Abstract
Successful oral feeding of preterm and other ill and fragile infants is an interactive process that requires (1) sensitive, ongoing assessment of an infant’s physiology and behavior, (2) knowledgeable decisions that support immediate and long-term enjoyment of food, and (3) competent skill in feeding. Caregivers can support feeding success by using the infant’s biological and behavioral channels of communication to inform their feeding decisions and actions. The Supporting Oral Feeding in Fragile Infants (SOFFI) Method is described here with text, algorithms and reference guides. Two of the algorithms and the reference guides are published separately as Philbin, Ross. SOFFI Reference Guides: Text, Algorithms, and Appendices, (in review). The information in all of these materials is drawn from sound research findings and, rarely, when such findings are not available, from expert, commonly accepted clinical practice. If the quality of a feeding takes priority over the quantity ingested, feeding skill develops pleasurably and at the infant’s own pace. Once physiologic organization and behavioral skills are established, an affinity for feeding and the ingestion of sufficient quantity occur naturally, often rapidly, and at approximately the same post-menstrual age as volume-focused feedings. Nurses, therapists, and parents alike can use the SOFFI Method to increase the likelihood of feeding success in the population of infants at risk for feeding problems that emerge in infancy and extend into the pre-school years.
Keywords: NICU, preterm infant, bottle, feeding, behavior, algorithm, manual, guide, quality, nursing care
Infant feeding, by its nature, is an interactive, developmental task.1 Current research in preterm infant feeding shows that the infant’s ability to feed well is closely related to the caregiver’s ability to understand and sensitively respond to his physiology and behavioral communications.1, 2 While breastfeeding is by far the superior means of feeding, the great majority of infants in American Newborn Intensive Care Units (NICUs) are fed by bottle 3. This article describes a method that is primarily concerned with the quality of a feeding rather than its quantity. As it is used here, a quality feeding is defined as a complex event in which the infant is safe, physiologically stable, actively participating, behaviorally organized generally and in oro-motor activity, and comfortable. The infant’s nutritional status and caloric intake are understood as baseline conditions. The quality of a feeding relies on the assessments, decisions, and actions of a caregiver who is knowledgeable about feeding the infant at hand, sensitive to the infant’s behavioral and physiologic communications, and who has competent feeding skills. Further, this caregiver is oriented toward positively reinforcing an association between feeding and pleasurable human contact and toward supporting the infant’s individual manner and pace of acquiring feeding abilities. Such a caregiver may be either an accomplished feeder or an active learner with the supervision or coaching of an accomplished feeder. The SOFFI Method prioritizes the quality of the experience before the quantity ingested because many studies show that most infants who develop feeding problems are averse to food and feeding. Their consequent refusal to feed is a source of anxiety and self-doubt for their parents and long term developmental difficulties for themselves.4
Parents come to the NICU with a wide range of understanding and capability for feeding an immature or ill infant. Knowing this, nurses and therapists can build parents’ competence and confidence by modeling and coaching high quality feeding interactions. Many studies show that parents place a high value on their infant’s feeding and growth and judge their parenting competence by these metrics.5, 6 When the unique behavior of an infant is understood as a communicative attempt and parents know how to respond to it effectively, feeding generally becomes successful. In this context, the attachment relationship tends to strengthen and parents’ anxiety tends to diminish.6 A knowledgeable and skilled nurse or therapist observing and coaching a parent during a feedings can measurably benefit this process.7 Indeed, collaboration between a nurse or therapist and parent in understanding and responding to an infant’s behavior can benefit infant development and parent-infant interaction in many ways and over long periods of time.1, 6-12
The literature offers various approaches to acquiring bottle feeding skill. Clinical pathways, such as the one by Kirk et al., base the progression of feeding on the volume ingested with little said about feeding skill.13 Scales, such as the one developed by Ludwig and Waitzman, use holistic assessments to determine the infant’s readiness or skill but do not address the conduct of the feeding itself.14 Recently, Kirk, Alder, et al. published a decision pathway for feeding progression based in part on infant behavior but also on the infant’s age and the quantity ingested without addressing individual variation and skill development.13 At present, there are no published methods that address both feeding readiness and real-time feeding management with quality as the primary objective. SOFFI fills the gap.
Basis of the SOFFI Method in Theory and Research
Synactive theory 16 provides the primary theoretical basis for the SOFFI Method because it is a construct with ample explanatory power consistent with the known physiology and behavior of preterm and other fragile infants. Additionally, it is the most widely accepted model for understanding and using preterm infant behavior to guide care.16 As such, NICU staff are likely to be familiar with SOFFI concepts and terminology.
Synactive theory posits that infants are biologically striving, throughout development, toward the self-regulation of increasingly complex abilities. Caregivers can support this emerging competence by attentively and knowledgeably responding to each, individual infant’s autonomic neurophysiology, behavioral state, and motor (or movement) behavior so that the infant remains functionally organized and self-regulated. 10-12 The SOFFI Method assumes the synactive stance and applies it to the achievement of safe, functional bottle feeding in the context of pleasurable behavioral-social reciprocity. The theory places a high value on the parent as the ideal caregiver both physically and socially. 9,11,16 Clinicians are seen as sources of skillful support for the infant’s development and the expanding parent-child relationship.10,11,12 The nurse, who typically provides the majority of feedings, uses the SOFFI Method herself and coaches the parent in understanding and adopting it.
