Abstract
Objective
To provide an account of published literature on the association between alcohol use and sexual risk-taking, focusing on Latin America.
Methods
A search of MEDLINE, Embase, Web of Science, LILACS, and Cochrane databases identified 561 unique articles. After excluding those that were not directly relevant, 30 studies were retained for review.
Results
Twenty-seven studies showed direct or indirect associations between alcohol abuse and unprotected/risky sex. Three studies, however, showed no association between these variables, suggesting that the public health message of safer sex may have been effective.
Conclusions
Further research is needed to identify factors and behaviors that could be modified to reduce the association between alcohol use disorders and risky sexual behavior.
Keywords: Alcoholic intoxication, alcohol-related disorders, alcoholism, sexual behavior, unsafe sex, HIV, sexually transmitted diseases, Latin America, South America
Alcoholic beverages have been consumed for centuries and, in one form or another, are intricately linked to local culture in many parts of the world. Alcohol is a central nervous system depressant and its consumption leads to euphoria, relaxation, and disinhibition. For that reason, its use can lead to symptoms of psychological and physical dependence and result in development of alcohol use disorders (AUDs) ranging from heavy drinking to alcoholism. The long-term consequences of AUDs can have dire effects on physical health, the most severe of which include liver failure and cancers. In addition to the physical effects, AUDs can lead to social and behavioral changes, such as violence, aggressiveness, and extensive risk-taking. AUDs have also been shown to negatively affect adherence to medications, including antiretroviral therapy (ART), thereby exacerbating the complications from HIV infection (1).
Sexual disinhibition has been shown to be among the behavioral consequences of alcohol consumption (2). Sexual risk-taking includes engaging in unprotected sex, having high numbers of sexual partners, and engaging in sex work and other situations where the risk for contracting sexually transmitted infections (STIs), including HIV, increases. STIs, especially when undetected for an extended period, can have severe consequences, including pain, sterility, organ failure, and death. Detection of STIs is easy in resource-rich settings where diagnostic facilities are readily available, but more difficult in low- and middle-income countries (LMICs), especially for STIs such as herpes simplex virus (HSV), human papillomavirus (HPV), and syphilis, which remain asymptomatic for years. Once detected, treating STIs is usually easy and leads to complete recovery; however, some STIs are incurable, such as HIV/AIDS and chronic viral infections, and require lifetime medical treatment. Moreover, the presence of STIs may facilitate HIV transmission. While ART can control viral replication in HIV, it must be taken daily for the rest of the patient’s life, and the cost of the regimen is prohibitive for many of the world’s most affected populations. Therefore, behavioral and/or medical interventions that reduce sexual risk-taking can have a significant impact on the health of those who need it most.
Latin America, defined herein as the countries of South America, Central America, and Mexico, comprises LMICs with a relatively low HIV prevalence (3). Nevertheless, in many of these countries, rampant concentrated epidemics are observed in vulnerable populations, such as men who have sex with men (MSM) and sexual and racial minorities. Alcohol use and abuse is a major concern in several countries in the region, including Brazil, Mexico, and Peru, and some data indicate that AUDs contribute considerably to sexual HIV risk-taking (4, 5), as well as a lack of awareness of HIV infection (6).
While a number of studies have examined the effect of alcohol use on sexual risk-taking in Latin America, to the best of the current authors’ knowledge, no other systematic review has comprehensively examined and interpreted the data to better inform researchers planning behavioral and/or medical interventions in these countries. The aim of this review is to examine the association between alcohol use and sexual risk-taking in Latin America by compiling and analyzing all published work in this field.
MATERIALS AND METHODS
This review followed the systematic review methodology previously published as part of the PRISMA3 guidelines (7). Literature searches were conducted in November 2012. The MEDLINE database (1948 to present) was searched using the OvidSP platform (Ovid, New York, USA). Three groups of Medical Subject Headings (MeSH)4 were used and combined in the final search. The group for alcohol contained the following terms: alcoholism, alcohol abuse, alcohol drinking, and alcohol intoxication. The group for geographic location contained the search term ‘explode’ South America (to capture data from all South American countries) plus Latin America and Mexico (island countries/territories in the Caribbean were not included in the analysis). The group for sexual risk-taking included unsafe sex, safe sex, sexual partners, sexual behavior, HIV infections, acquired immunodeficiency syndrome (AIDS), sexually transmitted infections, HIV, HIV-1, condoms, and risk-taking. Only articles written in English, Spanish, or Portuguese, about studies conducted in humans, were considered. The same search terms, adapted for syntax, were used in Scopus (which contains the Embase database) and in Web of Science, LILACS, and Cochrane Library databases.
Figure 1 shows the results of the literature search based on the PRISMA flowchart for systematic reviews. Briefly, the initial search, after eliminating duplicates, yielded 561 articles. Two of the authors of this review (PV and KTL) examined all of the articles to eliminate those that did not fit the search criteria in all three groups (e.g., studies that addressed alcohol use and sexual risk-taking but were conducted among Hispanic populations in the United States or Europe, and those that discussed AUDs within the context of driving, violence, or criminal activity versus sexual risk or unsafe sex). Where there was discordance about whether or not to eliminate an article from the review, a third author (FLA) broke the tie. Following this elimination process, 30 articles remained and were included in the review.
