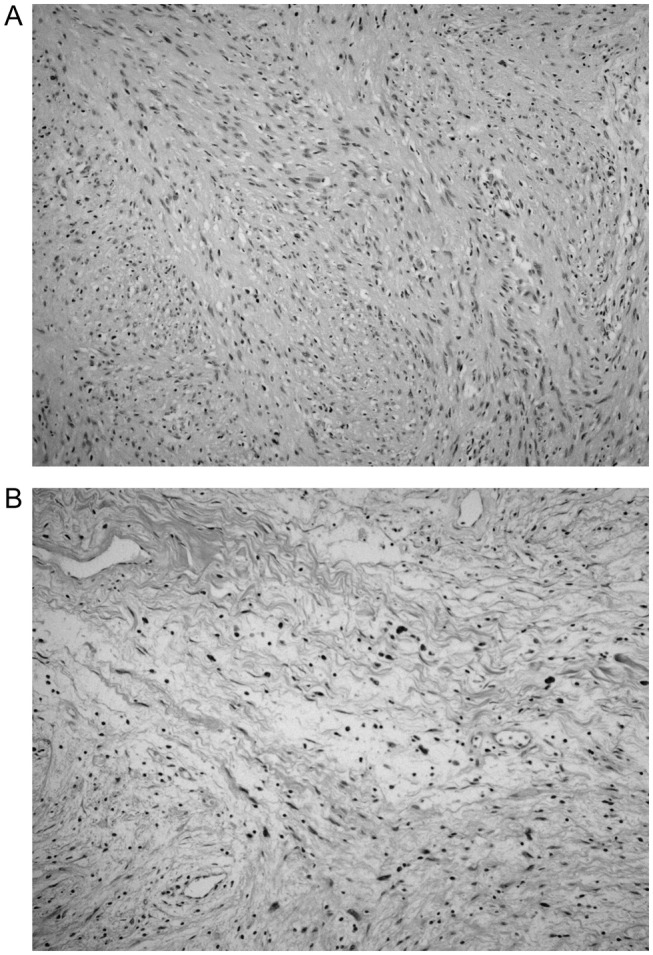
Histologic findings of schwannoma in the pelvis (hematoxylin and eosin, ×200). (A) The Antoni A pattern is composed of spindle cells arranged in intersection fascicles. Nuclear palisades are seen and mitoses are rarely observed. (B) The Antoni B pattern is composed of loose hypocellular tissue.
DISCUSSION
Pelvic schwannomas mostly arise from a sacral nerve or the hypogastric plexus [2]. In the present case, it may have originated from the hypogastric plexus. The proportion of retroperitoneal schwannomas has been reported to be 0.7–2.6% of all schwannomas [3]. Moreover, pelvic schwannnomas are very rare and account for <1% of all benign schwannomas [4]. In the literature, ∼60 cases of benign retroperitoneal schwannomas, of which <20 were located in the pelvis, have been reported [5].
There is no gold standard, non-invasive diagnostic method for schwannomas. Ultrasound (US), CT and MRI are non-specific in most cases. Li et al. [6] reported that only 15.9% were identified preoperatively by these imaging modalities in a review of 82 retroperitoneal schwannomas. Traditionally, pelvic tumors have been classified into congenital, inflammatory, neurogenic, osseous, specific soft-tissue masses and arteriovenous malformations [7]. In the present case, the preoperative diagnosis was a gastrointestinal stromal tumor of the mesentery.
Operable tumors do not generally require preoperative biopsy. CT-guided, fine needle aspiration (FNA) or endoscopic ultrasound (EUS)-FNA is unreliable in large schwannomas due to cellular pleomorphism in areas of degeneration. Since seeding of malignant cells and infection of cystic tumor are risks, complete operative removal remains the best biopsy. A few reports recently have described the usefulness of EUS-FNA for the diagnosis of small retroperitoneal schwannoma, especially for small tumors difficult to detect on CT or US [8]. Since most schwannomas are benign and seldom become malignant, patients with asymptomatic retroperitoneal schwannomas with no possibility of malignancy diagnosed by EUS-FNA may avoid unnecessary surgery. However, malignancy cannot be excluded accurately preoperatively or even intra-operatively with frozen section analysis. At present, surgical resection is the only accurate approach for pathologic evaluation to enable diagnosis of a pelvic schwannoma.
