Abstract
A 74-year old female was transferred to our institution because of blunt chest trauma. Chest X-ray and computed tomography (CT) revealed right haemothorax and little pericardial effusion. She was taken to the operating theatre for emergent operation because of hypotension and massive bleeding from the right-sided chest tube. Cardiopulmonary resuscitation was started during surgical exploration. There were three 1-cm lacerations actively bleeding from the right atrium and inferior vena cava junction, which were repaired successfully. Furthermore, we identified a 10 cm laceration in the right-side pleuropericardium and a communication existing between the pericardial space and the right pleural space.
Keywords: Blunt trauma, Cardiac rupture, Pericardial rupture, Haemothorax
INTRODUCTION
Massive traumatic haemothorax is a life-threatening condition that requires the surgeon's prompt treatment. Blunt traumatic cardiac rupture is a very rare occurrence accounting for 0.5% of blunt trauma cases and with a very high mortality rate [1]. Coexisting pericardial rupture in patients with cardiac rupture obscures the diagnosis and contributes to mortality [2]. This case report describes the successful treatment of a rare case of massive right-sided haemothorax caused by right atrial and pleuropericardial rupture.
CASE REPORT
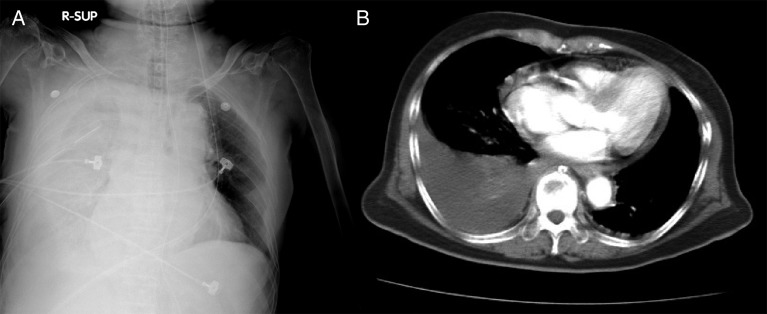
A 74-year old, restrained female passenger was involved in a high-speed, single motor vehicle crash. Upon arrival, her pulse was 155 and her blood pressure (BP) was 72/43 mmHg. The vital signs improved to BP 108/41, heart rate 108 after fluid challenge. Chest radiograph revealed left-sided serial rib fractures (from sixth to ninth) and a significant right-sided haemothorax (Fig. 1A). A right-sided chest tube was inserted and 1200cc blood was drained out. Laboratory analysis showed elevation of cardiac enzyme and a haemoglobin value of 11.4 g/dl. Focused assessment sonography (FAST) disclosed minor pericardial effusion without right ventricular diastolic collapse. The trauma-CT revealed right-sided massive haemothorax and minimal pericardial effusion without any other injury (Fig. 1B). The patient was taken emergently to the operation theatre for surgical exploration.
Figure 1:
(A) Preoperative chest X-ray: right-sided massive haemothorax, left-sided serial rib fractures (from sixth to ninth). (B) Preoperative computed tomographic scan showing the right-sided haemothorax and pericardial effusion.
Subxiphoid pericardial window was performed to be a confirmatory test before thoracotomy to exclude major great vessels injury. However, the Subxiphoid approach shifted to median sternotomy immediately because of catastrophic haemorrhage from pericardial window. Bradycardia followed by asystole occurred during surgical exploration of cardiac injury and direct cardiac massage was performed until spontaneous heart beat recovered. There were three 1-cm lacerations actively bleeding from the right atrium and inferior vena cava junction. Those lacerations were repaired successfully with 4–0 polypropylene monofilament sutures (Fig. 2A). Further examination disclosed a 10-cm laceration in the right-side pleuropericardium and a communication existing between the pericardial cavity and the right pleural space (Fig. 2B). No other injuries of the right thoracic cavity were noted after all blood clot was evacuated. The total cardiopulmonary cerebral resuscitation (CPCR) time was 15 min. This patient's bleeding subsided and vital sign was stabilized after the operation and blood transfusions of packed red blood cell 6 units, fresh frozen plasma 6 units and Platelet 12 units. However, she suffered from renal failure, hepatic failure and respiratory failure because of perioperative profound shock. This patient's multiorgan dysfunction gradually receded and the patient was discharged from the hospital on postoperative day 69.