FIGURE 1.
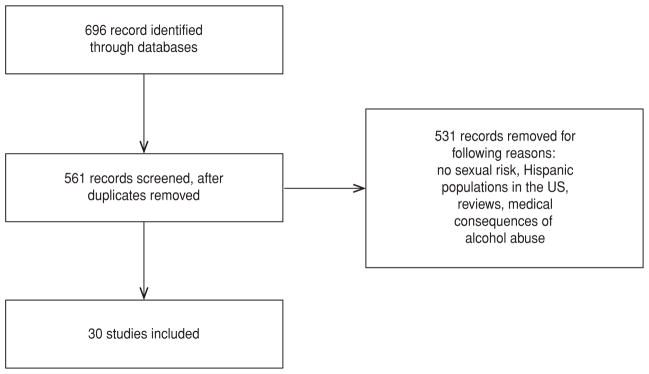
Results of search for literature on the association between alcohol use and sexual risk, Latin America, 2012a
a Based on the PRISMA flowchart for systematic reviews (7).
RESULTS
Table 1 lists the 30 studies selected for review, the definition used for problematic alcohol consumption, and the outcomes relating to sexual risk-taking. The definition of alcohol use varied greatly between studies, with only five of the studies reviewed (16.7%) using internationally validated instruments such as the AUDIT5 (8) or CAGE6 (9) screening instruments. Most studies used their own criteria to define what they perceived as problematic drinking (e.g., five or more drinks within a two-hour period (10)). Outcomes were also defined in multiple ways. While some articles used quantitative measures, such as odds ratios, others only indicated percentages of drinkers versus non-drinkers with a similar indication of unsafe sexual practices.
TABLE 1.
Studies selected for literature review of data on alcohol use and risky sexual behavior, including definition(s) used for problematic alcohol consumption and outcomes relating to sexual risk-taking, Latin America, 1999–2012
| Study/year published | Study site and population | n | Alcohol abuse definition | Sexual risk definition | Outcome | Limitations |
|---|---|---|---|---|---|---|
| (23) 2012 | Adolescents in Mexico | 1 238 | DSM-IV alcohol abuse and dependence symptoms and frequency of alcohol use | Unprotected sex; number of sexual partners | 61.9% of participants with 3 or more symptoms of alcohol abuse or dependence did not use a condom at last sexual encounter; 66.7% of those with 1–2 symptoms did not use a condom | No statistics for this measure |
| (25) 2012 | Young adults in Rio Grande do Sul, Brazil | 351 | AUDITa (0–7 points, low risk; 8–15, risky; 16–19, harmful; 20+, dependence) | Unprotected sex; number of sexual partners | 48.7% of students did not use condom at last sexual encounter; 10.5% had 3–10 sexual partners in last 12 months; 14% reported problematic alcohol use. | No statistics for this measure |
| (21) 2011 | Adolescent and adult travelers to Cusco, Peru, and their partners | 1 295 | Inebriation; self-reported | Unprotected sex | Inebriated (vs. non-inebriated) more likely to engage in sexual activity (odds ratio (OR) 10.6 [5.4–20.6]) and to be under the influence before sex (OR 36.1 [3.9–331.1]) No significant association between condom use and inebriation (OR 0.5 [0.1–2.6]) Women: inebriated, more likely than men not to use condoms (OR 6.4 [1.2–33.5]) |
Mostly foreign tourists, but sex with locals reported |
| (26) 2011 | Adult clients of FSWsb who work in bars, Mexico | 211 | Binge drinking (≥ 5 drinks at a time), being drunk during sex with FSWs, FSWs drunk during sex; self-reported | Unprotected sex; sex with FSWs | Drunk during sex with FSW (OR 3.12 [1.54–6.30]) FSW drunk during sex (OR 3.24 [1.43–7.45]) Unprotected sex due to lack of condoms (OR 1.92 [1.03–3.59]) |
Did not directly associate being drunk with risky sex |
| (12) 2011 | Adult MSWsc in Santo André, Brazil | 86 | AUDIT (mean scores) | Inconsistent condom use (“not always” vs. “always” or “never”) | Men with inconsistent condom use have significantly higher (P = 0.02) AUDIT scores vs. men with consistent condom use | |
| (24) 2010 | Secondary school students in Colombia | 3 575 | Lifetime alcohol use | Pattern of risky behavior for reproductive and sexual health (PRBRSH): sum of 2+ risky sexual practices (inconsistent condom use; sexual intercourse after alcohol consumption; sexual intercourse after illegal drugs consumption; or sexual intercourse with a casual partner) over lifetime | Lifetime alcohol use was associated (OR 2.5 [1.3–5.1]) with PRBRSH; 18.4% reported sexual intercourse following alcohol consumption | |
| (38) 2010 | Female adolescents in Porto Alegre, Brazil | 388 | Any alcohol use in last 30 days | Unprotected sex; sex for money; sex with IDU; sex for drugs; HIV infection | No significant association between alcohol and HIV infection (OR 0.71 [0.27–1.19]) | Talks about alcohol use in general |
| (28) 2009 | Adult residents of Bucaramanga, Colombia | 1 199 | Arbitrary categories, based on CAGEd and CP-alcohol testse | Increased sexual desire | Subjects with positive expectations on alcohol and sexuality are more likely to be in category C (dependent) (OR 1.6 [1–2.5]). Those with positive expectations related to disinhibition and feelings of power are more likely to be in category C (OR 2.2 [1.1–4.3]) | Did not directly associate alcohol abuse with risky sex |
| (29) 2009 | Young adult (18–30) residents of a shantytown in Lima, Peru | 793 | Heavy episodic drinking (HED) (≥ 5 drinks in a row, at least 1x/month) | Unprotected sex; sex with a casual partner; sex with sex worker; male homosexual sex; STIg symptom | HED associated with sex with casual partner, sex worker, or MSMf under the influence of alcohol (adjusted OR (AOR) 3.1 [1.4–6.8]) | |
