Abstract
The impact of heavy rainfall events on waterborne diarrheal diseases is uncertain. We conducted weekly, active surveillance for diarrhea in 19 villages in Ecuador from February 2004 to April 2007 in order to evaluate whether biophysical and social factors modify vulnerability to heavy rainfall events. A heavy rainfall event was defined as 24-hour rainfall exceeding the 90th percentile value (56 mm) in a given 7-day period within the study period. Mixed-effects Poisson regression was used to test the hypothesis that rainfall in the prior 8 weeks, water and sanitation conditions, and social cohesion modified the relationship between heavy rainfall events and diarrhea incidence. Heavy rainfall events were associated with increased diarrhea incidence following dry periods (incidence rate ratio = 1.39, 95% confidence interval: 1.03, 1.87) and decreased diarrhea incidence following wet periods (incidence rate ratio = 0.74, 95% confidence interval: 0.59, 0.92). Drinking water treatment reduced the deleterious impacts of heavy rainfall events following dry periods. Sanitation, hygiene, and social cohesion did not modify the relationship between heavy rainfall events and diarrhea. Heavy rainfall events appear to affect diarrhea incidence through contamination of drinking water, and they present the greatest health risks following periods of low rainfall. Interventions designed to increase drinking water treatment may reduce climate vulnerability.
Keywords: climate, diarrhea, Ecuador, heavy rainfall events, rain, social vulnerability, water treatment
Global climate change may increase the burden of diarrheal diseases, which are already a leading cause of childhood morbidity and mortality (1, 2). Diarrhea causes approximately 700,000 deaths annually in children under age 5 years (3), so even small proportional increases in risk can substantially increase disease burden. However, uncertainties about the impact of climate on the transmission of diarrheal pathogens have been a key limitation in quantifying the associations of climate change with health (1, 4).
Both temperature and rainfall have the potential to affect the transmission of waterborne diarrheal pathogens. Higher temperatures may increase pathogen replication and survival rates; rainfall pulses can flush fecal material into waterways; and droughts may concentrate microorganisms in water sources.
With few exceptions (e.g., see Milojevic et al. (5)), high temperatures and rainfall have been found to increase the risk of diarrhea, but considerable uncertainty remains. Higher temperatures have been consistently associated with higher rates of diarrhea (6–10), but risk estimates vary widely (4). While increased rainfall may increase diarrhea risk, evidence to date suggests that so too may low rainfall and drought. Increased gastrointestinal disease has been associated with any rainfall in the United States (11), with both low and high levels of rainfall in the Pacific Islands (10) and Bangladesh (7), and with low rainfall in a global cross-sectional study (12). Both Curriero et al. (13) and Thomas et al. (14) found positive associations between heavy rainfall events and waterborne disease outbreaks in North America. Flooding has been associated with increased diarrhea in Bangladesh (15, 16), Mozambique (17), and the United States (18), but Milojevic et al. (5) found no evidence of flooding-associated diarrhea risk in Bangladesh.
The Intergovernmental Panel on Climate Change defines vulnerability as the degree to which a system is susceptible to, and unable to cope with, the adverse effects of climate change (2). Social and environmental factors such as water and sanitation infrastructure, hygiene behaviors, and community cohesion directly affect the transmission of diarrheal pathogens (19, 20), and these same factors may determine a community's vulnerability to weather events, including temperature and rainfall extremes. For example, sanitation infrastructure may prevent the spread of pathogens during heavy rainfall events. Community social cohesion may affect the capacity of a community to respond to a flooding event. Similarly, prior weather patterns may modify the health impacts of weather events. For example, extended dry periods may allow for accumulation of pathogens through fecal deposition, leading to a greater input of pathogens into waterways when heavy rainfall occurs.
To account for the complex interplay between climate, social and environmental conditions, and health, differential sensitivity of human communities to the stresses imposed by climate variability must be taken into account (1, 21). While many frameworks and conceptual models exist (22, 23), there are few examples of successful integration of biophysical and social data into quantitative analyses of the impacts of climate change. Biophysical and social factors have been combined in quantitative analysis of heat vulnerability (24) and diarrhea (15), but these examples are rare. Such integrated approaches can improve our understanding of climate vulnerability and can shed light on the mechanisms by which weather events affect health.
We examined the extent to which social and biophysical factors modify climate-disease relationships, focusing on rainfall. Using a 3-year active surveillance data set of weekly diarrhea incidence from over 5,000 persons in 19 communities in northern coastal Ecuador, we tested the hypothesis that community drinking water treatment, improved sanitation, hygiene practices, social cohesion, and long-term rainfall patterns modify the relationship between heavy rainfall events and diarrhea incidence.
METHODS
Study population
The study was conducted in Esmeraldas Province, Ecuador, where approximately 125 villages lie along the Cayapas, Santiago, and Onzole rivers. These rivers flow toward Borbón, a town of approximately 5,000 people (Figure 1). Residents of the study villages generally had limited formal schooling and economic resources, as described previously (20, 25).
Figure 1.
