Abstract
In recent years there have been major advances in the treatment of breast cancer. However, taking the prescribed medication for a sufficient period of time is crucial to the success of any therapy. Thus far, no database-based studies have been published in German-speaking countries empirically examining the influence of the physician on the compliance of patients. The aim of this study is to investigate, quantify, and critically discuss the effect treating physicians have on the compliance of their breast cancer patients.
Patients with a confirmed breast cancer diagnosis who started therapy (tamoxifen or aromatase inhibitors) between January 2001 and December 2011 were selected from the representative IMS Disease Analyzer database and analyzed with regard to their compliance. Practices were grouped into two categories concerning the compliance of all treated patients. A regression model showed that a breast cancer patient who is treated in a practice with a trend toward poor compliance has a nearly 60% higher risk for treatment discontinuation than would be the case in a practice with good compliance. It shows how important it is to motivate physicians to strive toward good compliance rates.
Keywords: breast cancer, compliance, persistence, Disease Analyzer
Zusammenfassung
In den letzten Jahren gab es wichtige Fortschritte in der Brustkrebs-Behandlung. Jedoch ist die regelmäßige Einnahme des verordneten Medikamentes über einen ausreichenden Zeitraum entscheidend für den Therapieerfolg. Bisher gibt es im deutschsprachigen Raum keine datenbankbasierten Studien, die den Einfluss des Arztes auf die Compliance seiner Patienten empirisch untersuchen. In der vorliegenden Studie wurde der Einfluss behandelnder Ärzte auf die Compliance ihrer Brustkrebspatientinnen untersucht und diskutiert. Basis der Analyse war die repräsentative Disease Analyzer Datenbank von IMS Health. Patientinnen mit der gesicherten Diagnose Brustkrebs im Zeitraum 01/2001–12/2011, die mit einer Therapie (Tamoxifen bzw. Aromatasehemmer) begonnen haben, wurden selektiert und hinsichtlich ihrer Compliance ausgewertet. Praxen wurden im Bezug auf Compliance aller in diesen Praxen behandelten Patientinnen in zwei Kategorien unterteilt. Aus dem Regressionsmodel hat sich ergeben, dass Brustkrebspatienten, die in Praxis mit tendenziell schlechter Compliance behandelt werden, ein fast 60% höheres Risiko für den Therapieabbruch aufweisen, als es in Praxen mit guter Compliance der Fall ist. Es ist deswegen dringlich notwendig, Ärzte zu motivieren, für die Compliance ihrer Patienten zu sorgen.
Background
Breast cancer is the most common cancer type in women. In Germany, about 71,600 women were diagnosed with breast cancer in 2008 with about 17,000 deaths attributed to it [1]. This corresponds to approximately 30% of new cancer cases and 15% of cancer-related deaths [2].
In recent years there have been major advances in the treatment of breast cancer. Today, thanks to improved surgical methods and modern drugs, a large number of patients can be cured. To reduce the risk of recurrence, after the surgical removal of the carcinoma, affected patients receive adjuvant therapy with tamoxifen or aromatase inhibitors for a period of five years. The drug tamoxifen has proven successful as an adjuvant therapy after surgical tumor removal in pre-menopausal women and is considered the standard drug for antihormonal therapy and reduces the number of breast cancer recurrence by half [3], [4].
Aromatase inhibitors are used predominantly in post-menopausal women. Many studies have shown that the application of aromatase inhibitors is superior to that of tamoxifen [5], [6], [7], [8].
The regular intake of the prescribed medication for a sufficient period of time is crucial to the success of therapy [9], [10]. The extent to which a patient takes the medication as prescribed by her physician is known as compliance [11]. While compliance was originally understood to mean the passive obedience of the patient with regard to her treatment, it is now considered to include the communicative, cooperative exchange between a doctor and patient which focuses on the willingness of the patient to cooperate with the doctor and to participate in diagnostic and therapeutic measures [12]. Non-compliance with medical treatment instructions may not only have a very negative impact on the patient’s health and even lead to death, but may also carry severe economic consequences. Estimates suggest that non-compliance results in costs of up to € 7.5–10 billion per year [13], [14]. For this reason, non-compliance can be seen as one of the major problems in the care of chronically ill patients [15].
