Abstract
Background: International travel, migration and human population movements facilitate the spread of tuberculosis (TB).
Objective: To study the impact of poorly screened expatriates working in Saudi Arabia on the local incidence of TBs.
Patients and methods: This cross sectional study was carried out in the Chest Disease Hospital, Taif. All confirmed cases of TB from June 2009 to May 2010 admitted to the hospital were enrolled. Inclusion criteria were diagnosed cases of TB (pulmonary & extra-pulmonary) in patients between the ages of 14 to 65 years. Patients with HIV and coexistent malignancies were excluded. The age, gender and ethnic group of each patient was recorded, and patients were divided into two groups. Of the two groups, Group A consisted of Taif residents and group B of patients referred from other cities in the country.
Results: Of the 686 cases studied, 370 (54%) were Saudi nationals (Group A = 80 & Group B = 290) and 316 (46%) cases were from other countries. Males outnumbered females and most of the patients were aged 20 to 29 years. The number of cases from the areas close to the pilgrimage sites, i.e. Makah (233) and Jeddah (275), outnumbered those in Taif (110).
Conclusions: Our study identifies an increased prevalence of TB cases in areas close to the pilgrimage (Group B). The higher proportion of non-Saudi TB patients in group B is most likely explained by the higher number of poorly screened illegal expatriates in the region.
Keywords: tuberculosis, pilgrims, poor socioeconomic status, illegal expatriates
Zusammenfassung
Hintergrund: Internationale Reisen, Migration und Bevölkerungsbewegungen erleichtern die Ausbreitung der Tuberkulose (TBC).
Ziel: Untersuchung des Einflusses von wenig untersuchten ausländischen Arbeitern auf die lokale Inzidenz der TBC in Saudi-Arabien.
Patienten und Methoden: Diese Querschnittsstudie wurde im Chest Disease Hospital, Taif, Saudi-Arabien durchgeführt. Einbezogen wurden alle bestätigten Fälle von TBC, die im Zeitraum von Juni 2009 bis Mai 2010 in die Klinik eingewiesen wurden. Einschlusskriterien waren diagnostizierte Fälle von TBC (Lungen- und allgemeiner TBC) bei Patienten im Alter zwischen 14 und 65 Jahren. HIV-Patienten und Patienten mit koexistenten Krebserkrankungen wurden ausgeschlossen. Alter, Geschlecht und die ethnische Zugehörigkeit jedes Patienten wurden erfasst. Die Patienten wurden in zwei Gruppen aufgeteilt: Gruppe A bestand aus Einwohnern von Taif und Gruppe B aus Patienten, die aus anderen Regionen des Landes überwiesen wurden.
Ergebnisse: Von den 686 untersuchten Fällen waren 370 (54%) saudische Staatsangehörige (Gruppe A = 80, Gruppe B = 290) und 316 (46%) der Patienten stammten aus anderen Ländern. Die Zahl der Männer übertraf die der Frauen und die meisten Patienten waren 20–29 Jahre alt. Die Zahl der Fälle aus den Gebieten in der Nähe der Pilgerstätten, d.h. Makah (233) und Dschidda (275), übertraf die in Taif (110).
Schlussfolgerung: Diese Studie zeigt eine erhöhte Prävalenz der TBC-Fälle in Gebieten in der Nähe der Pilgerstätten (Gruppe B). Der höhere Anteil von TBC-Patienten nicht-saudischer Nationalität in Gruppe B ist am ehesten durch die größere Zahl von schlecht untersuchten illegalen Einwanderern in der Region zu erklären.
