Abstract
In patients who underwent revision TKA from 1993–2005 and responded to follow-up questionnaires 2- or 5-years post-revision TKA, we studied whether body mass index (BMI), comorbidity (measured by validated Deyo-Charlson index), gender and age predict activity limitation 2- and 5-years after Revision TKA. Overall moderate-severe activity limitation was defined as ≥2 activities (walking, stairs, rising chair) with moderate-severe limitation. Multivariable logistic regressions also adjusted for income, diagnosis, distance from medical center and American Society of Anesthesiologists Physical Status (ASA) score. The prevalence of overall moderate-severe activity limitation was high: 46.5% (677/1,456) at 2-years and 50.5% (420/832) at 5-years post-revision TKA. At both 2- and 5-year follow-up, BMI≥40, higher Deyo-Charlson score, female gender and age>80, each significantly predicted higher odds of moderate-severe overall activity limitation.
Keywords: Revision Total Knee Arthroplasty, Activity Limitation, Functional limitation, predictors, body mass index, age, gender, comorbidity
INTRODUCTION
Revision Total Knee Arthroplasty (TKAR) is a common procedure –38,000 procedures were performed in 2003 in the U.S. (1), projected to increase 6-times to 268,000 by 2030 (1). TKAR is a far more expensive surgery than the primary TKA, with average charge of $73,696 per procedure (2, 3) and is associated with less predictable outcomes (4, 5). In a meta-analysis of 42 TKAR studies comprising 1,515 patients, 22% reported functional outcomes that were only satisfactory or poor (6). These suboptimal TKAR outcomes can have a significant impact on patient satisfaction, medical costs and health care utilization.
The 2003 National Institutes of Health’s consensus statement on TKA concluded that more research was needed to examine the impact of patient-level factors on TKA outcomes (7). A better understanding of prognostic factors for poor TKAR outcomes can inform patients and surgeons and help us target modifiable risk factors to improve TKAR outcomes. Most studies examining predictors of patient-reported outcomes have been performed in patients with primary TKA, with a paucity of studies in patients with TKAR. It is possible that predictors of outcomes may be different for TKAR compared to those for primary TKA. For example, while pre-operative function predicts function in patients with primary TKA (8–11), it was found not to be related to function in a meta-analysis of TKAR studies (6).
Very few studies assessing outcomes after TKAR have been published. As reported above, preoperative function is not associated with post-operative function after TKAR (6). Gender was not associated with function outcome in 67 TKARs at 2-year follow-up (12). Other TKAR studies did not report the predictors of outcomes (13, 14). Thus, very few published studies have examined predictors after TKAR. Most previous studies had small sample sizes and therefore limited power to examine predictors of poor functional outcomes. In this study, we examined the impact of Body Mass Index (BMI), comorbidity, gender and age on functional outcomes 2- and 5-years after TKAR.
METHODS
Data Sources and Study Population
The Mayo Clinic Total Joint registry has prospectively captured pain and function data from every patient who has undergone knee or hip arthroplasty at the Mayo Clinic since 1993. A validated Mayo Knee questionnaire (15) is mailed, administered during the clinic visit or by telephone at 2- and 5-year time-points to patients after the TKAR. The study cohort consisted of patients with TKAR between 1993 and 2005 (to allow for a 2-year follow-up) that responded to at least one of the questionnaires at 2- or 5-year follow-up.
Predictor Variables of Interest
The four predictors of interest in our study were BMI, comorbidity, gender and age. BMI was categorized into <25, 25–29.9, 30–34.9, 35–39.9, ≥40 (16). Due to small numbers in <18.5 category, <18.5 and 18.5–24.9 were collapsed into single category. Comorbidity was assessed using Deyo-Charlson index, a validated measure of comorbidity that has been used extensively in both medical and surgical populations (17). The Deyo-Charlson index consists of a weighted scale of 17 comorbidities (including cardiac, pulmonary, renal, hepatic disease, diabetes, cancer, HIV etc.), expressed as a summative score (18, 19). We categorized age into four categories based on an a priori clinical decision by an experienced orthopedic surgeon (D.L.), (≤60, 61–70, 71–80, >80), similar to previous studies (20, 21). The reference categories for our variables of interest were, BMI <25, male gender and age ≤60, respectively. Deyo-Charlson index was treated as a continuous measure.
Functional Outcomes
The main outcome of interest in our study was moderate-severe limitation of overall activity. Overall activity limitation was defined as moderate/severe, if a patient had ≥2 key activities of daily living (walking, stairs, rising chair) with moderate or severe limitation (reference, <2 limitations), to allow an easier interpretation of the study findings. In addition, we studied limitations of each of the three activities including distance walked, stair climbing and rising from chair and dependence of walking-aids. The limitations were classified a priori as follows: (1) Distance walked: ‘Unlimited’ or ‘> 10 blocks’ = None; ‘5–10 blocks ‘ = Mild; ‘< 5 blocks ‘=Moderate; ‘Housebound’, ‘Indoors only’ or ‘Unable’ = Severe; (2) Stairs: ‘Normal Up and Down’=None; ‘‘Normal Up, Down with Rail’ = Mild; ‘Up and Down with Rail’ = Moderate; ‘Up with Rail, Down Unable’ OR ‘Unable ‘ = Severe; and (3) Rise from Chair: ‘Able, no arms’ = None; ‘Able, with Arms’ = Mild; ‘Able with difficulty’ = Moderate; ‘ Unable ‘ = Severe.