Non-compliance results not only from a lack of discipline on the part of the patient, but reveals the disturbed equilibrium in the doctor-patient relationship. An important consideration resulting in non-compliance relates to the communication between a physician and a patient. Factors that may lead to ineffective doctor-patient communication include, for example, inadequate information about the importance of treatment, potential side effects of a treatment or medication, the chances of recovery, treatment alternatives, etc. or a lack of satisfaction with the doctor, which may lead the patient to question his/her orders [12].
Although the number of studies on compliance in the adjuvant treatment of breast cancer has increased in recent years [16], most of them are based on relatively small numbers of patients [17]. Thus far, no database-based studies have been published in German-speaking countries empirically examining the influence of the physician on the compliance of his/her patients.
The present study aims to close this gap. The aim of this study was to investigate, quantify, and critically discuss the effect treating physicians have on the compliance of their breast cancer patients.
Research design
Database
The IMS Disease Analyzer database was used as the data source for this retrospective cohort study. The data contained in the Disease Analyzer are generated directly from the practice computer via standardized interfaces and provide information about the actual therapy and disease progression in the everyday operations of the practice. Patients and practices can be analyzed both cross-sectionally and longitudinally. Longitudinal analyses document patient histories that in Germany date back to 1992. Overall, the German database currently contains information from more than 3,000 practices with a total of 20 million patients. The basis of the Disease Analyzer patient database is the population of all physicians that is published annually by the German Medical Association. From this population, the panel design is determined using the following stratification criteria: professional group, federal state, community size, and age. The database contains only anonymized data in accordance with privacy policies. Previous analyses carried out in comparison with accepted reference statistics have demonstrated that the Disease Analyzer patient database is sufficiently representative and valid [18], [19].
Patient selection
The study included all patients with a confirmed breast cancer diagnosis (ICD 10: C50) who started therapy (tamoxifen or aromatase inhibitors) in the period between January 2001 and December 2011. These patients were either treated in gynecological practices or in primary care practices.
Definitions
Persistence is an important feature for determining compliance. Persistence refers to the period in which the patient complies with the recommended intake of medication [20]. In the present study, the end of persistence was defined by a gap of ≥180 days without treatment in patients who were still observable by the same doctor in the time after this gap.
Longer periods were considered gaps and the treatment of the patient was no longer classified as persistent (follow-up of up to three years). Each patient was assigned to one of the two groups depending on her persistence: the group of patients who were treated continuously for at least three years and the group of patients who discontinued treatment. Discontinuation of treatment was confirmed only if the patient visited the practice again after a treatment-free interval of at least 180 days.
The proportion of breast cancer patients who discontinued treatment compared to those who did not was calculated for each practice. To obtain meaningful results, the analysis was restricted to those practices in which at least ten patients were being treated with tamoxifen or aromatase inhibitors. Practices were divided in two categories based on the proportion of treatment dropouts: the percentage of dropouts was ≤50% (trend towards good compliance) versus the percentage of dropouts was >50% (trend towards poor compliance).
Statistical methods
To test the hypothesis that the probability of a patient discontinuing her treatment depends on the compliance category of her doctor, a multivariate Cox regression model was created. Discontinuation of therapy (1 for discontinuation and 0 for continuous treatment) was included as the dependent variable, while the compliance category of the treating practice served as an indicator variable. In addition, the region (Western versus Eastern Germany), community size (>100,000 versus <100,000 inhabitants), patient age, gender, medical specialty of the physician (gynecologist versus general practitioner), number of breast cancer patients receiving treatment in the practice, and co-diagnosis of depression were included as covariates. Data were analyzed using the statistical software package SAS version 9.2 (SAS Institute Inc., Cary, NC, USA). Two-sided tests were carried out and a p-value of <0.05 was considered statistically significant. Specific recommendations for retrospective database analyses were taken into account [21].
