Abstract
Objectives
To explore current practices and opinions regarding hospital management of Parkinson disease (PD) patients in specialized PD Centers.
Methods
Fifty-one out of 54 National Parkinson Foundation (NPF) Centers worldwide completed an online survey regarding hospitalization of PD patients.
Results
Many Centers were concerned about the quality of PD-specific care provided to their patients when hospitalized. Primary concerns were adherence to the outpatient medication schedule and poor understanding by hospital staff of medications that worsen PD. Few Centers had a policy with their primary hospital that notified them when their patients were admitted. Rather, notification of hospitalization came often from the patient or a family member. Several Centers (29%) reported not finding out about a hospitalization until a routine clinic visit after discharge. Quick access to outpatient PD care following discharge was a problem in many Centers. Elective surgery, fall/fracture, infection, and mental status changes, were identified as common reasons for hospitalization.
Conclusions
There is a perceived need for PD specialists to be involved during hospitalization of their patients. Improvement in communication between hospitals and PD Centers is necessary so that hospital clinicians can take advantage of PD specialists’ expertise. Education of hospital staff and clinicians regarding management of PD, complications of PD, and medications to avoid in PD is critical. Most importantly, outpatient access to PD specialists needs to be improved, which may prevent unnecessary hospitalizations in these patients.
Keywords: Parkinson’s disease, Hospitalization, Complications, Deep brain stimulation, International care
1. Introduction
Parkinson disease (PD) is a progressive neurological disorder that currently affects between 4.1 and 4.6 million individuals over the age of 50 worldwide, a number expected to double by the year 2030 [1]. Because dopaminergic medications are effective for the motor symptoms of PD, patients in the early stages generally do not require emergency treatment or hospitalization for their PD symptoms [2]. As PD advances, dyskinesias, motor fluctuations, falls and non-motor manifestations such as cognitive impairment and treatment related psychosis become more prominent [3] and may lead to hospitalization [4–6]. Since PD typically affects an older population, these patients also commonly suffer from comorbid conditions that may independently require hospitalization [7–9]. Hospitalization rates of patients with parkinsonism are 1.45 times higher than for age-matched controls [7,10]. Furthermore, PD patients with moderate to advanced disease may have special needs, such as precise timing of medications to avoid wearing off, that may be difficult to accommodate in a hospital setting. Currently, PD is commonly managed in the outpatient setting by general neurologists or movement disorder specialists, who are often not consulted when PD patients are hospitalized. Non-neurologists working in a hospital setting generally have had little experience with this complex condition, which may further impact care of hospitalized PD patients. Questions remain as to how PD is managed in an inpatient setting, and few publications exist that address the issue of hospitalization in PD patients.
Based on a survey of attendees of the 2010 Young Onset Parkinson’s Conference sponsored by the National Parkinson Foundation (NPF), hospitalization was identified as a major issue in the patient community. To address this, the NPF formed a committee to conduct a survey of NPF Centers, including both Centers of Excellence (COE) and Care Consortium Centers (CCC). The goal was to explore current practices and opinions at NPF Centers regarding hospitalization of PD patients.
2. Methods
2.1. Survey design
An internet-based survey was developed by the NPF Hospitalization Writing Committee and placed online using Survey Monkey (www.SurveyMonkey.com, Portland, OR). The survey was based on practice gaps identified from a literature search on the management of the hospitalized PD patient as well as a non-peer-reviewed article aimed at improving the hospitalization experience of PD patients [11]. The full survey is included in an online appendix to this article. The 54 NPF Centers in the network, comprised of 43 COEs and 11 CCCs around the world, were invited to complete the survey online. Of the 54 Centers invited to participate, all of the 43 COEs and 8 of the 11 (73%) CCCs submitted responses.
COEs are selected by a peer-reviewed process on the basis of their ongoing research, comprehensive care delivery, and professional education and patient outreach services. CCCs have to meet similar criteria except in the area of research. Hereafter, the term “Centers” refers to both COEs and CCCs. Thirty-five of these Centers (28 COEs and 7 CCCs) are located within the United States (US Centers), and 16 (15 COEs and 1 CCC) are outside the US (International Centers). Combined, these Centers care for over 50,000 PD patients worldwide.
