Abstract
Background: Risk of malignancy index (RMI) is the best method for discriminating benign and malignant pelvic masses. The aim of this study was to determine the RMI for preoperative evaluation of pelvic mass.
Methods: This study was performed on 182 women with adenexal mass referred to Yahyahnejiad Hospital of Babol University of Medical Sciences in Iran from 2007 to 2009.The sensitivity, specificity, positive (PPV) and negative predictive values (NPV) of menopausal status, ultrasound finding of pelvic mass and level of serum CA-125, separately or combined into the RMI were calculated and compared.
Results: The mean age of patients was 39.9±9.3 years. The RMI with the cut-off point of 265 had a sensitivity of 91.3%, specificity of 96.2 %, PPV of 77.7% and NPV of 98.7% for diagnosis of malignant masses.
Conclusion: Risk of malignancy index should be an effective method for evaluating a patient with adnexal masses before operation and a cut-off point of 265 which has a very high sensitivity, specificity and positive and negative predictive values for discriminating malignant and benign pelvic masses.
Key Words: Risk of Malignancy Index (RMI), CA125, Cut-off point
Pelvic mass is a challenge to refer to a gynecologist with one of the most common reasons of benign or malignant conditions (1). One of the pelvic masses is ovarian cancer, the second most common gynecologic malignancy, the fifth cause of death due to cancers and has more mortality than the other gynecologic malignancies (2, 3). Most cases are diagnosed at stage III or IV where prognosis is poor (4, 5). Diagnosis of pelvic masses including ovarian cancer by a variety of procedures is inaccurate and uncertain, therefore, in 1990, Jacob et al. developed a risk of malignancy index [RMI] based on serum level of CA125, menopausal state and ultrasound findings (6).
The RMI is a suitable index for evaluation of pelvic mass before surgery and confirms previous studies indicating that RMI improves the discrimination between non- malignant and malignant pelvic masses (5, 7). In many studies, the cut-off value of 200 for RMI is the best discrimination for benign and malignant pelvic mass because of its high sensitivity and specificity levels (5). This study was done on a group of patients with Jacob's criteria in order to find the sensitivity and specificity of RMI for the diagnosis of pelvic masses preoperatively in Babol, North of Iran.
Methods
This study included the records of 182 women with pelvic masses, who were admitted for laparatomy from 2007 and 2009, at Yahyahnejiad Gynecological Unit in Babol, north of Iran.
The postmenopausal status was defined as more than 1 year of amenorrhea or more than 50 years old in women who have had a hysterectomy. The risk of malignancy index (RMI) was calculated for all the patients (9). The purpose of this study was to determine the RMI for preoperative evaluation of pelvic mass. This study was approved by the Research Center of the Babol University of Medical Sciences and consent was obtained by all the patients. The patients underwent the laparatomy, and the specimens were sent to the Department of Pathology for histological examination.
Calculation of RMI: Ultrasound scans were scored as one point for each of the following characteristics: multilocular cyst, evidence of solid areas, evidence of metastases, presence of ascites, bilateral lesions using the scoring system suggested by Jacob et al. (6). Simple mass (U=0) (for ultrasound score of 0); semi complex mass (U=1) (for ultrasound score of 1); complex mass (U=3) (for ultrasound score of 2 or more) (8). The RMI was calculated for each patient using the equation of Jacob et al. RMI = M×U×serum CA125 level, (with M=1 for premenopausal status and M=3 for post menopausal status). The absolute values of CA125 serum level were entered directly in the formula (1, 8).
All data was analysed by SPSS version 18. We used the t-test, Fishers exact test, Pearson, Chi-square and Mann-Whitney U. where the appropriate receiver operating characteristics (ROC) curve was plotted and the sensitivity, specificity, positive and negative predictive values (PPV, NPV) were determined. The odds ratio with 95% confidence interval (CI) was calculated, in order to determine the cut-off point of RMI for the prediction of the chance of malignancy. A probability value of p<0.05 was considered to be statistically significant. The normal distribution of data was determined by One- Sample Kolmogorov- Smirnov test.
Results
A total of 182 patients were enrolled in this study. According to the histological examination of the specimens, 23 (12.7%) were malignant, 158 (87.3%) were benign and 1 (0.5%) had tuberculosis. The mean age of patients was 39.9±9.3 years. The distribution of age, menopausal status, ultrasound score (U), serum CA 125 level and RMI in women with benign (n=158) and malignant (n=23) pelvic masses are shown in table 1.
Table 1.