The details of the SOFFI Method are based on a review of the current and classic literature in the field. The databases OVID-CINAHL, PubMed, and the Cochran Database were used to identify literature concerning 1) synactive theory, 2) the use of synactive theory in providing care to support infant development, 3) feeding development in the preterm infant, and 4) models for preterm infant feeding. The search was generally limited to the period of 2002 to 2010, but without limits for synactive theory and models of feeding preterm, ill, or infants. Subsequently, the reference lists of entire articles were examined for potentially relevant material including editorials, commentaries, and case reports. All material was then reviewed for inclusion in the SOFFI Reference Guides.17
The literature review revealed a diverse body of research, commentary, and clinical practice. The major foci of these writings are the neuromotor and physiologic mechanisms of bottle feeding,18 the immediate bottle feeding experience,19, 20 and the long term cumulative learning acquired during repeated feeding experiences.2, 19 There are also models of bottle feeding readiness 2, 21 and bottle feeding outcomes 22, methods of enhancing bottle feeding efficiency 23, and descriptions of suck-swallow-breathe coordination.22
The SOFFI Method, Algorithms, and Reference Guides have been modified over time based on recommendations of nurse, therapist, and parent trainees, practicing clinicians, and by some of the experts whose studies are cited here.
The SOFFI Bottle Feeding Algorithm
The SOFFI Bottle Feeding algorithm displays a sequence of assessments, questions with “yes” or “no” answers, and decisions that lead to consequent actions. These actions affect the feeding and lead to the next set of assessments, decisions, and actions. In each case, the options for action are: (1) proceed along the algorithm to continue the feeding as is, (2) make a change to support stability or otherwise improve the feeding experience, (3) defer the feeding to a later time and gavage the remaining milk/formula, or (4) stop this bottle feeding and omit other closely following bottle feedings. The SOFFI Reference Guides with Appendices and the remaining two algorithms (The SOFFI Flow Rate Algorithm and the SOFFI Pacing Algorithm) provide the details for assessments, decisions, and actions referenced by letter in the SOFFI Bottle Feeding Algorithm.17
A Caveat Regarding the Use of the Algorithm
The SOFFI algorithm is meant to be learned away from the bedside. A caregiver or parent who is just acquiring skill in using them may want a quick visual check during a feeding but this must be accomplished without moving the hands or significantly changing the direction of gaze. The caregiver should maintain a virtually exclusive attention on the infant throughout the feeding. Such attention would preclude conversations with others, looking away from the infant, and stopping/re-starting a feeding to do tasks.
Decisions to Start a Feeding (See “Start” on the SOFFI Bottle Feeding Algorithm)
Physiologic Stability
The algorithm begins at “Start” with an assessment of the infant’s physiologic stability in bed during routine care or handling.24 Tenuous physiologic stability is likely to be revealed during common handling (e.g., a typical pre-feeding routine: unwrapping, diaper change, axillary temperature measurement, rewrapping). Physiologic stability for feeding is influenced by medical morbidity, demands on the synactive systems by medical or nursing tasks prior to the feeding, pre-feeding arousal level, oro-motor maturity, and previous feeding experience. Keep in mind that an infant crying from hunger or other distress for a period of time before a feeding has spent precious reserves and may be unable to sustain a physiologically stable, behaviorally organized, and pleasant feeding experience afterward.
Physiologic stability is the primary requirement for bottle feeding in the SOFFI Method for two reasons. First, feeding entails its own physiologic demands making it likely that an infant who is unstable before feeding would become even more unstable during a feeding and, therefore, less safe. Secondly, all other aspects of feeding are dependent on the infant’s physiologic stability. An infant might be able to ingest food while physiologically unstable but is unlikely to do so with self-regulation and comfort. Not surprisingly, physiologic stability during feeding is also shown to affect the long term development of feeding skill.22, 25
To be clear, physiologic stability is not defined here as recovery from critical illness. Rather, it is defined as stable vital signs, good color, and good muscle tone when the infant is alone in bed or during simple handling 24, 26. Stable vital signs are defined as a respiratory rate between 40 and 60 breaths per minute (or another range specified for that particular infant), a heart rate within 20% of recent resting levels (or a range specified for that particular infant), and blood oxygen saturation levels within the range specified by unit guidelines (or orders for that infant). The infant who is breathing outside of the acceptable respiratory rate is working very hard to maintain oxygenation. Good color is defined as pink in face and body with minimal to no paleness, mottled color, or localized duskiness/cyanosis, and good tone is defined as moderate flexion across shoulders, neck, trunk, and hips. These stability parameters are drawn from well-established information in the feeding physiology literature and are consistent with synactive theory.9, 27
Postponing or omitting a bottle feeding on the basis of physiologic instability, as defined here, spares the infant several likely, deleterious outcomes: (1) worsened physiologic instability during the feeding, (2) practice in using disorganized behaviors to manage the feeding, (3) an increased likelihood of solidifying disorganized behaviors in the repertoire, and (4) a feeding-associated aversive experience. Repeated experiences, whether organizing or disorganizing, create readily available behavior repertoires because they develop well defined neuronal connections. The Theory of Neuronal Grouping Selection suggests that neural maps in the cortex of the brain are established through repetitive experiences and behaviors in the present as well as the past 28.
