Abstract
Aims
Atrial fibrillation increases the risks of stroke, heart failure, and death, and anticoagulation therapy increases the risk of gastrointestinal haemorrhage. However, the relative event rates for these outcomes are not well described. We sought to define the risks of major clinical events in older adults after a new diagnosis of atrial fibrillation.
Methods and results
We undertook a population-based, retrospective cohort study of a nationally representative sample of fee-for-service Medicare beneficiaries 65 years or older with incident atrial fibrillation diagnosed between 1999 and 2007. The main outcome measures were mortality and hospitalization or emergency department care for heart failure, myocardial infarction, stroke, or gastrointestinal haemorrhage. Among 186 461 patients with atrial fibrillation and no recent hospitalizations for heart failure, myocardial infarction, stroke, or gastrointestinal haemorrhage, mortality was the most frequent of these major clinical events (19.5% at 1 year; 48.8% at 5 years). By 5 years, 13.7% of patients were hospitalized for heart failure, 7.1% developed new-onset stroke, and 5.7% had gastrointestinal haemorrhage. Myocardial infarction was less frequent (3.9% at 5 years). Rates of mortality, heart failure, myocardial infarction, stroke, and gastrointestinal bleeding increased with older age and higher CHADS2 scores. Among 44 479 patients with previous events, the 5-year risk of death was greatest among patients with recent bleeding events (70.1%) and stroke (63.7%) and lowest among those with recent myocardial infarction (54.9%).
Conclusion
After the diagnosis of incident atrial fibrillation in older adults, mortality was the most frequent major outcome during the first 5 years. Among non-fatal cardiovascular events, heart failure was the most common event.
Keywords: Atrial fibrillation, Heart failure, Outcome assessment (health care), Mortality
Introduction
Atrial fibrillation is a common problem among older adults,1 and it is associated with increased risks of heart failure, stroke, and death.2 The Institute of Medicine recently ranked the treatment of patients with atrial fibrillation among the highest priority topics for comparative effectiveness research.3 Effective treatment of patients with atrial fibrillation includes not only rate control, rhythm control, and prevention of stroke, but also management of cardiovascular risk factors and comorbid illnesses. Although atrial fibrillation is associated with increased risks of major cardiovascular events such as stroke and heart failure, the absolute and relative event rates of these competing outcomes are not well described. Optimal public health prioritization, clinical decision-making, and patient counselling require an understanding of the clinical course of disease states, including the potential risks of multiple subsequent clinical events. Therefore, we used survival analysis in a national sample of older adults to describe the incidence of death, heart failure, myocardial infarction, stroke, and gastrointestinal bleeding after the diagnosis of atrial fibrillation.
Methods
Study population
Using a 5% national sample of fee-for-service Medicare beneficiaries 65 years or older, we identified beneficiaries who received a diagnosis of incident atrial fibrillation between 1 January 1999 and 30 September 2007. We described our identification of the study population in detail previously.1 In brief, we considered beneficiaries to have incident atrial fibrillation if they had a single inpatient claim or two outpatient or physician claims with an atrial fibrillation diagnosis [International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code 427.31] in any position on the claim after two or more years of enrolment in fee-for-service Medicare with no atrial fibrillation diagnosis. Because of the requirement of prior enrolment without atrial fibrillation, beneficiaries in the study population were 67 years or older. For the purpose of our analyses, we excluded patients with atrial fibrillation initially diagnosed during a terminal hospitalization.
Data sources
For patients in the study population, we obtained inpatient, outpatient, and carrier claims and the corresponding denominator files from 1 January 1998 to 31 December 2009, from the US Centers for Medicare & Medicaid Services. The inpatient files contain institutional claims for inpatient services. The outpatient files contain institutional claims for outpatient services. The carrier files contain physician and other non-institutional claims for services. All files include service dates and ICD-9-CM diagnosis codes. The denominator files contain beneficiary demographic characteristics, date of death (if applicable), and Medicare enrolment information. All analyses were limited to periods of Medicare fee-for-service enrolment.