The distribution of age, menopausal status, ultrasound score (U), serum CA 125 level and RMI in women with benign and malignant pelvic masses
| Parameter | Non–Malignant (n=158) | Malignant (n=23) | P-value |
|---|---|---|---|
| Age (Mean) | 38.7±8.3 | 47.7±12.5 | 0.003* |
| menopausal status (M) | |||
| Premenopausal Postmenopausal |
145 (90.1%) 13 (65%) |
16 (9.9%) 7 (35%) |
0.006* |
| Ultrasound score (U) | |||
| U=0 U=1 U=2-5 |
45 (100%) 50 (100%) 63 (73.3%) |
0 (0%) 0 (0%) 23(26.7%) |
0.001* |
| SerumCA-125 (Mean Rank)(U/ml) |
81.3 | 157.0 | <0.001* |
| RMI (Mean Rank)(U/ml) | 80.8 | 160.8 | <0.001* |
*p<0.05
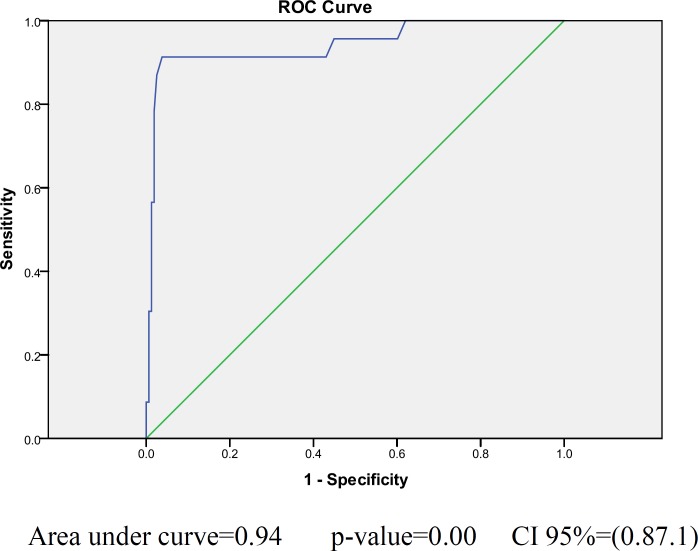
According to the receiver operating characteristic (ROC) curve evaluation results, the cut-off point of 265 was accepted for the RMI, the calculated values revealed for sensitivity were 91.3% and specificity of 96.2% (figure1).
Figure 1.
ROC curve showing the relationship between specificity and sensitivity for RMI 1 in differentiating between benign and malignant pelvic masses
The sensitivity, specificity, positive and negative predictive values and odd ratio (95% CI) of RMI in the different cut-off points are shown in table 2.
Table 2.
Sensitivity, specificity, positive, negative predictive values and odds Ratio of RMI at the different cut-off points
| Cut off point RMI | Sensitivity (%) |
Specificity
(%) |
PPV (%) |
NPV
(%) |
Odds Ratio
(CI 95%) |
LR+
(CI 95%) |
LR-
(CI 95%) |
|---|---|---|---|---|---|---|---|
| 265 | 91.3 | 96.2 | 77.7 | 98.7 | 76.81 (16.67, 353.88) |
24.04 (10.86, 53.24) |
0.09 (0.02, 0.37) |
| 150 | 91.3 | 80.37 | 41.38 | 98.44 | 43 (9.57, 193.28) |
4.65 (3.31, 6.65) |
0.11 (0.03, 0.41) |
| 200 | 91.3 | 88 | 52 | 98.58 | 76.81 (16.67, 353.88) |
7.59 (4.89, 11.79) |
0.1 (0.03, 0.37) |
Discussion
We found that the different serum levels of CA 125 in benign and malignant pelvic masses are similar to other studies (1, 9). The high sensitivity and specificity, PPV, NPV of the RMI at the optimal cut-off point of 265 in this study had a sensitivity of 91.3%, a specificity of 96.2% and a PPV of 77.7%, and an NPV of 98.7%. Bailey et al. on 182 women with pelvic mass indicated an RMI > at a cut-off point of 200 with sensitivity of 88.5% for diagnosing the invasive lesions while Enakpene et al. on 302 women with pelvic mass indicated an RMI at a cut-off point of 250, a sensitivity of 88.2%, a specificity of 74.3%, a PPV of 71.3%, and an NPV of 90% for diagnosing the invasive lesions (10, 11). In the current study, RMI at a cut-off point of 200 had a sensitivity of 91.3%, a specificity of 88% a PPV of 52%, and an NPV of 98.58%. According to table 3, the results of previous studies described that many studies showed the best cut-off point for RMI was 200 (1, 5-6, 8, 12-20).
Table 3.
