Abstract
Purpose
To report masked superior oblique tightness as a possible mechanism causing A-pattern exotropia with intorsion following inferior rectus recession in the context of thyroid eye disease.
Methods
Three patients with thyroid eye disease and involvement of the superior oblique muscle are presented, along with a fourth comparison case without superior oblique involvement. Intraoperative torsion assessment and exaggerated traction testing were performed after detachment of the involved rectus muscles. A surgical procedure involving recession of tight superior oblique(s) when recessing inferior rectus muscle(s) is presented, along with surgical results.
Results
The first case illustrated the problem of A-pattern exotropia and intorsion following inferior rectus muscle recessions and subsequent treatment with superior oblique tendon recessions. Patients 2 and 3 demonstrated signs of coexisting inferior rectus involvement and superior oblique involvement both preoperatively and intraoperatively, with a tight superior oblique muscle and marked intorsion, suggesting the need for superior oblique tendon recession at the time of inferior rectus recession. Postoperatively there was no symptomatic intorsion or A-pattern exotropia and both patients were heterophoric distance and near with only rare diplopia. The fourth case, without superior oblique involvement, illustrated management with inferior rectus muscle recessions alone.
Conclusions
Superior oblique involvement may be masked by coexistent inferior rectus involvement and if not identified and addressed at the time of the first surgery may result in symptomatic intorsion and A-pattern exotropia. The clinical finding of minimal extorsion, or frank intorsion, in the presence of a tight inferior rectus muscle, may be an important sign of masked superior oblique tightness. Intraoperative assessment of torsion and superior oblique tension may also help identify patients at risk. Superior oblique tendon recession, at the time of inferior rectus muscle recession, prevented development of a postoperative A-pattern exotropia and intorsion.
A-pattern exotropia with intorsion may develop following inferior rectus recession in the context of thyroid eye disease1–5 and has previously been thought to be caused by the secondary effects of inferior rectus weakening, which in turn results in superior oblique overaction.3,5 In contrast, based on our recent clinical experience, we speculated that A-pattern exotropia and intorsion may, be due to masked superior oblique tightness in some cases. The purpose of this study is to present case examples of A-pattern exotropia and intorsion due to masked superior oblique tightness in thyroid eye disease, to review the results of preoperative and intra-operative testing designed to detect the condition, and to present the results of surgery based on these findings.
Patients and Methods
Mayo Clinic Institutional Review Board approval was obtained and all data were collected in a manner compliant with the Health Insurance Portability and Accountability Act.
Patient 1
A 50-year-old woman presented with constant diplopia following bilateral orbital decompression surgery for thyroid eye disease. Her primary position deviation at distance fixation measured 50Δ of esotropia and 10Δ of left hypotropia by prism and alternate cover test (PACT). Double Maddox rod testing showed 3° of extorsion. On synoptophore evaluation, torsion correction was not needed to achieve fusion, and torsion fusional amplitudes were balanced (12° extorsion to 14° intorsion). On ocular motility assessment there were bilateral, symmetric limitations of abduction in each eye and bilateral limitations of elevation (in both adduction and abduction). Intraoperatively both medial rectus muscles and both inferior rectus muscles were tight on forced duction testing. Using the relaxed muscle technique6 for judging the optimum initial position of the tight rectus muscles, we recessed both medial rectus muscle 5 mm and both inferior rectus muscles 7 mm. The inferior rectus muscles were also nasally transposed 7 mm with the aim of reducing an expected exotropia in downgaze and reading position with such large inferior rectus recessions.5 Scleral bites were taken at the insertion in this case. Adjustable sutures were used on all muscles and nonabsorbable polyester sutures were used on the inferior rectus muscles to reduce the risk of late overcorrection. Postoperative adjustment required advancing each inferior rectus muscle 2 mm and recessing each medial rectus muscle 3 mm.