Presentation of results
Patient and practice characteristics
In total, 305 gynecological practices and 1,053 primary care practices were available. The study included 6,926 breast cancer patients who started adjuvant therapy with tamoxifen (N=4,359) or one of the three aromatase inhibitors (anastrozole, exemestane, letrozole) (N=2,567) between January 2001 and December 2011. In total, 3,785 patients were treated by a gynecologist and 3,141 by a general practitioner.
On average, a gynecological practice treated 14 breast cancer patients (minimum: 1, maximum: 105); general practitioners treated an average of 3 breast cancer patients (minimum: 1, maximum: 44).
After exclusion of practices with fewer than 10 breast cancer patients, 149 gynecologists with 3,103 patients and 24 general practitioners with 321 patients remained for analysis.
Based on our criteria, 98 practices were assigned to the group exhibiting a trend towards good compliance (percentage of dropouts ≤50%) and 75 practices were assigned to the group exhibiting a trend towards poor compliance (percentage of dropouts >50%).
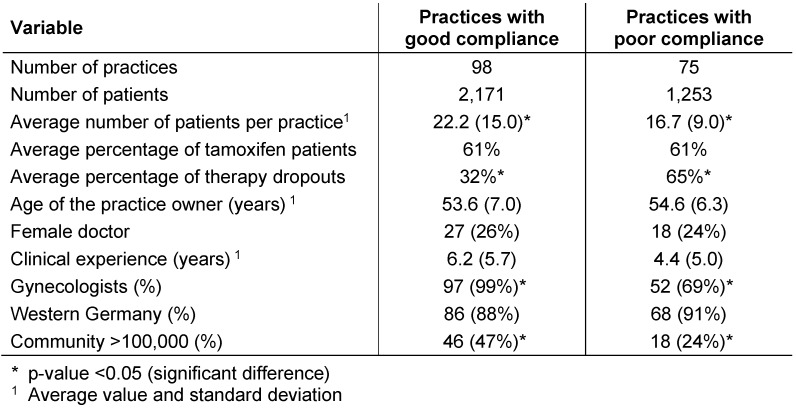
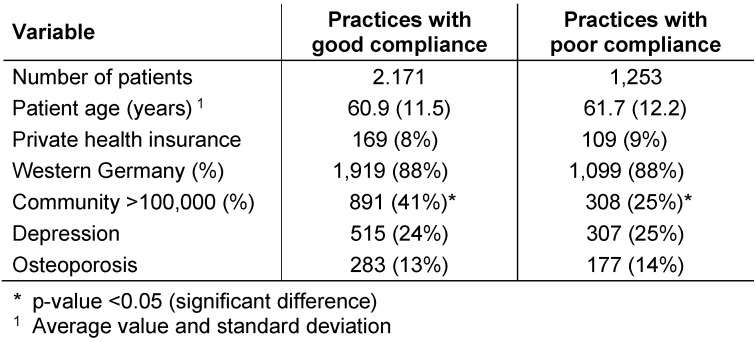
Table 1 (Tab. 1) lists practice characteristics and Table 2 (Tab. 2) lists patient characteristics for both compliance categories. The good compliance category included significantly more gynecologists than the poor compliance group; in addition, practices with good compliance had significantly more breast cancer patients per practice (22.2 versus 16.7). Practices with good compliance were more common in urban areas (>100,000 inhabitants). No differences between the two practice categories were found regarding the age of the practice owner, their clinical experience in treating breast cancer patients, or their gender. The patients treated in both practice groups were identical in relation to age and insurance status.
Table 1. Baseline characteristics of the practices included in the study.
Table 2. Baseline characteristics of patients included in the study.