The use of walking aids was categorized clinically as follows: ‘no aid’, ‘cane occasionally’ = no dependence; ‘cane full time’ = some dependence; ‘crutch’ ‘2 canes’, ‘2 crutches’, ‘walker’ or ‘unable to walk’ = complete dependence/unable.
We examined the association of predictors of interest with presence of moderate-severe limitation in overall activity, walking, climbing stairs, rising from chair and with some dependence on walking-aids or with complete dependence/unable (reference, no dependence for both).
Covariates/confounders
We obtained the underlying operative diagnosis from the Total Joint Registry and categorized as loosening/wear/osteolysis, dislocation/bone or prosthesis fracture/instability/ non-union or failed prior arthroplasty with components removed/infection for TKAR. We used other institutional research databases to obtain additional variables of interest, that were included in the multivariable regression analyses: (1) demographic: median annual household income (≤$35K, >$35K–$45K or >$45 K (reference category)) determined based on zip code and the median household income for geographical area using the census data for the respective year of survey; (2) American Society of Anesthesiologists Physical Status (ASA) score, a validated measure of peri- and post-operative outcomes, categorized as class I–II vs. III–IV (22, 23); and (3) distance from medical center (0–100 miles, >100–500 miles, >500 miles).
Statistical Analyses
Summary statistics (mean, standard deviation and percents) were calculated for cohort demographic and clinical characteristics. We performed all univariate and multivariable analyses using logistic regression with a generalized estimating equations (GEE) approach to adjust the standard errors for the correlation between observations on the same subject due to replacement of both knees and/or multiple operations on the same knee. The multivariable-adjusted regression analyses included the primary variables of interest (BMI, comorbidity, gender and age) and confounders (distance from medical center, income, underlying diagnosis and ASA score). Outcomes were moderate-severe limitation in overall activity and the three activities separately (walking, climbing, and rising from a chair).
We examined the association of BMI, comorbidity, age and gender with dependence on walking-aids at 2- and 5-years post-TKAR (some vs. no dependence and complete vs. no dependence) by using univariate and multivariable-adjusted polychotomous logistic regression analyses, using the same variables listed above. Odds ratios with 95% confidence intervals are presented. A p≤0.05 was considered significant.
Only the multivariable-adjusted results are discussed in results; detailed univariate and multivariable-adjusted associations are presented in the appendix for the interested readers. Responder bias was examined with logistic regression, assessing the associations of demographic and clinical characteristics with completion of a follow-up questionnaire at 2- and 5-years post-TKA.
RESULTS
Cohort Characteristics and Non-response Bias
Table 1 summarizes the baseline demographic and clinical characteristics of the TKAR cohort. The study population consisted of 1,533 TKARs at 2-years and 881 at 5-years after surgery. The cohorts had a mean age of 69 years and consisted of nearly equal proportions of men and women. Loosening, wear or osteolysis were the most common underlying indications for TKAR. The majority of patients (>85%) were overweight or obese, i.e., had BMI >25; 51% were above 70 years of age. The prevalence of overall moderate-severe overall activity limitation was high: 46.5% at 2-years and 50.5% at 5-years post-TKAR.
Table 1.
Demographic and clinical characteristics of study cohort
| Revision TKA | ||
|---|---|---|
|
| ||
| 2-year (n=1,533) | 5-year (n=881) | |
| Mean Age (±Standard Deviation) | 69±10 | 69±10 |
| Men/Women (% | 49%/51% | 51%/49% |
| Age groups n (%) | ||
| ≤60 yrs | 20% | 20% |
| 61–70 yrs | 29% | 31% |
| 71–80 yrs | 42% | 41% |
| >80 yrs | 9% | 8% |
| Body Mass index (in kg/m2) | ||
| ≤24.9 | 13% | 14% |
| 25–29.9 | 36% | 39% |
| 30–34.9 | 29% | 28% |
| 35–39.9 | 15% | 14% |
| ≥40 | 7% | 5% |
| American Society of Anesthesiologists Physical Status Score | ||
| Class I–II | 50% | 53% |
| Class III–IV | 50% | 47% |
| Underlying Diagnoses | ||
| Loosening/Wear or Osteolysis | 57% | 61% |
| Dislocation, Bone or Prosthesis Fracture, Instability, Non-Union | 22% | 20% |
| Failed Prior Arthroplasty with Components Removed or Infection* | 21% | 19% |
19% had an underlying diagnosis of failed prior arthroplasty with components removed at 2-years and 2% had the diagnosis of infection; Simialrly, among the 5-year cohort, 19% had failed prior arthroplasty with components removed and 2% infection as their underlying diagnosis
Of the 2,695 eligible TKAR patients, 1,533 (57%) completed a 2-year questionnaire. There were 1,842 patients eligible for 5-year follow-up and 881 (48%) completed a 5-year questionnaire. Non-responders were more likely than responders to have underlying diagnoses of failed arthroplasty with components removed or infection, had slightly higher comorbidity and were younger; other characteristics including gender, BMI, income category and distance from medical center were similar to the responders (Appendix 1).