Postoperatively, the patient developed an A-pattern exotropia measuring 14Δ in primary by PACT and 25Δ in downgaze, with 13° of intorsion in primary position and 18° in downgaze, so further surgery was planned. As described by Del Monte,5 each inferior oblique muscle was advanced underneath the belly of the lateral rectus muscle and reattached 2 mm above its superior border, 8 mm behind the lateral rectus muscle insertion. Nevertheless, postoperatively the intorsion recurred to 15° and the exodeviation recurred, measuring 20Δ by PACT in primary position and 30Δ in downgaze. The patient continued to be troubled by diplopia and further surgery was scheduled.
At the start of the third surgical procedure, routine forced duction testing revealed a slightly tight left superior rectus muscle but no tightness of other rectus muscles. Exaggerated traction testing of the oblique muscles7 revealed that both superior oblique muscles were tight and both inferior oblique muscles were also tight. Both superior oblique tendons were recessed 12 mm and hung back from a scleral bite at the anterior pole of the original insertion and a scleral bite 3 mm more posterior. The left superior rectus muscle was also recessed 3 mm. In addition, both medial rectus muscles were advanced 4 mm to address the primary position exotropia. Adjustable sutures were used for all muscles, but no adjustment of the vertical or torsional components was required.
Postoperatively, diplopia was much improved, with collapse of the A pattern and no symptomatic torsion. Twenty-two months postoperatively, the patient has been stable with orthophoria at distance in primary position, 2Δ right hyperphoria, 2Δ exophoria in upgaze and 2Δ right hyperphoria in downgaze. There was a 6Δ exophoria, 2Δ right hyperphoria at near and 2Δ vertical prism was prescribed to improve symptoms of occasional vertical diplopia. Measurements with double Maddox rods at 22 months confirmed stability of the torsional correction revealing 1° of extorsion. Our experience with this case influenced our management of the following 2 cases.
Patient 2
A 61-year-old woman with thyroid eye disease presented with one and a half years of increasing diplopia. There had been no previous decompression surgery. PACT in the primary position showed 35Δ of left hypotropia with 12Δ of esotropia at distance and 30Δ hypotropia with 6Δ esotropia at near (Figure 1A). There was 12Δ of esotropia by PACT in both up- and downgaze. Elevation of the left eye was limited, slightly more in adduction than in abduction, and there were mild limitations of abduction in both eyes (Figure 1A). Double Maddox rod testing showed 4° of extorsion in primary position, which we speculated was less than would be expected in the presence of an isolated, very tight inferior rectus muscle.
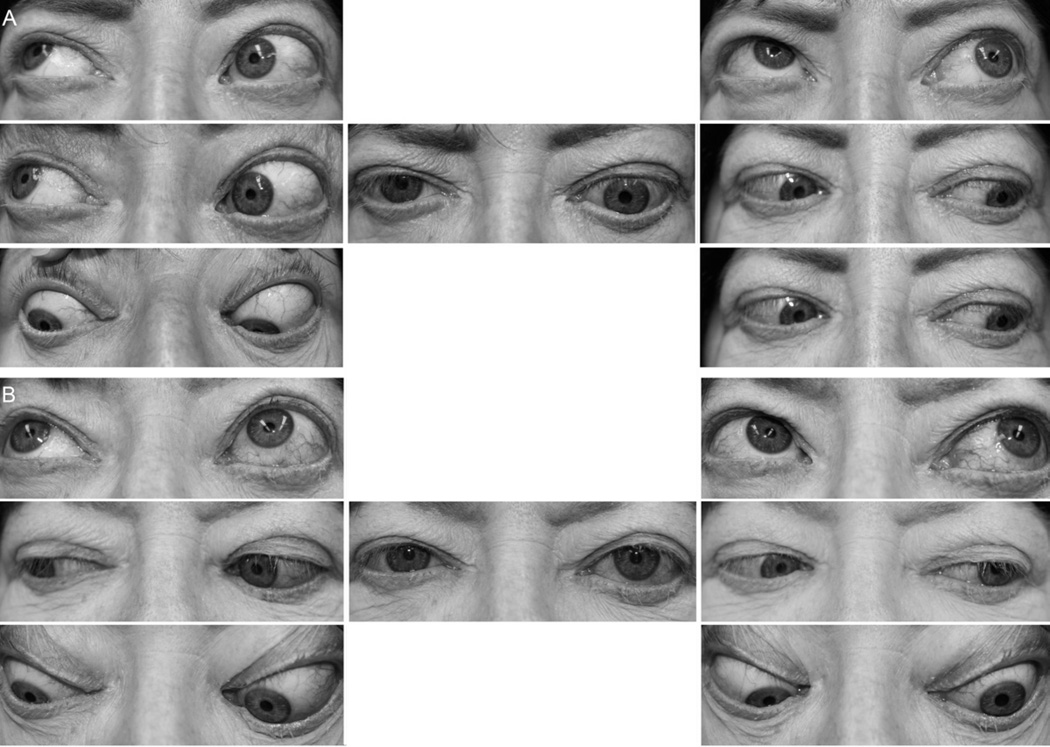
FIG 1.