Discontinuation of treatment
In those practices that were categorized as exhibiting good compliance, 68% of breast cancer patients remained in therapy for at least three years, while only 35% in practices with poor compliance did so (p<0.01). As can be seen from the Kaplan-Meier curve (Figure 1 (Fig. 1)), 19% of patients in practices with good compliance and 41% of patients in practices with poor compliance discontinued treatment as early as their first year of treatment. This means that more than 60% of dropouts did not continue therapy beyond the first year of treatment.
Figure 1. Kaplan-Meier curves of treatment time for adjuvant treatment over a three-year period in breast cancer outpatients.
Regression analyses
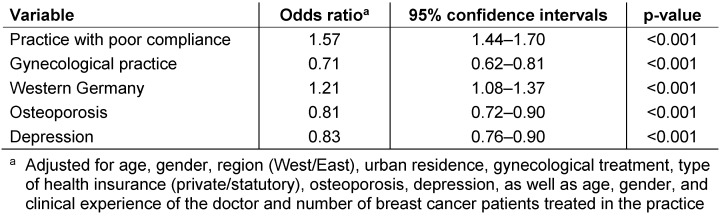
The results of the Cox regression model (Table 3 (Tab. 3)) show that those breast cancer patients who were treated in practices with poor compliance have a significantly higher risk of discontinuing treatment than patients in practices with good compliance (HR: 1.57; p<0.001). No significant differences were found for the demographic characteristics of the physician (age and gender) or his/her clinical experience in treating breast cancer patients. Patients seen in gynecological practices exhibited a lower risk for the discontinuation of treatment compared to patients treated by general practitioners. In addition, patients in Western Germany discontinued their treatment significantly more often. Co-diagnoses such as osteoporosis and depression had a positive effect on compliance.
Table 3. Relationship between practice category and early termination of adjuvant therapy (Cox regression).
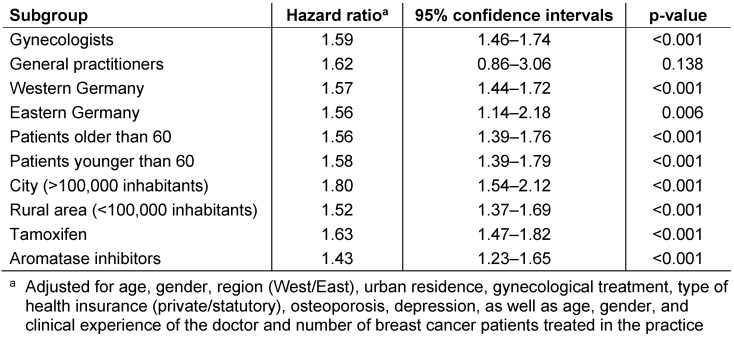
If we consider the impact of the compliance category on the risk of treatment discontinuation in various subgroups (Table 4 (Tab. 4)), we see that this influence is almost identical in all subgroups examined, with the highest hazard ratio found among physicians or patients in communities with >100,000 inhabitants.
Table 4. Relationship between practice category and early termination of adjuvant therapy in defined subgroups (Cox regression).
Discussion of results
More than half of breast cancer patients interrupt their adjuvant therapy early, the majority of them within the first year of treatment. This finding is not new. Several other studies reported similar numbers [17], [22], [23], [24], [25], [26], [27], [28].
A further analysis of the factors leading to the discontinuation of treatment is interesting, however. While earlier studies dealt exclusively with the patients’ behavior and the resulting consequences for compliance [29], later studies focused on the role of the physician. In the 1970s and 1980s, it was initially assumed that factors such as level of education, intelligence, social status, and ethnicity of the patient impacted compliance. The majority of studies did not, however, confirm this. The role of the physician was insufficiently examined at the time. Later studies found that the physicians have a significant impact on patient compliance. This corresponds with today’s view of the medical profession, according to which doctors and patients meet as equals [30]. Today, compliance research aims to view non-compliance from the perspective of the patient. Thus, the primary goal is to find out what changes must be made from the patient’s perspective so that she remains compliant [29]. This is reflected in the concept of adherence, which focuses more on a cooperative doctor-patient relationship and incorporates those factors that determine compliance from the perspective of the patient.