Appendix 1.
Characteristics of Non-responders
| 2-yr Revision TKA | 5-yr Revision TKA | |||
|---|---|---|---|---|
|
| ||||
| Events for non-responders (1162/2695) | OR (95 % CI) | Events for non-responders (961/1842) | OR (95 % CI) | |
| Gender | ||||
| Women | 621/1402 (44.3%) | 509/944 (53.9%) | ||
| Men | 541/1293 (41.8%) | 1.10 (0.94, 1.29) | 452/898 (50.3%) | 0.87 (0.72,1.05) |
| Age groups n (%) | ||||
| ≤60 yrs | 283/587 (48.2%) | 241/413 (58.4%) | ||
| 61–70 yrs | 365/816 (44.7%) | 0.87 (0.70,1.08) | 281/555 (50.6%) | 0.73 (0.56,0.96) * |
| 71–80 yrs | 391/1034 (37.8%) | 0.65 (0.53,0.81) ‡ | 350/714 (49%) | 0.69 (0.53,0.89) ‡ |
| >80 yrs | 123/258 (47.7%) | 0.98 (0.72,1.32) | 89/160 (55.6%) | 0.89 (0.61,1.31) |
| BMI Categorized | ||||
| ≤25 | 172/375 (45.9%) | 136/258 (52.7%) | ||
| 25–29.9 | 375/925 (40.5%) | 0.80 (0.63,1.03) | 310/655 (47.3%) | 0.81 (0.60,1.09) |
| 30–39.9 | 485/1149 (42.2%) | 0.86 (0.68,1.09) | 423/784 (54%) | 1.05 (0.79,1.41) |
| ≥40 | 123/229 (53.7%) | 1.37 (0.98,1.91) | 89/136 (65.4%) | 1.70 (1.09,2.66) * |
| ASA | ||||
| 1–2 | 505/1270 (39.8%) | 1.29 (1.10,1.51) ‡ | 432/899 (48.1%) | 1.38 (1.15,1.66) ‡ |
| 3–4 | 651/1414 (46%) | 1.16 (0.93,1.44) | 523/933 (56.1%) | 1.63 (1.21,2.20) ‡ |
| Deyo-Charlson index (5 point increase) | ||||
| Income | ||||
| >$45K | 236/548 (43.1%) | 163/304 (53.6%) | ||
| ≤$35K | 254/595 (42.7%) | 1.98 (0.77,1.25) | 243/488 (49.8%) | 0.86 (0.64, 1.15) |
| >$35K–$45K | 450/1050 (42.9%) | 0.99 (0.80,1.23) | 363/677 (53.6%) | 1.00 (0.76,1.32) |
| Distance | ||||
| 0–100 miles | 390/865 (45.1%) | 284/571 (49.7%) | ||
| >100–500 miles | 602/1449 (41.5%) | 0.87 (0.72,1.03) | 535/993 (53.9%) | 1.18 (0.95, 1.46) |
| >500 miles or Non-US | 129/293 (44%) | 0.96 (0.73,1.27) | 103/200 (51.5%) | 1.07 (0.77, 1.50) |
| Underlying Diagnoses | ||||
| Loosening/Wear or Osteolysis | 584/1453 (40.2%) | 475/1015 (46.8%) | ||
| Dislocation, Bone or Prosthesis Fracture, Instability, Non-Union | 254/597 (42.5%) | 1.10 (0.91,1.34) | 216/393 (55%) | 1.39 (1.10,1.76) ‡ |
| Failed Prior Arthroplasty with Components Removed or Infection | 324/645 (50.2%) | 1.50 (1.24,1.82) ‡ | 270/434 (62.2%) | 1.87 (1.48,2.36) ‡ |
P<0.05;
p<0.01,
p<0.001
All other p-values are ≥0.05, unless indicated as above
Functional Outcomes 2-years after Revision TKA
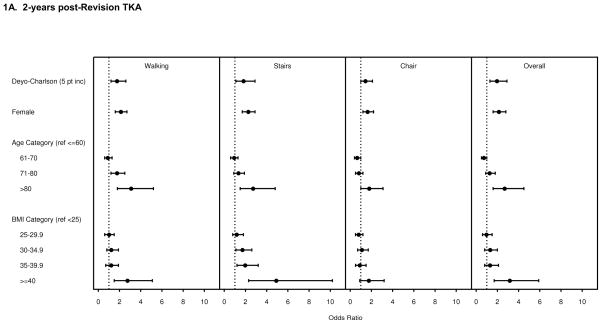
In multivariable analyses, the significant predictors of moderate-severe overall activity limitation and limitations in all three key activities (walking, stairs and rising from a chair) were: female gender and age >80 (relative to ≤60) (Figure 1A).
A higher comorbidity (Deyo-Charlson index) and BMI ≥40 (relative to <25) were associated with a moderate-severe limitation in walking, climbing stairs and overall activity, but not rising from a chair (Figure 1A). Age 71–80 (relative to ≤60) was associated with a moderate-severe limitation in walking, but not associated with moderate-severe limitation in climbing stairs, rising from a chair or in overall moderate-severe limitation. BMI 30–34.9 and 35–39.9 (each relative to BMI<25) were each associated with a moderate-severe limitation in climbing stairs only (Figure 1A).