Introduction
M. tuberculosis is spread through the inhalation of aerosolized droplet nuclei emanating from infected individuals. Millions around the globe are affected by this disease annually. Humans are important reservoirs of the bacillus. It has been shown that proper treatment constitutes a key factor in the control of the disease. Tuberculosis (TB) is common in most developing countries. However, with the advent of AIDS, it has re-emerged in developed countries as well [1], [2]. The causes of this increased incidence of TB in developing countries include ineffective control programs, the presence of human immunodeficiency virus (HIV), low socioeconomic status (poverty and civil unrest), rapidly increasing populations, and drug resistance. Similarly, in developed countries, immigration from high-prevalence TB areas, HIV, social deprivation and drug resistance contribute to the increasing incidence of the disease [1]. Studies have shown that international travel, migration and movement of populations can facilitate the spread of TB. Saudi Arabia has a unique population dynamic, as annually, more than two million pilgrims visit the country for the Hajj pilgrimage, and, in addition, more than six million expatriates living in Saudi Arabia come from endemic areas [3]. This study was undertaken to identify the proportion of TB cases due to the non-Saudi population and to estimate the impact of poorly screened expatriates working here on the tuberculsosis burden in Saudi Arabia.
Patients and methods
This cross sectional study was carried out in the Chest Disease Hospital, Taif, a tertiary care referral hospital in western region of Saudi Arabia. Cases were defined as patients with pulmonary TB (sputum positive) and extra-pulmonary TB, the diagnosis of which was based on standard clinical, radiological and histological criteria. The cases were divided into two groups. Group A consisted of Taif residents, and group B was made up of patients referred from other cities in the country. All confirmed cases of TB admitted to the hospital from June 2009 to May 2010 were enrolled. Patients were subsequently contacted and followed up until December 2012. Inclusion criteria were diagnosed cases of TB, aged between 14 and 65, and the study included patients with new onset and/or re-activation of previously diagnosed TB. Patients with HIV, and/or co-existent malignancies were excluded. Age, gender, ethnic group and socioeconomic status were recorded for each patient. Similarly, the pattern of their TB, individual diagnostic procedures and treatment plans, as well as any eventual complications were also recorded.
The study was carried out with the approval of the hospital ethical committee, and was conducted in full compliance with the guidelines laid down in 1964 and later amendments in the “Ethical Principles for Medical Research Involving Human Subjects” statement of the World Medical Assembly Declaration of Helsinki.
Statistical analysis
The data was entered on Microsoft Excel and statistical analysis was carried out using SPSS version 13. Descriptive statistics were used to describe the basic features of the data in this study. Univariate analysis was done to evaluate the patterns of distribution, the main tendencies and the dispersion of the disease.
Results
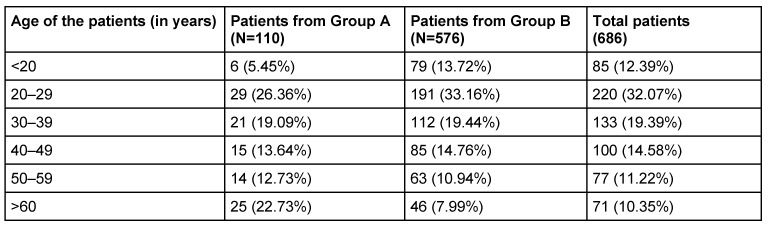
A total of 690 patients were enrolled in the study. 4 patients for potential inclusion were excluded (2 had carcinoma lung, 1 had hepatic encephalopathy and 1 had lymphoma), and finally data on 686 patients with confirmed TB was analyzed. Patients were divided into two groups. Group A (N=110) comprised patients from Taif and group B (N=576) consisted of patients coming from other cities. As shown in Table 1 (Tab. 1) in both groups, most of the patients were aged 20 to 29. Among the 110 patients in Group A, 65 were males (59.09%) and 45 females (40.91%). Similarly, among the 576 patients in Group B, 403 (69.97%) were males and 173 (30.03%) were females. Diverse ethnic groups were represented in both Group A and Group B. 80 patients in Group A were Saudi nationals, as were 290 in Group B (Table 2 (Tab. 2)). The total number of Saudi patients in both groups was 370 (54%). Thus 316 (46%) TB patients in both groups came from other countries. 110 patients came from Taif, 233 from Makah, 275 from Jeddah and 30 from Qunfuda (Figure 1 (Fig. 1)).
Table 1. Comparison of groups regarding the age of the patients.
Table 2. Nationality of the patients in Group A and Group B.
