Abstract
One of the hallmarks of the communication revolution over the past decade has been its support for participation, whether that be in the active engagement of patients searching the Web for answers to vital health questions, or in the collective energies of self-organizing communities through social media. At the same time, some of the major obstacles to achieving a full and equitable reach of evidence-based cancer control knowledge have been traced back to discontinuities in communication either within clinical care or the broader public awareness system. Communication scientists from the National Cancer Institute, the Centers for Disease Control and Prevention, and the American Cancer Society joined forces in 2010 to investigate ways in which communication science can be used to improve coordination and enhance participation in cancer control for the nation. From 2010 to 2013, the three organizations worked together in 1) convening two meetings designed to assess the status of funded research in communication science, 2) completing a systematic review of literature published over the previous 10 years, and 3) authoring a blueprint for coordinated efforts using the implications of communication science. The blueprint consists of three major goals: first, to identify high-yield targets of opportunity using the health impact pyramid articulated by Centers for Disease Control and Prevention Director, Thomas Frieden; second, to leverage opportunities within the new communication environment, including the opportunities catalyzed by national efforts to create an infrastructure for evidence implementation through health information technology; and third, to assist in coordinating efforts across collaborative entities through participative media.
In its 2010 report titled Envisioning a Digital Future: Federally Funded Research and Development in Networking and Information Technology, the President’s Council of Advisors on Science and Technology argued that one of the fundamental benefits of a highly connected communication and information environment is its essential support for personal engagement and social participation (1). This includes an expanded sense of personal engagement from patients in their own health care as documented by the National Cancer Institute’s (NCI’s) Health Information National Trends Survey (2); an energized sense of grass roots activism by citizens, as social networking tools begin to connect communities in new and powerful ways (3); and even an expanded sense of participation in research, as patients seek out new ways to engage in the enterprise as “citizen scientists” (4). New participatory media jargon terms such as “crowdsourcing” and “peer production” were virtually nonexistent just a decade ago but have now entered our vocabulary as mainstays in a digitally connected world (1,5).
In this paper, representatives from the NCI, the Centers for Disease Control and Prevention (CDC), and the American Cancer Society (ACS) explore how advances in the new communication environment over the last decade can be brought to bear on the task of coordinating partnerships within cancer control. The conclusions presented are built off of a 3-year program of coordinated activity between communication scientists at the NCI, the CDC, and the ACS.
The Case for Coordination
Communication is the voice of cancer prevention and control. This voice alerts the public to new findings; helps them understand what they can do to lower their risks of developing cancer; helps them navigate the health-care system; and, above all, it is the voice that helps guide them toward the possibility of a cure. To ensure that the voice we call cancer communication is credible, effective, accurate, familiar, and that it is heard by the right people, at the right time, in the right place with the right message, the communication process should be based on good research.
Comprehensive cancer control is an endeavor deeply dependent on successful partnerships and the robust communication structures used to support them (6–8). Failures at the seams of these often implicit, interdependent relationships can have negative implications for individuals and for populations. Medical chart reviews have revealed that when health systems fail to engage patients in routine and recommended cancer screenings, or when communication errors precipitate a loss to follow-up, the consequences of these lapses in coordination can be late-stage disease and decreased survival rates (9). Discontinuities at the handoff between primary care and the many facets of specialty care have been blamed for delays in treatment (which may prove fatal), missed opportunities for early intervention, and failures in monitoring (10–12). Among cancer survivors, the transition from focused specialty care to the fragmented support of a discontinuous health-care system can lead to feelings of abandonment, to missed diagnoses of recurrence, to unattended sequelae of previous treatments, and to avoidable decrements in quality of life (13). Variations in communication efforts to support cancer prevention in local communities can lead to knowledge and belief gaps, with downstream consequences leading to disparities in population outcomes (14–16).
Recognizing that disconnected efforts in cancer control can hamper progress, the President’s Cancer Panel reiterated a call for greater coordination of efforts among the many entities comprising what the Institute of Medicine referred to as the “National Cancer Program,” that is, the collective efforts of government entities, nonprofit charities, health-care practitioners and the systems through which they practice, and for-profit therapeutic developers (17). Finding effective mechanisms to help coordinate implementation efforts across components of the national program while preserving stakeholder autonomy, it was thought, should help optimize investments at a time when economic resources are limited and centralization is infeasible. To that end, communication scientists from the NCI, the CDC, and the ACS engaged in a series of activities from 2010 to 2013 aimed at creating a blueprint for coordinating efforts across the cancer control continuum (18,19) within the context of the new, participative communication environment.
Partnering Against Cancer Today
One of the first tasks of the cross-organization working group was to canvass the scientific environment in communication research. The working group did this in two ways. First, it convened a “state of the science” symposium to bring in leading researchers to discuss progress and next steps within each of their respective fields in Atlanta, Georgia, on February 14–15, 2011. Panels convened in the context of the conference were chosen to represent progress within different levels of influence including 1) the role of communication in empowering communities, 2) extending the reach and effectiveness of public health campaigns, 3) empowering patients directly through clinical settings, and 4) engaging health information consumers through networking and information technology. Panel participants were asked to report first on what they perceived as the most significant progress made over the preceding years within their own areas of research and then report next on what they perceived as the most important questions driving the field in the next 10 years. A set of overarching conclusions from the symposium (20,21) is provided in Table 1.