One individual from each Center was asked to respond to the survey, and the survey respondent was instructed to reflect the experience at the Center rather than personal opinion. The respondents were 32 physicians, 17 nurses/nurse practitioners, and 3 allied health personnel (i.e. social work, therapists, etc). The survey took approximately 15 min to complete and was posted for 2 months.
2.2. Statistical analyses
Descriptive statistics were used to summarize the results of the survey, and comparisons between US and International Centers were performed using Fisher’s exact test. Data were analyzed using SPSS v. 17.0 (SPSS Inc., Chicago, IL).
3. Results
3.1. Perceptions of hospital care for PD patients
Most centers were not confident about the quality of PD-specific care provided to their patients when hospitalized (Table 1). The majority of Centers (94%) were not confident that patients received medications on time when hospitalized. Also Centers were not confident that hospital professionals had general knowledge regarding more complex PD-specific contraindicated therapies; 71% were not confident that hospital staff knew that anti-emetics such as metoclopramide and prochlorperazine could worsen PD motor symptoms, and 80% were not confident that physicians knew clozapine and quetiapine were the least likely antipsychotics to worsen PD symptoms. The majority of Centers (72%) were confident that hospital staff knew that infections could cloud mental status. About half of Centers were confident that hospital staff knew that PD medications such as dopamine agonists, amantadine, and anticholinergics could affect mental status and that reducing these medications could improve psychosis and other behavioral issues.
Table 1.
PD specialists perception of PD patient hospital care.
| US Centers (n = 34a) |
International Centers (n = 16) |
Total C or VC (n = 50) |
|||||
|---|---|---|---|---|---|---|---|
| VC | C | NC | VC | C | NC | # (%) | |
| How confident are you that non-neurologists caring for PD patients in the hospital know: | |||||||
| That infections such as UTI’s can cloud mental status? | 8 | 18 | 8 | 2 | 8 | 6 | 36 (72) |
| That dopamine agonists, amantadine, and anticholinergics can cloud mental status? | 2 | 13 | 19 | 2 | 5 | 9 | 22 (44) |
| That reducing dopaminergic medications may improve hallucinations and behavioral issues? | 1 | 14 | 19 | 2 | 7 | 7 | 24 (48) |
| That metoclopramide and prochlorperazine make PD symptoms worse?b | 0 | 10 | 23 | 1 | 3 | 12 | 14 (29) |
| That quetiapine and clozapine are the safest antipsychotics in PD? | 0 | 4 | 30 | 1 | 5 | 10 | 10 (20) |
| That confident are you that PD patients get their medications on time? | 0 | 2 | 32 | 0 | 1 | 15 | 3 (6) |
VC = very confident; C = confident; NC = not confident; UTI = urinary tract infection.
1 US Center did not respond to this section.
Only 33 US Centers responded to this question.
3.2. Admission, hospitalization and discharge
Most NPF Centers (76%) admit PD patients more often to their own hospitals than outside hospitals (Table 2). For unplanned admissions or emergency room visits, few Centers (25%) had a mechanism in place that would trigger a call from the hospital physician to their Center. At 61% of the Centers, this was addressed by asking patients to have the emergency department (ED) contact their clinic when they presented for evaluation. Centers typically learned about a patient’s hospitalization at the actual time of admission (33%) or during hospitalization (47%). Notification of hospitalization came more often from the patient or family (71%) than from physicians (57%). Twenty-nine percent of the Centers learned about hospitalization at a follow-up clinical visit. If admitted to a Center’s own hospital, primary PD clinicians were involved in their hospital care either directly (63%), or less often, by phone consultation (26%).
Table 2.