Figure 1. Number of patients from different cities.
In Group A, 70 (63.64%) patients had pulmonary TB while 40 (36.36%) had extra-pulmonary TB. In Group B, 457 (79.34%) patients were diagnosed with pulmonary TB and 119 (20.66%) patients were suffering from extra-pulmonary TB. Thus pulmonary TB was found to be more prevalent in Group B, while the same was true of extra-pulmonary TB in Group A.
In Group A, 19 (17.27%) patients had a history of contact with TB individuals, while 91 (82.73%) had no previous history of contact. On the other hand, in Group B, out of 576 patients, 128 were found to have a history of TB patient contact (Table 3 (Tab. 3)).
Table 3. Clinical characteristics of tuberculosis in Group A and Group B.
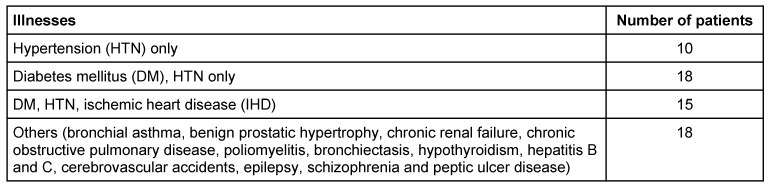
Overall, of the 686 patients in our study, 599 (87.32%) were newly diagnosed and 87 (12.68%) were re-treated cases of TB. Combined group analysis revealed comorbid illnesses among 61 patients. Ten patients suffered from hypertension (HTN), 18 patients had diabetes mellitus (DM) and HTN, and 15 had DM, HTN and ischemic heart disease (IHD). 18 patients had various other ailments such as bronchial asthma, benign prostatic hypertrophy, chronic renal failure, chronic obstructive pulmonary disease, poliomyelitis, bronchiectasis, hypothyroidism, hepatitis B and C, cerebrovascular accidents, epilepsy, schizophrenia and peptic ulcer disease (Table 4 (Tab. 4)). X-ray chest studies showed bilateral radiological characteristics of TB in 22 patients, whereas 65 had unilateral findings in which the upper lobe of lung (either right or left) was predominantly involved.
Table 4. Comorbid illnesses.
Treatment and follow-up
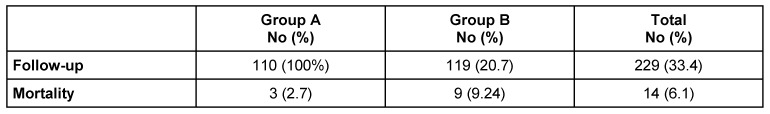
All patients had been treated with the standard treatment of four drugs (isonicotinylhydrazine (INH), rifampicin, ethambutol, pyrazinamide) for an initial 2 months, and, in cases of pulmonary TB, followed by a combination of INH and rifampicin for another 4 months. Treatment was continued for another 10 months in patients with abdominal TB. Patients were admitted as in-patients until their sputum was negative, and were then followed up in their local centers later. In group A all 110 patients could be contacted on phone and followed up while in group B only 119 out of 576 patients could be followed up. Hence, of a total of 686 patients, only 229 could be followed up. There were several reasons for this poor follow-up. In some cases, either the patients had provided wrong phone numbers, or else their telephone services had expired. Another common reason was that some of these patients could have been illegal immigrants who feared questioning, and we could not follow them. In group A, 3 patients had died (mortality rate 2.7%) and in group B, 11 patients had died (mortality rate 9.24%). Thus an overall mortality of 6.1% was to be observed in this study (Table 5 (Tab. 5)).
Table 5. Follow-up and mortality rate among Group A & Group B.