Functional Outcomes 5-years after Revision TKA
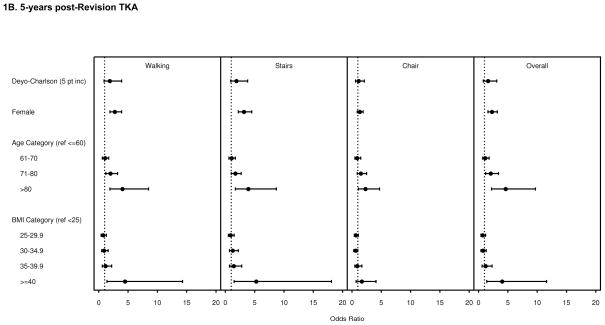
BMI ≥40 (relative to <25), age 71–80 and female gender were each associated with significantly higher odds of moderate-severe limitation in walking, stairs and overall activity, but not in chair-transfer (Figure 1B). Age >80 was associated with significantly higher odds of moderate-severe limitation in walking, stairs, chair-transfer and overall activity. Appendix 2–3 present univariate and multivariable odds ratios for all the results discussed above.
Appendix 2.
Association of BMI, comorbidity, age and gender with Moderate-Severe Limitations in Walking, Climbing Stairs, Rising from Chair and overall activity at 2-years post-Revision TKA
| Moderate-Severe Limitation in Walking (N=1477) | Moderate-Severe Limitation in Climbing Stairs (N=1498) | Moderate-Severe Limitation in Rising from Chair (N=1493) | Moderate-Severe Overall Activity Limitation (N=1456) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| Univariate | Multivariable | Univariate | Multivariable | Univariate | Multivariable | Univariate | Multivariable | ||||||
|
| |||||||||||||
| N | % | OR (95% CI) | OR (95% CI) | % | OR (95% CI) | OR (95% CI) | % | OR (95% CI) | OR (95% CI) | % | OR (95% CI) | OR (95% CI) | |
| BMI (kg/m2) | |||||||||||||
| <25 | 203 | 49.2 | 1.0 (ref.) | 1.0 (ref.) | 60.3 | 1.0 (ref.) | 1.0 (ref.) | 22.3 | 1.0 (ref.) | 1.0 (ref.) | 47.3 | 1.0 (ref.) | 1.0 (ref.) |
| 25–29.9 | 550 | 41.0 | 0.7 (0.5,1.01) | 1.0 (0.6,1.5) | 55.1 | 0.8 (0.6,1.1) | 1.2 (0.8,1.8) | 17.7 | 0.7 (0.5,1.1) | 0.8 (0.5,1.2) | 37.9 | 0.7* (0.5,0.97) | 1.0 (0.6,1.5) |
| 30–34.9 | 442 | 49.1 | 1.0 (0.7,1.4) | 1.2 (0.8,1.9) | 65.0 | 1.2 (0.9,1.8) | 1.7* (1.1,2.6) | 22.8 | 1.0 (0.7,1.5) | 1.1 (0.7,1.7) | 47.7 | 1.0 (0.7,1.4) | 1.3 (0.8,2.0) |
| 35–39.9 | 222 | 51.9 | 1.1 (0.7,1.7) | 1.2 (0.7,1.9) | 71.8 | 1.7* (1.1,2.6) | 2.0‡ (1.2,3.2) | 22.3 | 1.0 (0.6,1.6) | 0.9 (0.5,1.5) | 50.7 | 1.1 (0.8,1.7) | 1.3 (0.8,2.1) |
| ≥40 | 106 | 70.9 | 2.5‡ (1.5,4.2) | 2.7‡ (1.5,5.1) | 84.0 | 3.4‡ (1.9,6.4) | 4.9‡ (2.3,10.2) | 35.6 | 1.9‡ (1.1,3.2) | 1.7 (0.9,3.2) | 72.1 | 2.9‡ (1.7,4.9) | 3.2‡ (1.7,5.9) |
| missing | 10 | ||||||||||||
| Deyo-Charlson index (/5-pts) | 1531 | n/a | 1.8‡ (1.2,2.5) | 1.7‡ (1.2,2.6) | n/a | 1.9‡ (1.3,2.8) | 1.8‡ (1.1,2.9) | n/a | 1.5* (1.1,2.2) | 1.4 (0.95,2.1) | n/a | 1.8‡ (1.5,2.3) | 1.9‡ (1.3,2.9) |
| missing | 2 | ||||||||||||
| Gender | |||||||||||||
| Male | 752 | 40.0 | 1.0 (ref.) | 1.0 (ref.) | 54.8 | 1.0 (ref.) | 1.0 (ref.) | 18.1 | 1.0 (ref.) | 1.0 (ref.) | 38.2 | 1.0 (ref.) | 1.0 (ref.) |
| Female | 781 | 56.2 | 1.9‡ (1.6,2.4) | 2.1‡ (1.6,2.7) | 71.7 | 2.1‡ (1.7,2.6) | 2.2‡ (1.7,2.9) | 25.4 | 1.5‡ (1.2,2.0) | 1.6‡ (1.2,2.2) | 54.6 | 1.9‡ (1.6,2.4) | 2.1‡ (1.6,2.8) |
| Age (years) | |||||||||||||
| ≤60 | 304 | 44.7 | 1.0 (ref.) | 1.0 (ref.) | 60.8 | 1.0 (ref.) | 1.0 (ref.) | 23.3 | 1.0 (ref.) | 1.0 (ref.) | 46.5 | 1.0 (ref.) | 1.0 (ref.) |
| 61–70 | 451 | 38.9 | 0.8 (0.6,1.1) | 0.9 (0.6,1.3) | 57.9 | 0.9 (0.6,1.2) | 0.9 (0.6,1.3) | 18.1 | 0.7 (0.5,1.1) | 0.6* (0.4,0.97) | 37.4 | 0.7* (0.5,0.9) | 0.7 (0.5,1.05) |