Table 1.
Summary of conclusions from the February 14, 2011, State of the Science and Practice conference
| Number | Conclusion |
|---|---|
| 1 | Effective communication strategies are ready for dissemination through a national action plan. |
| 2 | Human relations and culture are important to establish trust with communities, even online. |
| 3 | Messages have to be high tech and high touch to engage and empower communities as active participants in health care. |
| 4 | Cancer communicators need to know how to adopt social media and mobile strategies while remaining cognizant of the digital divide and basic communication principles. |
| 5 | Infrastructure, privacy and regulation, and hardware compatibility issues need addressed to integrate health data. |
| 6 | Stories can be effective communication strategies but can cause misinformation. We need to identify the appropriate uses of testimonials and explore the costs vs benefits of this strategy. |
| 7 | Health literacy and numeracy are associated with health disparities and require our attention as health care becomes increasingly complex. |
| 8 | Patient–provider communication creates important indirect health outcomes when consistent with clinical evidence and patient values. Communication should be improved through changes in the medical school curriculum and innovative physician assessment methods. |
| 9 | To disseminate research into practice, we need to require business plans and systematic research designs such as rapid learning (eg, practitioners and researchers working together in real-world environments). |
| 10 | Novel, strategic community partners—from families and caregivers to lawmakers, media, and for-profits—have a unique role in dissemination. |
| 11 | Communication researchers and practitioners need more funding, especially for dissemination, social media, Web, and mobile applications. |
Following the conference, the three organizations commissioned a review of synthesis studies published during the decade from 2001 to 2011 (the 10 years preceding the state of the science symposium). Reviewers applied a predetermined set of search criteria with relevance to cancer communication across the PubMed, MEDLINE, Cochrane Reviews, and PsycINFO bibliographic databases. The initial search yielded a total of 2734 articles, from which a final list of 164 uniquely identified studies, meeting all of the predetermined set of criteria for high-quality meta-analytic and systematic reviews, was retained for final consideration. The resulting articles were categorized by stage within the cancer control continuum (18); that is, across efforts in prevention, detection, diagnosis, treatment, survivorship, and end-of-life and bereavement counseling. Reviews that could not be assigned to one position on the continuum were classified as “crosscutting” (20). From these combined inputs, the three funding organizations worked together to design a “blueprint” for using communication science to enhance partnership. What follows is a brief description of that blueprint.
A Blueprint for Using Communication Science to Enhance Partnerships
From a review of the literature, it was obvious that although communication processes underlie many of the activities conducted within the realm of cancer control and prevention, there was no “magic bullet” for improving all processes across all audiences. Rather, what did become apparent was that there were many proven techniques published in the literature that were consistent with communication and behavioral theory and that could be applied to the varying contexts of cancer control in replicable and predictive ways.
The first goal of the blueprint was to identify cancer-relevant communication targets across levels of influence (derived from the health impact pyramid described below) and across the cancer care continuum and then to suggest effective ways of reaching and influencing these targets. The second goal was to highlight ways in which structural changes in the health information environment could be leveraged to achieve accelerated success in actualizing cancer control goals. The third goal emphasized the application of implementation science principles to support the translation of evidence-based practices into the fabric of communications.
Goal 1: Focus on High-Yield Targets of Opportunity
To guide our efforts in identifying high-yield targets of opportunity, we relied on the multitiered health impact pyramid articulated by CDC Director, Thomas Frieden (22). The value of the pyramid, we believed, was to guide our thinking around communication support across the various levels of public health intervention available to constituencies in the cancer control context. Some interventions, such as those aimed at changing the social norms surrounding tobacco consumption through public service announcements and through restrictions on marketing from industry, can be expected to have a broad population impact over time. Other interventions, such as offering behavioral consulting to patients struggling with nicotine dependency, may be more resource intensive because of their individualized nature and may be sufficient to accomplish broad population change on their own. Using the example of tobacco control in California, Dr Frieden illustrated how public health efforts conducted at each of the levels of the health impact framework worked in concert to achieve a marked reduction in deaths from lung and bronchus cancer, as well as other tobacco-related diseases, over time (23).
Strategy 1-1: Identify Level of Impact.
In Figure 1, we have adapted Frieden’s multitiered framework to illustrate the role that communication efforts may play in achieving impact across multiple levels of influence. In doing so, we recognize that communication may only play a small, albeit frequently essential, role in creating sustainable change. For example, the foundational tier of the health impact pyramid in Figure 1 lists a host of social determinants—poverty, education, occupation, and living conditions—that can exert an almost intractable influence on the public’s health. Many of these influences are currently beyond the reach of cancer communication practitioners and will require the concerted efforts of policy makers, community leaders, and volunteer organizations to address (24).
Figure 1.