Discussion
Tuberculosis (TB) is an endemic infection in Saudi Arabia. Its incidence has increased, due to the interesting and unique population dynamics of this country. Of 6 million expatriate workers living in Saudi Arabia, the majority come from areas where TB is endemic, a factor which could be affecting the increased prevalence of TB in Saudi Arabia [1]. In our study, most of the patients referred to us came from Makah and Jeddah. These cities are close to the Hajj regions, where more than 2 million pilgrims from all over the world come annually to perform Hajj. Most of them are adults, often elderly with underlying medical conditions [2]. Previous studies have shown that TB infection in Jeddah (the main sea and airport for pilgrims arriving into Mecca) can reach up to 64 cases per 100,000, compared with 32 per 100,000 in central regions like Riyadh. The higher rate in Jeddah may have been caused by influx of pilgrims [3], [4]. Qureshi et al. [5] observed that cough was the most common complaint, affecting more than 50% of pilgrims, and also that the commonest cause of pneumonia among hospitalized pilgrims visiting Saudi Arabia during the Hajj was TB [6]. In our study of 686 patients, 316 (46.1%) were non-Saudi, working in this country, as shown in Table 2 (Tab. 2). These immigrant nationalities have a high incidence of TB [7]. Of Saudi cities, Qunfuda City had the highest number of TB cases, probably because of poor socioeconomic living standards and may be the high numbers of illegal expatriates working there. This leads to the suspicion that workers coming to Saudi Arabia are not properly evaluated in their home countries before leaving to take up employment in Saudi Arabia. It raises many questions about the fitness certificates issued by the various health institutions of these parent countries prior to their nationals leaving them to seek employment in Saudi Arabia. This issue has been addressed by Al-Hajoj et al. [8]. The authors concluded in their study that the large number of falsified health certificates issued by their home countries to non-national drivers working in Saudi Arabia added to the transmission of TB. Having said this, it is pertinent to mention that the Ministry of Health in Saudi Arabia urgently needs to take up the matter with various countries so that employees and pilgrims are properly evaluated in their countries of origin prior to their visit to Saudi Arabia.
This phenomenon also has implications for public health on an international scale. Wilder-Smith et al. [9] conducted a prospective study among Singaporean Hajj pilgrims by applying quantiferon tests both before and 3 months after their Hajj. They observed 10% conversion rates to tubercular infection in these returning Hajj subjects. The authors of this study were of the opinion that pilgrims may be at a higher risk of acquiring TB during Hajj. Consequently, all countries need to co-operate to ensure proper screening of pilgrims for the Hajj and the Umrah in order to avoid the pooling of TB and its subsequent transmission. The Saudi Arabian Ministry of Health has previously recommended the use of face masks during pilgrimage in order to prevent the spread of airborne diseases during pilgrimages but unfortunately compliance remains poor [10].
The question of which methods to use for the identification of latent TB (LTBI) is open. The tuberculin skin test (TST) has high sensitivity, but low specificity, especially in Bacillus Calmette-Guérin (BCG)-vaccinated individuals, because of cross-reactivity to non-tubercular mycobacterias (NTM) or due to a booster-effect caused by repetitive testing [11]. Blood based interferon-gamma release assays (IGRA) offer better specificity (98–100%) and at least as good sensitivity (70–97%) as the TST, since they are unaffected by previous BCG vaccination and most NTM [12] ,[13], [14], [15]. Concerning the cost factors, whether routine IGRA would be better for screening instead mass usage of TST prior to Hajj and Umrah needs to be studied.
Our study has shown an increased incidence of TB among young adult males (in both Group A and Group B), and these results concur with the conclusions of other researchers as well [16], [17]. We observed pulmonary TB more frequently than extra-pulmonary TB with predominant unilateral and apical lobe lung involvement. Because of its high potential for transmission to others, the discovery of cases of pulmonary TB raises the alarm among health planners, and emphasizes the need for hyper-conservative approach to prevent its spread. Control measures such as health education, actively searching for and identifying cases, and prompt and well-supervised medical treatment are all needed to curb the ongoing transmission of TB. It has been recommended that more studies using molecular techniques are carried out in order to establish the real incidence of cross infection in Saudi Arabia. In addition, molecular techniques are to be instituted in all reference laboratories to help the detection of ongoing active transmission and the molecular epidemiology of this infection [8].
