Abstract
Endobronchial tumours requiring sleeve resection have been usually considered a contraindication for video-assisted thoracoscopic surgery (VATS). However, with new technical advances and the experience gained in VATS, sleeve lobectomy has been performed by thoracoscopy in experienced VATS centres. Right-sided sleeve anastomoses are easier to perform by VATS than left-sided ones because of the presence of the pulmonary artery and aortic arch on the left side. Most surgeons use a 3 to 4 incision VATS technique for sleeve anastomosis but the surgery can be performed by using only one incision. This is the first report of a left-sided sleeve lobectomy by uniportal approach.
Keywords: Sleeve lobectomy, Thoracoscopy/video-assisted thoracic surgery, Minimally invasive surgery, Lobectomy, Lung cancer
INTRODUCTION
Left lower lobectomy with sleeve bronchial resection is one of the most complex resections that can be performed by video-assisted thoracic surgery (VATS). There are few cases reported in the literature describing this thoracoscopic anastomosis in the left side. Here, we present the technique for left lower lobectomy with a sleeve resection by uniportal (single incision) VATS approach.
SURGICAL TECHNIQUE
A 71-year old female was admitted for surgery. Computed tomography (CT) scan revealed a carcinoid tumour in the left lower lobe (LLL) associated with bronchial occlusion of the main bronchus. Bronchoscopy confirmed the carcinoid tumour nearly occluding the left main bronchus. Following this VATS, resection was performed. The patient was placed in a right lateral decubitus position. A VATS approach using a single 5-cm incision was made in the fifth intercostal space with no rib spreading (no soft tissue retractor and no direct visualization). The camera was placed in the posterior portion of the incision with instruments inserted parallel to and below the camera. A left lower lobectomy was performed leaving the bronchus as the last step of the procedure. The left upper lobe bronchus was dissected and exposed. The mainstem and the upper lobe bronchi were cut circumferentially with a knife on a long handle and scissors, and the lobe was removed in a protective bag (Fig. 1, Supplementary Video 1).
Supplementary Video 1:
Sleeve resection.
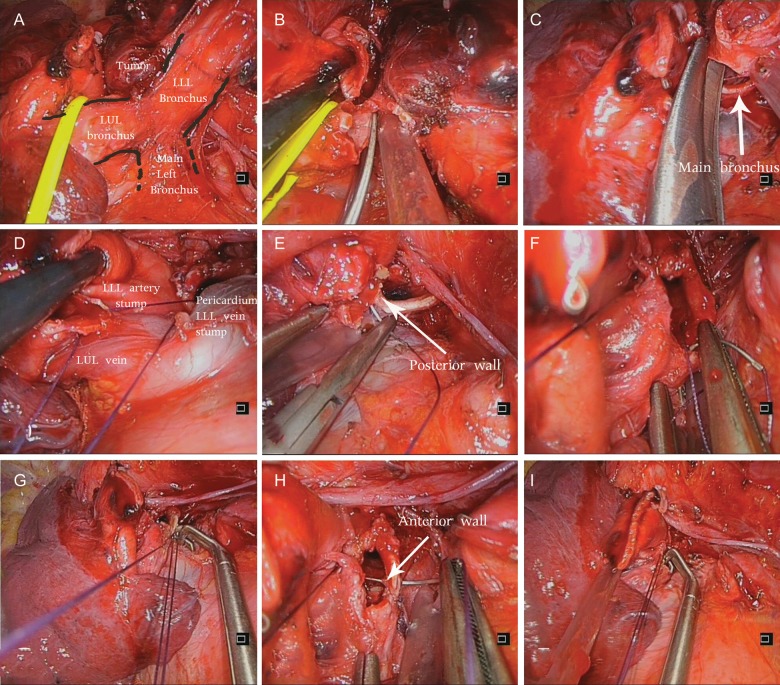
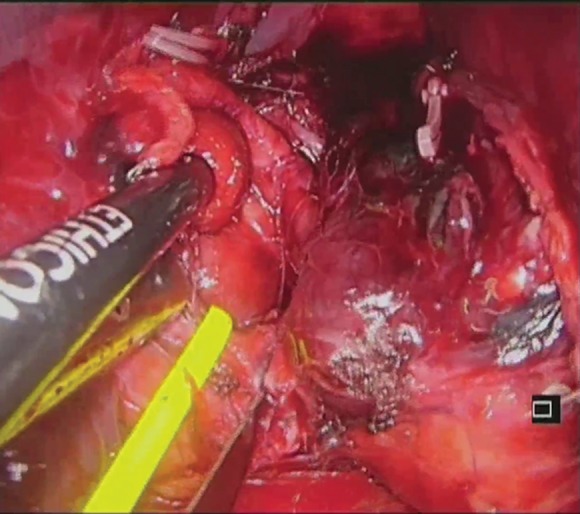
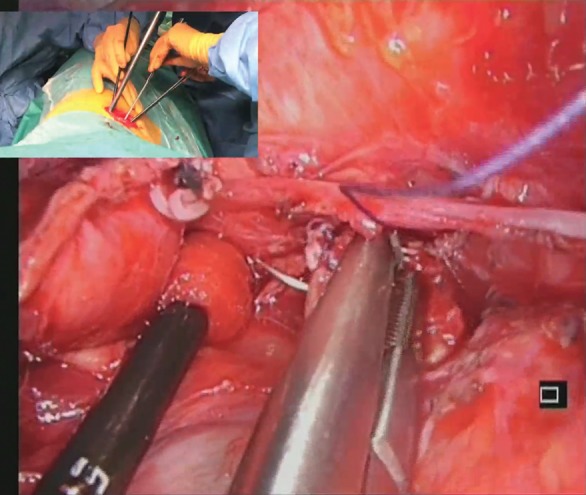