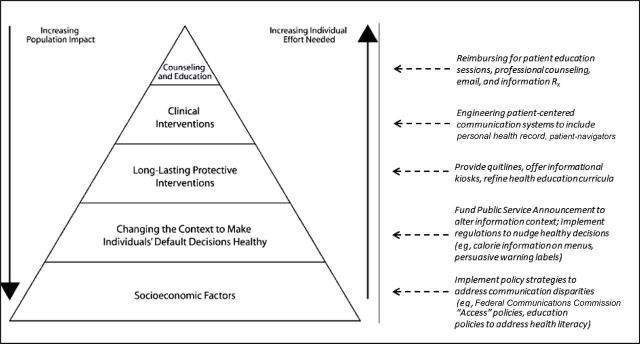
Frieden’s health impact framework applied to communication strategies [adapted from Frieden (22) with permission from American Public Health Association].
Nevertheless, there is much to be gained in considering evidence for the roles that communication may play within interventions aimed at each level of the health impact pyramid. Communication programs aimed at altering influences within the more foundational tiers of the framework have demonstrated some success in changing public norms around risky behaviors such as cigarette smoking (25) (tier 1), whereas efforts to change the informational context around decisions, say by placing graphic warning labels on tobacco products, have been shown to decrease youth initiation and promote cessation intentions (25–28) (tier 2). Creating more persuasive or tailored outreach programs to forestall the negative consequences of precancerous or early-stage neoplastic mutation, say through screening programs (29) or human papillomavirus vaccination (30), is a way of supporting long-lasting interventions (tier 3). Health systems programs designed to enable efficient information flow, support decision making, help patients cope with distress, facilitate patient self-management, and nurture healing relationships constitute successful communication strategies at the clinical level of patient-centered care (31,32) (tier 4). Finally, highly effective counseling programs designed to help improve patient outcomes through education and motivational interviewing constitute successful interventions in communication at the individualized apex of the pyramid (33) (tier 5).
Strategy 1-2: Identify Targets Along the Cancer Control Continuum.
Although the health impact pyramid offers an orientation to levels of influence, cancer control planners must also locate their efforts strategically across the cancer control continuum. The benefit here is that common communication mechanisms can be identified to assist cancer control efforts irrespective of specific cancer site. Much work has already been done to identify the needs for communication support in the areas of primary prevention (34,35), for screening and early detection (9), at diagnosis and across the environs of care (36,37), and for survivorship planning (13,38). Work has also been done on the sensitive communications that must take place at end of life, although those conversations do not always occur in reliable ways (39,40). Throughout all of this work, the general theme has been to identify the actors (or audiences) implicated at targeted points along the continuum, to identify the behaviors that need changing or bolstering, and then to create a replicable program for improving behavioral support around these targets through awareness campaigns, small media (brochures, educational materials), Web sites, specialty personnel (eg, patient navigators), patient portals, or more recently mobile interventions (41).
A general principle in cancer control is that the biggest impact in population health will come from intervening early in the etiology of the disease, by preventing some cancers from occurring altogether or preventing growth and metastasis through early preemption (42,43). Aggressive treatment, which is more expensive in terms of real human and financial costs, would be used for those cases that elude prevention and other preemption efforts. Communication models will need to adapt to changes in the medical paradigm by exploring ways of involving patients proactively in discussions of scientific evidence while supporting the complex cognitive demands of shared decision making (44). As medicine transforms, macro-level influences in health care will need to be addressed through communication research to address the very real problem of unanticipated labor shortages and to ensure accountability across multidisciplinary care teams (45).
Goal 2: Leverage Opportunities Within the New Communication Environment
In 2004, President George Bush set a national goal in his State of the Union address to improve the health care of Americans through the strategic use of health information technologies, and he announced an Office of the National Coordinator for Health Information Technology to oversee those investment efforts (46). In 2009, Congress passed the Health Information Technology for Economic and Clinical Health Act to speed adoption and to focus incentives on the “meaningful use” (47) of the technologies in accordance with a 2009 report by the National Research Council (48). By 2011, data from the CDC’s National Ambulatory Medical Care Survey suggested that overall adoption of electronic health record technologies among physicians hovered around the 50% mark, whereas coverage within health maintenance organizations climbed to 100% penetration (49). More generally, marketing data suggest that Internet access has diffused rapidly within the general population, cell phone technologies are proliferating, and consumer-facing health applications, or apps, are becoming commonplace. What is needed, though, is attention to how this new environment can be engineered to achieve improved outcomes for physicians, patients, and their caregivers (48).
Strategy 2-1: Use Health Information Technologies to Implement Evidence-Based Practices.
Evidence reviews have suggested that implementation of functional electronic health record systems can yield replicable improvements in care or communication efficiencies (50), can systematically remove barriers to cancer screening to cancer screening (51), can reduce errors (50), can reduce administrative costs (52), and can improve decision making (53). Current installations of electronic health record systems, however, have also been associated with decreases in provider satisfaction (50), disruptions in workflow (54), and uneven success in overall quality improvement (48). A simple proliferation of health information technologies will be insufficient to effect long-term change. Ongoing efforts will be needed to improve the usability of these systems (55), to improve system level integration (56), and to coordinate workflows for better organizational performance (54). The next phase of the health information revolution in cancer prevention and control must be guided by attention to issues of human systems integration, usability, quality improvement, workflow, and support for team process (45,48,54,55).