Pilgrims and many illegal expatriate workers in Saudi Arabia who develop TB do not report to the hospitals fearing questioning etc. As has been described in this study of 686 patients, we could follow only 286 patients, as illegal residents commonly escape follow-up after 2 to 3 weeks of treatment. Unfortunately, often these individuals take refuge on large farms or within the households of local nationals. In so doing, they ultimately contribute towards the transmission of TB and the development of drug resistant strains of the disease [18].
The limitations of our study are that, due to the factors described above, owing to the difficulty we experienced in following up some of the patients in the study, we could neither predict resistant cases of TB, nor could we identify the predictors of mortality. Possibly a proper way of reception, documentation, admissions and reassurance regarding the confidentiality of our follow-up of the patients could rectify such limitations in future.
In conclusion, our study brings to the fore the urgent need for improved TB surveillance of non-Saudi workers and pilgrims, in their home countries. The conclusions drawn from this study highlight the need for concerted and effective action by those international health services connected with pilgrimage and migrant labour as well as by the Ministry of Health Saudi Arabia so that burden of TB is effectively controlled.
Notes
Competing interests
The authors declare that they have no competing interests.
References
- 1.Memish ZA, Venkatesh S, Ahmed QA. Travel epidemiology: the Saudi perspective. Int J Antimicrob Agents. 2003 Feb;21(2):96–101. doi: 10.1016/S0924-8579(02)00364-3. Available from: http://dx.doi.org/10.1016/S0924-8579(02)00364-3. [DOI] [PubMed] [Google Scholar]
- 2.El-Kassimi FA, Abdullah AK, al-Orainey IO, Lambourne A, Bener AB, al-Hajjaj MS. Tuberculin survey in the Eastern Province of Saudi Arabia. Respir Med. 1991 Mar;85(2):111–116. doi: 10.1016/S0954-6111(06)80287-8. Available from: http://dx.doi.org/10.1016/S0954-6111(06)80287-8. [DOI] [PubMed] [Google Scholar]
- 3.Al-Hajoj SA. Tuberculosis in Saudi Arabia: can we change the way we deal with the disease? J Infect Public Health. 2010;3(1):17–24. doi: 10.1016/j.jiph.2009.12.001. Available from: http://dx.doi.org/10.1016/j.jiph.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 4.Al-Jahdali H, Memish ZA, Menzies D. Tuberculosis in association with travel. Int J Antimicrob Agents. 2003 Feb;21(2):125–130. doi: 10.1016/S0924-8579(02)00283-2. Available from: http://dx.doi.org/10.1016/S0924-8579(02)00283-2. [DOI] [PubMed] [Google Scholar]
- 5.Qureshi H, Gessner BD, Leboulleux D, Hasan H, Alam SE, Moulton LH. The incidence of vaccine preventable influenza-like illness and medication use among Pakistani pilgrims to the Haj in Saudi Arabia. Vaccine. 2000 Jul;18(26):2956–2962. doi: 10.1016/S0264-410X(00)00116-X. Available from: http://dx.doi.org/10.1016/S0264-410X(00)00116-X. [DOI] [PubMed] [Google Scholar]
- 6.Alzeer A, Mashlah A, Fakim N, Al-Sugair N, Al-Hedaithy M, Al-Majed S, Jamjoom G. Tuberculosis is the commonest cause of pneumonia requiring hospitalization during Hajj (pilgrimage to Makkah) J Infect. 1998 May;36(3):303–306. doi: 10.1016/S0163-4453(98)94315-8. Available from: http://dx.doi.org/10.1016/S0163-4453(98)94315-8. [DOI] [PubMed] [Google Scholar]
- 7.Irfan S, Hassan Q, Hasan R. Assessment of resistance in multi drug resistant tuberculosis patients. J Pak Med Assoc. 2006 Sep;56(9):397–400. [PubMed] [Google Scholar]