Hospitalization statistics.
| US Centers (n = 35) |
International Centers (n = 16) |
|||
|---|---|---|---|---|
| # | % | # | % | |
| How many Centers admit PD patients more often to own hospital vs. other hospital? | 27 | 77 | 12 | 75 |
| How many Centers instruct patients who present to the ER to have the ER contact the PD clinic? | 21 | 60 | 10 | 63 |
| How many Centers have a mechanism in place that will trigger a call from the hospital physician to the Center if their PD patient is admitted? | 9 | 26 | 4 | 25 |
| When does your Center learn about a patient’s hospitalization?a | ||||
| Before admission | 8 | 23 | 6 | 38 |
| At time of admission | 12 | 34 | 5 | 31 |
| During hospitalization | 18 | 51 | 6 | 38 |
| After discharge | 9 | 26 | 3 | 19 |
| How do you learn about a patient’s hospitalization?a | ||||
| Phone call from another MD | 18 | 51 | 11 | 69 |
| Phone call from patient/family | 22 | 63 | 14 | 88 |
| Automatic/electronic notification | 4 | 11 | 5 | 31 |
| Don’t learn until patient follows up in clinic | 10 | 29 | 5 | 31 |
| For PD cases admitted to the hospital from your practice, are your center’s neurologists or nurse practitioners:a | ||||
| Directly/physically involved | 20 | 57 | 12 | 75 |
| Involved by phone | 10 | 29 | 3 | 19 |
| Not usually involved | 3 | 9 | 2 | 13 |
| Involved during follow-up | 5 | 14 | 2 | 13 |
For these questions, respondents could answer multiple options.
Approximately half of the Centers (45%) could admit patients electively for medication management, 53% could admit electively for behavioral management and 59% could admit electively for rehabilitation programs (Table 3). A greater percentage of Centers (80%) could send patients to acute inpatient rehabilitation after hospitalization. For these items, there were no significant differences in responses between US and International Centers. At 66% of Centers, patients could be seen within 2 weeks of hospital discharge. More international (75%) than US Centers (43%) responded that they had an incentive to provide readily available outpatient care in order to avoid admissions (p = 0.04). Despite such an incentive, many Centers had difficulty providing patients with readily available outpatient appointments. Significantly more international (38%) than US Centers (6%) responded that their earliest appointment for follow-up after hospital discharge was greater than 4 weeks (p = 0.008).
Table 3.
Admission and discharge policies.
| US Centers (n = 35) |
International Centers (n = 16) |
p value | |||
|---|---|---|---|---|---|
| # | % yes | # | % yes | ||
| Can your center: | |||||
| Admit patients electively for medication management? | 13 | 37 | 10 | 63 | 0.13 |
| Admit patients electively for behavioral management? | 17 | 49 | 10 | 63 | 0.38 |
| Admit patients electively for rehabilitation programs? | 23 | 66 | 7 | 44 | 0.22 |
| Send patients over for inpatient rehab after hospitalization for acute care? | 28 | 80 | 13 | 81 | 1.00 |
| How soon can patients be seen after hospital discharge for follow-up in your PD clinic? | |||||
| Within 1 week | 11 | 31 | 4 | 25 | 0.75 |
| Within 2 weeks | 14 | 40 | 5 | 31 | 0.76 |
| Within 4 weeks | 8 | 23 | 1 | 6 | 0.24 |
| Greater than 4 weeks | 2 | 6 | 6 | 38 | 0.008 |
| Is there an incentive to provide excellent and readily available outpatient care to try to avoid admissions? | 15 | 43 | 12 | 75 | 0.04 |
p values are <0.05.