Strategy 2-2: Create Systems That Make “Real Differences in Peoples’ Lives.”
Outside of systems of care, people are beginning to rely on advances in communication and information technologies to support real and indispensable decision making in the multiple facets of their lives. People are becoming accustomed to accessing goods and services immediately as a result of ubiquitous access to the Internet. They can balance their checkbooks online, they can purchase and display airline tickets with their mobile devices, and they can navigate through unfamiliar neighborhoods effortlessly using Global Positioning System–enabled cell phones and automobiles. Yet, many of these same people find it difficult to negotiate the labyrinthine architectures of government Web sites or to acquire the right information they need at the right time to make important decisions about their health and welfare. In an executive memorandum dated May 23, 2012, President Barack Obama challenged public servants and private sector developers to create the applications that will make “real differences in peoples’ lives” (57).
Strategy 2-3: Advance the Research Agenda for a New Communication Ecosystem.
In spite of tremendous advances in health information technology, the ability for the public to exploit the new ecology reliably and equitably in its current form appears to be lacking. For example, although the percentage of Americans who went online to look for health or medical information grew from an estimated 50.6% of the adult population in 2003 to 77.6% in 2012, the indications have been that this newfound access was not resulting in a clearer sense of what do to prevent cancer. In fact, confusion over conflicting recommendations for cancer prevention appears to be increasing (2,58). Too much information presented through a cacophony of channels may be creating a type of “data smog” for consumers. Additionally, communication scientists have expressed concerns over the unequal diffusion of benefits from computer-based technologies (14), the effects of virally transmitted “misinformation” through social media networks (59), and the consequences of an unregulated market of personal health apps based on conjecture rather than scientific evidence (60).
In a series of reports, the President’s Council of Advisors on Science and Technology has cautioned that the country’s ability to capitalize on a “digital future” in health and other spheres would be dependent on an ongoing research agenda to optimize the fit between technological developments and human social interaction (1,5). Specifically, the Council urged for collaborative funding from the National Science Foundation and components of the Department of Health and Human Services (ie, the National Institutes of Health, the CDC, others) to create a new knowledge base to guide future design and development at the intersections of health and technology (1,5). Topics of specific interest include 1) creating a new area of scientific focus on “social computing” (1), 2) updating our understanding the health literacy (61) and the digital divide (62) in the new media landscape (63), 3) developing a sociological or organizational understanding of network effects in an era of massive patient and public connectivity (64), and 4) redefining the relationship between science, the public, and the media to achieve mutually supported population goals (1).
Goal 3: Align Systems
In focusing on how evidence-based programs can be coordinated to improve population impact, implementation scientists look for ways to align efforts across systems to maximize reach and effectiveness. In this section, we explore how the organizational structure of an “Evidence Implementation Triangle” can be used within the new communication ecosystem to improve collective intelligence and align efforts within communities of practice (65). There are three essential strategies, depicted as vertices within the evidence implementation triangle, which can be used to anchor implementation efforts as described below.
Strategy 3-1: Coordinate Efforts Around Data.
One of the hallmark characteristics of the new media environment, argued publisher Tim O’Reilly, is its interconnected use of data. Data will become the new “Intel Inside,” he argued, as interlocking information systems provide users with data-based intelligence for the myriad decisions they make on a daily basis (66). The use of shared data standards may have been essential in constructing real-time decision supports for national and local weather systems, and the identification of open Geographic Information System standards may have been essential for powering Global Positioning System technologies, but until now, these shared standards have been relatively absent in medicine and public health. The Department of Health and Human Services and the Institute of Medicine have sought to address this problem with their announcement in 2010 of the joint Community Health Data Initiative (67). Likewise, the National Institutes of Health is partnering with the National Science Foundation to create improved participatory platforms for turning “Big Data” into practicable knowledge. Ultimately, the goal is to help coordinate efforts and improve situational awareness with highly accessible community dashboards and other types of data visualizations (68,69).
Strategy 3-2: Promote the Use of Evidence-Based Communication Strategies.
In 2010, communication researchers Dearing and Kreuter noted that the best innovations in cancer communication do not necessarily achieve broad uptake by researchers, public health and clinical practitioners, and policy makers (70). What is needed, the researchers noted, is a “push–pull capacity” infrastructure that will allow communication innovators to extend the reach, effectiveness, adoption, implementation, and maintenance of evidence-based programs to the public. One such structure is the “Cancer Control P.L.A.N.E.T. (Plan, Link, Act, Network with Evidence-based Tools)” Web portal sponsored jointly by the NCI, the CDC, and other allied funding agencies (71). Its purpose is to make research-based intervention tools easily available to cancer control planners to local customization and implementation. Another structure is the CDC’s HealthCommWorks (www.cdc.gov/HealthCommWorks) Web site designed to provide health communicators with the tools needed to plan, execute, and evaluate both broadcast and social media health communication campaigns.