Events
The outcomes of interest were death and hospitalization or emergency department care for heart failure, myocardial infarction, stroke, or gastrointestinal haemorrhage in the 5 years after a diagnosis of incident atrial fibrillation. We used the Medicare denominator files to identify deaths. We identified all other outcomes by searching for inpatient or emergency department claims containing a primary diagnosis of stroke (ICD-9-CM codes 430, 431, 433.x1, 434.x1, 435.x, 436), heart failure (428.x, 402.x1, 404.x1, 404.x3), myocardial infarction (410.x1), or gastrointestinal haemorrhage (456.0, 530.7, 530.82, 531.0x, 531.2x, 531.4x, 531.6x, 532.0x, 532.2x, 532.4x, 532.6x, 533.0x, 533.2x, 533.4x, 533.6x, 534.0x, 534.2x, 534.4x, 534.6x, 535.x1, 537.83, 537.84, 562.02, 562.03, 562.12, 562.13, 569.3, 569.85, 578.x). If a hospitalization or emergency department visit resulted in death, we classified the event as a death regardless of the associated primary diagnosis. In a sensitivity analysis, we counted these hospitalizations and emergency department visits towards the other outcomes, when applicable.
Study cohorts
Within the study population, we defined a primary study cohort and several secondary cohorts on the basis of events in the 3 months before the atrial fibrillation diagnosis. We treated these groups separately, because we expected recent events to have a strong effect on subsequent outcome trajectories. The recent events of interest were the same as those described above except death (i.e. heart failure, myocardial infarction, stroke, and gastrointestinal haemorrhage). The primary study cohort included patients who had no recent events. The secondary study cohorts included patients who had one or more recent events—heart failure alone, myocardial infarction alone, stroke alone, gastrointestinal haemorrhage alone, or multiple events.
Statistical analysis
For the primary study cohort, we described demographic characteristics (age, sex, and race), comorbid conditions (cancer, cerebrovascular disease, chronic obstructive pulmonary disease, coronary heart disease, dementia, diabetes mellitus, heart failure, hypertension, peripheral vascular disease, renal disease, and valvular heart disease), devices in place at the time of diagnosis (implantable cardioverter-defibrillator and pacemaker), and the setting of the atrial fibrillation diagnosis (inpatient or outpatient). We identified comorbid conditions using diagnoses from both inpatient and outpatient claims and previously validated coding algorithms.4,5 To summarize risk, we used both the CHADS2 and CHA2DS2-VASc risk scores.6,7 For categorical variables, we report frequencies and percentages. For continuous variables, we report means and SDs.
For all study cohorts, we used Kaplan–Meier methods to estimate mortality rates. We treated death as a competing risk for all other events and used the cumulative incidence function to estimate rates for each event. We censored data at the time of disenrollment from fee-for-service Medicare or at the end of data availability (31 December 2009), if applicable. We also plotted cumulative incidence curves for each cohort. In the primary cohort, we summarized the observed cumulative incidence rates for a number of subgroups, defined according to age, sex, setting of diagnosis, and CHADS2 score.
We used SAS version 9.2 (SAS Institute, Inc.) for all analyses.
Results
The study population included 230 940 Medicare beneficiaries with incident atrial fibrillation. The primary study cohort included 186 461 patients (81%) who did not have any of the clinical events of interest during the preceding 3 months. The 44 479 patients (19%) who did have a recent event were included in the secondary study cohorts. The median follow-up was 4.4 years (inter-quartile range, 4.1–5.0). Table 1 shows the baseline characteristics of the primary cohort. Most patients (60.1%) were first diagnosed with atrial fibrillation in inpatient settings. The mean age was 79.5 (SD: 7.3) years, 44.6% of the patients were men, and 92.0% were white. The mean CHADS2 score was 2.8 (SD: 1.4) and the mean CHA2DS2-VASc score was 5.0 (SD: 1.7).
Table 1.