| (27) 2009 | Young adult (18–30) residents of a shantytown in Lima, Peru | 793 | AUDIT (0–7, not hazardous; 8+, hazardous) | Sex-related alcohol expectancies (SRAEs) | Men with 1 or 2 SRAEs more likely to be hazardous drinkers (AOR 2.3 [1.4–3.8]) Men with 3 or more SRAEs more likely to be hazardous drinkers (AOR 3.9 [2.1–7.3]) No associations in women |
Did not directly associate alcohol abuse with risky sex |
| (13) 2009 | Adolescents in Minas Gerais, Brazil | 5 981 | Alcohol use: “never,” “experienced/no longer use,” “sometimes/always” | Unprotected sex | Males were less likely to use condoms consistently if under the influence of alcohol. Consistent condom use was less frequent among those that used alcohol compared to those who did not drink (60.7% vs. 71.1%). | |
| (22) 2008 | Young adult (18–30) male residents of a shantytown in Lima, Peru | 312 | HED (> 5 drinks in a row, at least 1×/month) | Number of partners; sex with casual partner; sex with sex worker; unprotected sex; SRAEs | HED related to multiple partners (AOR 3.1, P < 0.05) SRAEs related to unprotected sex last encounter (AOR 1.24, P < 0.01) and unprotected sex with casual partner (AOR 1.33, P < 0.05) |
|
| (37) 2008 | Adult residents of Lima, Peru | 396 | Latin American Alcoholism Test | HIV infection | HIV positive are more likely to be alcoholics (AOR 2.47 [1.56–3.93]) | Did not directly associate alcohol abuse with risky sex |
| (30) 2008 | Pregnant adolescents in Piracicaba, Brazil | 220 | Weekly drinking | Pregnancy | Weekly intake of alcohol over 12 months associated with becoming pregnant (OR 4.2 [1.7–10.3]) | |
| (14) 2008 | Adult urban area residents in Brazil | 5 040 | > 4×/week | Unprotected sex | Regular alcohol (or drug) use leads to less frequent condom use (P = 0.012 for those in stable relationships; P = 0.007 for males 16–24 years old with casual partners) | |
| (15) 2008 | Adults in Brazil | 5 040 | Regular alcohol use | Unprotected sex | 18% used alcohol regularly; 8.2% did not use condom because they were under the influence of alcohol | |
| (33) 2008 | Immigrant and native adult FSWs in Argentina, Bolivia, Ecuador, and Uruguay | 1 845 | Any use of alcohol | Unprotected sex; history of STIs (including HIV infection) | Use of alcohol is significantly associated with immigrant (vs. native) FSWs in Uruguay (AOR 2.25 [1.05–4.83]); no association in Argentina, Bolivia, or Ecuador (unprotected sex included in multivariate model) | Did not directly associate alcohol abuse with risky sex |
| (20) 2007 | Adult tourists in São Paulo State, Brazil | 77 | Any use of alcohol | Unprotected sex | Qualitative interview transcripts suggesting alcohol increases vulnerability to HIV through unsafe sex | Qualitative |
| (19) 2006 | Adult truck drivers and FSWs in Itajaí, Brazil | 43 | Daily/weekly use | Unprotected sex | Majority of truckers (67%) and FSWs (62%) used alcohol at least weekly; all engaged in risky sexual behavior (unprotected sex with FSWs and truck-stop employees) | No quantitative measures |
| (16) 2006 | STI clinic clients in Bahia, Brazil | 625 | CAGE | Unprotected sex; STIs | Non-alcoholic men significantly more likely (P = 0.009) to use alcohol before risky sex vs. women; no difference among alcoholic men and women | |
| (39) 2006 | Adult FSWs in Isla Margarita, Venezuela | 613 | > 1×/day | Unprotected sex; STIs (including HIV) | Low alcohol abuse (12%), high condom use (80%) with clients, 0% HIV-infected | No statistics |
| (17) 2004 | Adolescent and adult women in Rio de Janeiro, Brazil | 200 | > 5×/one occasion | Unprotected sex; STIs; number of partners; sex work | Alcohol consumption significantly associated with STIs (P = 0.03) | |
| (18) 2004 | Adolescents in Salvador, Brazil | 76 | Any use of alcohol | Condom use | Adolescents believe alcohol is associated with unprotected sex | Qualitative |
| (32) 2004 | Adolescents in Rio de Janeiro, Brazil | 356 | ≥ 6×/previous month | Unprotected sex; STIs | Significant (P < 0.05) association with having STI | |
| (40) 2003 | Adult MSWs in Córdoba, Argentina | 31 | 5-point scale from “never” to “daily” | Unprotected sex | Alcohol (53.3% weekly, 3% daily) and unsafe sex practices (9.7% insertive anal sex without condom, 0% receptive anal sex without condom) | Did not directly associate alcohol abuse with risky sex |
| (10) 2003 | Adolescents in São Paulo, Brazil | 1 808 | HED (≥ 5 drinks in 2 hours) | Unprotected sex | In public school students: unprotected sex more likely in drinkers (AOR 2.98 [1.22–7.27]) and heavy episodic drinkers (AOR 3.69 [1.49–9.12]) vs. abstainers | |