- 8.Al-Hajoj SA, Mohammed VK, Al-Hokail AA. Usefulness of molecular techniques to identify ongoing tuberculosis transmission in Saudi Arabia. Saudi Med J. 2007 Feb;28(2):268–270. [PubMed] [Google Scholar]
- 9.Wilder-Smith A, Foo W, Earnest A, Paton NI. High risk of Mycobacterium tuberculosis infection during the Hajj pilgrimage. Trop Med Int Health. 2005 Apr;10(4):336–339. doi: 10.1111/j.1365-3156.2005.01395.x. Available from: http://dx.doi.org/10.1111/j.1365-3156.2005.01395.x. [DOI] [PubMed] [Google Scholar]
- 10.Al-Hajoj S, Varghese B, Shoukri MM, Al-Omari R, Al-Herbwai M, Alrabiah F, Alrajhi AA, Abuljadayel N, Al-Thawadi S, Zumla A, Zignol M, Raviglione MC, Memish Z. Epidemiology of antituberculosis drug resistance in Saudi Arabia: findings of the first national survey. Antimicrob Agents Chemother. 2013 May;57(5):2161–2166. doi: 10.1128/AAC.02403-12. Available from: http://dx.doi.org/10.1128/AAC.02403-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Menzies D. What does tuberculin reactivity after bacille Calmette-Guérin vaccination tell us? Clin Infect Dis. 2000 Sep;31 Suppl 3:S71–S74. doi: 10.1086/314075. Available from: http://dx.doi.org/10.1086/314075. [DOI] [PubMed] [Google Scholar]
- 12.Nahid P, Pai M, Hopewell PC. Advances in the diagnosis and treatment of tuberculosis. Proc Am Thorac Soc. 2006;3(1):103–110. doi: 10.1513/pats.200511-119JH. Available from: http://dx.doi.org/10.1513/pats.200511-119JH. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pai M, Kalantri S, Dheda K. New tools and emerging technologies for the diagnosis of tuberculosis: part I. Latent tuberculosis. Expert Rev Mol Diagn. 2006 May;6(3):413–422. doi: 10.1586/14737159.6.3.413. Available from: http://dx.doi.org/10.1586/14737159.6.3.413. [DOI] [PubMed] [Google Scholar]
- 14.Andersen P, Munk ME, Pollock JM, Doherty TM. Specific immune-based diagnosis of tuberculosis. Lancet. 2000 Sep;356(9235):1099–1104. doi: 10.1016/S0140-6736(00)02742-2. Available from: http://dx.doi.org/10.1016/S0140-6736(00)02742-2. [DOI] [PubMed] [Google Scholar]
- 15.Diel R, Goletti D, Ferrara G, Bothamley G, Cirillo D, Kampmann B, Lange C, Losi M, Markova R, Migliori GB, Nienhaus A, Ruhwald M, Wagner D, Zellweger JP, Huitric E, Sandgren A, Manissero D. Interferon-γ release assays for the diagnosis of latent Mycobacterium tuberculosis infection: a systematic review and meta-analysis. Eur Respir J. 2011 Jan;37(1):88–99. doi: 10.1183/09031936.00115110. Available from: http://dx.doi.org/10.1183/09031936.00115110. [DOI] [PubMed] [Google Scholar]
- 16.Murad MA, Abdulmageed SS. Tuberculosis screening among health sciences students in Saudi Arabia in 2010. Ann Saudi Med. 2012 Sep-Oct;32(5):527–529. doi: 10.5144/0256-4947.2012.527. Available from: http://dx.doi.org/10.5144/0256-4947.2012.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.El-Hazmi MM, Al-Otaibi FE. Predictors of pulmonary involvement in patients with extra-pulmonary tuberculosis. J Family Community Med. 2012 May;19(2):88–92. doi: 10.4103/2230-8229.98287. Available from: http://dx.doi.org/10.4103/2230-8229.98287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Asaad AM, Alqahtani JM. Primary anti-tuberculous drugs resistance of pulmonary tuberculosis in Southwestern Saudi Arabia. J Infect Public Health. 2012 Aug;5(4):281–285. doi: 10.1016/j.jiph.2012.03.005. Available from: http://dx.doi.org/10.1016/j.jiph.2012.03.005. [DOI] [PubMed] [Google Scholar]