| 71–80 | 643 | 52.7 | 1.4 * (1.02,1.9) | 1.7‡ (1.2,2.5) | 65.4 | 1.2 (0.9,1.6) | 1.3 (0.9,1.9) | 20.8 | 0.9 (0.6,1.2) | 0.8 (0.5,1.2) | 48.9 | 1.1 (0.8,1.5) | 1.2 (0.9,1.8) |
| >80 | 135 | 66.2 | 2.4‡ (1.5,3.8) | 3.1‡ (1.8,5.2) | 77.4 | 2.2‡ (1.4,3.6) | 2.7‡ (1.5,4.8) | 35.7 | 1.8‡ (1.1,2.9) | 1.8* (1.02,3.1) | 65.4 | 2.2‡ (1.4,3.4) | 2.7‡ (1.6,4.5) |
P<0.05;
p≤0.01,
p<0.001;
All other p-values are ≥0.05, unless indicated as above; Significant odds ratios are in bold
Multivariable model adjusted for: gender, age, Deyo-Charlson index, BMI, ASA score, distance from medical center, operative diagnosis, income category
Appendix 3.
Odds of Moderate-Severe Limitations in Walking, Climbing Stairs, Rising from Chair and Overall Activity at 5-years post-Revision TKA
| Moderate-Severe Limitation in Walking (N=839) | Moderate-Severe Limitation in Climbing Stairs (N=853) | Moderate-Severe Limitation in Rising from Chair (N=847) | Moderate-Severe Overall Activity Limitation (N=832) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| Univariate | Multivariable | Univariate | Multivariable | Univariate | Multivariable | Univariate | Multivariable | ||||||
| N | % | OR (95% CI) | OR (95% CI) | % | OR (95% CI) | OR (95% CI) | % | OR (95% CI) | OR (95% CI) | % | OR (95% CI) | OR (95% CI) | |
| BMI (kg/m2) | |||||||||||||
| <25) | 122 | 52.1 | 1.0 (ref.) | 1.0 (ref.) | 63.9 | 1.0 (ref.) | 1.0 (ref.) | 28.0 | 1.0 (ref.) | 1.0 (ref.) | 50.0 | 1.0 (ref.) | 1.0 (ref.) |
| 25–29.9 | 345 | 46.6 | 0.8 (0.5,1.2) | 0.7 (0.4,1.3) | 60.2 | 0.9 (0.6,1.3) | 0.9 (0.5,1.5) | 23.4 | 0.8 (0.5,1.3) | 0.6 (0.4,1.1) | 44.5 | 0.8 (0.5,1.2) | 0.7 (0.4,1.2) |
| 30–34.9 | 242 | 51.9 | 1.0 (0.6,1.6) | 0.9 (0.5,1.6) | 67.0 | 1.1 (0.7,1.8) | 1.2 (0.7,2.2) | 21.5 | 0.7 (0.4,1.2) | 0.6 (0.3,1.0) | 47.0 | 0.9 (0.6,1.4) | 0.7 (0.4,1.3) |
| 35–39.9 | 119 | 63.7 | 1.6 (0.9,2.8) | 1.1 (0.6,2.2) | 76.9 | 1.9* (1.1,3.4) | 1.4 (0.7,2.8) | 29.3 | 1.1 (0.6,1.9) | 0.9 (0.5,1.7) | 62.6 | 1.7 (0.99,2.8) | 1.2 (0.6,2.3) |
| ≥40 | 47 | 84.4 | 5.0‡ (2.1,12.0) | 4.4‡ (1.4,14.3) | 87.2 | 3.9 ‡ (1.5,9.8) | 5.2 ‡ (1.5,18.1) | 39.1 | 1.7 (0.8,3.5) | 1.6 (0.7,4.1) | 80.0 | 4.0‡ (1.8,9.0) | 4.0 ‡ (1.4,11.6) |
| missing | 6 | ||||||||||||
| Deyo-Charlson index (/5-pts) | 880 | n/a | 2.0* (1.1,3.7) | 1.8 (0.9,3.9) | n/a | 1.9* (1.02,3.4) | 1.8 (0.9,3.8) | n/a | 1.6 (0.9,2.7) | 1.1 (0.6,2.1) | n/a | 1.6 (0.96,2.8) | 1.6 (0.8,3.1) |
| Missing | 1 | ||||||||||||
| Gender | |||||||||||||
| Male | 446 | 41.8 | 1.0 (ref.) | 1.0 (ref.) | 55.7 | 1.0 (ref.) | 1.0 (ref.) | 22.6 | 1.0 (ref.) | 1.0 (ref.) | 40.2 | 1.0 (ref.) | 1.0 (ref.) |
| Female | 435 | 64.9 | 2.6 ‡ (1.9,3.4) | 2.7 ‡ (1.9,3.9) | 77.4 | 2.7 ‡ (2.0,3.7) | 3.1 ‡ (2.2,4.5) | 27.8 | 1.3 (0.95,1.8) | 1.3 (0.9,1.9) | 60.9 | 2.3 ‡ (1.7,3.1) | 2.3 ‡ (1.6,3.2) |
| Age (years) | |||||||||||||
| ≤60 | 172 | 45.5 | 1.0 (ref.) | 1.0 (ref.) | 59.0 | 1.0 (ref.) | 1.0 (ref.) | 17.6 | 1.0 (ref.) | 1.0 (ref.) | 41.1 | 1.0 (ref.) | 1.0 (ref.) |
| 61–70 | 274 | 48.9 | 1.1 (0.8,1.7) | 1.0 (0.6,1.7) | 61.6 | 1.1 (0.7,1.7) | 1.0 (0.6,1.7) | 21.3 | 1.3 (0.8,2.1) | 0.8 (0.5,1.5) | 45.1 | 1.2 (0.8,1.8) | 1.1 (0.7,1.8) |