Characteristics of the primary study cohort of Medicare beneficiaries with incident atrial fibrillation
| Characteristic | Patients (n = 186 461) |
|---|---|
| Age, mean (SD), year | 79.5 (7.3) |
| Male, n (%) | 83 079 (44.6) |
| Race, n (%) | |
| Black | 9852 (5.3) |
| White | 171 579 (92.0) |
| Other/unknown | 5030 (2.7) |
| Comorbid conditions, n (%) | |
| Cancer | 38 509 (20.7) |
| Cerebrovascular disease | 53 047 (28.4) |
| Chronic obstructive pulmonary disease | 71 093 (38.1) |
| Coronary heart disease | 101 299 (54.3) |
| Dementia | 17 320 (9.3) |
| Diabetes mellitus | 54 659 (29.3) |
| Heart failure | 72 746 (39.0) |
| Hypertension | 149 673 (80.3) |
| Peripheral vascular disease | 51 021 (27.4) |
| Renal disease | 20 684 (11.1) |
| Valvular heart disease | 69 905 (37.5) |
| Risk scores, n (%) | |
| CHADS2, mean (SD) | 2.8 (1.4) |
| CHA2DS2-VASc, mean (SD) | 5.0 (1.7) |
| Devices, n (%) | |
| Implantable cardioverter-defibrillator | 1636 (0.9) |
| Pacemaker | 9666 (5.2) |
| Clinical setting of diagnosis, n (%) | |
| Inpatient | 112 097 (60.1) |
| Outpatient | 74 364 (39.9) |
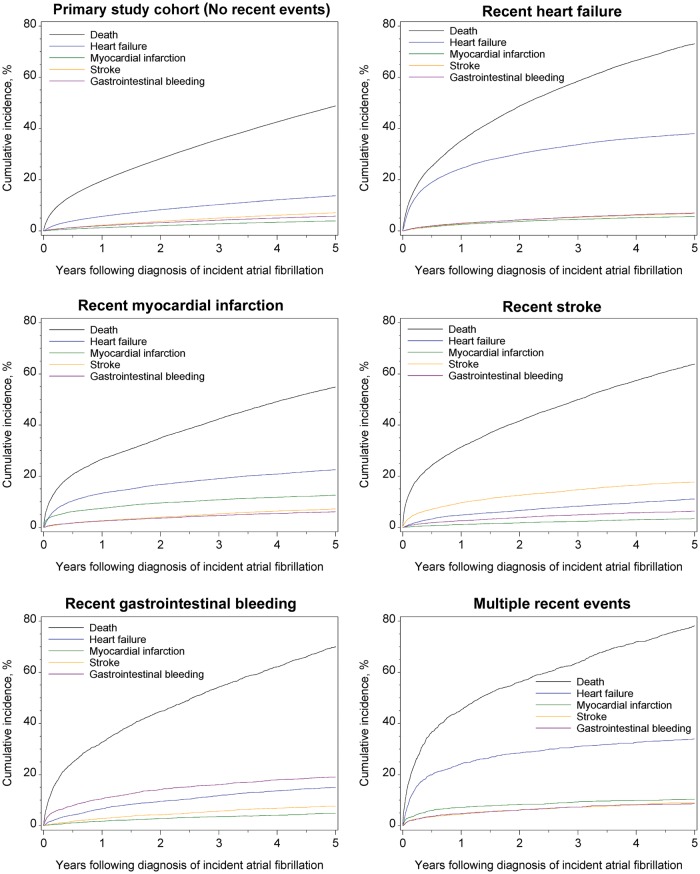
Figure 1 shows the cumulative incidence of each event over 5 years after the diagnosis of atrial fibrillation. Mortality was the most common event after the diagnosis of atrial fibrillation, with a cumulative incidence of 19.5% at 1 year and 48.8% at 5 years. At 5 years, 13.7% of the patients with incident atrial fibrillation had a hospitalization or emergency department visit for heart failure, 7.1% developed new-onset stroke, and 5.7% had gastrointestinal bleeding (Table 2). Myocardial infarction was the least frequent event, with a cumulative incidence of 1.2% at 1 year and 3.9% at 5 years. In a sensitivity analysis that considered all hospitalizations and emergency department visits, regardless of subsequent inpatient mortality, the findings were similar.