| (35) 2003 | Adolescent hotel employees in Puerto Vallarta, Mexico | 288 | Any alcohol use prior to intercourse | Unprotected sex | 41% drank alcohol before intercourse; 77.3% engaged in unsafe sex; alcohol drinking by peers and hotel guests associated with alcohol drinking by subjects (peers OR 2.52 [1.23–5.2], guests OR 2.60 [1.11–6.11]) | Did not directly associate alcohol abuse with risky sex |
| (31) 2002 | Adolescents and young adults in Morelos, Mexico | 194 | Weekly | Human papillomavirus (HPV) infection | High alcohol consumption (men 75%, women 83%). Women with 2 or more partners during year, more likely to get HPV (OR 6 [1.7–21.1]) | Did not directly associate alcohol abuse with risky sex |
| (34) 1999 | Adolescents in Cali, Colombia | 230 | Any alcohol use prior to intercourse | Condom use; number of partners | 14% used alcohol prior to intercourse; age associated with higher alcohol use (AOR 3.6 [1.49–8.44]) | Did not directly associate alcohol abuse with risky sex |
| (36) 1999 | Adult FSWs in Guyana | 124 | Any alcohol use | Unprotected sex | 88% reported regular alcohol consumption while looking for clients; 72% never used condoms with regular sex partners; 35% never used condoms with clients | Did not directly associate alcohol abuse with risky sex |
Alcohol Use Disorders Identification Test developed by the World Health Organization.
FSWs: female sex workers.
MSWs: male sex workers.
CAGE: alcoholism screening instrument containing the following questions: “Have you ever felt you needed to Cut down on your drinking?” “Have people Annoyed you by criticizing your drinking?” “Have you ever felt Guilty about drinking?” and “Have you ever felt you needed a drink first thing in the morning (Eye-opener) to steady your nerves or to get rid of a hangover?”
Alcohol screening instrument for identifying problematic consumption (consumo problematico, CP) (41).
MSM: men who have sex with men.
STI: sexually transmitted infection.
Fourteen of the 30 articles that were reviewed directly associated alcohol use with unprotected sex. A number of studies reviewed were conducted in Brazil, South America’s largest country. A study among male sex workers (MSWs), a group previously identified as consuming considerable quantities of alcohol (11), showed a significant association between inconsistent condom use and higher AUDIT scores (12). A study in adolescents associated inconsistent condom use with being under the influence of alcohol (13). Two studies among Brazilian urban residents found significant associations between “regular” alcohol use and unprotected sex; this association was even stronger in younger males (14, 15). A study among STI clinic clients showed that non-alcoholic men were significantly more likely to use alcohol before risky sex than women, but among alcoholics, there was no difference between men and women, who were equally likely to engage in risky sex (16). Brazilian adolescents were shown to be approximately threefold more likely to engage in unprotected sex if they were moderate or heavy drinkers compared to those who abstain from alcohol use (10). Brazilian women were significantly more likely to acquire a STI following heavy alcohol consumption compared to those who did not consume more than five drinks on one occasion (17). Three qualitative studies in Brazil, one conducted among truck drivers and commercial sex workers (CSWs), another in adolescents, and the third in adult travelers, suggested that alcohol consumption leads to unprotected sex and vulnerability for HIV infection (18–20). Two studies in Peru found a high prevalence of AUDs, and associations between alcohol consumption and unprotected sex (21, 22). A study among shantytown dwellers in Lima indicated that sex-related alcohol expectancies (SRAEs) were significantly associated with unprotected sex (22). Another study among travelers to Cuzco, Peru, indicated that inebriated subjects were tenfold more likely to engage in “any” sexual activity, compared to those that reported no inebriation, and 36-fold more likely to be under the influence of alcohol before any sex (21). One study found that only 16% of respondents failed to use condoms, but there was no significant association between alcohol consumption and unprotected sex. However, the same study did show that inebriated women were more likely than men not to use condoms. Although this study mainly interviewed foreign travelers, 40% of participants reported sexual relations with locals and/or local sex workers. Another study conducted in Mexico found that more than 60% of participants with one or more symptoms of alcohol abuse did not use condoms during their last sexual encounter (23). Finally, a study in secondary school students in Colombia found a significant association between alcohol use and risky sexual behaviors (24).