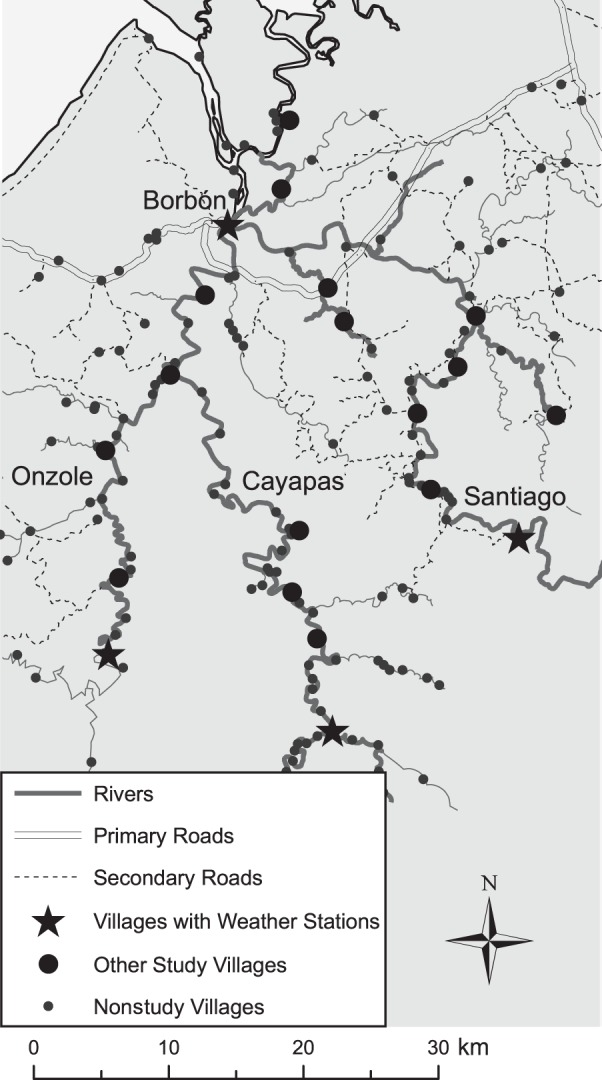
Map of the region in northern coastal Ecuador included in a study of heavy rainfall events and diarrhea incidence, showing the location of study villages and rainfall monitors, 2004–2007.
Diarrhea surveillance
Originally, 21 villages representative of the study region were selected (for details, see Eisenberg et al. (26)), and all households were recruited for enrollment. Consenting households (95% of those recruited) were visited weekly by local community health workers who were supervised by a nurse employed by the study investigators. This analysis included 19 villages because of the poor quality of diarrhea surveillance in 2 villages, which were excluded after a systematic evaluation of the consistency and quality of data for each village. Self-identified heads of households were asked about illnesses and symptoms in household members during the previous week. The World Health Organization-accepted definition of a diarrhea episode was used: 3 or more loose stools in a 24-hour period during the previous week. Diarrhea incidence was calculated for each village each week as the number of incident cases—diarrhea in persons who had not experienced diarrhea during the preceding week—divided by the population at risk. Consent was obtained at the village and household levels. Institutional review boards at the University of Michigan, the University of California, Berkeley, Trinity College, and Universidad San Francisco de Quito approved all protocols.
Rainfall
Precipitation was measured in 4 locations in the study region using HOBO data-logging rain gauges (Onset Corporation, Borne, Massachusetts). Because of equipment malfunction, gaps existed in the rainfall data for the period of study (see Web Figure 1, available at http://aje.oxfordjournals.org/). We restricted our analysis to the continuous period during which rainfall was measured at 1 or more locations each day: February 18, 2004, through April 18, 2007. During this period, rainfall measurements were available from at least 2 sites for 49% of days and from 3 sites for 12% of days. We used a 2-step imputation procedure to estimate rainfall in villages and weeks for which observed data were not available (for details, see Web Appendix 1 and Web Tables 1 and 2). Measurements were summarized by week to correspond with the resolution of diarrhea incidence measures. We first used linear interpolation to estimate average and maximum 24-hour rainfall for each weather-monitoring location in weeks when rainfall measures were missing. We then used a nonparametric kriging approach to impute rainfall values for all study villages, based on data from the 4 weather-monitoring locations. Kriging has been found to provide more accurate climate predictions than other methods, such as inverse-distance weighting, linear regression, and nearest-neighbor predictions (27–29). Additionally, this method is appropriate for sparsely observed data.
We defined a heavy rainfall event as maximum 24-hour rainfall above the 90th percentile value (56 mm) in a given 7-day period across all villages within the study period. We decided a priori to evaluate the impact of 1- and 2-week-lagged heavy rainfall events on diarrhea incidence because a 1-week lag is consistent with the incubation periods of common diarrheal pathogens and a 2-week lag would account for secondary transmission of pathogens within the community.
Because we hypothesized that the impact of heavy rainfall events on diarrhea incidence may depend on long-term prior rainfall patterns, we included a term for total rainfall during the 8 weeks preceding the measurement of heavy rainfall events. Use of this definition helped us avoid temporal overlap with the heavy rainfall variable. To avoid assumptions of linearity, we categorized 8-week rainfall into tertiles.
Social vulnerability
We also evaluated whether social variables known to directly affect diarrhea risk, including sanitation, drinking water treatment, hygiene practices, and social cohesion, modified the relationship between heavy rainfall events and diarrhea incidence. These variables were defined at the village level as follows:
Sanitation: Percentage of households that reported using a public or private septic pit or a latrine (30).
Water treatment: Percentage of households that reported using filtration, boiling, or chlorination to treat their drinking water (30).
Hygiene: Average community score in a 23-item household hygiene evaluation conducted by study staff. The hygiene assessment included latrine cleanliness, the presence of soap, and water storage conditions.
Social cohesion: Average number of contacts reported by each village resident in a sociometric survey that asked, “In general, with whom do you spend time in your community, outside of household members?” (20, 26).