After evaluating various studies on compliance, Hadji et al. list therapy-related, patient-related, and socio-economic factors as important reasons for non-compliance. The essential component of non-compliance is the communication and exchange of information between physician and patient [20].
Clear communication of the seriousness of the situation, the usefulness of the treatment, and its side effects is important. The physician must engage with the patient and communicate with her to motivate her to correctly take her medication as prescribed. Practical advice is essential for compliance and may include, for example, keeping an intake diary for self-monitoring. In addition, a written reminder, a call, or other aids, such as a pillbox can all help the patient to comply. Involvement of the family in treatment is another motivator mentioned. Furthermore, the physician should praise patients with good compliance and acknowledge their behavior. This motivates the patient to be compliant even during difficult phases.
Other studies have reached similar conclusions regarding the importance of the doctor-patient relationship for compliance. Reports of the German Institute for Medical Documentation and Information (DIMDI) indicate that the patient must accept the treatment and be convinced of its benefits as factors positively influencing compliance. In addition, she must be satisfied with the medical advice and care and should receive support from her social environment. A poor doctor-patient relationship, lack of confidence in the doctor or treatment, insufficient information, or problems with taking the medication are again considered as factors negatively influencing compliance [31], [32].
As illustrated by research, each patient exhibits different compliance behavior. If compliance were only due to patient characteristics, one would expect the proportion of treatment dropouts to be the same or at least similar in each practice. Using the example of breast cancer treatment, the present study demonstrates, however, that the proportion of treatment dropouts varies widely from practice to practice, allowing for the differentiation of practice into two categories. Practices and patients in both categories exhibited no major differences in terms of the demographic characteristics examined, with the exception of two important variables for which the differences are particularly noticeable: Most practices with good compliance are gynecological clinics. In contrast, this group (with a trend towards good compliance) contains only a few primary care practices. This result may indicate a relationship between the specialization of the physician and compliance. In addition, the first group comprises a much greater number of patients, pointing to a greater degree of practical experience of the doctor and a possible correlation with better compliance.
A definite statement regarding the influence of the physician on the patient’s compliance can be made based on the results of the regression analyses. Patients treated in a practice with poor compliance have a nearly 60% higher risk for discontinuing therapy than would be the case in a practice with good compliance. Since this effect was adjusted for a number of other variables, it is a direct measure of the physician’s influence. The hypothesis that the physician has an impact on compliance is thus supported by empirical, quantitative data.
Limitations
The present study is a retrospective study based on a large epidemiological database. Such studies are subject to certain limitations. These include the fact that the data map only individual practices and that patient histories cannot be represented. The analyses presented are, thus, only an excerpt of the entire treatment process (the same holds true for the number of prescriptions per patient). Moreover, it is not possible to draw conclusions about the degree of networking between various specialist groups. This fact may also be the reason why patients exhibit poorer compliance at general practitioners’ offices, since the general practitioner may be responsible for only part of the treatment in certain cases and the patient may be treated by her gynecologist more regularly.
Another limitation consists in the fact that the database contains only the age and gender of the practice owner but not that of the treating physician. As some of the practices were group practices, however, adequate examination of this variable was not possible. The real reasons for the discontinuation of treatment, therefore, warrant further analysis to reach definite conclusions.
It may be noted, however, that patients who are treated in a practice with good compliance have a significantly better chance of completing treatment. It shows how important it is to motivate physicians to strive toward good compliance rates. This not only reduces unnecessary follow-up costs for the healthcare system, but also and above all has positive effects on patient well-being and health.
Notes
Competing interests
The authors declare that they have no competing interests.