A total of 13 of the 30 articles reviewed provided indirect links between alcohol abuse and sexual risk (i.e., the studies they described did not provide direct associations between alcohol abuse and unprotected sex but contained implied associations). A study among university students in Brazil found that 14% of participants had an AUD, and almost half of all participants (48.7%) did not use condoms during their last sexual encounter (25). A study of Mexican female sex workers (FSWs) and their clients showed that both were more likely to be drunk than not during sex; unprotected sex was also found to occur more often under these circumstances. The reason for the risky sexual behavior provided by the subjects in this study, however, was lack of condoms, not the use of alcohol (26), implying some element of cognitive dissonance. Two studies in Colombia and Peru associated alcohol dependence or hazardous drinking with positive SRAEs and sexual disinhibition (27, 28). Another study in Peru found that heavy drinkers were threefold more likely than infrequent drinkers to engage in high-risk sexual activities, such as sex with casual partners, MSM, or sex workers (29). A study of Brazilian adolescent females found that those who drank regularly over a 12-month period were fourfold more likely to become pregnant (30), an indicator of unsafe sex. A similar study in Mexico found that 22% of women drank weekly; those with multiple partners were sixfold more likely to acquire HPV, another indicator of unsafe sexual practices (31). A study among Brazilian adolescents found an association between alcohol use and having an STI (32). In a multi-country study of FSWs, immigrant FSWs in Uruguay were found to be twice as likely as native FSWs to use alcohol regularly; unprotected sex in this study was included as a covariate and significant in the multivariate model (33). Two studies of adolescents in Colombia and Mexico showed that they were more likely than not to use alcohol before sex (34, 35), and a high percentage of those asked (> 77% in the Mexican study) reported engaging in unprotected sex (35). In the Colombian study, the mean number of partners reported was 2, and only 22% used condoms (34). A study of FSWs in Guyana showed that the vast majority of those interviewed (88%) used alcohol regularly and did not use condoms with regular partners (72%), and some (35%) did not use condoms with clients (36). A case-control study among HIV-infected patients showed that they were twofold more likely than HIV-negative patients to be “alcoholic” (37).
Finally, three of the 30 studies reviewed found no association between alcohol abuse and risky sexual behaviors. A study among female adolescents in Brazil found no association between alcohol use and HIV infection, but showed that more than 70% of participants had used alcohol in the past 30 days (38). A study of Venezuelan FSWs showed high levels of condom use with clients (80%), and low alcohol use (12%), and did not identify any HIV-infected FSWs (39). Similarly, a study of Argentine MSWs found a relatively low prevalence of unsafe sexual practices (e.g., only 9.7% of sexual encounters were unprotected anal insertive sex, and there was no unprotected anal receptive sex) and a very moderate level of drinking (57% drank weekly, and 3% drank daily) (40).
DISCUSSION
This is the first systematic review to examine the association between alcohol use and sexual risk-taking in Latin American countries. While the subject of alcohol and sexual risk has been studied extensively, to the best of the authors’ knowledge no previous systematic reviews have focused specifically on Latin America—a place where alcohol, as the evidence above indicates, is associated with high-risk sexual behaviors that can contribute to STI risk and an expanding HIV epidemic. Like many other cultures around the world, Latin American culture is intricately interwoven with drinking practices. Most countries in the region produce their own liquors and beers, and drinking is highly prevalent among most age groups. Recent work in Peru has shown that AUDs defined using international screening criteria are highly prevalent and seem to be one of the primary factors fueling STI transmission and the HIV epidemic (5). Therefore, a review of available peer-reviewed literature is timely and serves to highlight an area that merits more focused research in the future, especially where the HIV epidemic is still concentrated but there is growing evidence of a generalizing epidemic.
The vast majority of studies reviewed here were cross-sectional. The lack of prospective longitudinal studies and randomized controlled trials serves as additional evidence that AUDs and their correlation to risky sexual behaviors have been understudied in this locale. Most of these studies were problematic because of the diverse definitions used within them for alcohol use and/or internationally recognized screening tools. The majority of them showed significant associations between “some” level of alcohol consumption (versus none) and sexual risk-taking, both directly and indirectly. Most studies did not clearly distinguish alcohol abuse, alcohol dependence, or binge drinking from what could be perceived as social drinking within the Latin American context. Codifying the level of alcohol consumption is important because the effectiveness of certain interventions differs depending on the severity of alcohol consumption. Therefore, there remains a need for scientific standardization among researchers’ methods. The WHO AUDIT questionnaire (8) is currently considered one of the most useful tools in assessing drinking patterns because it not only defines alcohol dependence but also distinguishes among lower levels of AUDs, defined as “hazardous” or “harmful” drinking. Future studies assessing alcohol consumption should make use of these types of internationally standardized and validated tools, when possible.