It has been argued that the local recurrence rate ranges from 16 to 54% after conservative intralesional enucleation [9]. On the other hand, because this is a benign mass, an enucleation or a partial resection of the mass is sufficient and have reported no increase in the size of the mass over a 6- and 14-year period [10]. However, because the possibility of malignancy is not completely excluded with the exception of viewing enough tissue, the best treatment of schwannomas is complete surgical resection.
During the present operation, the mass was easy to dissect off from adjacent organs such as the internal iliac vessels and ureter. The proximity of the mass to the ureter may require its preoperative catheterization. A sponge dissection was useful for dividing the mass from the internal iliac vein or the anterior sacral fascia as in the present case. Laparoscopy is a safe and efficient tool for approaching benign pelvic schwannomas and might offer the advantage of better visualization of structures with the magnification of the laparoscopic view, especially in narrow anatomic spaces.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Borghese M, Corigliano N, Gabriele R, Antoniozzi A, Izzo L, Barbaro M, et al. Benign schwannoma of the pelvic retroperitoneum. Report of a case and review of the literature. G Chir. 2000;21:232–8. [PubMed] [Google Scholar]
- 2.Aubert J, Debiais F, Irani J, Dore B, Levillain P. Schwannome et appareil urinaire. A propos D`une tumeur du nerf obturateur [in French] Prog Urol. 1999;9:528–33. [PubMed] [Google Scholar]
- 3.Ueda M, Okamoto Y, Ueki M. A pelvic retroperitoneal schwannoma arising in the right paracolpium. Gynecol Oncol. 1996;60:480–3. doi: 10.1006/gyno.1996.0077. [DOI] [PubMed] [Google Scholar]
- 4.Tong RSK, Collier N, Kaya AH. Chronic sciatica secondary to retroperitoneal pelvic schwannoma. J Clin Neurosci. 2003;10:108–11. doi: 10.1016/s0967-5868(02)00107-8. [DOI] [PubMed] [Google Scholar]
- 5.Deboudt C, Labat J, Riant T, Bouchot O, Robert R, Rigaud J. Pelvic schwannoma: robotic laparoscopic resection. Neurosurgry. 2013;72:2–5. doi: 10.1227/NEU.0b013e31826e2d00. [DOI] [PubMed] [Google Scholar]
- 6.Li Q, Gao C, Juzi JT, Hao X. Analysis of 82 cases of retroperitoneal schwannoma. ANZ J Surg. 2007;77:237–40. doi: 10.1111/j.1445-2197.2007.04025.x. [DOI] [PubMed] [Google Scholar]
- 7.Neifer R, Nguyen GK. Aspiration cytology of solitary schwannoma. Acta Cytol. 1985;29:12–14. [PubMed] [Google Scholar]
- 8.Hijioka S, Sawaki A, Mizuno N, Hara K, Mekky MA, et al. Endoscopic ultrasound-guided fine-needle aspiration for the diagnosis of retroperitoneal schwannoma. Endoscopy. 2010;42(Suppl. 2):E 296. doi: 10.1055/s-0030-1255786. [DOI] [PubMed] [Google Scholar]
- 9.Andonian S, Karakiewicz PI, Herr HW. Presacral cystic schwannoma in a man. Urology. 2003;62:8–10. doi: 10.1016/s0090-4295(03)00481-3. [DOI] [PubMed] [Google Scholar]
- 10.Regan JF, Juler GL, Schmutzer KJ. Retroperitoneal neurilemoma. Am J Surg. 1997;134:140–5. doi: 10.1016/0002-9610(77)90297-5. [DOI] [PubMed] [Google Scholar]