Sanitation was assessed during the annual village census. Social cohesion was measured as part of a complete census of the population conducted in 2004 and 2007. Water treatment and hygiene were assessed during a concurrent case-control study of diarrhea in the same villages between August 2003 and October 2008 (26). Village measures for these 2 variables were estimated by weighting each observed household using the inverse probability of being sampled. Measures were matched to surveillance data using data from the most recent survey.
Statistical analysis
In order to understand whether biophysical and social factors modify the relationship between heavy rainfall events and diarrhea incidence, we evaluated interactions between heavy rainfall events and biophysical and social variables, starting with the simplest model. For each analysis, we employed random-effects Poisson regression (31) with the number of incident diarrhea cases in a given village as the outcome. We included an offset for village population, allowing us to interpret the results in terms of the rate of diarrhea per unit of susceptible population. Models also included a random intercept for each village, to account for stable within-village correlations due to unobserved variables. Adjusted models additionally included diarrhea incidence 1 week prior, to account for short-term temporal autocorrelation of diarrhea incidence, and remoteness, a metric based on cost and duration of travel to the nearest city, because we have previously observed strong associations between diarrhea and remoteness and considered it a potential confounder (26). All analyses were conducted using Stata 12 (StataCorp LP, College Station, Texas).
Prior rainfall as an effect modifier
We first tested the hypothesis that total rainfall in the previous 8 weeks modified the association between heavy rainfall events and diarrhea incidence. We included heavy rainfall, 8-week rainfall, and interaction terms in the statistical model and tested the significance of the interaction using the likelihood ratio test, comparing the above model with a model that had no interaction terms. Separate models were fitted using rainfall measures lagged by 1 and 2 weeks. While we did not expect lags beyond 2 weeks to be biologically meaningful, we additionally fitted models with 3- and 4-week-lagged rainfall measures to confirm that any associations observed between rainfall and diarrhea using shorter time lags attenuated toward the null over longer time lags.
To assess the sensitivity of our findings to our definition of heavy rainfall events, we modified our definition of heavy rainfall events to include maximum 24-hour rainfall above the 80th percentile value (41.3 mm) in a given 7-day period, following the approach taken by Curriero et al. (13).
Social vulnerability as an effect modifier
We tested the hypothesis that water treatment, sanitation, hygiene, and social cohesion modify the association between heavy rainfall events and diarrhea incidence. Starting with the rainfall-diarrhea model above, we developed a model that included second-order interaction terms for interactions between each social vulnerability measure, modeled as a continuous variable, and both heavy rainfall events and total 8-week rainfall. We tested the significance of the interactions using the likelihood ratio test. Each social vulnerability metric was evaluated for interactions with rainfall separately.
RESULTS
Diarrhea incidence over 425,757 person-weeks was 4.12 cases per 1,000 person-weeks for all participants (5,170 people in 19 villages) and study weeks, and it ranged from 1.83 per 1,000 person-weeks to 11.57 per 1,000 person-weeks by village (Table 1). Diarrhea incidence in children under 5 years of age was 13.08 cases per 1,000 person-weeks; however, because they contributed only 65,918 person-weeks, we did not carry out a subanalysis in children. We restricted our sample to villages and weeks for which diarrhea incidence in both the current week and the previous week was available; this included 2,626 of the 2,786 total village-weeks surveyed (94%). Diarrhea incidence was 4.09 cases per 1,000 person-weeks in the village-weeks included in the analysis.
Table 1.
Weekly Diarrhea Incidence and Rainfall in 19 Villages in Rural Coastal Ecuador, February 18, 2004–April 18, 2007
| Villagea | Duration of Surveillance, weeks | Population Meanb (SD) | Diarrhea Incidencec | No. of Heavy Rainfall Eventsd | Annual Rainfall, mme | Remotenessf |
|---|---|---|---|---|---|---|
| 1 | 161 | 42 (5) | 3.57 | 10 | 2,759 | 0.20 |
| 2 | 161 | 105 (19) | 4.95 | 10 | 2,861 | 0.20 |
| 3 | 152 | 195 (37) | 7.55 | 12 | 3,122 | 0.06 |
| 4 | 154 | 297 (116) | 4.20 | 20 | 3,524 | 0.13 |
| 5 | 162 | 511 (124) | 2.81 | 15 | 3,222 | 0.07 |
| 7 | 155 | 69 (9) | 3.84 | 20 | 3,564 | 0.25 |
| 8 | 140 | 116 (34) | 6.45 | 20 | 3,548 | 0.20 |
| 9 | 157 | 203 (55) | 4.21 | 20 | 3,826 | 0.77 |
| 10 | 136 | 109 (19) | 2.16 | 20 | 3,656 | 0.62 |
| 11 | 148 | 203 (25) | 1.83 | 25 | 4,133 | 0.78 |
| 12 | 90 | 33 (12) | 11.57 | 10 | 2,800 | 0.11 |
| 13 | 134 | 70 (20) | 6.73 | 12 | 2,933 | 0.31 |
| 15 | 134 | 63 (6) | 2.24 | 12 | 3,014 | 0.40 |
| 16 | 163 | 71 (17) | 5.27 | 13 | 3,199 | 0.71 |
| 17 | 139 | 233 (102) | 3.71 | 14 | 3,305 | 0.96 |
| 18 | 135 | 89 (19) | 6.36 | 17 | 3,369 | 0.57 |
| 19 | 159 | 221 (72) | 3.01 | 19 | 3,587 | 0.83 |
| 20 | 150 | 73 (25) | 1.91 | 19 | 3,431 | 0.80 |
| 21 | 156 | 112 (14) | 7.52 | 27 | 4,607 | 1.00 |
Abbreviation: SD, standard deviation.
a Villages 6 and 14 were excluded from this analysis because of the poor quality of diarrhea surveillance in these villages.
b Mean number of people captured by active surveillance each week.
c Per 1,000 person-weeks.
d Number of weeks (out of 165) in which the maximum 24-hour rainfall exceeded the 90th percentile value, 56 mm.
e Mean annual rainfall, calculated for three 52-week periods from February 2004 to February 2007.
f A measure of the cost and duration of travel to the nearest city, scaled so that the most remote village had a value of 1.