Patient 2, showing ocular motility preoperatively (A) and 7 weeks postoperatively (B). The preoperative primary position deviation measured 35Δ left hypotropia with 12Δ esotropia at distance by prism and alternate cover test. Left eye elevation was limited, slightly more in adduction than abduction. Postoperatively primary position deviation measured 2Δ esophoria (4Δ esophoria in upgaze, 2Δ esophoria in downgaze) by prism and alternate cover test, with normal elevation of the left eye.
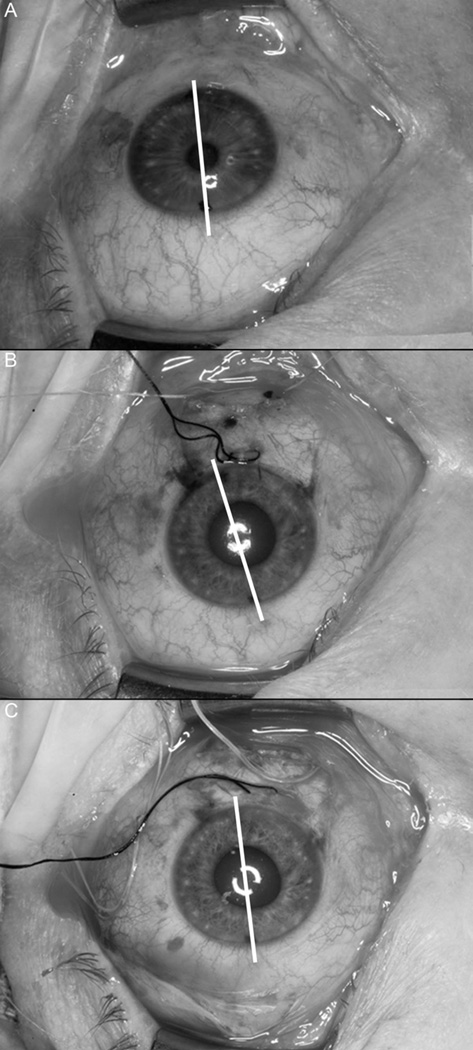
Intraoperatively, forced duction testing revealed a very tight left inferior rectus muscle but no tightness of other rectus muscles in either eye. Exaggerated traction testing of the oblique muscles7 suggested a tight left superior oblique muscle, but it was felt that this test result may have been confounded by the tight inferior rectus muscle. The inferior rectus muscle was therefore isolated, imbricated with a 6-0 nonabsorbable polyester suture and disinserted. On disinsertion of the inferior rectus muscle, marked intorsion of the left eye was noted when inspecting the position of limbal dots preplaced at 12 and 6 using a skin marking pen (Figure 2A and 2B).8 Forced duction testing was then repeated and elevation found to be markedly improved in abduction but only minimally improved in adduction. Repeating the exaggerated traction test revealed a markedly tight superior oblique muscle. TΔhe superior oblique tendon was therefore recessed 15 mm on an adjustable hang back suture taking scleral bites at the anterior pole of the original insertion and 3 mm more posterior. Using the relaxed muscle technique6 for judging the optimum initial position of the inferior rectus muscle, it was recessed 7.5 mm on an adjustable polyester suture. The muscle was also simultaneously nasally transposed 5 mm in an attempt to reduce any consecutive exotropia in downgaze. Scleral bites were taken 2 mm back from the insertion to reduce the amount of hang back that might have reduced the transposition effect. Forced duction and exaggerated traction tests were repeated and found to be normalized and inspection of the preplaced limbal dots showed they had returned to their original 12 and 6 o’clock orientation (Figure 2C), confirming the intorsion had been addressed by recessing the superior oblique tendon. Postoperative adjustment required advancement of the inferior rectus 1 mm.