If the infant is judged to be physiologically unstable (a “no” answer), the consequent action is to omit the bottle feeding (“stop”) and intervene to improve stability. The caregiver is referred to specific lettered Reference Guides for the means of accomplishing stabilization.17 The feeding is then completed with a slow gavage.
Readiness to Feed
If the infant is stable enough to engage in bottle-feeding generally, the next assessment on the algorithm is the infant’s readiness to feed at that moment. Clinical opinion and research indicate that an infant will feed most competently when showing signs of hunger and readiness to feed. These readiness signs include moving extremities and head, moving hands onto face or mouth, moving the face against bed linens or hands, mouthing or sucking movements, and behavior state arousal.25, 29-31 In young preterm infants just learning to feed, these readiness behaviors may occur at short, irregular intervals and be subtle and fleeting32. Therefore, the nurse or parent must be watchful for them lest the arousal opportunity passes by and the infant returns to sleep. Should these readiness indicators be absent, the caregiver is directed to defer the bottle feeding until they are present and to accomplish the feeding by slow gavage.
If signs of readiness are judged to be present (a “yes” decision), the assessment continues with the infant held in arms and offered an opportunity to suck nonnutritively. McCain and colleagues (2001) showed that infants acquired full oral feedings sooner when the basis for offering a feeding was the infant’s ability to maintain an alert behavioral state while sucking nonnutritively prior to all nutritive feedings.33
If the infant cannot maintain physiologic stability and a drowsy or alert state with non-nutritive sucking while held in arms (a “no” decision), the feeding is deferred because it is unlikely that comfort and physiologic stability will follow given requirements of the feeding itself. In this case, the action is to stabilize the infant and accomplish the feeding by slow gavage possibly with a positive oral experience such as tasting or smelling milk.
If the infant is judged able and ready to feed at this point (a “yes” decision) the consequent action is to offer the bottle.
Decisions during the Feeding
Supporting Physiologic Stability and Self-Regulation
The caregiver continues to assess physiologic stability throughout the feeding noting particularly a major desaturation, vital signs outside the infant’s parameters for more than a moment or repeatedly, or multiple coughs or choking. Particular care in observation and decision is required for infants with respiratory distress syndrome as they are more likely to have atypical feeding skills including apneic swallows (≥ 3 swallows without a breath).34 If these or equivalent signs of significant physiologic instability or compromise are present at any time (a “yes” answer) the caregiver is directed to stop the feeding, re-stabilize the infant, and give the remaining milk/formula by slow gavage. Physiologic events that do not indicate significant instability (a ‘no” answer) lead the caregiver to support self-regulation throughout the feeding as described in the SOFFI Reference Guides.17 Measures supporting self-regulation may include holding in an upright or side-lying position to improve suck, swallow, and breathe coordination or pausing for a rest break.
Engagement / Participation
If the infant is physiologically stable while feeding the algorithm next indicates assessing engagement or participation. Is the infant actively trying to nipple? If the answer is “no”, (e.g., low tone, sleeping, not sucking spontaneously, or trying to escape) the feeding terminates in the central “stop” oval. Active participation is necessary for learning coordinated, well-regulated feeding behavior. The studies of Thoyre et al. (2004) conclude that infant engagement and contingent caregiver responses are the best measure of feeding success.1 Similarly, McCain, et al. show a more rapid acquisition of feeding skills when the infant’s alertness and participation, rather than the volume ingested, determine the continuation of a feeding.29, 33 Of course infants can be made to suck by moving the nipple around in the mouth to stimulate the suck reflex. However stimulating involuntary sucking has deleterious consequences including protecting the airway with poorly coordinated and defensive feeding behavior, and, not surprisingly, an association between feeding and aversive experience.
Feeding Efficiency – Nipple Unit Flow Rate (See Flow Rate Algorithm and Appendix A in the SOFFI Reference Guides.17)
While the infant remains physiologically stable and engaged, the caregiver maintains an ongoing assessment of feeding efficiency; that is the amount taken from the bottle compared to the amount swallowed and the effort expended. The amount taken from the bottle with one suck, the bolus, is determined by the infant’s suck strength and coordination AND the rate of flow through the nipple with each suck. Feeding is not efficient if the nipple flow rate is too fast (delivers too large a bolus with one suck) or too slow (little or no flow despite coordinated feeding efforts). Feeding efficiency has been addressed in a number of studies. The SOFFI Flow Rate Algorithm, Appendix A 17 walks the caregiver through the process of determining the nipple with the most efficient flow rate for an individual infant and includes relevant references.
Drooling out some of the milk/formula may indicate that the nipple flow rate is too fast for that baby35. For example Chang et al., (2007) showed improved efficiency (greater ingested volume in a shorter period of time) when infants used a slower flow, single-hole nipple rather than a faster flow, cross-cut nipple.19 Similarly, Amaizu, et al., found that a nipple flow rate appropriate to the infant’s physiologic stability and oral-motor skill improved feeding safety, efficiency, and self-regulation.23 Gewolb, et al. showed that a slower flow nipple and rest breaks improved efficiency for infants with respiratory distress.34, 36 Slowing the rate of flow often improves suck-swallow-breathe coordination and reduces fluid loss.19, 23, 37-39 The first strategy for slowing the flow rate is using a slower flow nipple because pacing, another strategy, requires more diligence and education to implement correctly. A single slower-flowing nipple unit provides consistency across caregivers and a common element for oro-motor practice.