Figure 1.
Observed cumulative incidence of events in the 5 years after the diagnosis of incident atrial fibrillation by study cohort. Numbers of patients at risk of death over time.
Table 2.
Observed cumulative incidence of events over 1, 2, and 5 years after the diagnosis of incident atrial fibrillation by study cohort
| Outcome | Study cohort |
|||||
|---|---|---|---|---|---|---|
| No recent events (n = 186 461)a | Recent heart failure (n = 17 928)a | Recent myocardial infarction (n = 12 408)a | Recent stroke (n = 8801)a | Recent gastrointestinal bleeding (n = 3633)a | Multiple recent events (n = 1709)a | |
| 1 year, n (%) | ||||||
| Death | 36 153 (19.5) | 6260 (35.2) | 3286 (26.6) | 2748 (31.4) | 1181 (32.7) | 770 (45.3) |
| Heart failure | 10 499 (5.7) | 4329 (24.3) | 1649 (13.4) | 419 (4.8) | 240 (6.7) | 411 (24.2) |
| Myocardial infarction | 2272 (1.2) | 444 (2.5) | 915 (7.4) | 95 (1.1) | 62 (1.7) | 121 (7.1) |
| Stroke | 4122 (2.2) | 495 (2.8) | 317 (2.6) | 842 (9.6) | 104 (2.9) | 78 (4.6) |
| Gastrointestinal bleeding | 3751 (2.0) | 526 (3.0) | 303 (2.5) | 225 (2.6) | 382 (10.6) | 80 (4.7) |
| 2 years, n (%) | ||||||
| Death | 51 778 (28.2) | 8595 (48.7) | 4274 (34.9) | 3611 (41.5) | 1601 (44.6) | 949 (56.2) |
| Heart failure | 15 170 (8.3) | 5320 (30.0) | 2048 (16.7) | 571 (6.6) | 341 (9.5) | 481 (28.4) |
| Myocardial infarction | 3723 (2.0) | 646 (3.7) | 1169 (9.5) | 151 (1.7) | 102 (2.9) | 141 (8.3) |
| Stroke | 6825 (3.7) | 751 (4.3) | 486 (4.0) | 1092 (12.6) | 154 (4.3) | 104 (6.2) |
| Gastrointestinal bleeding | 5912 (3.2) | 762 (4.3) | 441 (3.6) | 338 (3.9) | 509 (14.2) | 103 (6.1) |
| 5 years, n (%) | ||||||
| Death | 82 917 (48.8) | 12 183 (73.1) | 6314 (54.9) | 5194 (63.7) | 2345 (70.1) | 1252 (78.1) |
| Heart failure | 23 389 (13.7) | 6509 (37.9) | 2650 (22.6) | 890 (11.1) | 503 (15.0) | 560 (33.9) |
| Myocardial infarction | 6597 (3.9) | 934 (5.6) | 1486 (12.6) | 270 (3.4) | 159 (4.8) | 169 (10.3) |
| Stroke | 11 920 (7.1) | 1124 (6.8) | 814 (7.2) | 1462 (17.7) | 255 (7.7) | 142 (8.9) |
| Gastrointestinal bleeding | 9748 (5.7) | 1156 (7.0) | 700 (6.1) | 517 (6.4) | 654 (19.1) | 139 (8.6) |
aRecent events were events within 3 months before the diagnosis of atrial fibrillation.