FIG 2.
Patient 2, showing intraoperative monitoring of changes in ocular torsion by monitoring of preplaced limbal dots. Lines joining the blue dots are drawn on the figures to aid identification in these photographs. A, limbal dots at 12 and 6 o’clock at the commencement of the procedure. B, following inferior rectus muscle detachment the left eye shows marked intorsion. C, following left superior oblique recession, the torsion of the left eye returned to baseline.
Seven weeks postoperatively the patient reported a 90% improvement in diplopia and was orthotropic, with 2Δ of esophoria by PACT in primary position at distance (4Δ esophoria in upgaze, 2Δ esophoria in downgaze [Figure 1B]) and 2Δ of exophoria with 1Δ of left hyperphoria at near. Double Maddox rod testing showed 1° of intorsion. Elevation was greatly improved compared with preoperatively (Figure 1B). One year following surgery, she reported no diplopia in all positions of gaze and was orthotropic with 8Δ esophoria and 1Δ left hypotropia in primary position at distance (8Δ esophoria in upgaze, 6Δ esophoria in downgaze) and 2Δ exophoria with 1Δ left hyperphoria at near. There was 2° of extorsion on double Maddox rod testing.
Patient 3
A 64-year-old woman presented with a 9-month history of diplopia. She had been treated for accommodative esotropia as a child, but had no previous strabismus surgery. She had been diagnosed with thyroid eye disease 14 years previously but had no previous decompression surgery. Primary position PACT showed a 12Δ right hypotropia with 2Δ esotropia at distance and a 12Δ right hypotropia at near. There was no significant change in the amount of horizontal deviation in upgaze (0Δ) and downgaze (2Δ esotropia). Assessment of ductions revealed limitation of upgaze of the right eye both in abduction and adduction. There also was a slight overaction of the right superior oblique muscle. Double Maddox rod testing showed 1° of intorsion, which we felt was inconsistent with isolated inferior rectus muscle tightness where one would expect to find extorsion.3, 9 We therefore suspected masked involvement of the superior oblique muscle.
Intraoperatively there was marked tightness of the right inferior rectus muscle on forced duction testing. There was suspected tightness of the right superior oblique muscle on exaggerated traction testing,7 and after disinsertion of the inferior rectus muscle, elevation of the right eye was improved, especially in abduction, but repeating the exaggerated traction test revealed that the superior oblique muscle was still extremely tight. Also, on inspecting the preplaced limbal dots8 after disinsertion of the inferior rectus muscle, the right eye had become notably intorted, consistent with tightness of the superior oblique muscle. The superior oblique tendon was therefore recessed 12 mm on an adjustable suture. Forced duction tests and exaggerated traction testing indicated residual tightness of the superior oblique muscle. Therefore, the superotemporal quadrant was explored and a residual superior oblique tendon fiber was found attached to the sclera just in anterior to the superotemporal vortex vein. This strand was carefully cut at its insertion. Repeat exaggerated traction testing revealed complete release of the superior oblique tendon. The previously noted intorsion evident on inspection of the limbal blue dots had resolved. Using the relaxed muscle technique6 for judging the optimum initial position of the right inferior rectus muscle, it was recessed 3 mm. No postoperative adjustment was needed.