Infants with chronic lung disease or conditions causing oromotor weakness may suck with a well-developed pattern of short suck-swallow bursts and pauses and yet have inefficient feeding because they do not have the suction strength to pull the milk/formula out of the bottle. They may appear to be feeding efficiently, but take little in. For these infants a nipple that is faster flowing (e.g., the standard flow nipple) than the usually-preferred or baseline slow-flow nipple may improve efficiency while delivering a flow rate that the infant can control with his typically weak suction strength. However, the effects of the faster-flowing nipple must be observed carefully. If it delivers more volume per suck than the infant can swallow between breaths, the interruption of regular breathing may result in apnea and oxygen desaturation, aspiration, or choking. To reiterate, a faster flowing nipple is seldom indicated and care must be taken with its use. The SOFFI Reference Guide Appendix A 17 guides the assessment of safety, efficiency, and comfort related to nipple flow.
External Pacing (See Flow Rate Algorithm and Appendix B in the Reference Guides)17
If the infant is feeding efficiently, whether with the original nipple or an alternative as selected above, the answer to the question regarding the presence of spillage, gulping, etc. would be “no”. That is to say, none of those behaviors is observed. The algorithm arrow then directs the caregiver to bypass other algorithm components to arrive at the long vertical rectangle. This component directs the caregiver to continue, throughout the feeding, to assess, decide, and act with respect to physiologic stability, engagement, efficiency, and coordinated suck-swallow-breathe sequences.
If the caregiver has tried to solve the efficiency problem by changing the characteristics of the nipple but must still answer “yes” to the algorithm question about spillage, gulping, etc., the algorithm leads to the action “add support”. The caregiver then externally paces suck-swallow-breathe coordination using the SOFFI Pacing Algorithm and the SOFFI Reference Guides Appendix B.17
Pacing is a set of maneuvers that entrains sucking bursts to a pattern that allows sufficient opportunity and time to breathe. In pacing, the caregiver counts the number of sucks before a breath and interrupts flow after 3 to 5 sucks with no breath. The number of allowable suck-swallow combinations without a breath (between one and five) is determined for each infant based on the limits of respiratory effort necessary to maintain physiologic stability. For example, some infants who have more than three consecutive suck-swallows without a breath will maintain physiologic stability initially but gradually desaturate. They will benefit from external pacing to interrupt sucking after three suck-swallow combinations without a breath. The goal of the interruption is to maintain physiologic stability (e.g., oxygenation), rather than respond to distress after desaturation or an untoward event (e.g., choking) has occurred.
The integration of suck-swallow-breathe is usually well developed in newborn term infants and appears as a seamless whole (inhale, suck, swallow, exhale) with each segment running into the next and breathing barely apparent. However, medically compromised term infants (e.g., infants with a cardiac defect, or with neurologic impairment) often lack a mature or well integrated suck-swallow-breathe sequence. Preterm and other fragile infants may have a sucking reflex that excludes breathing because it is very strong and difficult or impossible to interrupt, particularly when hungry. A series of more than three to five suck-swallow combinations without a breath constitutes feeding apnea and has a variety of deleterious consequences. For example, air hunger may force the infant to breathe while continuing to suck and consequently inhale or aspirate milk/formula. Alternatively, the infant may suck more than can be swallowed and reflexively protect the airway by adducting the false vocal focal fold; that is to say, the infant may choke. Lack of breathing while feeding, or feeding apnea, can lower blood oxygen concentration beyond limits set for that child. It can also induce the “diving response” in which a lowering respiratory rate triggers the fetal response of slowing the heart rate (i.e., becoming bradycardic) thus causing hypoxia. For some infants this apnea and bradycardia can become self-sustaining and require intervention to re-instate breathing. The diving response is physiologically functional for the fetus, who does not need to breathe, but it is not functional for an extra-uterine fetus (i.e., a preterm infant). With pacing, however, physiologic stability can be maintained and sucking efficiency improved.37 External pacing can also provide the neurobehavioral “practice” that facilitates development of mature suck-swallow-breathe coordination. Law-Morstatt and colleagues (2003) found a decrease in bradycardic episodes and improved sucking efficiency when the infant was externally paced to maintain physiologic stability.37
Decisions to End a Feeding
At some point the infant either will have taken the prescribed amount of milk/formula or qualified for a decision to “stop”. Decisions to end or “stop” a feeding are indicated throughout the SOFFI Feeding Algorithm. Decisions to “stop” are based on physiologic instability, lack of engagement in feeding, inefficient effort, and/or difficulty integrating suck-swallow-breathe combinations despite caregiver efforts. These bases for stopping are well supported in the literature.1, 21, 29, 30, 33, 41 For example, McCain’s feeding protocol calls for stopping if the infant shows instability such as gasping or fatigue.29, 33 Thoyre, Shaker and Pridham (2005) recommend stopping if the infant has motoric changes such as flaccidity in the face (particularly the lower face) or limbs, or if the infant tries to escape the bottle by extending arms and legs or arching the trunk or neck.20 With the exception of obvious physiologic compromise (e.g. choking, bradycardia), ending a feeding based on the volume ingested appears to be a common criterion despite the literature cited here showing the validity of other “stop” criteria.38