| 71–80 | 364 | 57.0 | 1.6 * (1.1,2.4) | 2.0‡ (1.2,3.2) | 70.2 | 1.6 * (1.1,2.4) | 1.7 * (1.03,2.7) | 29.6 | 2.0 ‡ (1.2,3.1) | 1.5 (0.9,2.5) | 55.2 | 1.8 ‡ (1.2,2.6) | 2.0 ‡ (1.2,3.4) |
| >80 | 71 | 71.9 | 3.1 ‡ (1.6,5.8) | 4.0‡ (1. 9,8.5) | 84.3 | 3.7 ‡ (1.8,7.7) | 3.9 ‡ (1.7,8.7) | 35.7 | 2.6 ‡ (1.4,5.0) | 2.3 * (1.1,4.7) | 71.2 | 3.5 ‡ (1.9,6.7) | 4.6 ‡ (2.2,9.7) |
P<0.05;
p≤0.01,
p≤0.001;
All other p-values are ≥0.05, unless indicated as above; Significant odds ratios are in bold
Multivariable model adjusted for: gender, age, Deyo-Charlson index, BMI, ASA score, distance from medical center, income category, underlying
diagnosis
Use of Walking Aids
At 2-years and 5-years, respectively, the significant predictors of complete dependence (reference, no dependence) on walking aids were: BMI, 25–29.9 (relative to <25), odd ratios (95% CI), 0.5 (0.3,0.9) at 2-years and 0.5 (0.2, 0.96) at 5-years; higher Deyo-Charlson score, 1.7 (1.0,2.7) and 2.3 (1.1,4.9); female gender, 2.5 (1.7,3.9) and 2.3 (1.4,3.7); age>80, 5.3 (2.7,10.5) and 4.7 (2.1,10.8). BMI≥40, age 61–70 and 71–80 were associated with significantly higher odd ratios (95% CI) of some dependence at 2-years, 2.8 (1.1, 6.8), 2.6 (1.1,5.8) and 3.5 (1.6,7.7), respectively, but not with complete dependence (Appendix 4).
Appendix 4.
Association of BMI, comorbidity, gender and age with some or complete dependence on walking aids
| 2--year Revision TKA | 5-year Revision TKA | |||
|---|---|---|---|---|
|
| ||||
| Some dependence | Complete Dependence/unable | Some dependence | Complete Dependence/unable | |
| BMI (Ref, <25 kg/m2) | ||||
| 25–29.9 | 0.9 (0.4,1.8) | 0.5 ‡ (0.3,0.9) | 0.8 (0.3,2.1) | 0.5 * (0.2,0.96) |
| 30–34.9 | 0.9 (0.4,1.9) | 0.6 (0.3,1.1) | 0.8 (0.3,2.1) | 0.6 (0.3,1.3) |
| 35–39.9 | 1.6 (0.7,3.5) | 0.8 (0.4,1.5) | 1.6 (0.6,4.2) | 1.0 (0.4,2.1) |
| ≥40 | 2.8 * (1.1,6.8) | 1.5 (0.7,3.3) | 1.3 (0.3,5.8) | 2.6 (1.00,7.0) |
| Deyo-Charlson index (5-point change) | 1.1 (0.6,2.0) | 1.7 * (1.00,2.7) | 2.3 (0.97,5.6) | 2.3 * (1.1,4.9) |
| Female Gender (Ref, Male) | 1.5 (1.0,2.4) | 2.5 † (1.7,3.9) | 2.0 * (1.1,3.6) | 2.3 † (1.4,3.7) |
| Age (Ref, ≤60 yrs) | ||||
| 61–70 | 2.6 * (1.1,5.8) | 0.7 (0.4,1.4) | 1.0 (0.4,2.4) | 0.7 (0.3,1.4) |
| 71–80 | 3.5 ‡ (1.6,7.7) | 1.4 (0.8,2.4) | 1.7 (0.7,3.9) | 1.2 (0.6,2.3) |
| >80 | 6.0 † (2.3,15.7) | 5.3 ‡ (2.7,10.5) | 1.5 (0.4,5.6) | 4.7 † (2.1,10.8) |
P<0.05;
p≤0.01,
p≤0.001;
All other p-values are ≥0.05, unless indicated as above; Significant odds ratios are in bold
In addition to the variable reported in the Appendix, the multivariable model includes ASA score, distance from medical center, operative diagnosis, income category and type of implant (in case of primary TKAs only),
DISCUSSION
Our study found that BMI, female gender and older age significantly impact activity outcomes after TKAR at 2-years. BMI, female gender, older age and comorbidity impact 5-year activity outcomes and dependence on walking-aids 2- and 5-years after TKAR. Almost half of the TKAR patients reported moderate-severe activity limitation (limitation of ≥2 key activities).