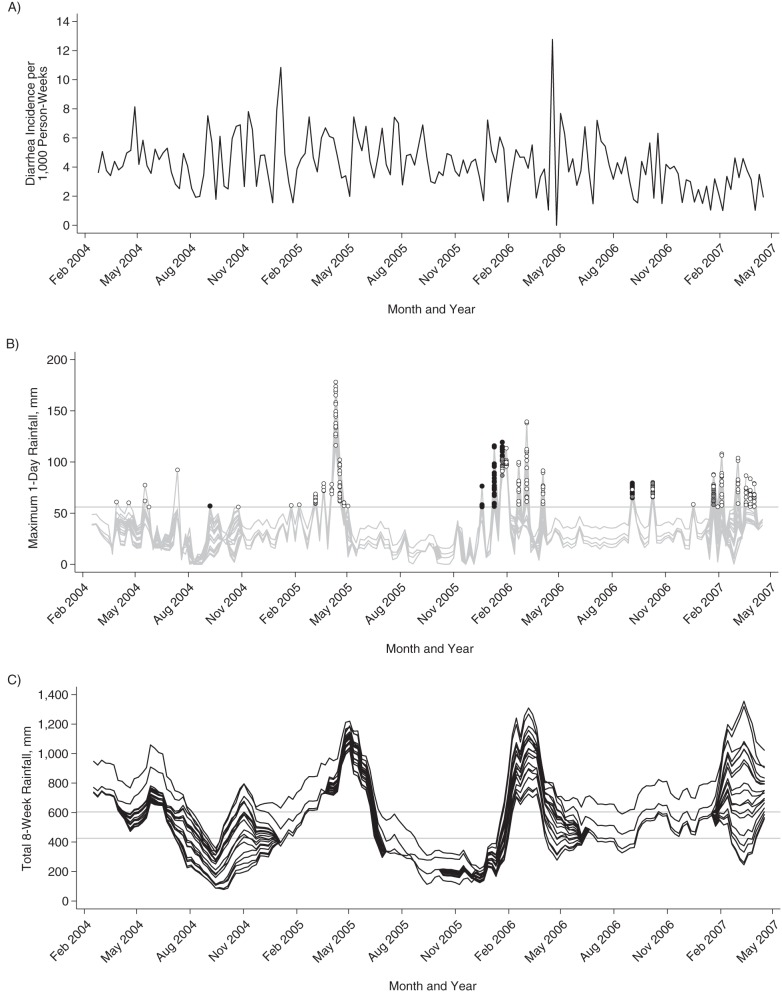
Rainfall showed distinct seasonal patterns, but the timing, severity, and duration of dry and wet periods varied by year (Figure 2). Most heavy rainfall events occurred during the months January through May, but heavy rainfall events occurred throughout the year.
Figure 2.
Diarrhea incidence (A) and rainfall (B and C) in 19 study villages in a study of heavy rainfall events and diarrhea incidence, Ecuador, February 2004–April 2007. A) Weekly diarrhea incidence (cases per 1,000 person-weeks) across all villages. B) Maximum 24-hour rainfall in a 1-week period for each village. The graph shows heavy rainfall events occurring following periods of low (black dots), moderate (gray dots), and high (white dots) 8-week rainfall. The horizontal line shows the 90th percentile value (56 mm), used to define heavy rainfall events. C) Total rainfall in the previous 8 weeks for each village. Horizontal lines indicate the 33rd (426 mm) and 66th (605 mm) percentile values, used to delineate low, moderate, and high 8-week rainfall. Aug, August; Feb, February; Nov, November.
On average, 29% of households in a given village and week reported treating their drinking water, and 46% reported access to improved sanitation (range for both: 0%–100%). Village hygiene scores ranged from 0.16 to 0.88 (mean = 0.57; maximum possible score, 1.00). Village social connectivity ranged from 1.5 contacts per person to 8.1 contacts per person (mean = 3.7).
Prior rainfall as an effect modifier
Total rainfall during the previous 8 weeks modified the association between heavy rainfall events and diarrhea incidence, using a 2-week-lagged model (P = 0.0034) (Table 2). Heavy rainfall events were associated with increased diarrhea incidence during periods when 8-week rainfall was low (incidence rate ratio (IRR) = 1.39, 95% confidence interval (CI): 1.03, 1.87) and decreased diarrhea incidence during periods when 8-week rainfall was high (IRR = 0.74, 95% CI: 0.59, 0.92). The interaction was not statistically significant in the 1-week-lagged model (P = 0.9348). Using 3- and 4-week-lagged models, estimates attenuated toward the null (Web Table 3).
Table 2.