Philbin, et al. conducted meticulous real time observations of 118 bottle feedings of 20 preterm infants in a prominent academic NICU.38 These feedings were not noticeably different than those observed by any of the investigators over many years in many different hospitals. During the feeding the nurse was asked to tell the observer the reason for each pause or stop in feeding as it occurred. If the nurse did not, the observer inquired in a neutral manner and otherwise refrained from interaction. The data show that quantity of intake rather than quality of feeding dominated decisions and actions. For example, the top four reasons for pausing/stopping a feeding concerned inefficient feeding even though 3 out of 4 unstable physiologic conditions were observed more frequently. Multiple swallows without breathing (i.e., feeding apneas) were observed 10 times more often than cited as a reason to pause/stop. Overall, physiologic and behavioral indicators of distress were observed 3 to 10 times more frequently than cited as reasons to pause/stop and increased after the first pause (e.g., to burp). A smaller study by Verno, et al. (n = 56) in a large suburban NICU compared the outcomes of infants fed as usual with outcomes of infants fed using a SOFFI-based method to guide decisions to stop a feeding.40 The infants fed by the SOFFI-based method started bottle feeding 5 days post-menstrual age (PMA) older than the infants fed as usual but were completely bottle-feeding at the same age, 37 weeks PMA. Further, they were less likely to be transferred to a specialty hospital for feeding problems (p = 0.03) and less likely to be referred to a feeding clinic by three months corrected age (p = 0.04).44
Documenting Infant Progression and Staff Feeding Activity Using the SOFFI Bottle Feeding Algorithm
An infant’s progression in feeding competence can be documented by circling the “stop” point on successive algorithm pages.
Such documentation can also assist in tracking staff consistency in using the SOFFI Method indicating a need for further guided practice in its use. More precise documentation of infant progression and staff consistency can be achieved with a modified version of the algorithm available from the authors.
Decisions to Increase Feeding Frequency and/or Volume
There is little evidence for strategies to “advance feedings” (i.e., offering additional feeds within a certain period of time). The authors’ clinical experience, research, and consultations in the United States and internationally is that most nurseries add feedings based on a measure of the volume previously ingested with a secondary regard for the quality of the feeding behavior.38 For example, Simpson et al. (2002) demonstrated more rapid progression when feedings were advanced by one feeding a day only when the current number of oral feedings were fully completed.40 Many NICUs use this strategy which appears to be based on the idea that stamina rather than skill is the key factor in feeding development. Other NICUs give several bottle-plus-gavage feedings within a 24-hour period, increasing the amount taken by bottle over time. McCain, et al., (2001) shortened time to full bottle feedings by 5 days using this protocol.33 This approach could provide more beneficial practice opportunities if the feedings were done with attention to quality. On the other hand, it could provide more non-functional practice (defensive, uncoordinated feeding behaviors) if the feeding is focused on quantity. Decisions about the number of bottle feedings are also influenced by the method of gavage supplementation. NICUs that use intermittently placed oro-gastric or naso-gastric tubes for feeding frequently require the infant to complete a full feed before attempting a second because of the stress of placing the tube after a partial feeding. In contrast, NICUs that use flexible, indwelling feeding tubes tend to attempt bottle feedings more frequently in a 24-hour period. The SOFFI Feeding Algorithms and Reference Guides remain applicable whatever the means of advancement because they involve continuous assessment, decision, and action based on the infant’s behavior.
The SOFFI Method in Practice
SOFFI concepts and decision parameters have been disseminated to NICU clinicians through many consultations and training conferences (e.g., the Rocky Mountain Fragile Infant Feeding Institute.)42, 43 The SOFFI Method is established clinical practice in a relatively small number of NICUs across the US and internationally with a thorough adoption of more than 10 years in the first author’s practice site.44 In randomized, controlled trials a similar approach to overall caregiving (including feeding) showed that sensitive responding to feeding behaviors resulted in earlier acquisition of competent feeding skills and full feedings by bottle.9, 11, 12, 44 Refinements to the SOFFI Feeding Algorithm have been suggested by practicing clinicians and by some of the experts whose studies are cited here.
In a systematic, on line evaluation completed two months after SOFFI training45, ninety percent of respondents judged the SOFFI Method as “easy to understand”, and 100% judged that it “helps to think aloud about the decisions made during a feeding.” Ninety-four percent thought the SOFFI Method was helpful in making decisions about supportive interventions, and 82% thought it was useful in explaining why a feeding was stopped to family members. During training, some participants thought the SOFFI Bottle Feeding Algorithm was “intimidating” when they first saw it. However, this appraisal was nearly always eliminated with explanation of the algorithm and use in practice. Identified benefits of the SOFFI Method for clinicians and parents include: 1) a common language for communication about feeding between staff and with parents, 2) a systematic, theory-based means of evaluating feeding development, 3) a means of providing anticipatory guidance to parents, and 4) a means of assessing staff performance.