As communication technologies advance, and wireless sensors and mobile self-management tools extend health care into the home, there will be an even more substantive need to ensure that these new types of medical devices are reliable and effective (72). New types of partnerships will help ensure that the efficacy of these care extenders is ensured and protected. In some instances, creating new and innovative partnerships between the public and private sectors may help ensure that user effectiveness becomes a competitive advantage in an emerging marketplace. In other instances, national standards bodies may be created to ensure that the new innovations do no harm, which includes protecting data security and privacy. The certification procedures authorized under the Health Information Technology for Economic and Clinical Health Act (73) may also be used to boost demand for evidence-based interventions (56,74).
Strategy 3-3: Encourage Participation.
Another hallmark characteristic of the new communication environment is its shifting in emphasis away from one-to-many communications, to a distributed environment of many-to-many communications, for example, from broadcast media monologues to social media dialogues (66). Rather than relying solely on limited, top–down approaches to achieve strategic objectives, many of the more successful organizations in the new environment are striving to build better platforms to support broad participation and a sense of collective intelligence (75). Wikipedia, Yelp, and TripAdvisor are all examples of successful platforms designed to capture the distributed intelligence of participating members. In cancer, the Association of Cancer Online Resources preceded many other online meeting places where patients could share information and strategies with each other outside of the clinical encounter (76). Other collaborative activities, such as the Patients Like Me collaborative portal (patientslikeme.com) (77), the 23andMe consumer genomics site (23andme.com) (44), and research crowdsourcing (4), all bear watching as emerging models for a Medicine 2.0 paradigm shift (78).
Conclusions
Recent collaboration between communication scientists from the NCI, the CDC, and the ACS have resulted in this baseline blueprint as an important first step toward understanding the gaps and pointing the way toward opportunities for improving communication. With this in mind, our blueprint is an invitation to the cancer prevention community to work together in leveraging opportunities within the new communication environment across the cancer control continuum. The good news is that changes in the communication environment (8) may help facilitate better coordination, if designed correctly, at the personal, health system, local, national, and even global levels (7,79,80). Researchers and program administrators who can partner together to exploit this new capacity may begin to accelerate diffusion of current knowledge (43), while catalyzing discovery (64) through both energized public engagement and high-throughput data collection and analysis (81). In this new environment, participation and partnership may be an essential part of the “disruptive technology” (82) in cancer control that may make all of this possible.
Funding
BWH and GE are federal employees (National Institutes of Health and the Centers for Disease Control and Prevention). Efforts were conducted as part of their official duties.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Cancer Institute, the Centers for Disease Control and Prevention, or the American Cancer Society.
References
- 1. President’s Council of Advisors on Science and Technology Designing a digital future: federally funded research and development in networking and information technology http://www.whitehouse.gov/sites/default/files/microsites/ostp/pcast-nitrd-report-2010.pdf Published December 2010. Accessed October 15, 2013
- 2. Hesse BW, Moser RP, Rutten LJ. Surveys of physicians and electronic health information. N Engl J Med. 2010;362(9):859–860 [DOI] [PubMed] [Google Scholar]
- 3. Hesse BW, O’Connell M, Augustson EM, Chou WY, Shaikh AR, Rutten LJ. Realizing the promise of Web 2.0: engaging community intelligence. J Health Commun. 2011;16(suppl 1):10–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Swan M. Crowdsourced health research studies: an important emerging complement to clinical trials in the public health research ecosystem. J Med Internet Res. 2012;14(2):e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. President’s Council of Advisors on Science and Technology Designing a digital future: federally funded research and development in networking and information technology http://www.whitehouse.gov/sites/default/files/microsites/ostp/pcast-nitrd2013.pdf Published January 2013. Accessed October 15, 2013
- 6. Rochester PW, Townsend JS, Given L, Krebill H, Balderrama S, Vinson C. Comprehensive cancer control: progress and accomplishments. Cancer Causes Control. 2010;21(12):1967–1977 [DOI] [PubMed] [Google Scholar]