Figure 2:
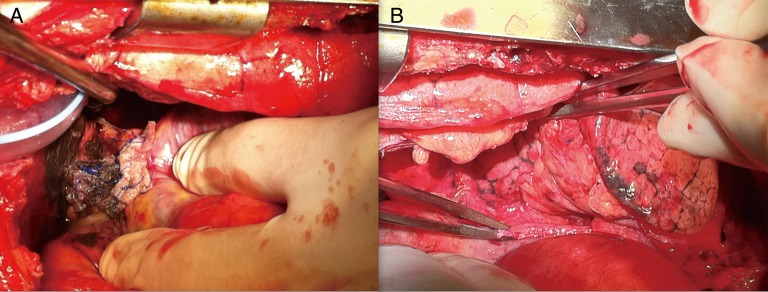
(A) Intraoperative photography: three 1-cm lacerations of right atrium and inferior vena cava junction were repaired with 4–0 polypropylene monofilament sutures. (B) Intraoperative photography: a 10-cm laceration in the right-side pleuropericardium and a communication existing between the pericardial and the right pleural space.
DISCUSSION
A number of causes may be responsible for blunt traumatic haemothorax including pulmonary parenchymal laceration, intercostal vessel injuries, rupture of pleural adhesion and mediastinal injury with or without great vessels injury. And rarely, cardiac injury combined with pericardial laceration.
Cardiovascular injuries are the second most common cause of death after blunt trauma following after central nervous system injuries. Blunt traumatic pericardial rupture is a rare injury and the diagnosis is challenging and is commonly made at the time of surgery [3]. Combined blunt pericardial and cardiac injury associated with high mortality rate because of the decompression into the pleural space makes the diagnosis more difficult [2, 4]. Fulda et al. [4] also reported that the incidence of combined pericardial and cardiac chamber rupture was 8% for those patients suffering blunt chest trauma and that the rate of survival was <15% for blunt heart rupture.
Prompt and correct diagnosis is the key to successful outcomes for blunt cardiac rupture but it remains a challenge. Traumatic pericardial effusion diagnosed by FAST, CT or Echo, even in small amounts, mandates surgical pericardial window and subsequent sternotomy in the presence of gross blood. Not only can surgical pericardial window drain out pericardial effusion to release cardiac tamponade in minutes, but can also be a confirmatory test before sternotomy or thoracotomy for those with FASTs that are inconclusive or negative with a large haemothorax [5]. Furthermore, we preferred the Subxiphoid approach because it is easier to shift to full sternotomy. It offers the best cardiac exposure, facilitates inspection and allows direct cardiac massage and repair as in our presenting case.
In conclusion, our case highlights the need for a high degree of suspicion regarding the possibility of cardiac rupture after blunt chest trauma and to keep in mind the possibility of combined pericardial laceration presenting as haemothorax without cardiac tamponade signs. Establishing and strictly following a proposed algorithm for blunt chest trauma has been key to increasing the diagnosis rate and may save some critical patients.
To the best of our knowledge, this is the only well-documented patient who survived after CPCR and repair of combined blunt cardiac and pericardial rupture with initial presentation of right-sided haemothorax. This case report clearly displayed the intraoperative picture. We hope that our current successful experience can help with future cases.
Conflict of interest: none declared.
REFERENCES
- 1.Martin TD, Flynn TC, Rowlands BJ. Blunt cardiac rupture. J Trauma. 1984;24:287–90. doi: 10.1097/00005373-198404000-00001. [DOI] [PubMed] [Google Scholar]
- 2.May AK, Patterson MA, Rue LW, III, Schiller HJ, Rotondo MF, Schwab CW. Combined blunt cardiac and pericardial rupture: review of the literature and report of a new diagnostic algorithm. Am Surg. 1999;65:568–74. [PubMed] [Google Scholar]
- 3.Farhataziz N, Landay MJ. Pericardial rupture after blunt chest trauma. J Thorac Imaging. 2005;20:50–2. doi: 10.1097/01.rti.0000139391.26138.dd. [DOI] [PubMed] [Google Scholar]
- 4.Fulda G, Rodriguez A, Turney SZ, Cowley RA. Blunt traumatic pericardial rupture. A ten-year experience 1979 to 19889. J Cardiovasc Surg. 1990;31:525–30. [PubMed] [Google Scholar]
- 5.Huang YK, Lu MS, Liu KS, Liu EH, Chu JJ, Tsai FC, et al. Traumatic pericardial effusion: impact of diagnostic and surgical approaches. Resuscitation. 2010;81:1682–6. doi: 10.1016/j.resuscitation.2010.06.026. [DOI] [PubMed] [Google Scholar]