Conclusion
The SOFFI Method for bottle feeding preterm and other fragile infants is based on established, tested theory with details drawn almost exclusively from the research literature. It integrates readily with staff education and clinical practice programs that are based on synactive theory because both use the same vocabulary and indicators of physiologic and behavioral organization. As a whole it provides a common language and concrete feeding plan (the algorithm) orienting feeding to the quality of the infant’s experience and long term feeding success. The shared SOFFI orientation supports staff-staff and staff-parent collaboration in successful feeding development. By building common goals for feeding, a common knowledge base and feeding path, and a common skill set for nurses, therapists, and parents, the SOFFI Method supports the infant’s physical growth, expands the infant’s behavioral repertoire, establishes feeding as a pleasurable activity, and strengthens mutually beneficial infant-parent interaction and attachment.
Figure 1. SOFFI Method Algorithm for Bottle-Feeding.
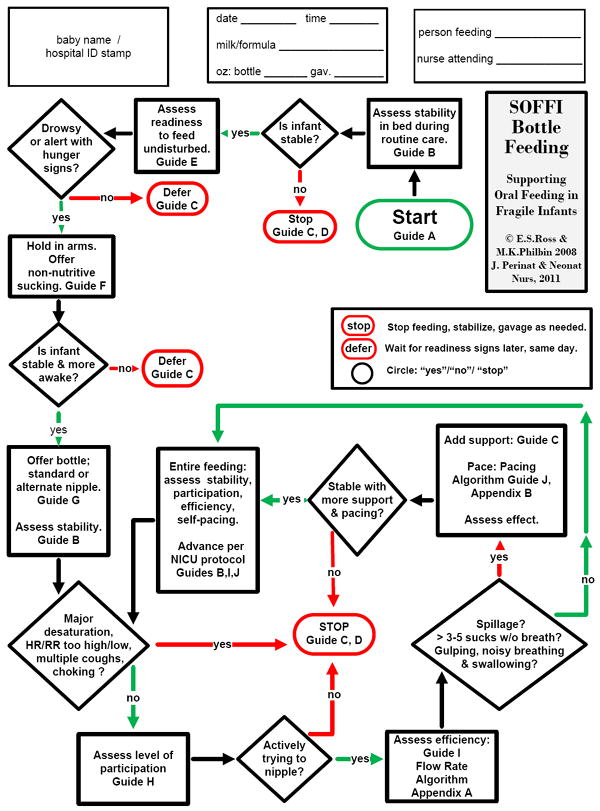
Beginning at START, the SOFFI Bottle Feeding Algorithm guides the caregiver through a sequence of assessments, decisions, and actions to realize a safe, high quality feeding that builds competent feeding behaviors and enjoyment of food and feeding. Letters in the algorithm indicate identically lettered sections in The SOFFI Reference Guides: Text, Algorithms, and Appendices: A Manualized Method for Quality Bottle Feedings. (Philbin & Ross, in review). The SOFFI Reference Guides provide details of assessment observations, decision explanations, and clinical action options. The algorithm is more easily followed in an enlarged format and printed in color. Contact the authors for a color copy. “No” decisions are shown in red and “yes” decisions in green. “STOP” indicates ending or pausing a feeding to stabilize the infant. The algorithm should be learned away from the bedside. Newly trained clinicians and parents may want to use the algorithm for a quick reference glance while feeding, but attention should be focused primarily on the infant and on the caregiver’s own behavior. The figure is used here with permission of the authors.
Acknowledgments
We gratefully acknowledge our colleagues and mentors in the global NIDCAP community and the many nurses, occupational therapists, speech-language pathologists, researchers, infants, and parents who have helped to develop our thinking over the years. Sharon Sables-Baus helped with early versions of the algorithms. Manuscript preparation was supported by: (ESR) NIH #5 T32 DK 07658-17, (MKP) The Children’s Hospital of Philadelphia and The College of New Jersey.
Biographies
Erin Ross, PhD, CCC-SLP has provided feeding and developmental consultation in Level II and III NICUs for 20 years. She evaluates and treats children in an outpatient feeding clinic and lectures nationally and internationally.
M. Kathleen Philbin, RN, PhD has specialized in adapting Level II and III NICU practices for optimal preterm infant development for 20 years. She teaches, does trainings in preterm infant handling and feeding, and consults widely regarding evidence-based care to support preterm infant development.
Contributor Information
Erin Sundseth Ross, Assistant Clinical Professor, University of Colorado Denver, School of Medicine, Department of Pediatrics, JFK Partners, Denver, Colorado; Honorary Research Fellow, Children’s Nutrition Research Centre, University of Queensland, Brisbane, Australia.
M. Kathleen Philbin, Associate Professor, The College of New Jersey Ewing, New Jersey; Adjunct Associate Professor, University of Pennsylvania School of Nursing, Philadelphia, Pennsylvania.