At 8 weeks postoperatively, the patient reported only rare diplopia. In primary position she was orthotropic at distance and at near with orthophoria by PACT at distance (orthophoria in downgaze, 1Δ exophoria in upgaze) and 6Δ of esophoria by PACT at near. There was 3° of extorsion on double Maddox rod testing.
Patient 4
A 61-year-old man presented with constant diplopia following right decompression surgery for thyroid eye disease. Ten months following recession of the right inferior rectus muscle and right medial rectus muscles, the patient had a recurrence of misalignment, reporting horizontal diplopia at distance due to recurrent esotropia and adopted a chin elevation head posture for comfortable primary position viewing due to moderate limitation of elevation of each eye. At distance there was 20Δ esotropia with 2Δ right hypotropia by PACT, with 25Δ esotropia in upgaze and 12Δ esotropia in downgaze. At near there was 6Δ esophoria by PACT, with 5° extorsion on Double Maddox Rod testing. Further surgery was scheduled.
Intraoperatively there was marked tightness of both inferior rectus muscles. The right was recessed an additional 2 mm from 7 mm recessed to 9 mm recessed, maintaining previous nasal transposition, and the left was recessed 5 mm with nasal transposition of 5 mm. Both medial rectus muscles were also tight and were recessed. After disinsertion of both inferior rectus and medial rectus muscles there was no change in the torsional position of the eye based on observation of the preplaced limbal blue dots, and the exaggerated traction test showed no tightness of either superior oblique, therefore no superior oblique recession was performed. No postoperative adjustment was needed.
Eight weeks postoperatively the patient reported no diplopia and was orthophoric by PACT in primary position at distance with 2Δ exophoria in upgaze and 1Δ esophoria in downgaze. There was 6Δ exophoria at near and 2° of extorsion on Double Maddox Rod testing. Elevation of both eyes was markedly improved. This case illustrates that bilateral inferior rectus tightness can be managed with inferior rectus muscle recessions alone when the superior obliques are not tight.
Discussion
Our index case illustrated the problem of postoperative intorsion and A-pattern exotropia following inferior rectus recessions for involved inferior rectus muscles. The intorsion was successfully addressed when we subsequently identified involved superior oblique muscles and performed bilateral superior oblique recessions. Our clinical suspicion for masked superior oblique tightness in thyroid eye disease was then heightened and so we were then able to identify superior oblique muscle involvement in 2 subsequent cases, in which we avoided postoperative intorsion and A-pattern exotropia by addressing superior oblique tightness at the time of the initial surgery. We concluded that the intraoperative finding of masked superior oblique involvement, and addressing the tight superior oblique at the time of the initial strabismus surgery, prevented consecutive intorsion. In contrast, patient 4 illustrates that, in the absence of superior oblique tightness, inferior rectus recession may be performed without simultaneous weakening of the superior oblique, and without developing postoperative A pattern and extorsion. We propose that clues for masked superior oblique muscle tightness are, first, minimal preoperative extorsion, or frank preoperative intorsion, and, second, superior oblique muscle tightness identified intraoperatively by performing the exaggerated traction test7 after tight rectus muscles have been disinserted.
Superior oblique muscle involvement in thyroid eye disease has been previously described by Goldstein and colleagues,10 Hughes and colleagues,11 and Chatzistefanou and colleagues12 in single case reports and then in a small case series by Thacker and colleagues.13 In Thacker’s 4 cases, superior oblique muscle involvement was evident on preoperative clinical examination by observation of superior oblique overaction and inferior oblique underaction or by noting the presence of intorsion (range, 2°–14°). In addition, Thacker and colleagues13 reported enlargement of the superior oblique muscle using orbital imaging. Our report differs from Thacker and colleagues because in our cases the superior oblique involvement was masked by coexisting ipsilateral inferior rectus muscle involvement. We believe that it is important for the clinician to be aware of the existence of masked superior oblique involvement because failure to identify such involvement may result in intorsion and A-pattern exotropia as illustrated by our first index case.