Association Between Heavy Rainfall Eventsa and Diarrhea Incidence, According to Amount of Rainfall During the Previous 8 Weeks, Ecuador, 2004–2007
| Total 8-Week Rainfallc | 1-Week Lag |
2-Week Lag |
||||||
|---|---|---|---|---|---|---|---|---|
| Adjustedb |
Unadjusted |
Adjustedb |
Unadjusted |
|||||
| IRR | 95% CI | IRR | 95% CI | IRR | 95% CI | IRR | 95% CI | |
| Low | 0.95 | 0.67, 1.34 | 0.94 | 0.66, 1.32 | 1.39 | 1.03, 1.87 | 1.39 | 1.03, 1.87 |
| Moderate | 0.86 | 0.57, 1.30 | 0.85 | 0.56, 1.28 | 0.70 | 0.44, 1.11 | 0.70 | 0.44, 1.11 |
| High | 0.92 | 0.74, 1.13 | 0.91 | 0.74, 1.12 | 0.74 | 0.59, 0.92 | 0.73 | 0.59, 0.92 |
Abbreviations: CI, confidence interval; IRR, incidence rate ratio.
a A heavy rainfall event was defined as maximum 24-hour rainfall above the 90th percentile value (56 mm) during a 1-week period. Estimates were modeled using random-effects Poisson regression, with a random intercept for each village.
b Results were adjusted for diarrhea incidence during the prior week and remoteness (cost and duration of travel to the nearest city, scaled so that the most remote village had a value of 1).
c Total rainfall during the previous 8 weeks, defined as low (78–425 mm), moderate (426–604 mm), or high (605–1,356 mm) on the basis of the 33rd and 66th percentile values.
A sensitivity analysis in which heavy rainfall events were defined using the 80th percentile value (41.3 mm) revealed similar but attenuated results (Web Table 4). We selected the model with 2-week-lagged rainfall measures and an interaction between heavy rainfall events and total 8-week rainfall to evaluate whether social vulnerability further modified the relationship between heavy rainfall events and diarrhea.
Social vulnerability as an effect modifier
Water treatment modified the relationship between heavy rainfall events and diarrhea incidence (P = 0.0036) (Figure 3 and Web Table 5). When rainfall during the prior 8 weeks was low and community water treatment was high, the association between heavy rainfall events and diarrhea incidence was diminished. Similarly, when rainfall during the prior 8 weeks was moderate or high and community water treatment was high, heavy rainfall events were associated with a decreased incidence of diarrhea.
Figure 3.
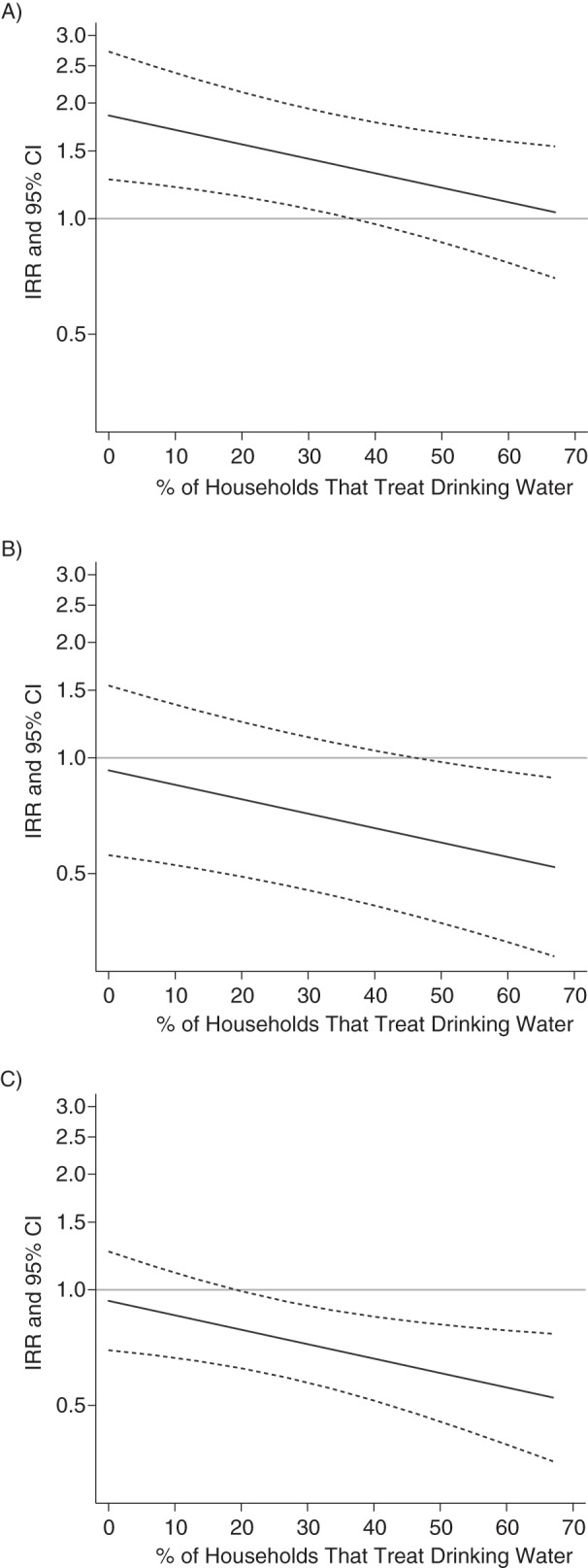
Estimated association between heavy rainfall events and diarrhea incidence at different levels of community drinking-water treatment when rainfall during the previous 8 weeks was low (A), moderate (B), or high (C), Ecuador, 2004–2007. The incidence rate ratio (IRR; solid line) and 95% confidence interval (CI; dashed lines) are shown for the 10th through 90th percentiles of water treatment values observed in this study. Water treatment was defined as filtration, boiling, or chlorination of drinking water.