After careful retraction of the artery stump and pericardium (with a endoscopic peanut), we initiated the end-to-end anastomosis with a posterior 3–0 absorbable suture in the cartilaginous-membranous junction (Fig. 2A) to help appose the upper lobe bronchi and mainstem bronchi, and then proceeded with interrupted sutures in the posterior wall of airway (the most difficult part of anastomosis). Once the posterior wall of the anastomosis was completed (from cranial to caudal), we placed a 3–0 interrupted absorbable suture at the angle of the anterior portion of the bronchial cartilage. Both sutures were tied with the help of a thoracoscopic knot-pusher (Scanlan International, Inc., St. Paul, MN, USA). We continued with a simple continuous absorbable suture for the membranous portion of the bronchial membrane (running from caudal to cranial). The cartilaginous portion of the anterior bronchial wall was sutured with 3–0 interrupted sutures and a knot was formed between the last simple interrupted suture and the membranous continuous suture (Fig. 1, Supplementary Video 2).
Figure 2:
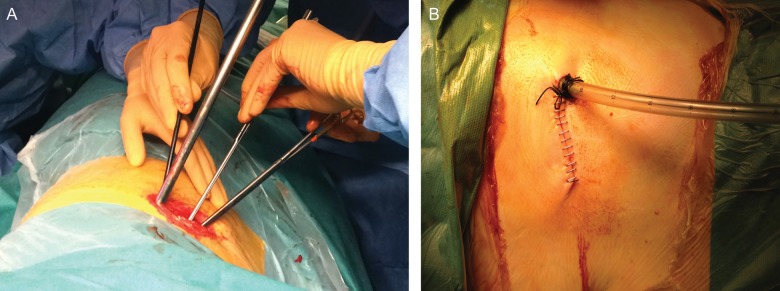
(A) Surgical image of uniportal instrumentation during sleeve anastomosis. (B) Postoperative result with the chest tube placed in the posterior part of the incision.
Figure 1:
Sequence of sleeve resection and anastomosis. (A) Exposure of left upper, lower and main bronchi. (B) Transection of left upper lobe bronchus. (C) Transection of main bronchus. (D) Retraction of artery and apposition of main and upper lobe bronchi with a 3–0 interrupted suture. (E) Posterior wall of anastomosis. (F) Interrupted 3–0 absorbable suture at the angle of anterior portion of the bronchial cartilage. (G) Continuous and interrupted sutures tied with the help of a thoracoscopic knot-pusher. (H) Continuous suture for the membranous portion of the bronchial membrane. (I) Use of endoscopic knot-pusher to tie the continuous suture with the last interrupted cranial suture to complete the anastomosis.
Supplementary Video 2:
Sleeve anastomosis.
The anastomosis was not buttressed. The remaining lung was re-expanded and the anastomosis was checked for an air leak under water. A single chest tube was placed through the incision (Fig. 2B). The total surgical time was 250 min. The patient was discharged home on postoperative day 6. Pathological examination revealed a 2.5 cm carcinoid tumour with no lymph node involvement (T1bN0M0). The follow-up bronchoscopy and CT scan confirmed no stenosis and no signs of recurrence.