References
- 1.Zentrum für Krebsregisterdaten am Robert Koch Institut. Krebs in Deutschland. ICD-10 C50 (Brustdrüse) [accessed August 20, 2012]. Available from: http://www.krebsdaten.de/Krebs/DE/Home/Datenbankabfrage/datensaetze_gesamt_tabelle.html.
- 2.Ferlay J, Parkin DM, Steliarova-Foucher E. Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer. 2010 Mar;46(4):765–781. doi: 10.1016/j.ejca.2009.12.014. Available from: http://dx.doi.org/10.1016/j.ejca.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 3.Carlson RW, Allred DC, Anderson BO, Burstein HJ, Carter WB, Edge SB, Erban JK, Farrar WB, Goldstein LJ, Gradishar WJ, Hayes DF, Hudis CA, Jahanzeb M, Kiel K, Ljung BM, Marcom PK, Mayer IA, McCormick B, Nabell LM, Pierce LJ, Reed EC, Smith ML, Somlo G, Theriault RL, Topham NS, Ward JH, Winer EP, Wolff AC NCCN Breast Cancer Clinical Practice Guidelines Panel. Breast cancer. Clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2009 Feb;7(2):122–192. doi: 10.6004/jnccn.2009.0012. [DOI] [PubMed] [Google Scholar]
- 4.Early Breast Cancer Trialists' Collaborative Group (EBCTCG) Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005 May 14-20;365(9472):1687–1717. doi: 10.1016/S0140-6736(05)66544-0. Available from: http://dx.doi.org/10.1016/S0140-6736(05)66544-0. [DOI] [PubMed] [Google Scholar]
- 5.Rao RD, Cobleigh MA. Adjuvant endocrine therapy for breast cancer. Oncology (Williston Park, NY) 2012 Jun;26(6):541–7, 550, 552 passim. [PubMed] [Google Scholar]
- 6.Burstein HJ, Prestrud AA, Seidenfeld J, Anderson H, Buchholz TA, Davidson NE, Gelmon KE, Giordano SH, Hudis CA, Malin J, Mamounas EP, Rowden D, Solky AJ, Sowers MR, Stearns V, Winer EP, Somerfield MR, Griggs JJ American Society of Clinical Oncology. American Society of Clinical Oncology clinical practice guideline: update on adjuvant endocrine therapy for women with hormone receptor-positive breast cancer. J Clin Oncol. 2010 Aug;28(23):3784–3796. doi: 10.1200/JCO.2009.26.3756. Available from: http://dx.doi.org/10.1200/JCO.2009.26.3756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howell A, Cuzick J, Baum M, Buzdar A, Dowsett M, Forbes JF, Hoctin-Boes G, Houghton J, Locker GY, Tobias JS ATAC Trialists’ Group. Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet. 2005 Jan 1-7;365(9453):60–62. doi: 10.1016/S0140-6736(04)17666-6. [DOI] [PubMed] [Google Scholar]
- 8.Forbes JF, Cuzick J, Buzdar A, Howell A, Tobias JS, Baum M Arimidex, Tamoxifen, Alone or in Combination (ATAC) Trialists’ Group. Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 100-month analysis of the ATAC trial. Lancet Oncol. 2008 Jan;9(1):45–53. doi: 10.1016/S1470-2045(07)70385-6. Available from: http://dx.doi.org/10.1016/S1470-2045(07)70385-6. [DOI] [PubMed] [Google Scholar]
- 9.Balkrishnan R. The importance of medication adherence in improving chronic-disease related outcomes: what we know and what we need to further know. Med Care. 2005 Jun;43(6):517–520. doi: 10.1097/01.mlr.0000166617.68751.5f. Available from: http://dx.doi.org/10.1097/01.mlr.0000166617.68751.5f. [DOI] [PubMed] [Google Scholar]