3.3. Reasons for hospitalization of the PD patient
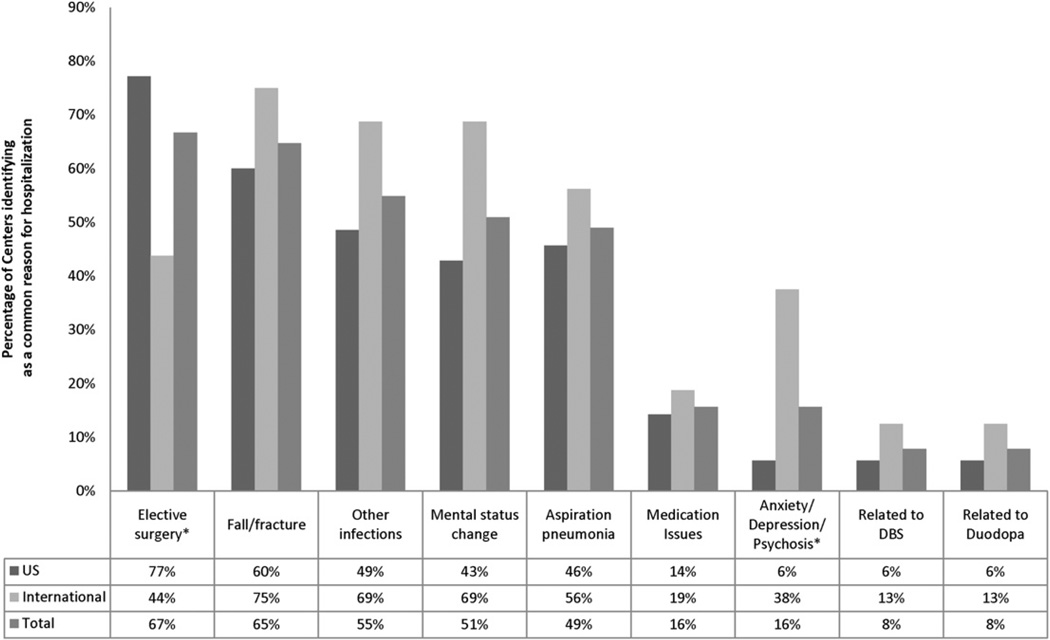
More than half of the Centers listed elective surgery, fall/fracture, infection unrelated to pneumonia, and mental status change as common reasons for hospitalization, while almost half of the Centers (49%) listed aspiration pneumonia (Fig. 1). More US Centers thought their patients were hospitalized for elective surgery than international Centers (77% vs. 44%, p = 0.03), while more international Centers identified psychiatric issues (anxiety/depression/psychosis) as more common reasons for hospitalization than US Centers (38% vs. 6%, p = 0.008). Admissions for deep brain stimulation (DBS) and intestinal levodopa infusions were uncommon.
Fig. 1.
Common reasons for hospitalization of PD patients. *p < 0.05.
3.4. DBS hospitalizations
Approximately 80% of NPF Centers perform DBS surgery (Table 4). Only 18% of Centers overall could admit patients to the hospital for prolonged initial programming, with no difference between US and International Centers. There were no differences between US and international Centers in the ability to admit for DBS programming issues, caring for patients implanted at other sites, or providing guidance on handling DBS issues.
Table 4.
Hospitalization for DBS.
| US Centers (n = 35) |
International Centers (n = 16) |
p value | |||
|---|---|---|---|---|---|
| # | % yes | # | % yes | ||
| Does your Center perform DBS surgery? | 28 | 80 | 13 | 81 | 1.00 |
| Can your Center have prolonged admissions for initial DBS programming? | 5 | 14 | 4 | 25 | 0.44 |
| Can your Center admit patients for management of DBS related programming issues? | 19 | 54 | 12 | 75 | 0.22 |
| If DBS patients are implanted at other Centers, are they allowed to come to your Center for care? | 32 | 91 | 13 | 81 | 0.36 |
| Is a member of your DBS team available to go to the hospital and check a hospitalized patient’s device, if hospitalized in your hospital system? | 30 | 86 | 13 | 81 | 0.69 |
| Is a member of your DBS team available to provide guidance to outside physicians/hospitals on handling the DBS device? | 32 | 91 | 13 | 81 | 0.36 |
4. Discussion
PD is generally managed in the outpatient setting, so hospitalbased clinicians, nurses and other hospital staff may be unfamiliar with the management of the complicated PD patient. The goal of this exploratory survey was to uncover current hospitalization practices for PD patients and to gather perceptions regarding the hospital management of PD patients across NPF Centers. The findings highlight several critical issues regarding inpatient PD care that need improvement.