Strengths and Limitations
Study strengths include analysis of a large cohort of TKARs, adjustment for multiple covariates (socio-demographic, clinical and implant factors) and inclusion of 2- and 5-year follow-up. Analyses were not adjusted for pre-operative function, based on findings from a recent meta-analysis that it does not predict post-TKAR functional outcomes (6), and since this would have reduced the generalizability of our findings due to a greater non-response bias. There are several limitations to our study. Potential non-response bias may have affected our estimates. For example, higher comorbidity among the non-responders would bias our results towards null (non-significance), but the younger age of non-responders would bias our results away from the null (make non-significant results significant). Therefore the exact direction of bias is unclear. A prospective multi-center cohort is needed to avoid many study limitations, including controlling for additional potential confounders such as psychological state, social support and pre-operative function. Such a study can also provide data on longer-term outcomes.
Many findings in this study merit further discussion. First, the association of BMI ≥40, but not other categories (30–34.9 and 35–39.9), with more activity limitation and more dependence on walking-aids at both 2- and 5-years is a significant finding of this study. The increase in odds was 2.5–5 times, which is very significant clinically. In absence of any prior studies of the relationship of these BMI categories to TKAR function outcomes, comparisons are not possible. This finding was surprising and rejected our hypothesis that all BMI categories above 25 would be associated with more activity limitation. Surgeons should consider discussing weight-loss strategies with patients with BMI ≥40 before TKAR. Studies of impact of weight-loss prior to or after TKAR in those with BMI ≥40 to post-TKAR functional outcomes can help us determine the best strategy to improve outcomes in TKAR patients with BMI ≥40.
Second, the association of higher comorbidity with more activity limitation at 2-years, but not 5-years post-TKAR is very interesting. Higher comorbidity was also associated with complete dependence on walking-aids at 2- and 5-years post-TKAR. It remains to be seen whether an optimization of treatment of other medical conditions prior to and following TKAR can improve the functional outcomes after TKAR.
Third, the association of older age and female gender with more activity limitation and greater walking-aid dependence 2- and 5-years post-TKAR adds to the literature. The odds were higher by 2–4 times in most outcomes. This implies that women and patients >80 years should be counseled pre-operatively that their risk of moderate-severe activity limitation is much higher than their male and younger counterparts.
In summary, we found that very high BMI, higher comorbidity, female gender and older age each predicted more severe activity limitation and more dependence on walking-aids in TKAR patients at 2- and 5-year follow-up. Interventions in patients with very high BMI and higher comorbidity may improve functional and activity outcomes after TKAR.
Figure 1.
Multivariable-adjusted Odds ratio (95% confidence interval) for Moderate-Severe Limitations in Walking, Climbing Stairs, Rising from Chair and Moderate-Severe Overall Activity limitation at 2-years post-Revision TKA (1A) and at 5-years post-Revision TKA (1B)
Acknowledgments
Grant support: NIH CTSA Award 1 KL2 RR024151-01 (Mayo Clinic Center for Clinical and Translational Research) and the Department of Orthopedic Surgery, Mayo Clinic School of Medicine, Rochester, MN.