- 10.Davidson B, Vogel V, Wickerham L. Oncologist-patient discussion of adjuvant hormonal therapy in breast cancer: results of a linguistic study focusing on adherence and persistence to therapy. J Support Oncol. 2007 Mar;5(3):139–143. [PubMed] [Google Scholar]
- 11.Schäfer C. Patientencompliance – Messung, Typologie, Erfolgsfaktoren. 1. ed. Wiesbaden: Gabler; 2011. pp. 21–33. Available from: http://dx.doi.org/10.1007/978-3-8349-6334-5. [DOI] [Google Scholar]
- 12.Leunikava I. Wissentransfer in medizinischen Packungsbeilagen. Was verstehen Patienten? Hamburg: Diplomica; 2011. p. 11. [Google Scholar]
- 13.Gräf M. Die volkswirtschaftlichen Kosten der Non-Compliance: Eine entscheidungsorientierte Analyse. Bayreuth: P.C.O. Verlag; 2007. (Schriften zur Gesundheitsökonomie; 56). [Google Scholar]
- 14.Volmer T, Kielhorn A. Kosten der Non-Compliance. Gesundhökon Qualmanag. 1999;4:55–61. [Google Scholar]
- 15.World Health Organization. Adherence to long-term therapies: Evidence for action. Geneva: World Health Organization; 2003. Available from: http://whqlibdoc.who.int/publications/2003/9241545992.pdf. [Google Scholar]
- 16.Hadji P. Improving compliance and persistence to adjuvant tamoxifen and aromatase inhibitor therapy. Crit Rev Oncol Hematol. 2010 Feb;73(2):156–166. doi: 10.1016/j.critrevonc.2009.02.001. Available from: http://dx.doi.org/10.1016/j.critrevonc.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 17.Ziller V, Kalder M, Albert US, Holzhauer W, Ziller M, Wagner U, Hadji P. Adherence to adjuvant endocrine therapy in postmenopausal women with breast cancer. Ann Oncol. 2009 Mar;20(3):431–436. doi: 10.1093/annonc/mdn646. Available from: http://dx.doi.org/10.1093/annonc/mdn646. [DOI] [PubMed] [Google Scholar]
- 18.Becher H, Kostev K, Schröder-Bernhardi D. Validity and representativeness of the “Disease Analyzer” patient database for use in pharmacoepidemiological andpharmacoeconomic studies. Int J Clin Pharmacol Ther. 2009 Oct;47(10):617–626. doi: 10.5414/CPP47617. Available from: http://dx.doi.org/10.5414/CPP47617. [DOI] [PubMed] [Google Scholar]
- 19.Ogdie A, Langan SM, Parkinson J, Dattani H, Kostev K, Gelfand JM. Medical Record Databases. In: Strom BL, Kimmel SE, Hennessy S, editors. Pharmacoepidemiology. 5th ed. Oxford: Wiley-Blackwell; 2012. pp. 224–243. Available from: http://dx.doi.org/10.1002/9781119959946.ch15. [DOI] [Google Scholar]
- 20.Hadji P, Ziller V, Kalder M, Torode J, Jackisch C. Non-Compliance in der adjuvanten endokrinen Therapie des Mammakarzinoms. Frauenarzt. 2007;48(2):146–150. [Google Scholar]
- 21.Motheral B, Brooks J, Clark MA, Crown WH, Davey P, Hutchins D, Martin BC, Stang P. A checklist for retrospective database studies – report of the ISPOR Task Force on Retrospective Databases. Value Health. 2003 Mar-Apr;6(2):90–97. doi: 10.1046/j.1524-4733.2003.00242.x. [DOI] [PubMed] [Google Scholar]
- 22.Partridge AH, LaFountain A, Mayer E, Taylor BS, Winer E, Asnis-Alibozek A. Adherence to initial adjuvant anastrozole therapy among women with early-stage breast cancer. J Clin Oncol. 2008 Feb;26(4):556–562. doi: 10.1200/JCO.2007.11.5451. Available from: http://dx.doi.org/10.1200/JCO.2007.11.5451. [DOI] [PubMed] [Google Scholar]