References
- 1.Thoyre SM, Brown RL. Factors contributing to preterm infant engagement during bottle-feeding. Nurs Res. 2004;53:304–13. doi: 10.1097/00006199-200409000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pickler RH. A Model of Feeding Readiness for Preterm Infants. Neonatal Intensive Care. 2004;17:31–36. [PMC free article] [PubMed] [Google Scholar]
- 3.Pineda RG. Predictors of breastfeeding and breastmilk feeding among very low birth weight infants. Breastfeed Med. 2011;6:15–9. doi: 10.1089/bfm.2010.0010. [DOI] [PubMed] [Google Scholar]
- 4.Wolke D, Samara M, Bracewell M, Marlow N. Specific language difficulties and school achievement in children born at 25 weeks of gestation or less. J Pediatr. 2008;152:256–62. doi: 10.1016/j.jpeds.2007.06.043. [DOI] [PubMed] [Google Scholar]
- 5.Deloian B. Caring connections: Nursing support transitioning premature infants and their families home from the hospital. Denver: University of Colorado Health Sciences Center, School of Nursing; 1998. [Google Scholar]
- 6.Pridham K, Lin CY, Brown R. Mothers’ evaluation of their caregiving for premature and full-term infants through the first year: contributing factors. Res Nurs Health. 2001;24:157–69. doi: 10.1002/nur.1019. [DOI] [PubMed] [Google Scholar]
- 7.Pridham K, Brown R, Clark R, Limbo RK, Schroeder M, Henriques J, et al. Effect of guided participation on feeding competencies of mothers and their premature infants. Res Nurs Health. 2005;28:252–67. doi: 10.1002/nur.20073. [DOI] [PubMed] [Google Scholar]
- 8.Achenbach TM, Howell CT, Aoki MF, Rauh VA. Nine-year outcome of the Vermont intervention program for low birth weight infants. Pediatrics. 1993;91:45–55. [PubMed] [Google Scholar]
- 9.Als H, Gilkerson L, Duffy FH, McAnulty GB, Buehler DM, Vandenberg K, et al. A three-center, randomized, controlled trial of individualized developmental care for very low birth weight preterm infants: medical, neurodevelopmental, parenting, and caregiving effects. J Dev Behav Pediatr. 2003;24:399–408. doi: 10.1097/00004703-200312000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Kaaresen PI, Ronning JA, Ulvund SE, Dahl LB. A randomized, controlled trial of the effectiveness of an early-intervention program in reducing parenting stress after preterm birth. Pediatrics. 2006;118:e9–19. doi: 10.1542/peds.2005-1491. [DOI] [PubMed] [Google Scholar]
- 11.Westrup B, Kleberg A, von Eichwald K, Stjernqvist K, Lagercrantz H. A randomized, controlled trial to evaluate the effects of the newborn individualized developmental care and assessment program in a Swedish setting. Pediatrics. 2000;105:66–72. doi: 10.1542/peds.105.1.66. [DOI] [PubMed] [Google Scholar]
- 12.Peters KL, Rosychuk RJ, Hendson L, Cote JJ, McPherson C, Tyebkhan JM. Improvement of short- and long-term outcomes for very low birth weight infants: Edmonton NIDCAP trial. Pediatrics. 2009;124:1009–20. doi: 10.1542/peds.2008-3808. [DOI] [PubMed] [Google Scholar]
- 13.Kirk AT, Alder SC, King JD. Cue-based oral feeding clinical pathway results in earlier attainment of full oral feeding in premature infants. J Perinatol. 2007 doi: 10.1038/sj.jp.7211791. [DOI] [PubMed] [Google Scholar]
- 14.Ludwig S, Waitzman KA. Changing Feeding Documentation to Reflect Infant-Driven Feeding Practice. Newborn and Infant Nursing Reviews. 2007;7:155–60. [Google Scholar]
- 15.Perry BD, Pollard RA, Blakeley WL, Vigilante D. Childhood Trauma, the Neurobiology of Adaptation, and “Use-dependent” Development of the Brain: How “States” Become “Traits”. Infant Mental Health Journal. 1995;16:271–91. [Google Scholar]
- 16.Als H. Toward a synactive theory of development: Promise for the assessment and support of infant individuality. Infant Mental Health Journal. 1982;3:229–43. [Google Scholar]
- 17.Philbin MK, Ross E. Support of oral feeding for fragile infants (SOFFI) reference guide, algorithms, and appendices: A manualized process for quality bottle feedings in review. 2011 doi: 10.1097/JPN.0b013e31823529da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pickler RH, Reyna BA. Effects of non-nutritive sucking on nutritive sucking success in newborn intensive care. The New Jersey Neonatal Society. 2010 [Google Scholar]
- 19.Chang YJ, Lin CP, Lin YJ, Lin CH. Effects of single-hole and cross-cut nipple units on feeding efficiency and physiological parameters in premature infants. J Nurs Res. 2007;15:215–23. doi: 10.1097/01.jnr.0000387617.72435.c6. [DOI] [PubMed] [Google Scholar]
- 20.Thoyre SM, Shaker CS, Pridham KF. The early feeding skills assessment for preterm infants. Neonatal Netw. 2005;24:7–16. doi: 10.1891/0730-0832.24.3.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McGrath JM, Braescu AV. State of the science: feeding readiness in the preterm infant. J Perinat Neonatal Nurs. 2004;18:353–68. doi: 10.1097/00005237-200410000-00006. quiz 69-70. [DOI] [PubMed] [Google Scholar]