A similar issue identified in this review was the use of non-standardized definitions for risky sexual behavior. Most articles (22, or 73%) clearly defined this term as unprotected sex (i.e., sex without a condom), but some (8, or 27%) used more indirect definitions of risky sex (e.g., “has STI infection”), most likely because their primary aims were to assess other factors, such as pregnancy (30) or acquisition of a specific STI (17). Moreover, statistical associations between alcohol consumption and unsafe sex were not performed by all studies, making it harder to draw quantitative conclusions. Future studies would benefit by including more numerical data and appropriate statistical tests.
The study that examined alcohol and sexual risk among foreign tourists in Peru, in which 40% reported engaging in sexual activity with locals (21), illustrates how globalization and the vastly increased movement of people affect global health and potential HIV transmission. Areas or regions with low incidence of certain diseases may not have fully developed programs to protect their populations from exposure to those diseases. For example, the “safe sex” message may not have spread as much in low–HIV prevalence areas such as the countries of Latin America compared to higher- prevalence areas such as sub-Saharan Africa and Southeast Asia. Visitors originating from the latter areas (or tourists that have previously been to those areas) may unwittingly contribute to the rapid spread of these diseases.
Only three (10%) of studies reviewed here found either no association between alcohol consumption and unsafe sex or a very low prevalence of such risky behaviors (38–40). In some cases, this may be because the associations were not specific enough. For example, looking at general alcohol consumption and unlikely events such as HIV infection is unlikely to show statistically significant associations (38). In other cases, the results from these three studies versus the other 27 studies reviewed may lead to speculation that behavior modification interventions such as public health campaigns about safe sex have worked in certain locales, although without previous data from the same areas for comparison it is impossible to make an informed conclusion.
Limitations
Although this study provides the first systematic review examining the association of alcohol consumption and risky sex, it had important limitations. First, the use of MeSH terms for the selection of journal articles in some databases (such as OvidSP) may have introduced selection bias. However, the use of more generic search terms in other databases (such as LILACS) should have captured any potential “misses” resulting from the use of MeSH terms.
Conclusion
This systematic review on alcohol consumption and sexual risk in Latin America, the first of its kind, confirms that alcohol can lead to risky sexual behaviors in the region, as has been suggested by the results of studies conducted in other parts of the world. The relatively small number of studies that have examined this issue and the suggestions of high occurrence of alcohol abuse in Latin America suggest that this region is in need of more detailed studies to identify modifiable factors and practices in order to reduce alcohol abuse and dependence, improve sexual health, and reduce the incidence of STIs.
Footnotes
Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Vocabulary thesaurus of the U.S. National Library of Medicine.
Alcohol Use Disorders Identification Test developed by the World Health Organization (WHO).
Alcoholism screening instrument containing the following questions: “Have you ever felt you needed to Cut down on your drinking?” “Have people Annoyed you by criticizing your drinking?” “Have you ever felt Guilty about drinking?” and “Have you ever felt you needed a drink first thing in the morning (Eye-opener) to steady your nerves or to get rid of a hangover?”
Conflicts of interest. None.
References
- 1.Hendershot CS, Stoner SA, Pantalone DW, Simoni JM. Alcohol use and antiretroviral adherence: review and meta-analysis. J Acquir Immune Defic Syndr. 2009;52(2):180–202. doi: 10.1097/QAI.0b013e3181b18b6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Justus AN, Finn PR, Steinmetz JE. The influence of traits of disinhibition on the association between alcohol use and risky sexual behavior. Alcohol Clin Exp Res. 2000;24(7):1028–35. [PubMed] [Google Scholar]
- 3.Joint United Nations Programme on HIV/AIDS. Global report: UNAIDS report on the global AIDS epidemic 2012. Geneva: UNAIDS; 2012. [Google Scholar]