- 7. Vinson C, La Porta M, Todd W, Palafox NA, Wilson KM, Fairley T. Research and comprehensive cancer control coalitions. Cancer Causes Control. 2010;21(12):2033–2040 [DOI] [PubMed] [Google Scholar]
- 8. Viswanath K. Science and society: the communications revolution and cancer control. Nat Rev Cancer. 2005;5(10):828–835 [DOI] [PubMed] [Google Scholar]
- 9. Zapka JG, Puleo E, Taplin SH, et al. Processes of care in cervical and breast cancer screening and follow-up–the importance of communication. Prev Med. 2004;39(1):81–90 [DOI] [PubMed] [Google Scholar]
- 10. Taplin SH, Rodgers AB. Toward improving the quality of cancer care: addressing the interfaces of primary and oncology-related subspecialty care. J Natl Cancer Inst Monogr. 2010;2010(40):3–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zapka J, Taplin SH, Price RA, Cranos C, Yabroff R. Factors in quality care–the case of follow-up to abnormal cancer screening tests–problems in the steps and interfaces of care. J Natl Cancer Inst Monogr. 2010;2010(40):58–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mazor KM, Roblin DW, Greene SM, et al. Toward patient-centered cancer care: patient perceptions of problematic events, impact, and response. J Clin Oncol. 2012;30(15):1784–1790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hewitt ME, Ganz PA, eds. From Cancer Patient to Cancer Survivor: Lost in Transition: An American Society of Clinical Oncology and Institute of Medicine Symposium. Washington, DC: National Academies Press; 2006 [Google Scholar]
- 14. Viswanath K, Breen N, Meissner H, et al. Cancer knowledge and disparities in the information age. J Health Commun. 2006;11(suppl 1):1–17 [DOI] [PubMed] [Google Scholar]
- 15. Viswanath K, Kreuter MW. Health disparities, communication inequalities, and eHealth. Am J Prev Med. 2007;32(5 suppl):S131–S133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kreuter MW. Reach, effectiveness, and connections: the case for partnering with 2-1-1 to eliminate health disparities. Am J Prev Med. 2012; 43 (6 suppl 5):S420–S421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. President’s Cancer Panel Maximizing our nation’s investment in cancer: three crucial actions for America’s health. In: Leffall LD, Armstrong L, Kripke ML, eds. President’s Cancer Panel Annual Reports. Bethesda, MD: National Cancer Institute; 2008; 33–36 [Google Scholar]
- 18. National Cancer Institute The cancer control continuum. National Cancer Institute Web site http://cancercontrol.cancer.gov/od/continuum.html Modified July 5, 2013. Accessed October 15, 2013
- 19. Stange KC, Breslau ES, Dietrich AJ, Glasgow RE. State-of-the-art and future directions in multilevel interventions across the cancer control continuum. J Natl Cancer Inst Monogr. 2012;2012(44):20–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Oak Ridge Institute for Science and Education Cancer Communication: State of the Science and Practice Conference Summary. Atlanta, GA: Centers for Disease Control and Prevention; 2011 [Google Scholar]
- 21. Oak Ridge Institute for Science and Education Cancer Communication Systematic Review. Atlanta, GA: Centers for Disease Control and Prevention; 2012 [Google Scholar]
- 22. Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100(4):590–595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Centers for Disease Control and Prevention Achievements in public health, 1900–1999: tobacco use – United States, 1900–1999. MMWR Morb Mortal Wkly Rep. 1999;48(43):986–993 [PubMed] [Google Scholar]
- 24. Benjamin RM. The national prevention strategy: shifting the nation’s health-care system. Public Health Rep. 2011;126(6):774–776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. National Cancer Institute. Influence of tobacco marketing on smoking behavior In: David RM, Gilpin EA, Loken B, Viswanath K, Wakefield MA, eds. The Role of the Media in Promoting and Reducing Tobacco Use. Tobacco Control Monograph No. 19 Bethesda, MD: National Cancer Institute, US Department of Health and Human Services; 2008; 211–291 [Google Scholar]
- 26. Centers for Disease Control and Prevention Cigarette package health warnings and interest in quitting smoking—14 countries, 2008–2010. MMWR Morb Mortal Wkly Rep. 2010;60(20):645–651 [PubMed] [Google Scholar]
- 27. Pakhale S, Leone F, White AC. The argument in favor of graphic warning labels on cigarette packages. Ann Am Thorac Soc. 2013;10(1):50–52 [DOI] [PubMed] [Google Scholar]
- 28. Strasser AA, Tang KZ, Romer D, Jepson C, Cappella JN. Graphic warning labels in cigarette advertisements: recall and viewing patterns. Am J Prev Med. 2012;43(1):41–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kreuter MW, Garibay LB, Pfeiffer DJ, et al. Small media and client reminders for colorectal cancer screening: current use and gap areas in CDC’s Colorectal Cancer Control Program. Prev Chronic Dis. 2012;9:e131. doi:10.5888/pcd9.110317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kontos EZ, Emmons KM, Puleo E, Viswanath K. Contribution of communication inequalities to disparities in human papillomavirus vaccine awareness and knowledge. Am J Public Health. 2012;102(10):1911–1920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Epstein R, Street RJ. Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering. Bethesda, MD: National Cancer Institute; 2007 [Google Scholar]