Comparison of the current study's results with the previous studies
| study | N | Sensitivity % | Specificity% | PPV% | NPV% | Year |
|---|---|---|---|---|---|---|
| Jacobs et al (6) * | 143 | 85.4 | 96.6 | - | - | 1990 |
| Davies et al (12) * | 124 | 87 | 89 | - | - | 1993 |
| Tingulstad et al (13) | 173 | 71 | 96 | 89 | 88 | 1996 |
| Tingulstad et al (14) | 365 | 71 | 92 | 69 | 92 | 1999 |
| Morgante et al (15) | 124 | 58 | 95 | 78 | 87 | 1999 |
| Manjunath et al (16) | 152 | 73 | 91 | 93 | 67 | 2000 |
| Ma et al (17) | 140 | 87.3 | 84.4 | 82.1 | 89 | 2003 |
| Torres et al (18)* | 158 | 73 | 86 | - | - | 2003 |
| Andersen et al (19) | 180 | 70.6 | 87.7 | 66.1 | 89.8 | 2003 |
| Obeidat et al (1) | 100 | 90 | 89 | 96 | 78 | 2004 |
| Leelahakorn et al (20) | 175 | 88.6 | 90.7 | 70.5 | 97 | 2005 |
| Ulusoy et al (8) | 296 | 71.7 | 80.5 | 67.3 | 83.6 | 2007 |
| Van den Akker et al (5) | 548 | 81 | 85 | 48 | 96 | 2010 |
| Current study | 182 | 91.3 | 88 | 52 | 98.58 |
Values were given for RMI = 200 *In the studies Jacobs et al. Davies et al. and Torres. and PPV and NPV were not given .
A systematic review study by Geomini et al. in 2009, 116 diagnostic studies for adnexal malignancy was reviewed. The reported result showed that RMI at cut-off point of 200 had a sensitivity of 78% and a specificity 87% for malignant mass diagnoses which was similar to our results (21).
According to the results of Ulusoys et al. in 2007, the RMI in a cut-off level of 153 showed a sensitivity of 76.4%, a specificity of 77.9%, a PPV of 65.9%, and an NPV of 85.5% for prediction of malignancy (8). In the present study, RMI, at a cut-off level of 150 had a sensitivity of 91.3%, a specificity of 80.37%, a PPV of 41.38%, and an NPV of 98.44% for detection of malignancy. In conclusion, based on our study, the risk of malignancy index should be an effective index for evaluating a patient with adnexal masses before operation and a cut-off point of 265 shows a very high sensitivity, specificity and positive and negative predictive values for discriminating malignant and benign pelvic masses.
Acknowledgments
We would like to thank the Vice Chancellor of Research and Technology Center of Babol University of Medical Sciences for the approval of this study, and to all the patient participants.
References
- 1.Obeidat B, Amarin Z, Latimer J, Crawford RA. Risk of malignancy index in the preoperative evaluation of pelvic masses. Int J Gynecol Obstet. 2004;85:255–8. doi: 10.1016/j.ijgo.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 2.Greenlee RI, Hill-Harmon MB, Murray T, Thun M. Cancer statistics, 2001. CA cancer J Clin. 2001;51:15–36. doi: 10.3322/canjclin.51.1.15. [DOI] [PubMed] [Google Scholar]
- 3.Landis S, Murray T, Bolden S, Wingo PA. Cancer statistics. Ca Cancer J Clin. 1998;48:6–29. doi: 10.3322/canjclin.48.1.6. [DOI] [PubMed] [Google Scholar]
- 4.Goldstein SR. Postmenopausal adnexal cysts: how clinical management has evolved. Am J Obstet Gynecol. 1996;175:1498–501. doi: 10.1016/s0002-9378(96)70097-2. [DOI] [PubMed] [Google Scholar]
- 5.Van den Akker PA, Aalders AL, Snijders MP, et al. Evaluation of the risk of malignancy index in daily clinical management of adnexal masses. Gynecol Oncol. 2010;116:384–8. doi: 10.1016/j.ygyno.2009.11.014. [DOI] [PubMed] [Google Scholar]
- 6.Jacobs I, Oram D, Fairbanks J, et al. A risk of malignancy index incorporating CA 125, ultrasound and menopausal status for the accurate preoperative diagnosis of ovarian cancer. Br J Obstet Gynaecol. 1990;97:922–9. doi: 10.1111/j.1471-0528.1990.tb02448.x. [DOI] [PubMed] [Google Scholar]