Many NPF Centers have a catchment area significantly larger than that of their “home” hospital. Therefore, it is not uncommon for patients to travel long distances to see a PD specialist at an NPF Center, yet seek urgent care at a local medical facility. Only the establishment of broad regional communication systems will ensure that the treating PD specialist is notified of every hospitalization at the time of admission. In the absence of such a system, it is the patient’s and families’ responsibility to ensure that their treating neurologists are notified. In an attempt to ensure expert care, many Centers try to admit their PD patients to their “home” hospital, because PD expert staff and clinicians can be readily involved in that patient’s care. The survey found, however, that communication between Center staff and the hospital is not always consistent. Only a quarter of the participating Centers have a policy in their own hospital that would trigger a contact from the hospital to their office alerting them that their patient had presented for emergency evaluation. Moreover, many Centers have yet to implement a systematic process of patient education and engagement in the hospitalization process. Only 61% of Centers reported that they instructed patients to contact their PD Center if presenting to an ER. Therefore, based on this survey, one important step toward improving hospital care of the PD patient involves improving patient (and family) engagement as well as the implementation of a system to improve communication between both local and regional hospitals and PD Centers regarding ER visits and hospital admissions.
A surprising finding was how many Centers felt they could admit patients electively for medication management, behavioral management and rehabilitation. Admission for medication management was felt to be a viable option at 37% of US Centers. However, in the US, third-party payers may not pay for an elective hospitalization for “medication management”. A similar percentage (37.5%) of Canadian Centers replied that they could electively admit PD patients for medication management, though one Canadian Center indicated that lack of bed availability made elective admissions for medication management difficult in reality. Thus, it is likely that each individual filling out our survey had a different definition of an “elective” admission and that multiple factors influence the feasibility of such admissions. Outside the US and Canada, it may be easier to electively admit patients for medication management, and 7 of the 8 non-Canadian International Centers responded that they could do so. A study from Italy reported that the most frequent reason for admission in their PD patients was a planned hospital stay to adjust dopaminergic therapy [8]. An Australian study reported 116 of 761 PD admissions were performed for “confirming diagnosis…or for the management of motor fluctuations and dyskinesias”, though the study did not specifically mention how many were elective admissions [6]. In contrast, a report from the United Kingdom specifically stated that they did not admit patients for medication adjustment [5], suggesting a wide variation in elective admissions policies worldwide.
Elective surgery, fall/fracture, infection unrelated to pneumonia, mental status change, and aspiration pneumonia were considered by our Centers as common reasons for hospitalization. These data are consistent with several studies that have identified falls, pneumonia and other infections as common reasons for hospital admission [5–7]. Admissions for DBS and intestinal levodopa infusion (not available in the US) were less common, likely because they applied only to a subset of PD patients. There were no differences between US and international Centers regarding DBS hospitalization issues, though only 80% of NPF Centers perform DBS surgery.
Interestingly, psychiatric issues (anxiety/depression/psychosis) were cited as more common reasons for hospitalization in international than US Centers (38% vs. 6%). This may be because the US health care system does not reimburse well for psychiatric hospitalizations. Yet, therewas no difference in the number of US Centers and International Centers who felt they could admit patients electively for behavioral management. Another finding was that more US Centers thought their patients were hospitalized for elective surgery than did international Centers. This may reflect differences in private insurance and Medicare reimbursement in the US compared to other countries. Alternatively, international Centers may not be notified as often as their US counterparts when their patients undergo elective surgery.
Avoiding unnecessary admissions is important to the overall well-being of PD patients. In a study examining the events leading to hospital admissions for PD patients, Martignoni et al. [8] reported that more than half of PD patients did not require specific treatment for the acute comorbid event prompting admission; patients improved with adjustment of PD medications only. Similarly, a Center in Israel adopted an “open door” policy where patients could come without an appointment, and found that their average number of admissions per year dropped from 40 to 18 over a 3 year period [12]. In the Netherlands, the ParkinsonNet concept (a nationwide series of regional community networks of therapists specifically trained in PD) improved the quality of care in the community, obviating the need for more expensive admissions [13]. These collective results suggest that if readily available, expert outpatient care can be provided for frequent adjustment of PD medications, many hospital admissions could be avoided. When asked if there was an incentive to provide readily available outpatient care, significantly more international (75%) than US Centers (43%) reported an incentive. However, quick access to outpatient PD care is not being achieved in our Centers, as patients have waits of greater than 4 weeks for follow-up appointments at 16% of Centers.