Sanitation, hygiene, and social cohesion did not modify the relationship between heavy rainfall events and diarrhea incidence (P = 0.1216, P = 0.0848, and P = 0.3607, respectively). Third-order interaction terms did not improve any of the social vulnerability models.
Because village 12 contributed the fewest surveillance weeks and had the highest diarrhea incidence, we repeated analyses after excluding village 12. Estimates of association and inference were consistent with those of the principal analysis (results not shown).
DISCUSSION
In this study, the relationship between heavy rainfall events and diarrhea incidence depended on recent rainfall patterns and drinking water treatment. Heavy rainfall events were associated with increased diarrhea incidence following relatively dry periods and with decreased diarrhea incidence following relatively wet periods. Drinking water treatment lessened the negative health impacts of heavy rainfall events following dry periods and amplified the positive health impacts of heavy rainfall events following wet periods. These findings shed light on potential mechanisms by which rainfall contributes to diarrhea incidence and suggest that drinking water treatment could be an important adaptation measure for climate-driven changes in rainfall.
We propose that heavy rainfall events can increase diarrhea rates by flushing pathogens into surface drinking water sources—pathogens that have accumulated in the environment due to improper disposal of feces. Humans ingest these pathogens when they consume untreated drinking water. In tropical conditions, bacteria such as Escherichia coli can survive and even regrow outside of animal hosts (32). Rainfall can flush accumulated pathogens into surface water directly, through runoff, and indirectly, through the mobilization of bacteria in soil. During wet periods, rainfall may regularly flush pathogens from the village environment. Heavy rainfall events following wet periods may further dilute pathogen concentrations, decreasing opportunities for transmission to humans. In contrast, during dry periods the lack of rainfall may allow pathogens to build up in the environment. Heavy rainfall events following dry periods have the potential to deliver a concentrated pulse of pathogens into surface water. Our finding that recent rainfall modifies the relationship between heavy rainfall events and diarrhea incidence supports this surface-water contamination model and implies that pathogen accumulation in the environment plays an important role in determining the health risks of heavy rainfall events.
We also observed that drinking water treatment reduced the negative health impacts of heavy rainfall events during dry periods. During the study period, people depended on surface water, rainwater, and, to a limited extent, unprotected wells for drinking water. Household water treatment is known to be effective in reducing diarrhea incidence by reducing ingestion of pathogens (19, 33). In our analysis, when 71% of households in a community reported water treatment, heavy rainfall events had no impact on diarrhea incidence during dry periods (IRR = 1.00, 95% CI: 0.66, 1.52). Thus, if pathogens are introduced into drinking water sources by heavy rainfall events, drinking water treatment may reduce population exposure to rainfall-washed pathogens.
This analysis demonstrates that both environmental and social drivers can modify the relationship between climate and disease, and might explain why other researchers have found inconsistent relationships between rainfall and diarrhea. Biophysical and social conditions determine a community's vulnerability to extreme weather events such as heavy rainfall, drought, flooding, and increasing temperatures. These conditions must be taken into account in investigations of the impact of climatic drivers on disease outcomes.
While biophysical conditions may be beyond a community's control, human interventions can alter social conditions. We found that the deleterious health impacts of heavy rainfall events were greatest in communities where drinking water treatment was rare. Investments in water treatment interventions could reduce the excess burden of diarrheal diseases under future climatic conditions with more highly variable rainfall patterns. Improving water treatment can be a local adaptation strategy, through household water treatment, or a more centralized effort to improve municipal water treatment and distribution infrastructure. Sanitation, hygiene, and social cohesion did not modify the relationship between rainfall events and diarrhea. This may indicate a lack of involvement in the rainfall-diarrhea disease pathway, underscoring the importance of drinking water treatment. Alternatively, it could be due to limitations in how we characterized these factors. These metrics were measured at annual (water treatment, hygiene, and sanitation) or 3-year (social cohesion) intervals. Behaviors such as latrine usage may vary in relation to weather patterns. The impact of social networks on disease in this region (20) may work at a longer time scale than the scales associated with heavy rainfall events, and other metrics might better reflect a community's ability to respond or adapt to heavy rainfall events than the social-network variable we chose a priori to evaluate. Latrines might concentrate pathogens and, if not sealed, could overflow during a heavy rainfall event, increasing exposure to pathogens. Communities with higher open defecation rates might experience more dispersion of microbial contamination during regular rainfall events.
We found that heavy rainfall events affected diarrheal disease incidence 2 weeks later, but not 1 week later. The incubation period for diarrheal pathogens commonly found in this region, primarily rotavirus and pathogenic E. coli (26), is typically on the order of 1 week. This suggests that heavy rainfall events following dry periods might cause a limited number of primary infections that subsequently trigger a set of secondary transmission events that are detectable 2 weeks later.
Our analysis was based on imputed rainfall values, which are subject to error, particularly when imputing maximum values, which we used to classify heavy rainfall events. Our cross-validation showed that our estimates were unbiased and correlated with observed rainfall measures, but there was greater error for our estimates of maximum 24-hour rainfall than for our estimates of average rainfall. Generally, nondifferential error biases estimates toward the null, making our estimates conservative. To evaluate the impact of the imputation on our findings, we conducted a sensitivity analysis restricting our sample to observed rainfall data and villages located within 10 km of a rainfall monitor. We found relationships between heavy rainfall events and 8-week rainfall and diarrhea incidence that are consistent with our main findings, albeit with considerable uncertainty given the smaller sample size (Web Appendix 2, Web Table 6).