- 32. Beckjord EB, Rechis R, Nutt S, Shulman L, Hesse BW. What do people affected by cancer think about electronic health information exchange? Results from the 2010 LIVESTRONG Electronic Health Information Exchange Survey and the 2008 Health Information National Trends Survey. J Oncol Pract. 2011;7(4):237–241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Miller SM, Bowen DJ, Croyle RT, Rowland JH, eds. Handbook of Cancer Control and Behavioral Science: A Resource for Researchers, Practitioners, and Policymakers. Washington, DC: American Psychological Association; 2009 [Google Scholar]
- 34. Committee on Communication for Behavior Change in the 21st Century: Improving the Health of Diverse Populations Speaking of Health: Assessing Health Communication Strategies for Diverse Populations. Washington, DC: National Academies Press; 2002 [Google Scholar]
- 35. Gorin SS, Wang C, Raich P, Bowen DJ, Hay J. Decision making in cancer primary prevention and chemoprevention. Ann Behav Med. 2006;32(3):179–187 [DOI] [PubMed] [Google Scholar]
- 36. Adler NE, Page A, eds; Committee on Psychosocial Services to Cancer Patients/Families in a Community Setting Cancer Care for the Whole Patient:Meeting Psychosocial Health Needs. Washington, DC: National Academies Press; 2008 [PubMed] [Google Scholar]
- 37. Aiello Bowles EJ, Tuzzio L, Wiese CJ, et al. Understanding high-quality cancer care: a summary of expert perspectives. Cancer. 2008;112(4):934–942 [DOI] [PubMed] [Google Scholar]
- 38. Hesse BW, Arora NK, Burke Beckjord E, Finney Rutten LJ. Information support for cancer survivors. Cancer. 2008;112(11)(suppl):2529–2540 [DOI] [PubMed] [Google Scholar]
- 39. Barnes S, Gardiner C, Gott M, et al. Enhancing patient-professional communication about end-of-life issues in life-limiting conditions: a critical review of the literature. J Pain Symptom Manage. 2012;44(6):866–879 [DOI] [PubMed] [Google Scholar]
- 40. Brereton L, Gardiner C, Gott M, Ingleton C, Barnes S, Carroll C. The hospital environment for end of life care of older adults and their families: an integrative review. J Adv Nurs. 2012;68(5):981–993 [DOI] [PubMed] [Google Scholar]
- 41. Kreps GL. Health Communication. Los Angeles, CA: Sage; 2010 [Google Scholar]
- 42. Hiatt RA, Rimer BK. A new strategy for cancer control research. Cancer Epidemiol Biomarkers Prev. 1999;8(11):957–964 [PubMed] [Google Scholar]
- 43. Cancer Center Directors Working Group Accelerating Successes Against Cancer. Washington, DC: Department of Health and Human Services; 2006 [Google Scholar]
- 44. Hesse BW, Arora NK, Khoury MJ. Implications of Internet availability of genomic information for public health practice. Public Health Genomics. 2012;15(3–4):201–208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Clauser SB, Wagner EH, Aiello Bowles EJ, Tuzzio L, Greene SM. Improving modern cancer care through information technology. Am J Prev Med. 2011;40(5)(suppl 2):S198–S207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hesse BW. Harnessing the power of an intelligent health environment in cancer control. Stud Health Technol Inform. 2005;118:159–176 [PubMed] [Google Scholar]
- 47. Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363(6):501–504 [DOI] [PubMed] [Google Scholar]
- 48. Stead WW, Lin HS. Computational Technology for Effective Health Care: Immediate Steps and Strategic Directions. Washington, DC: National Academies Press; 2009 [PubMed] [Google Scholar]
- 49. Jamoom E, Beatty P, Bercovitz A, Woodwell D, Palso K, Rechtsteiner E. Physician Adoption of Electronic Health Record Systems: United States, 2011. Hyattsville, MD: National Center for Health Statistics; 2012. NCHS Data Brief No. 98. [PubMed] [Google Scholar]
- 50. Buntin MB, Jain SH, Blumenthal D. Health information technology: laying the infrastructure for national health reform. Health Aff (Millwood). 2010;29(6):1214–1219 [DOI] [PubMed] [Google Scholar]
- 51. Friedberg MW, Coltin KL, Safran DG, Dresser M, Zaslavsky AM, Schneider EC. Associations between structural capabilities of primary care practices and performance on selected quality measures. Ann Intern Med. 2009;151(7):456–463 [DOI] [PubMed] [Google Scholar]
- 52. Chen C, Garrido T, Chock D, Okawa G, Liang L. The Kaiser Permanente Electronic Health Record: transforming and streamlining modalities of care. Health Aff (Millwood). 2009;28(2):323–333 [DOI] [PubMed] [Google Scholar]
- 53. Berner ES. Clinical Decision Support Systems: State of the Art. Rockville, MD: Agency for Healthcare Research and Quality; 2009 [Google Scholar]
- 54. Karsh B-T. Clinical Practice Improvement and Redesign: How Change in Workflow Can Be Supported by Clinical Decision Support. Rockville, MD: Agency for Healthcare Research and Quality; 2009 [Google Scholar]