We suggest that an important clinical clue to the existence of masked superior oblique involvement is the finding of minimal extorsion in the presence of marked inferior rectus muscle tightness. The association of extorsion with inferior rectus tightness has been previously described.3,9,14,15 We suggest that the clinical finding of minimal extorsion, or frank intorsion, in the presence of a tight inferior rectus muscle, is an important sign of probable masked superior oblique tightness.
Based on the current understanding that intorsion and A-pattern exotropia following inferior rectus recession results from secondary overaction of the superior oblique, Kushner3 suggested simultaneous superior oblique recessions. Jampolsky16 and Prieto-Diaz17 advocated a similar approach, recommending simultaneous superior oblique weakening procedures when performing inferior rectus muscle recession in thyroid eye disease. It is possible that superior oblique weakening in the context of thyroid eye disease is most effective when the superior oblique is tight. In the absence of a tight superior oblique muscle, Del Monte’s approach of inferior oblique muscle advancement may be more effective in correcting iatrogenic A-pattern exotropia and intorsion.5 We now suggest that it is important to identify whether or not the superior oblique is involved prior to performing superior oblique surgery.
Both our patients 2 and 3 underwent unilateral inferior rectus recessions and therefore might be considered to be at lower risk for developing A-pattern exotropia and intorsion postoperatively.5 Nevertheless, our intraoperative findings, of marked induced intorsion following disinsertion of the inferior rectus, strongly suggest that postoperative intorsion may have been problematic if it had not been addressed simultaneously (Figure 2). Our method8 of routinely placing limbal dots at 12 and 6 o’clock at the commencement of surgery, enables monitoring of relative changes in ocular torsion at various stages of the procedure.
We found it important to perform the exaggerated traction test for the superior oblique muscle.7 We suggest it is difficult to interpret the exaggerated traction test in the presence of tight rectus muscles and therefore we recommend repeat testing after disinsertion of tight rectus muscles. Repeating the exaggerated traction test was also found to be of value after disinsertion of the superior oblique in patient 3, where it showed residual tightness, due to residual posterior fibers, which needed to be identified and addressed.
Our study would have been strengthened by preoperative imaging of the superior oblique muscles as described by Thacker and colleagues,13 but we believe our clinical and intraoperative findings are compelling. Our technique of identifying and addressing masked superior oblique tightness has only been performed on 2 patients so far, but we believe these case reports are instructive. An additional weakness is that we have only applied our findings to unilateral cases, so the effectiveness of our approach in bilateral cases remains to be explored, although we strongly suspect the same principles apply.
Patients with thyroid eye disease who have tight inferior rectus muscles should be carefully evaluated for possible masked superior oblique muscle involvement, using intraoperative monitoring of torsion and exaggerated traction testing for the superior oblique. Identifying and treating coexisting superior oblique involvement may prevent the development of postoperative A-pattern exotropia and intorsion in patients with strabismus due to thyroid eye disease.
Acknowledgments
Supported by the National Institutes of Health Grants EY018810 (JMH), Research to Prevent Blindness, New York, NY (JMH as Olga Keith Weiss Scholar and an unrestricted grant to the Department of Ophthalmology, Mayo Clinic), and Mayo Foundation, Rochester, Minnesota.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented in part at the British Isles Pediatric Ophthalmology and Strabismus Association meeting, October 14, 2011.