- 7.Akdeniz N, Kuyumcuoglu U, Kale A, Erdemoglu M, Caca F. Risk of malignancy index for adnexal masses. Eur J Gynaecol Oncol. 2009;30:178–80. [PubMed] [Google Scholar]
- 8.Ulusoy S, Akbayir O, Numanoglu C, et al. The risk of malignancy index in discrimination of adnexal masses. Int J Gynecol Obstet. 2007;96:186–91. doi: 10.1016/j.ijgo.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 9.Yamamoto Y, Yamada R, Oguri H, Maeda N, Fukaya T. Comparison of four malignancy risk indices in the preoperative evaluation of patients with pelvic masses. Eur J Obstet Gynecol Reprod Biol. 2009;144:163–7. doi: 10.1016/j.ejogrb.2009.02.048. [DOI] [PubMed] [Google Scholar]
- 10.Bailey J, Tailor A, Naik R, et al. Risk of malignancy index for referral of ovarian cancer cases to a tertiary center: does it identify the correct cases? Int J Gynecol Cancer. 2006;16:30–4. doi: 10.1111/j.1525-1438.2006.00468.x. [DOI] [PubMed] [Google Scholar]
- 11.Engelen MJA, Bongaerts AHH, Sluiter WJ, de Haan HH, Bogchelman DH, TenVergert EM, et al. Distinguishing benign and malignant pelvic masses: The value of different diagnostic methods in everyday clinical practice. Eur J Obstet Gynecol Reprod Biol. 2008;136:94–101. doi: 10.1016/j.ejogrb.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 12.Davies A, Jacobs I, Woolas R, Fish A, Oram D. The adnexal mass: benign or malignant? Evaluation of a risk of malignancy index. Br J Obstet Gynaecol. 1993;100:927–31. doi: 10.1111/j.1471-0528.1993.tb15109.x. [DOI] [PubMed] [Google Scholar]
- 13.Tingulstad S, Hagen B, Skjeldestad F, Onsrud M, Kiserud T, Halvorsen T, et al. Evaluation of a risk of malignancy index based on serum CA125, ultrasound findings and menopausal status in the pre operative diagnosis of pelvic masses. Br J Obstet Gynaecol. 1996;103:826–31. doi: 10.1111/j.1471-0528.1996.tb09882.x. [DOI] [PubMed] [Google Scholar]
- 14.Tingulstad S, Hagen B, Skjeldestad FE. The risk-of-malignancy index to evaluate potential ovarian cancers in local hospitals. Obstet Gynecol. 1999;93:448–52. [PubMed] [Google Scholar]
- 15.Morgante G, La Marca A, Ditto A, De Leo V. Comparison of two malignancy risk indices based on serum CA125, ultrasound score and menopausal status in the diagnosis of ovarian masses. Br J Obstet Gynaecol. 1999;106:524–7. doi: 10.1111/j.1471-0528.1999.tb08318.x. [DOI] [PubMed] [Google Scholar]
- 16.Manjunath AP, Pratapkumar , Sujatha K, Vani R. Comparison of Three Risk of Malignancy Indices in Evaluation of Pelvic Masses. Gynecol Oncol. 2001;81:225–9. doi: 10.1006/gyno.2001.6122. [DOI] [PubMed] [Google Scholar]
- 17.Ma S, Shen K, Lang J. A risk of malignancy index in preoperative diagnosis of ovarian cancer. Chin med J (Engl) 2003;116:396–9. [PubMed] [Google Scholar]
- 18.Torres J, Derchain SE, Faúndes A, et al. Risk-of-Malignancy Index in preoperative evaluation of clinically restricted ovarian cancer. Sao Paulo Med J. 2002;120:72–6. doi: 10.1590/S1516-31802002000300003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andersen ES, Knudsen A, Rix P, Johansen B. Risk of Malignancy Index in the preoperative evaluation of patients with adnexal masses. Gynecol Oncol. 2003;90:109–12. doi: 10.1016/s0090-8258(03)00192-6. [DOI] [PubMed] [Google Scholar]
- 20.Leelahakorn S, Tangjitgamol S, Manusirivithaya S. Comparison of Ultrasound Score, CA125, Menopausal Status, and Risk of Malignancy Index in Differentiating between Benign and Borderline or Malignant Ovarian Tumors. J Med Assoc Thai. 2005;88:S22–30. [PubMed] [Google Scholar]
- 21.Geomini P, Kruitwagen R, Bremer G, Cnossen J, Mol BW. The accuracy of risk scores in predicting ovarian malignancy: a systematic review. Obstet Gynecol. 2009;113:384–94. doi: 10.1097/AOG.0b013e318195ad17. [DOI] [PubMed] [Google Scholar]