- 23.Sedjo RL, Devine S. Predictors of non-adherence to aromatase inhibitors among commercially insured women with breast cancer. Breast Cancer Res Treat. 2011 Jan;125(1):191–200. doi: 10.1007/s10549-010-0952-6. Available from: http://dx.doi.org/10.1007/s10549-010-0952-6. [DOI] [PubMed] [Google Scholar]
- 24.Partridge AH, Wang PS, Winer EP, Avorn J. Nonadherence to adjuvant tamoxifen therapy in women with primary breast cancer. J Clin Oncol. 2003 Feb 15;21(4):602–606. doi: 10.1200/JCO.2003.07.071. [DOI] [PubMed] [Google Scholar]
- 25.Huiart L, Bouhnik AD, Rey D, Tarpin C, Cluze C, Bendiane MK, Viens P, Giorgi R. Early discontinuation of tamoxifen intake in younger women with breast cancer: is it time to rethink the way it is prescribed? Eur J Cancer. 2012 Sep;48(13):1939–1946. doi: 10.1016/j.ejca.2012.03.004. Available from: http://dx.doi.org/10.1016/j.ejca.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 26.Wigertz A, Ahlgren J, Holmqvist M, Fornander T, Adolfsson J, Lindman H, Bergkvist L, Lambe M. Adherence and discontinuation of adjuvant hormonal therapy in breast cancer patients: a population-based study. Breast Cancer Res Treat. 2012 May;133(1):367–373. doi: 10.1007/s10549-012-1961-4. Available from: http://dx.doi.org/10.1007/s10549-012-1961-4. [DOI] [PubMed] [Google Scholar]
- 27.Nekhlyudov L, Li L, Ross-Degnan D, Wagner AK. Five-year patterns of adjuvant hormonal therapy use, persistence, and adherence among insured women with early-stage breast cancer. Breast Cancer Res Treat. 2011 Nov;130(2):681–689. doi: 10.1007/s10549-011-1703-z. Available from: http://dx.doi.org/10.1007/s10549-011-1703-z. [DOI] [PubMed] [Google Scholar]
- 28.Danilak M, Chambers CR. Adherence to adjuvant endocrine therapy in women with breast cancer. J Oncol Pharm Pract. 2013 Jun;19(2):105–110. doi: 10.1177/1078155212455939. Available from: http://dx.doi.org/10.1177/1078155212455939. [DOI] [PubMed] [Google Scholar]
- 29.Möbes J. Compliance: Neue Positionen am Beispiel des Diabetes mellitus. Z Allg Med. 2003;79(5):238–243. doi: 10.1055/s-2003-40715. Available from: http://dx.doi.org/10.1055/s-2003-40715. [DOI] [Google Scholar]
- 30.Gießen H. Der „Halbgott in Weiß“ hat ausgedient. [accessed 24.12.2012];Pharm Z. 2011 (19) Available from: http://www.pharmazeutische-zeitung.de/index.php?id=37827. [Google Scholar]
- 31.Gorenoi V, Schönermark MP, Hagen A. Maßnahmen zur Verbesserung der Compliance bzw. Adherence in der Arzneimitteltherapie mit Hinblick auf den Therapieerfolg. Köln: DIMDI; 2007. (Schriftenreihe Health Technology Assessment; 65). Available from: http://portal.dimdi.de/de/hta/hta_berichte/hta206_bericht_de.pdf. [Google Scholar]
- 32.Thiel I. Bedeutung von Compliance/Adherence für eine erfolgreiche Brustkrebstherapie. Facharzt Gynäkologie/Urologie. 2010;19(2):4–5. Available from: http://www.mediziner.at/upload/2317158_FACHARZT_Gynkologie_Urologie_2_2010.pdf. [Google Scholar]