- 55. Middleton B, Bloomrosen M, Dente MA, et al. Enhancing patient safety and quality of care by improving the usability of electronic health record systems: recommendations from AMIA. J Am Med Inform Assoc. 2013;20(e1):e2–e8. 10.1136/amiajnl-2012-001458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Committee on Patient Safety and Health Information Technolgy Health IT and Patient Safety: Building Safer Systems for Better Care. Washington, DC: The National Academies Press; 2012 [PubMed] [Google Scholar]
- 57. Building a 21st century digital government. Fed Regist. 2012;77(106): 32391–32392 [Google Scholar]
- 58. Niederdeppe J, Levy AG. Fatalistic beliefs about cancer prevention and three prevention behaviors. Cancer Epidemiol Biomarkers Prev. 2007;16(5):998–1003 [DOI] [PubMed] [Google Scholar]
- 59. Chou WY, Prestin A, Lyons C, Wen KY. Web 2.0 for health promotion: reviewing the current evidence. Am J Public Health. 2013;103(1):e9–e18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Abroms LC, Padmanabhan N, Thaweethai L, Phillips T. iPhone apps for smoking cessation: a content analysis. Am J Prev Med. 2011;40(3):279–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Nielsen-Bohlman L, Panzer AM, Kindig DA, eds; Commitee on Health Literacy Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004 [PubMed] [Google Scholar]
- 62. Kreps GL, Gustafson D, Salovey P, et al. The NCI Digital Divide Pilot Projects: implications for cancer education. J Cancer Educ. 2007; 22(1 suppl):S56–S60 [DOI] [PubMed] [Google Scholar]
- 63. Parker JC, Thorson E. Health Communication in the New Media Landscape. New York, NY: Springer; 2009 [Google Scholar]
- 64. Nielsen MA. Reinventing Discovery:The New Era of Networked Science. Princeton, NJ: Princeton University Press; 2012 [Google Scholar]
- 65. Glasgow RE, Green LW, Taylor MV, Stange KC. An evidence integration triangle for aligning science with policy and practice. Am J Prev Med. 2012;42(6):646–654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. O’Reilly T. What is Web 2.0: design patterns and business models for the next generation of software O’Reilly Media Web site. http://www.oreillynet.com/pub/a/oreilly/tim/news/2005/09/30/what-is-web-20.html Published September 30, 2005. Accessed October 15, 2013
- 67. Hesse BW, Hansen D, Finholt T, Munson S, Kellogg W, Thomas JC. Social participation in health 2.0. Computer (Long Beach Calif). 2010;43(11):45–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Shneiderman B, Plaisant C, Hesse BW. Improving healthcare with interactive visualization. Computer. 2013;46(5):58–66 [Google Scholar]
- 69. Hesse BW, Suls JM. Informatics-enabled behavioral medicine in oncology. Cancer J. 2011;17(4):222–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Dearing JW, Kreuter MW. Designing for diffusion: how can we increase uptake of cancer communication innovations? Patient Educ Couns. 2010;81(suppl 1):S100–S110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Sanchez MA, Vinson CA, Porta ML, Viswanath K, Kerner JF, Glasgow RE. Evolution of Cancer Control P.L.A.N.E.T.: moving research into practice. Cancer Causes Control. 2012;23(7):1205–1212 [DOI] [PubMed] [Google Scholar]
- 72. Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: are our theories up to the task? Transl Behav Med. 2011;1(1):53–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Health Information Technology for Economic and Clinical Health Act, 42 USC §139w-4(0)(2) (2009)
- 74. Albright HW, Moreno M, Feeley TW, et al. The implications of the 2010 Patient Protection and Affordable Care Act and the Health Care and Education Reconciliation Act on cancer care delivery. Cancer. 2011;117(8):1564–1574 [DOI] [PubMed] [Google Scholar]
- 75. Shirky C. Here Comes Everybody: The Power of Organizing Without Organizations. New York, NY: Penguin Press; 2008 [Google Scholar]
- 76. Meier A, Lyons EJ, Frydman G, Forlenza M, Rimer BK. How cancer survivors provide support on cancer-related Internet mailing lists. J Med Internet Res. 2007;9(2):e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Frost J, Okun S, Vaughan T, Heywood J, Wicks P. Patient-reported outcomes as a source of evidence in off-label prescribing: analysis of data from PatientsLikeMe. J Med Internet Res. 2011;13(1):e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Van De Belt TH, Engelen LJ, Berben SA, Schoonhoven L. Definition of Health 2.0 and Medicine 2.0: a systematic review. J Med Internet Res. 2010;12(2):e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Bernhardt JM, Mays D, Kreuter MW. Dissemination 2.0: closing the gap between knowledge and practice with new media and marketing. J Health Commun. 2012;16(suppl 1):32–44 [DOI] [PubMed] [Google Scholar]
- 80. Belle Isle L, Plescia M, La Porta M, Shepherd W. In conclusion: looking to the future of comprehensive cancer control. Cancer Causes Control. 2010;21(12):2049–2057 [DOI] [PubMed] [Google Scholar]
- 81. Chismar W, Horan TA, Hesse BW, Feldman SS, Shaikh AR. Health cyberinfrastructure for collaborative use-inspired research and practice. Am J Prev Med. 2011;40(5)(suppl 2):S108–S114 [DOI] [PubMed] [Google Scholar]
- 82. Topol EJ. The Creative Destruction of Medicine: How the Digital Revolution Will Create Better Health Care. New York, NY: Basic Books; 2012 [Google Scholar]