Implications under future climate scenarios
Regional climate models predict more intense and/or frequent rainfall extremes in northwestern Ecuador (34, 35). Our findings suggest that the cumulative impact of climate change on diarrhea in the region will depend on the number of heavy rainfall events that occur during dry periods versus wet periods. Our model predicts a rise in diarrhea incidence from 4.12 cases per 1,000 people (baseline incidence in this study) to 5.73 (range, 4.24–7.70) cases per 1,000 people for each week with a heavy rainfall event when average rainfall has been low and a decline in diarrhea incidence to 3.05 (range, 2.43–3.79) cases per 1,000 people for each week with a heavy rainfall event when average rainfall has been high, assuming no change in water treatment behaviors. These estimates pertain to perturbations in rainfall patterns within the range of our observed data, not to extreme rainfall events such as 100-year floods, which are also predicted to increase under future climate scenarios (2). These results have implications for areas of the world that are expected to experience higher variability in precipitation in the future. They are consistent with findings in the United States (13), where heavy rainfall events have taxed well-developed water and sanitation infrastructures to the point where they have been associated with outbreaks of gastrointestinal illness.
Conclusions
Heavy rainfall events present the greatest risk of diarrhea transmission following periods of low rainfall. Interventions designed to increase drinking water treatment may reduce the incidence of rainfall-associated diarrhea. Our findings underscore the need to account for social and biophysical factors when evaluating the effects of climate on disease.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Environmental and Occupational Health, Colorado School of Public Health, University of Colorado, Anschutz Medical Campus, Aurora, Colorado (Elizabeth J. Carlton); Department of Epidemiology, School of Public Health, University of Michigan, Ann Arbor, Michigan (Joseph N. S. Eisenberg, Jason Goldstick); Centro de Biomedicina, Universidad Central del Ecuador, Quito, Ecuador (William Cevallos); Department of Anthropology, Trinity College, Hartford, Connecticut (James Trostle); and Department of Environmental Health, Rollins School of Public Health, Emory University, Atlanta, Georgia (Karen Levy).
Data collection and manuscript development were supported by grants from the US National Institute of Allergy and Infectious Diseases (grant R01AI050038) and the Fogarty International Center (grant R21TW009032).
We thank the Ecologia, Desarrollo, Salud, y Sociedad (EcoDeSS) field team for their invaluable contributions to data collection. We especially thank the members of the Asociacion de Promotores de Salud in Borbón, who were responsible for collecting the active surveillance data, and Carmen Campaña, who directly supervised the data collection. We also acknowledge Amanda Markovitz, who prepared the active surveillance data set.
This project was carried out in collaboration with researchers at the Universidad San Francisco de Quito.
Conflict of interest: none declared.
REFERENCES
- 1.Portier CJ, Thigpen Tart K, Carter SR, et al. A Human Health Perspective on Climate Change: A Report Outlining the Research Needs on the Human Health Effects of Climate Change. Research Triangle Park, NC: Environmental Health Perspectives/National Institute of Environmental Health Sciences; 2010. [Google Scholar]
- 2.Intergovernmental Panel on Climate Change. Climate Change 2007: Impacts, Adaptation and Vulnerability. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, United Kingdom: Cambridge University Press; 2007. [Google Scholar]
- 3.Walker CL, Rudan I, Liu L, et al. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013;381(9875):1405–1416. doi: 10.1016/S0140-6736(13)60222-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kolstad EW, Johansson KA. Uncertainties associated with quantifying climate change impacts on human health: a case study for diarrhea. Environ Health Perspect. 2011;119(3):299–305. doi: 10.1289/ehp.1002060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Milojevic A, Armstrong B, Hashizume M, et al. Health effects of flooding in rural Bangladesh. Epidemiology. 2012;23(1):107–115. doi: 10.1097/EDE.0b013e31823ac606. [DOI] [PubMed] [Google Scholar]
- 6.Checkley W, Epstein LD, Gilman RH, et al. Effects of El Nino and ambient temperature on hospital admissions for diarrhoeal diseases in Peruvian children. Lancet. 2000;355(9202):442–450. doi: 10.1016/s0140-6736(00)82010-3. [DOI] [PubMed] [Google Scholar]
- 7.Hashizume M, Armstrong B, Hajat S, et al. Association between climate variability and hospital visits for non-cholera diarrhoea in Bangladesh: effects and vulnerable groups. Int J Epidemiol. 2007;36(5):1030–1037. doi: 10.1093/ije/dym148. [DOI] [PubMed] [Google Scholar]
- 8.Lama JR, Seas CR, Leon-Barua R, et al. Environmental temperature, cholera, and acute diarrhoea in adults in Lima, Peru. J Health Popul Nutr. 2004;22(4):399–403. [PubMed] [Google Scholar]
- 9.Onozuka D, Hashizume M, Hagihara A. Effects of weather variability on infectious gastroenteritis. Epidemiol Infect. 2010;138(2):236–243. doi: 10.1017/S0950268809990574. [DOI] [PubMed] [Google Scholar]