DISCUSSION
Bronchoplastic resections with preservation of parenchyma should be attempted whenever possible when treating centrally located endobronchial carcinoid tumours rather than performing a pneumonectomy. With skills and experience obtained from performing complex VATS procedures, these operations can be performed by thoracoscopy [1]. Most surgeons use a 3 to 4 incision VATS technique, but the surgery can be accomplished by only one port [2].
There have been a few series of cases published in the literature of VATS total sleeve resection [3–5]. Most cases reported are right upper lobe anastomoses which are easier to perform due to the lateral distribution of the anastomosis. The left lower sleeve lobectomy is technically somewhat more difficult because of the presence of the pulmonary artery (which should be retracted), the atrium and upper lobe vein [4]. The orientation to perform the anastomosis is also difficult because the upper lobe bronchus needs to be reimplanted on the main bronchus from an anterior view, and the main bronchus is usually deeply located.
The placement of the incision is crucial for a thoracoscopic sleeve procedure [6], especially when performing on the left side. We made the incision through the fifth intercostal space in a more lateral position than for conventional VATS (posterior axillary line). By using this location, the anastomosis can be completed in a manner similar to the traditional approach in anterior thoracotomy. The camera through the utility incision provides a direct stereoscopic view of the operative field and this incision provides a broader space in which to handle the instruments with bimanual instrumentation.
The success in performing uniportal complex VATS lobectomies is a result of skills and experience accumulated over time from performing uniportal VATS surgery [7]. The advantage of using the camera in coordination with the instruments through the same incision is that we can obtain an angle of view similar to that obtained in open surgery directed to the target tissue and we are bringing in the instruments to accomplish the anastomosis from a straight perspective. Instruments inserted parallel and underneath the videothoracoscope also mimic inside the chest manoeuvers performed during open sleeve surgery. Furthermore, we believe that by avoiding the use of the trocar, the possibility of an intercostal nerve injury could be minimized in comparison with conventional VATS.
The management of the instruments and sutures is more important in VATS than in an open thoracotomy. It is very important to keep tension and tie the interrupted sutures once they are placed. For left lower sleeve anastomosis, the posterior bronchial wall is deep and difficult to access, making it the most challenging part of the surgery. We used both continuous and interrupted suture techniques for the membranous and cartilaginous portions of the bronchus, respectively.
Supplementary material
Supplementary material is available at ICVTS online.
Conflict of interest: none declared.
REFERENCES
- 1.Santambrogio L, Cioffi U, De Simone M, Rosso L, Ferrero S, Giunta A. Video-assisted sleeve lobectomy for mucoepidermoid carcinoma of the left lower lobar bronchus: a case report. Chest. 2002;121:635–6. doi: 10.1378/chest.121.2.635. [DOI] [PubMed] [Google Scholar]
- 2.Gonzalez-Rivas D, Fernandez R, Fieira E, Rellan L. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg. 2013;145:1676–7. doi: 10.1016/j.jtcvs.2013.02.052. [DOI] [PubMed] [Google Scholar]
- 3.Li Y, Wang J. Video-assisted thoracoscopic surgery sleeve lobectomy with bronchoplasty: an improved operative technique. Eur J Cardiothorac Surg. 2013:1–5. doi: 10.1093/ejcts/ezt199. [DOI] [PubMed] [Google Scholar]
- 4.Mahtabifard A, Fuller CB, McKenna RJ., Jr Video-assisted thoracic surgery sleeve lobectomy: a case series. Ann Thorac Surg. 2008;85:729–32. doi: 10.1016/j.athoracsur.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 5.Agasthian T. Initial experience with video-assisted thoracoscopic bronchoplasty. Eur J Cardiothorac Surg. 2013:1–8. doi: 10.1093/ejcts/ezt166. [DOI] [PubMed] [Google Scholar]
- 6.Nakanishi K. Video-assisted thoracic surgery lobectomy with bronchoplasty for lung cancer: initial experience and techniques. Ann Thorac Surg. 2007;84:191–5. doi: 10.1016/j.athoracsur.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez-Rivas D, Paradela M, Fernandez R, Delgado M, Fieira E, Mendez L, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg. 2013;95:426–32. doi: 10.1016/j.athoracsur.2012.10.070. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.