In general, hospital lengths of stay are longer for PD patients when compared to non-PD patients [5,10]. This may be because when hospitalized, PD patients are often cared for by health care professionals who are not familiar with PD. The majority of Centers were not confident that medication schedules were adhered to during hospital stays perhaps because the importance of medication timing in PD was not well understood by hospital staff. Moreover, the complexity of dosing in moderate to advanced PD places considerable strain on the often limited hospital staff. A recent study demonstrated that 71% of PD patients admitted to a surgical ward had missed doses of PD medication during their hospital stay, with 34% of patients missing over 10% of prescribed doses [14]. Since Martignoni et al. [8] reported that some hospital comorbidities could be improved or prevented by adjustment of PD medications alone, medication adherence is critical in helping to decrease length of hospital stays. In addition, the fact that PD may be worsened by antipsychotics (either typical or atypical) or antinausea medications such as metoclopramide is under-recognized among non-specialists [15,16]. The majority of Centers were not confident that hospital clinicians knew that clozapine and quetiapine were the two atypical antipsychotics of choice to treat PD psychosis. As psychosis is the main reason for repeated admissions in PD [12], more understanding regarding the effects of antipsychotics on PD motor and non-motor symptoms may improve hospitalization-related outcomes in PD.
This survey is not without limitations. The responses represent the experiences and opinions of the individual completing the survey, and not necessarily all clinicians at each site. While most of the surveys were completed by physicians, some were completed by nurses, social workers or therapists. These different professions/individuals may have interpreted questions differently. Furthermore, these responses reflect the perception of care provided by others, which may be different from the reality of care provided by others. This survey is therefore best regarded as a first step toward addressing an understudied topic that has international ramifications for PD care. Additional surveys on this topic are encouraged.
PD patients are vulnerable when hospitalized, as they are typically under the care of non-specialist providers. As specialist input has been demonstrated to improve the care of stroke patients [17], research is needed on whether involving PD specialists could improve hospitalization of the PD patient. This survey has identified three specific targets for improvement. First, mechanisms need to be established to ensure notification of the treating neurologist that a PD patient in their practice has been admitted to the hospital. Relying on patients in crisis to alert their own physicians is neither optimal nor foolproof, but should continue to be encouraged. Communication between hospitals and PD neurologists regarding ER visits and hospital admissions needs streamlining, so that PD specialists can have input into the inpatient aspect of PD care. Second, interventional educational programs need to be studied and implemented for training hospital staff and non-neurologist clinicians regarding management of PD (including timing of dopaminergic therapies), complications of PD, and medications to avoid in PD patients. Finally, a plan to improve access to outpatient care is essential to prevent unnecessary hospitalizations of PD patients. All of the issues uncovered by this project can be addressed and improved through both future studies and outreach and education of hospital systems.
Supplementary Material
Appendix
The members of the NPF Working Group on Hospitalization in PD are: Michael J. Aminoff, MD, Ivan Bodis-Wollner, MD, Bastian R. Bloem, MD, PhD, Susan Calne, CM, RN, Kelvin L. Chou, MD, ChadW. Christine, MD, Joseph H. Friedman, MD, Nir Giladi, MD, Mark Guttman, MD, FRCPC, Robert Iansek, MD, Kelly E. Lyons, PhD, Irene A. Malaty, MD, Joyce Oberdorf, Wolfgang H. Oertel, MD, Michael S. Okun, MD, Rajesh Pahwa, MD, Sotirios A. Parashos, MD, PhD, Catherine C. Price, PhD, Nadia Romero, Peter Schmidt, PhD, Oksana Suchowersky, MD, Jorge Zamudio, MD.