- 22.Pickler RH, Best AM, Reyna BA, Gutcher G, Wetzel PA. Predictors of nutritive sucking in preterm infants. J Perinatol. 2006;26:693–9. doi: 10.1038/sj.jp.7211590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Amaizu N, Shulman R, Schanler R, Lau C. Maturation of oral feeding skills in preterm infants. Acta Paediatr. 2008;97:61–7. doi: 10.1111/j.1651-2227.2007.00548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Browne J, Ross E. Rocky Mountain Fragile Infant Feeding Institute (RMFIFI) Training curriculum. Denver, CO: University of Colorado Health Sciences Center; 2001. BROSS: Baby regulated organization of systems and sucking. [Google Scholar]
- 25.Pickler RH, Best AM, Reyna BA, Wetzel PA, Gutcher GR. Prediction of feeding performance in preterm infants. Newborn and Infant Nursing Reviews. 2005;5:116–23. doi: 10.1053/j.nainr.2005.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ross ES, Browne JV. Developmental progression of feeding skills: an approach to supporting feeding in preterm infants. Seminars in Neonatology. 2002;7:469–75. doi: 10.1053/siny.2002.0152. [DOI] [PubMed] [Google Scholar]
- 27.Browne JV, MacLeod AM, Smith-Sharp S. The Family Infant Relationship Support Training Program (FIRST©), Training Guide. Denver, CO: The Denver Children’s Hospital Association, The Center for Family and Infant Interaction; 2001. [Google Scholar]
- 28.Edelman GM. The Theory of Neuronal Group Selection. New York: Basic Books, Inc; 1987. Neural Darwinism. [DOI] [PubMed] [Google Scholar]
- 29.McCain GC. An evidence-based guideline for introducing oral feeding to healthy preterm infants. Neonatal Network - Journal of Neonatal Nursing. 2003;22:45–50. doi: 10.1891/0730-0832.22.5.45. [DOI] [PubMed] [Google Scholar]
- 30.McGrath JM, Medoff-Cooper B. Alertness and feeding competence in extremely early born preterm infants. Newborn and Infant Nursing Reviews. 2002;2:174–86. [Google Scholar]
- 31.Pickler RH, Reyna BA. Effects of non-nutritive sucking on nutritive sucking, breathing, and behavior during bottle feedings of preterm infants. Adv Neonatal Care. 2004;4:226–34. doi: 10.1016/j.adnc.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 32.Peters KL. Association between autonomic and motoric systems in the preterm infant. Clin Nurs Res. 2001;10:82–90. doi: 10.1177/c10n1r8. [DOI] [PubMed] [Google Scholar]
- 33.McCain GC, Gartside PS, Greenberg JM, Lott JW. A feeding protocol for healthy preterm infants that shortens time to oral feeding. J Pediatr. 2001;139:374–9. doi: 10.1067/mpd.2001.117077. [DOI] [PubMed] [Google Scholar]
- 34.Gewolb IH, Vice FL. Abnormalities in the coordination of respiration and swallow in preterm infants with bronchopulmonary dysplasia. Dev Med Child Neurol. 2006;48:595–9. doi: 10.1017/S0012162206001241. [DOI] [PubMed] [Google Scholar]
- 35.Eishima K. The analysis of sucking behaviour in newborn infants. Early Hum Dev. 1991;27:163–73. doi: 10.1016/0378-3782(91)90192-6. [DOI] [PubMed] [Google Scholar]
- 36.Gewolb IH, Bosma JF, Reynolds EW, Vice FL. Integration of suck and swallow rhythms during feeding in preterm infants with and without bronchopulmonary dysplasia. Dev Med Child Neurol. 2003;45:344–8. doi: 10.1017/s001216220300063x. [DOI] [PubMed] [Google Scholar]
- 37.Law-Morstatt L, Judd DM, Snyder P, Baier RJ, Dhanireddy R. Pacing as a treatment technique for transitional sucking patterns. J Perinatol. 2003;23:483–8. doi: 10.1038/sj.jp.7210976. [DOI] [PubMed] [Google Scholar]
- 38.Philbin MK, Medoff-Cooper B, Thomas T, Mooney C, Abbasi S. Quantity or quality: what controls the decision to pause/stop a NICU bottle feeding? Pediatric Academic Societies. 2010;3739:417. [Google Scholar]
- 39.Shaker CS, Woida AM. An evidence-based approach to nipple feeding in a level III NICU: nurse autonomy, developmental care, and teamwork. Neonatal Netw. 2007;26:77–83. doi: 10.1891/0730-0832.26.2.77. [DOI] [PubMed] [Google Scholar]
- 40.Simpson C, Schanler RJ, Lau C. Early introduction of oral feeding in preterm infants. Pediatrics. 2002;110:517–22. doi: 10.1542/peds.110.3.517. [DOI] [PubMed] [Google Scholar]
- 41.Thoyre SM, Carlson JR. Preterm infants’ behavioural indicators of oxygen decline during bottle feeding. J Adv Nurs. 2003;43:631–41. doi: 10.1046/j.1365-2648.2003.02762.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ross E. Supportive Interventions for Nipple Feeding. Rocky Mountain Fragile Infant Feeding Institute; Westminster, Colorado: 2010. [Google Scholar]
- 43.Ross ES. Feeding the Most Fragile: From NICU to Early Intervention. Aurora, IL: 2011. [Google Scholar]
- 44.Verno A, Dickerson N, Corn N, Philbin MK. Effects of infant-driven feeding on feeding success in newborn intensive care. The New Jersey Neonatal Society. 2010 [Google Scholar]
- 45.Ross E. Evaluation of the SOFFI Algorithm. 2009 [Google Scholar]