Footnotes
Financial Conflict: One of the authors (DL) has received royalties/speaker fees from Zimmer, has been a paid consultant to Zimmer and has received institutional research funds from DePuy, Stryker and Zimmer.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007 Apr;89(4):780–5. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Lavernia C, Lee DJ, Hernandez VH. The increasing financial burden of knee revision surgery in the United States. Clin Orthop Relat Res. 2006 May;446:221–6. doi: 10.1097/01.blo.0000214424.67453.9a. [DOI] [PubMed] [Google Scholar]
- 3.Lavernia CJ, Drakeford MK, Tsao AK, Gittelsohn A, Krackow KA, Hungerford DS. Revision and primary hip and knee arthroplasty. A cost analysis. Clin Orthop Relat Res. 1995 Feb;(311):136–41. [PubMed] [Google Scholar]
- 4.Hanssen AD, Rand JA. A comparison of primary and revision total knee arthroplasty using the kinematic stabilizer prosthesis. J Bone Joint Surg Am. 1988 Apr;70(4):491–9. [PubMed] [Google Scholar]
- 5.Saleh KJ, Mulhall KJ. Revision total knee arthroplasty: editorial comment. Clin Orthop Relat Res. 2006 May;446:2–3. doi: 10.1097/01.blo.0000214432.26657.92. [DOI] [PubMed] [Google Scholar]
- 6.Saleh KJ, Dykes DC, Tweedie RL, Mohamed K, Ravichandran A, Saleh RM, et al. Functional outcome after total knee arthroplasty revision: a meta-analysis. J Arthroplasty. 2002 Dec;17(8):967–77. doi: 10.1054/arth.2002.35823. [DOI] [PubMed] [Google Scholar]
- 7.NIH Consensus Statement on total knee replacement December 8–10, 2003. J Bone Joint Surg Am. 2004 Jun;86-A(6):1328–35. doi: 10.2106/00004623-200406000-00031. [DOI] [PubMed] [Google Scholar]
- 8.Fitzgerald JD, Orav EJ, Lee TH, Marcantonio ER, Poss R, Goldman L, et al. Patient quality of life during the 12 months following joint replacement surgery. Arthritis Rheum. 2004 Feb 15;51(1):100–9. doi: 10.1002/art.20090. [DOI] [PubMed] [Google Scholar]
- 9.Fortin PR, Clarke AE, Joseph L, Liang MH, Tanzer M, Ferland D, et al. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999 Aug;42(8):1722–8. doi: 10.1002/1529-0131(199908)42:8<1722::AID-ANR22>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 10.Jones CA, Voaklander DC, Johnston DW, Suarez-Almazor ME. The effect of age on pain, function, and quality of life after total hip and knee arthroplasty. Arch Intern Med. 2001 Feb 12;161(3):454–60. doi: 10.1001/archinte.161.3.454. [DOI] [PubMed] [Google Scholar]
- 11.Lingard EA, Katz JN, Wright EA, Sledge CB. Predicting the outcome of total knee arthroplasty. J Bone Joint Surg Am. 2004 Oct;86-A(10):2179–86. doi: 10.2106/00004623-200410000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Pun SY, Ries MD. Effect of gender and preoperative diagnosis on results of revision total knee arthroplasty. Clin Orthop Relat Res. 2008 Nov;466(11):2701–5. doi: 10.1007/s11999-008-0451-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deehan DJ, Murray JD, Birdsall PD, Pinder IM. Quality of life after knee revision arthroplasty. Acta Orthop. 2006 Oct;77(5):761–6. doi: 10.1080/17453670610012953. [DOI] [PubMed] [Google Scholar]
- 14.Fehring TK, Odum S, Griffin WL, Mason JB. Outcome comparison of partial and full component revision TKA. Clin Orthop Relat Res. 2005 Nov;440:131–4. doi: 10.1097/01.blo.0000186560.70566.dc. [DOI] [PubMed] [Google Scholar]
- 15.McGrory BJ, Morrey BF, Rand JA, Ilstrup DM. Correlation of patient questionnaire responses and physician history in grading clinical outcome following hip and knee arthroplasty. A prospective study of 201 joint arthroplasties. J Arthroplasty. 1996 Jan;11(1):47–57. doi: 10.1016/s0883-5403(96)80160-4. [DOI] [PubMed] [Google Scholar]
- 16.WHO. Obesity: preventing and managing the global epidemic. Geneva: World Health Organization; 2000. [PubMed] [Google Scholar]
- 17.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992 Jun;45(6):613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 18.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 19.Charlson ME, Sax FL, MacKenzie CR, Braham RL, Fields SD, Douglas RG., Jr Morbidity during hospitalization: can we predict it? J Chronic Dis. 1987;40(7):705–12. doi: 10.1016/0021-9681(87)90107-x. [DOI] [PubMed] [Google Scholar]
- 20.Bourne R, Mukhi S, Zhu N, Keresteci M, Marin M. Role of obesity on the risk for total hip or knee arthroplasty. Clin Orthop Relat Res. 2007 Dec;465:185–8. doi: 10.1097/BLO.0b013e3181576035. [DOI] [PubMed] [Google Scholar]
- 21.Singh JA, Gabriel S, Lewallen D. The impact of gender, age, and preoperative pain severity on pain after TKA. Clin Orthop Relat Res. 2008 Nov;466(11):2717–23. doi: 10.1007/s11999-008-0399-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dripps RD, Lamont A, Eckenhoff JE. The role of anesthesia in surgical mortality. JAMA. 1961 Oct 21;178:261–6. doi: 10.1001/jama.1961.03040420001001. [DOI] [PubMed] [Google Scholar]
- 23.Weaver F, Hynes D, Hopkinson W, Wixson R, Khuri S, Daley J, et al. Preoperative risks and outcomes of hip and knee arthroplasty in the Veterans Health Administration. J Arthroplasty. 2003 Sep;18(6):693–708. doi: 10.1016/s0883-5403(03)00259-6. [DOI] [PubMed] [Google Scholar]