US Centers
The 35 US Centers are as follows (asterisk* indicates Care Consortium Center):
Barrow Neurological Institute, Phoenix, AZ
University of Southern California, Los Angeles, CA
University of California, San Francisco, San Francisco, CA
The Parkinson’s Institute and Clinical Center, Sunnyvale, CA
Colorado Neurological Institute, Englewood, CO*
Georgetown University Hospital, Washington, DC
University of Florida, Gainesville, FL
University of Miami, Miami, FL
Tallahassee Memorial Hospital Parkinson’s Care Center, Tallahassee, FL*
University of South Florida, Tampa, FL
Medical College of Georgia, Augusta, GA
University of Hawaii, Honolulu, HI*
Northwestern University, Chicago, IL
University of Kansas Medical Center, Kansas City, KS
University of Louisville, Louisville, KY
Johns Hopkins Medical Institute, Baltimore, MD
Massachusetts General Hospital, Boston, MA
Beth Israel Deaconess Medical Center, Boston, MA
Struthers Parkinson’s Center, Golden Valley, MN
Parkinson’s Clinic of the Ozarks, Springfield, MO*
SUNY Downstate Medical Center, Brooklyn, NY
University at Buffalo, Buffalo, NY*
Beth Israel Medical Center, New York, NY
Mount Sinai School of Medicine, New York, NY
NYU Langone Medical Center, New York, NY
University of Rochester Medical Center, Rochester, NY
University of North Carolina at Chapel Hill, Chapel Hill, NC
Duke University Medical Center, Durham, NC
Oregon Health & Science University, Portland, OR
University of Pennsylvania, Philadelphia, PA
Vanderbilt University Medical Center, Nashville, TN
Baylor College of Medicine, Houston, TX
Texas A&M Health Science Center, Plummer Movement Disorders Center, Temple, TX*
Booth Gardner Parkinson’s Care Center, Kirkland, WA
Aurora Sinai Medical Center, Milwaukee, WI*.
International Centers
The 16 International Centers are as follows (asterisk* indicates Care Consortium Center):
Victorian Comprehensive Parkinson’s Program, Cheltenham, Victoria, Australia
University of Calgary/Alberta Health Services, Calgary Zone, Canada
University of Alberta/Alberta Health Services, Edmonton Zone, Canada
University of British Columbia, Vancouver, British Columbia, Canada
Deer Lodge Centre Movement Disorder Clinic, Winnipeg, Manitoba, Canada*
University of Western Ontario, London, Ontario, Canada
Markham Stouffville Hospital, Markham, Ontario, Canada
Toronto Western Hospital, Toronto, Ontario, Canada
McGill Movement Disorders Clinic, Montreal, Quebec, Canada
Derby Hospitals, Derby, England
King’s College Hospital, London, England
Philipps University, Marburg, Hessen, Germany
Tel Aviv Sourasky Medical Center, Tel Aviv, Israel;
Radboud University, Nijmegen Medical Centre, Nijmegen, Netherlands
National Neuroscience Institute, Singapore
National Taiwan University Hospital, Taipei, Taiwan.
Footnotes
The review of this paper was entirely handled by an Associate Editor, R.L. Rodnitzkyi.
None of the authors have any conflict of interest or financial disclosures to make.
Appendix. Supplementary material
The Supplementary data associated with this article can be found online, at doi:10.1016/j.parkreldis.2011.03.002.