- 4.Deiss RG, Clark JL, Konda KA, Leon SR, Klausner JD, Caceres CF, et al. Problem drinking is associated with increased prevalence of sexual risk behaviors among men who have sex with men (MSM) in Lima, Peru. Drug Alcohol Depend. 2013;132(1–2):134–9. doi: 10.1016/j.drugalcdep.2013.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ludford KT, Vagenas P, Lama JR, Peinado J, Gonzales P, Leiva R, et al. Screening for drug and alcohol use disorders and their association with HIV-related sexual risk behaviors among men who have sex with men in Peru. PLoS ONE. 2013;8(8):e69966. doi: 10.1371/journal.pone.0069966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vagenas P, Ludford KT, Gonzales P, Peinado J, Cabezas C, Gonzales F, et al. Being unaware of being HIV-infected is associated with alcohol use disorders and high-risk sexual behaviors among men who have sex with men in Peru. AIDS Behav. 2013 May 14; doi: 10.1007/s10461-013-0504-2. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Babor TF, de la Fuente JR, Saunders J. AUDIT: the Alcohol Use Disorders Identification Test: guidelines for use in primary health care. Geneva: World Health Organization; 1992. [Google Scholar]
- 9.Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA. 1984;252(14):1905–7. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- 10.Carlini-Marlatt B, Gazal-Carvalho C, Gouveia N, de Souza MF. Drinking practices and other health-related behaviors among adolescents of São Paulo City, Brazil. Subst Use Misuse. 2003;38(7):905–32. doi: 10.1081/ja-120017617. [DOI] [PubMed] [Google Scholar]
- 11.de Graaf R, Vanwesenbeeck I, van Zessen G, Straver CJ, Visser JH. Alcohol and drug use in heterosexual and homosexual prostitution, and its relation to protection behaviour. AIDS Care. 1995;7(1):35–47. doi: 10.1080/09540129550126948. [DOI] [PubMed] [Google Scholar]
- 12.Cortez FC, Boer DP, Baltieri DA. Psychosocial pathways to inconsistent condom use among male sex workers: personality, drug misuse and criminality. Sex Health. 2011;8(3):390–8. doi: 10.1071/SH10136. [DOI] [PubMed] [Google Scholar]
- 13.Bertoni N, Bastos FI, Mello MB, Makuch MY, Sousa MH, Osis MJ, et al. Uso de alcool e drogas e sua influencia sobre as praticas sexuais de adolescentes de Minas Gerais, Brasil. Cad Saude Publica. 2009;25(6):1350–60. doi: 10.1590/s0102-311x2009000600017. [DOI] [PubMed] [Google Scholar]
- 14.Bastos FI, Cunha CB, Bertoni N. Grupo de Estudos em População, Sexualidade e Aids. Uso de substâncias psicoativas e métodos contraceptivos pela população urbana brasileira, 2005. Rev Saude Publica. 2008;42 (Suppl 1):118–26. doi: 10.1590/s0034-89102008000800014. [DOI] [PubMed] [Google Scholar]
- 15.Bastos FI, Bertoni N, Hacker MA. Grupo de Estudos em População, Sexualidade e Aids. Consumo de alcool e drogas: principais achados de pesquisa de ambito nacional, Brasil 2005. Rev Saude Publica. 2008;42 (Suppl 1):109–17. doi: 10.1590/s0034-89102008000800013. [DOI] [PubMed] [Google Scholar]
- 16.de Codes JS, Cohen DA, de Melo NA, Teixeira GG, Leal Ados S, de Silva TJ, et al. Deteccao de doencas sexualmente transmissiveis em ambientes clinicos e nao clinicos na Cidade de Salvador, Bahia, Brasil. Cad Saude Publica. 2006;22(2):325–34. doi: 10.1590/s0102-311x2006000200010. [DOI] [PubMed] [Google Scholar]
- 17.Cook RL, May S, Harrison LH, Moreira RI, Ness RB, Batista S, et al. High prevalence of sexually transmitted diseases in young women seeking HIV testing in Rio de Janeiro, Brazil. Sex Transm Dis. 2004;31(1):67–72. doi: 10.1097/01.OLQ.0000105004.85419.17. [DOI] [PubMed] [Google Scholar]
- 18.Levinson RA, Sadigursky C, Erchak GM. The impact of cultural context on Brazilian adolescents’ sexual practices. Adolescence. 2004;39(154):203–27. [PubMed] [Google Scholar]
- 19.Malta M, Bastos FI, Pereira-Koller EM, Cunha MD, Marques C, Strathdee SA. A qualitative assessment of long distance truck drivers’ vulnerability to HIV/AIDS in Itajaí, southern Brazil. AIDS Care. 2006;18(5):489–96. doi: 10.1080/09540120500235241. [DOI] [PubMed] [Google Scholar]
- 20.de Santos AO, Paiva V. Vulnerabilidade ao HIV: turismo e uso de alcool e outras drogas. Rev Saude Publica. 2007;41 (Suppl 2):80–6. doi: 10.1590/s0034-89102007000900013. [DOI] [PubMed] [Google Scholar]
- 21.Cabada MM, Mozo K, Pantenburg B, Gotuzzo E. Excessive alcohol consumption increases risk taking behaviour in travellers to Cusco, Peru. Travel Med Infect Dis. 2011;9(2):75–81. doi: 10.1016/j.tmaid.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 22.Gálvez-Buccollini JA, Paz-Soldan V, Herrera P, DeLea S, Gilman RH, Anthony JC. Links between sex-related expectations about alcohol, heavy episodic drinking and sexual risk among young men in a shantytown in Lima, Peru. Int Fam Plan Perspect. 2008;34(1):15–20. doi: 10.1363/ifpp.34.015.08. [DOI] [PubMed] [Google Scholar]