- 10.Singh RB, Hales S, de Wet N, et al. The influence of climate variation and change on diarrheal disease in the Pacific Islands. Environ Health Perspect. 2001;109(2):155–159. doi: 10.1289/ehp.01109155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drayna P, McLellan SL, Simpson P, et al. Association between rainfall and pediatric emergency department visits for acute gastrointestinal illness. Environ Health Perspect. 2010;118(10):1439–1443. doi: 10.1289/ehp.0901671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lloyd SJ, Kovats RS, Armstrong BG. Global diarrhoea morbidity, weather and climate. Clim Res. 2007;34(2):119–127. [Google Scholar]
- 13.Curriero FC, Patz JA, Rose JB, et al. The association between extreme precipitation and waterborne disease outbreaks in the United States, 1948–1994. Am J Public Health. 2001;91(8):1194–1199. doi: 10.2105/ajph.91.8.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thomas KM, Charron DF, Waltner-Toews D, et al. A role of high impact weather events in waterborne disease outbreaks in Canada, 1975–2001. Int J Environ Res Public Health. 2006;16(3):167–180. doi: 10.1080/09603120600641326. [DOI] [PubMed] [Google Scholar]
- 15.Hashizume M, Wagatsuma Y, Faruque AS, et al. Factors determining vulnerability to diarrhoea during and after severe floods in Bangladesh. J Water Health. 2008;6(3):323–332. doi: 10.2166/wh.2008.062. [DOI] [PubMed] [Google Scholar]
- 16.Schwartz BS, Harris JB, Khan AI, et al. Diarrheal epidemics in Dhaka, Bangladesh, during three consecutive floods: 1988, 1998, and 2004. Am J Trop Med Hyg. 2006;74(6):1067–1073. [PMC free article] [PubMed] [Google Scholar]
- 17.Kondo H, Seo N, Yasuda T, et al. Post-flood–infectious diseases in Mozambique. Prehosp Disaster Med. 2002;17(3):126–133. doi: 10.1017/s1049023x00000340. [DOI] [PubMed] [Google Scholar]
- 18.Wade TJ, Sandhu SK, Levy D, et al. Did a severe flood in the Midwest cause an increase in the incidence of gastrointestinal symptoms? Am J Epidemiol. 2004;159(4):398–405. doi: 10.1093/aje/kwh050. [DOI] [PubMed] [Google Scholar]
- 19.Fewtrell L, Kaufmann RB, Kay D, et al. Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. Lancet Infect Dis. 2005;5(1):42–52. doi: 10.1016/S1473-3099(04)01253-8. [DOI] [PubMed] [Google Scholar]
- 20.Zelner JL, Trostle J, Goldstick JE, et al. Social connectedness and disease transmission: social organization, cohesion, village context, and infection risk in rural Ecuador. Am J Public Health. 2012;102(12):2233–2239. doi: 10.2105/AJPH.2012.300795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Intergovernmental Panel on Climate Change. Climate Change 2001: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Third Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, United Kingdom: Cambridge University Press; 2001. [Google Scholar]
- 22.Polsky C, Neff R, Yarnal B. Building comparable global change vulnerability assessments: the vulnerability scoping diagram. Glob Environ Change. 2007;17(3-4):472–485. [Google Scholar]
- 23.Turner BL, 2nd, Kasperson RE, Matson PA, et al. A framework for vulnerability analysis in sustainability science. Proc Natl Acad Sci U S A. 2003;100(14):8074–8079. doi: 10.1073/pnas.1231335100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reid CE, Mann JK, Alfasso R, et al. Evaluation of a heat vulnerability index on abnormally hot days: an environmental public health tracking study. Environ Health Perspect. 2012;120(5):715–720. doi: 10.1289/ehp.1103766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Markovitz AR, Goldstick JE, Levy K, et al. Where science meets policy: comparing longitudinal and cross-sectional designs to address diarrhoeal disease burden in the developing world. Int J Epidemiol. 2012;41(2):504–513. doi: 10.1093/ije/dyr194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eisenberg JNS, Cevallos W, Ponce K, et al. Environmental change and infectious disease: how new roads affect the transmission of diarrheal pathogens in rural Ecuador. Proc Natl Acad Sci U S A. 2006;103(51):19460–19465. doi: 10.1073/pnas.0609431104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hofstra N, Haylock M, New M, et al. Comparison of six methods for the interpolation of daily, European climate data. J Geophys Res. 2008;113(D21110) [Google Scholar]
- 28.Ly S, Charles C, Degré A. Geostatistical interpolation of daily rainfall at catchment scale: the use of several variogram models in the Ourthe and Ambleve catchments, Belgium. Hydrol Earth Syst Sci. 2011;15(7):2259–2274. [Google Scholar]
- 29.Romero R, Guijarro JA, Ramis C, et al. A 30-year (1964–1993) daily rainfall data base for the Spanish Mediterranean regions: first exploratory study. Int J Climatol. 1998;18(5):541–560. [Google Scholar]
- 30.World Health Organization, United Nations Children's Fund. Core Questions on Drinking-Water and Sanitation for Household Surveys. Geneva, Switzerland:: World Health Organization; 2006. [Google Scholar]
- 31.Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata. 2nd ed. College Station, TX: Stata Press; 2008. [Google Scholar]
- 32.Hardina CM, Fujioka RS. Soil: the environmental source of Escherichia coli and enterococci in Hawaii's streams. Environ Toxicol Water Qual. 1991;6(2):185–195. [Google Scholar]
- 33.Gundry S, Wright J, Conroy R. A systematic review of the health outcomes related to household water quality in developing countries. J Water Health. 2004;2(1):1–13. [PubMed] [Google Scholar]
- 34.Intergovernmental Panel on Climate Change. Climate Change 2007: The Physical Science Basis. Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, United Kingdom: Cambridge University Press;; 2007. [Google Scholar]
- 35.Marengo JA, Ambrizzi T, da Rocha RP, et al. Future change of climate in South America in the late twenty-first century: intercomparison of scenarios from three regional climate models. Clim Dyn. 2010;35(6):1073–1097.. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.