References
- 1.Dorsey ER, Constantinescu R, Thompson JP, Biglan KM, Holloway RG, Kieburtz K, et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology. 2007;68:384–386. doi: 10.1212/01.wnl.0000247740.47667.03. [DOI] [PubMed] [Google Scholar]
- 2.Factor SA, Molho ES. Emergency department presentations of patients with Parkinson’s disease. Am J Emerg Med. 2000;18:209–215. doi: 10.1016/s0735-6757(00)90023-8. [DOI] [PubMed] [Google Scholar]
- 3.Hely MA, Morris JG, Reid WG, Trafficante R. Sydney Multicenter Study of Parkinson’s disease: non-L-dopa-responsive problems dominate at 15 years. Mov Disord. 2005;20:190–199. doi: 10.1002/mds.20324. [DOI] [PubMed] [Google Scholar]
- 4.Tan LC, Tan AK, Tjia HT. The profile of hospitalised patients with Parkinson’s disease. Ann Acad Med Singap. 1998;27:808–812. [PubMed] [Google Scholar]
- 5.Woodford H, Walker R. Emergency hospital admissions in idiopathic Parkinson’s disease. Mov Disord. 2005;20:1104–1108. doi: 10.1002/mds.20485. [DOI] [PubMed] [Google Scholar]
- 6.Temlett JA, Thompson PD. Reasons for admission to hospital for Parkinson’s disease. Intern Med J. 2006;36:524–526. doi: 10.1111/j.1445-5994.2006.01123.x. [DOI] [PubMed] [Google Scholar]
- 7.Guttman M, Slaughter PM, Theriault ME, DeBoer DP, Naylor CD. Parkinsonism in Ontario: comorbidity associated with hospitalization in a large cohort. Mov Disord. 2004;19:49–53. doi: 10.1002/mds.10648. [DOI] [PubMed] [Google Scholar]
- 8.Martignoni E, Godi L, Citterio A, Zangaglia R, Riboldazzi G, Calandrella D, et al. Comorbid disorders and hospitalisation in Parkinson’s disease: a prospective study. Neurol Sci. 2004;25:66–71. doi: 10.1007/s10072-004-0232-5. [DOI] [PubMed] [Google Scholar]
- 9.Nanhoe-Mahabier W, de Laat KF, Visser JE, Zijlmans J, de Leeuw FE, Bloem BR. Parkinson disease and comorbid cerebrovascular disease. Nat Rev Neurol. 2009;5:533–541. doi: 10.1038/nrneurol.2009.136. [DOI] [PubMed] [Google Scholar]
- 10.Guttman M, Slaughter PM, Theriault ME, DeBoer DP, Naylor CD. Burden of parkinsonism: a population-based study. Mov Disord. 2003;18:313–319. doi: 10.1002/mds.10333. [DOI] [PubMed] [Google Scholar]
- 11.Chou KL, Okun MS, Fernandez HH, Breslow D, Friedman JH. Five frequently asked questions about hospitalization for patients with Parkinson’s disease. Parkinson Rep. 2007;18:7–12. [Google Scholar]
- 12.Klein C, Prokhorov T, Miniovitz A, Dobronevsky E, Rabey JM. Admission of Parkinsonian patients to a neurological ward in a community hospital. J Neural Transm. 2009;116:1509–1512. doi: 10.1007/s00702-009-0302-1. [DOI] [PubMed] [Google Scholar]
- 13.Munneke M, Nijkrake MJ, Keus SH, Kwakkel G, Berendse HW, Roos RA, et al. Efficacy of community-based physiotherapy networks for patients with Parkinson’s disease: a cluster-randomised trial. Lancet Neurol. 2010;9:46–54. doi: 10.1016/S1474-4422(09)70327-8. [DOI] [PubMed] [Google Scholar]
- 14.Derry CP, Shah KJ, Caie L, Counsell CE. Medication management in people with Parkinson’s disease during surgical admissions. Postgrad Med J. 2010;86:334–337. doi: 10.1136/pgmj.2009.080432. [DOI] [PubMed] [Google Scholar]
- 15.Avorn J, Bohn RL, Mogun H, Gurwitz JH, Monane M, Everitt D, et al. Neuroleptic drug exposure and treatment of parkinsonism in the elderly: a case-control study. Am J Med. 1995;99:48–54. doi: 10.1016/s0002-9343(99)80104-1. [DOI] [PubMed] [Google Scholar]
- 16.Esper CD, Factor SA. Failure of recognition of drug-induced parkinsonism in the elderly. Mov Disord. 2008;23:401–404. doi: 10.1002/mds.21854. [DOI] [PubMed] [Google Scholar]
- 17.Albright KC, Raman R, Ernstrom K, Hallevi H, Martin-Schild S, Meyer BC, et al. Can comprehensive stroke centers erase the ‘weekend effect’? Cerebrovasc Dis. 2009;27:107–113. doi: 10.1159/000177916. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.