- 23.Mancha BE, Rojas VC, Latimer WW. Alcohol use, alcohol problems, and problem behavior engagement among students at two schools in northern Mexico. Alcohol. 2012;46(7):695–701. doi: 10.1016/j.alcohol.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Campo-Arias A, Ceballo GA, Herazo E. Prevalence of pattern of risky behaviors for reproductive and sexual health among middle- and high-school students. Rev Lat Am Enfermagem. 2010;18(2):170–4. doi: 10.1590/s0104-11692010000200005. [DOI] [PubMed] [Google Scholar]
- 25.Baumgarten LZ, Gomes VLO, Fonseca AD. Consumo alcoólico entre universitários(as) da área da saúde da Universidade Federal do Rio Grande/RS: subsídios para enfermagem. Esc Anna Nery Rev Enferm. 2012;16(3):530–5. [Google Scholar]
- 26.Goldenberg SM, Strathdee SA, Gallardo M, Nguyen L, Lozada R, Semple SJ, et al. How important are venue-based HIV risks among male clients of female sex workers? A mixed methods analysis of the risk environment in nightlife venues in Tijuana, Mexico. Health Place. 2011;17(3):748–56. doi: 10.1016/j.healthplace.2011.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gálvez-Buccollini JA, Paz-Soldán VA, Herrera PM, DeLea S, Gilman RH. Gender differences in sex-related alcohol expectancies in young adults from a peri-urban area in Lima, Peru. Rev Panam Salud Publica. 2009;25(6):499–505. doi: 10.1590/s1020-49892009000600005. [DOI] [PubMed] [Google Scholar]
- 28.Herrán OF, Ardila MF. Tipologia de los consumidores de alcohol y sus factores determinantesen Bucaramanga, Colombia. Biomedica. 2009;29(4):635–46. [PubMed] [Google Scholar]
- 29.Gálvez-Buccollini JA, DeLea S, Herrera PM, Gilman RH, Paz-Soldan V. Sexual behavior and drug consumption among young adults in a shantytown in Lima, Peru. BMC Public Health. 2009;9:23. doi: 10.1186/1471-2458-9-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Freitas GV, Cais CF, Stefanello S, Botega NJ. Psychosocial conditions and suicidal behavior in pregnant teenagers: a case-control study in Brazil. Eur Child Adolesc Psychiatry. 2008;17(6):336–42. doi: 10.1007/s00787-007-0668-2. [DOI] [PubMed] [Google Scholar]
- 31.Sánchez-Alemán MA, Uribe-Salas F, Conde-González CJ. La infeccion por el virus del papiloma humano, un posible marcador biológico de comportamiento sexual en estudiantes universitarios. Salud Publica Mex. 2002;44(5):442–7. [PubMed] [Google Scholar]
- 32.Taquette SR, de Vilhena MM, de Paula MC. Doencas sexualmente transmissiveis na adolescencia: estudo de fatores de risco. Rev Soc Bras Med Trop. 2004;37(3):210–4. doi: 10.1590/s0037-86822004000300003. [DOI] [PubMed] [Google Scholar]
- 33.Bautista CT, Mosquera C, Serra M, Gianella A, Avila MM, Laguna-Torres V, et al. Immigration status and HIV-risk related behaviors among female sex workers in South America. AIDS Behav. 2008;12(2):195–201. doi: 10.1007/s10461-007-9270-3. [DOI] [PubMed] [Google Scholar]
- 34.Becher JC, Garcia JG, Kaplan DW, Gil AR, Li J, Main D, et al. Reproductive health risk behavior survey of Colombian high school students. J Adolesc Health. 1999;24(3):220–5. doi: 10.1016/s1054-139x(98)00084-6. [DOI] [PubMed] [Google Scholar]
- 35.Rasmussen-Cruz B, Hidalgo-San Martín A, Alfaro-Alfaro N. Comportamientos de riesgo de ITS/SIDA en adolescentes trabajadores de hoteles de Puerto Vallarta y su asociación con el ambiente laboral. Salud Publica Mex. 2003;45 (Suppl 1):S81–91. [PubMed] [Google Scholar]
- 36.Persaud NE, Klaskala W, Tewari T, Shultz J, Baum M. Drug use and syphilis. Co-factors for HIV transmission among commercial sex workers in Guyana. West Indian Med J. 1999;48(2):52–6. [PubMed] [Google Scholar]
- 37.Chincha LO, Samalvides CF, Bernabé-Ortiz A, Kruger PH, Gotuzzo HE. Asociacion entre el consumo de alcohol y la infeccion por virus de inmunodeficiencia humana. Rev Chilena Infectol. 2008;25(1):49–53. [PubMed] [Google Scholar]
- 38.Bassols AM, Boni R, Pechansky F. Alcohol, drugs, and risky sexual behavior are related to HIV infection in female adolescents. Rev Bras Psiquiatr. 2010;32(4):361–8. doi: 10.1590/s1516-44462010000400008. [DOI] [PubMed] [Google Scholar]
- 39.Munoz B, Pacheco ME, Aponte C, Michini A, Taibo ME, Pinto B, et al. Assessment of human immunodeficiency virus type 1 and risk practices among female commercial sex workers in Isla Margarita, Venezuela. Mil Med. 2006;171(1):1–6. doi: 10.7205/milmed.171.1.1. [DOI] [PubMed] [Google Scholar]
- 40.Mariño R, Minichiello V, Disogra C. Male sex workers in Córdoba, Argentina: sociodemographic characteristics and sex work experiences. Rev Panam Salud Publica. 2003;13(5):311–9. doi: 10.1590/s1020-49892003000400006. [DOI] [PubMed] [Google Scholar]
- 41.Herrán OF, Ardila MF, Barba DM. Consumo problemático de alcohol en Bucaramanga, Colombia: diseño y validación de una prueba. Biomedica. 2008;28(1):25–37. [PubMed] [Google Scholar]