References
- 1.Scott WE, Thalacker JA. Diagnosis and treatment of thyroid myopathy. Ophthalmology. 1981;88:493–498. doi: 10.1016/s0161-6420(81)34988-4. [DOI] [PubMed] [Google Scholar]
- 2.Roper-Hall G, Burde RM. A-pattern exotropia as a complication of thyroid ophthalmopathy. In: Lenk-Schafer M, Calcutt C, Doyle M, Moore S, editors. Orthoptic Horizons. Transactions of the Sixth International Orthoptic Congress. London: Harrogate: British Orthoptic Society; 1987. [Google Scholar]
- 3.Kushner BJ. Torsional diplopia after transantral orbital decompression and extraocular muscle surgery associated with Graves’ orbitopathy. Am J Ophthalmol. 1992;114:239–240. doi: 10.1016/s0002-9394(14)74004-8. [DOI] [PubMed] [Google Scholar]
- 4.Metz HS. Strabismus related to Graves ophthalmopathy. In: Rosenbaum AL, Santiago AP, editors. Clinical strabismus management: Principles and surgical techniques. Philadelphia: W.B. Saunders Company; 1999. pp. 285–295. [Google Scholar]
- 5.Del Monte MA. 2001—An ocular odyssey: Lessons learned from 25 years of surgical treatment for graves eye disease. Am Orthopt J. 2002;52:40–57. doi: 10.3368/aoj.52.1.40. [DOI] [PubMed] [Google Scholar]
- 6.Dal Canto AJ, Crowe S, Perry JD, Traboulsi EI. Intraoperative relaxed muscle positioning technique for strabismus repair in thyroid eye disease. Ophthalmology. 2006;113:2324–2330. doi: 10.1016/j.ophtha.2006.04.036. [DOI] [PubMed] [Google Scholar]
- 7.Guyton DL. Exaggerated traction test for the oblique muscles. Ophthalmology. 1981;88:1035–1040. doi: 10.1016/s0161-6420(81)80033-4. [DOI] [PubMed] [Google Scholar]
- 8.Holmes JM, Hatt SR, Leske DA. Intraoperative monitoring of torsion to prevent vertical deviations during augmented vertical rectus transposition surgery. J AAPOS. 2012;16:136–140. doi: 10.1016/j.jaapos.2011.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flanders M, Hastings M. Diagnosis and surgical management of strabismus associated with thyroid-related orbitopathy. J Pediatr Ophthalmol Strabismus. 1997;34:333–340. doi: 10.3928/0191-3913-19971101-04. [DOI] [PubMed] [Google Scholar]
- 10.Goldstein JH, Schneekloth BB, Babb J, Schussler GC, Kapoor V. Acquired Brown's superior oblique tendon syndrome due to euthyroid Graves’ disease ophthalmomyopathy. Binocul Vis Quart. 1990;5:93–97. [Google Scholar]
- 11.Hughes DS, Beck L, Hill R, Plenty J. Dysthyroid eye disease presenting as Brown's syndrome. Acta Ophthalmol (Copenh) 1992;70:262–265. doi: 10.1111/j.1755-3768.1993.tb05000.x. [DOI] [PubMed] [Google Scholar]
- 12.Chatzistefanou K, Kushner BJ, Moschos MN. An unusually large incyclotropia associated with dysthyroid ophthalmopathy. Br J Ophthalmol. 2008;92:291–292. doi: 10.1136/bjo.2007.119735. [DOI] [PubMed] [Google Scholar]
- 13.Thacker NM, Velez FG, Demer JL, Rosenbaum AL. Superior oblique muscle involvement in thyroid ophthalmopathy. J AAPOS. 2005;9:174–178. doi: 10.1016/j.jaapos.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 14.Caygill WM. Excyclotropia in dysthyroid ophthalmopathy. Am J Ophthalmol. 1972;73:437–441. doi: 10.1016/0002-9394(72)90073-6. [DOI] [PubMed] [Google Scholar]
- 15.Chen VM, Dagi LR. Ocular misalignment in Graves disease may mimic that of superior oblique palsy. J Neuroophthalmol. 2008;28:302–304. doi: 10.1097/WNO.0b013e31818f133e. [DOI] [PubMed] [Google Scholar]
- 16.Jampolsky A. Management of vertical strabismus. Trans New Orleans Acad Ophthalmol. 1986;34:141–171. [PubMed] [Google Scholar]
- 17.Prieto-Diaz J, Souza-Dias C. Strabismus. 4th ed. Boston: Butterworth-Heinemann; 2000. Restrictions; pp. 359–399. [Google Scholar]