Figure 1 and Table 2 also show the incidence of clinical events among patients with recent heart failure, myocardial infarction, stroke, gastrointestinal haemorrhage, or multiple events in the secondary study cohorts. Among patients with recent heart failure, the cumulative incidence of heart failure hospitalization was 37.0% at 5 years and the cumulative incidence of death was 73.1% at 5 years (Table 2). In patients with recent stroke, the most frequent non-fatal event after a diagnosis of atrial fibrillation was recurrent stroke (17.7% at 5 years). Among patients with any recent events, the cumulative incidence of death at 5 years was greatest among patients with multiple events (78.1%) and lowest among those with prior myocardial infarction (54.9%)
When we analysed rates of events by the setting of the atrial fibrillation diagnosis, the cumulative incidence of mortality was higher among patients diagnosed in inpatient settings. For example, 1-year cumulative incidence of mortality was 55.7% among patients with an inpatient diagnosis, compared with 38.4% among those with an outpatient diagnosis. The cumulative incidence rates of heart failure, myocardial infarction, stroke, and gastrointestinal bleeding were similar between patients diagnosed in inpatient and outpatient settings (Figure 2). Table 3 shows the cumulative incidence rates of mortality, heart failure, myocardial infarction, stroke, and gastrointestinal bleeding in other subgroups. All outcome rates increased with older age and higher CHADS2 scores.
Figure 2.
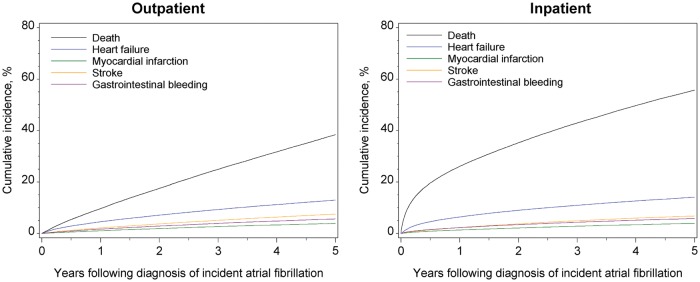
Observed cumulative incidence of events in the 5 years after the diagnosis of incident atrial fibrillation by setting of diagnosis in the primary study cohort. Numbers of patients at risk of death over time.
Table 3.
Observed cumulative incidence of events over 5 years after the diagnosis of incident atrial fibrillation by the subgroup of the primary study cohort
| Subgroup | No. of patients | Cumulative incidence, n (%) |
||||
|---|---|---|---|---|---|---|
| Mortality | Heart failure | Myocardial infarction | Stroke | Gastrointestinal bleeding | ||
| Sex | ||||||
| Female | 103 382 | 46 105 (49.0) | 13 233 (14.0) | 3482 (3.7) | 7456 (8.0) | 5579 (5.9) |
| Male | 83 079 | 36 812 (48.5) | 10 156 (13.3) | 3115 (4.2) | 4464 (6.0) | 4169 (5.5) |
| Age group | ||||||
| 67–69 year | 16 294 | 4211 (28.8) | 1626 (11.0) | 471 (3.3) | 728 (5.0) | 644 (4.4) |
| 70–74 year | 37 153 | 10 876 (32.3) | 4082 (12.1) | 1199 (3.6) | 1902 (5.7) | 1652 (4.9) |
| 75–79 year | 44 396 | 16 155 (40.1) | 5401 (13.3) | 1538 (3.9) | 2749 (6.9) | 2375 (5.9) |
| 80–84 year | 41 450 | 19 603 (52.1) | 5710 (15.1) | 1611 (4.3) | 3023 (8.1) | 2402 (6.4) |
| 85–89 year | 28 657 | 17 526 (67.0) | 4179 (15.8) | 1161 (4.4) | 2324 (8.9) | 1741 (6.6) |
| ≥ 90 year | 18 511 | 14 546 (84.3) | 2391 (13.7) | 617 (3.6) | 1194 (6.9) | 934 (5.4) |
| Setting of incident diagnosis of atrial fibrillation | ||||||
| Outpatient setting | 74 364 | 25 276 (38.4) | 8756 (13.0) | 2602 (3.9) | 5009 (7.5) | 3778 (5.7) |
| Inpatient setting | 112 097 | 57 641 (55.7) | 14 633 (14.1) | 3995 (3.9) | 6911 (6.8) | 5970 (5.8) |
| CHADS2 score | ||||||
| 0–1 | 35 719 | 10 124 (31.0) | 2039 (6.3) | 859 (2.7) | 1594 (4.9) | 1229 (3.8) |
| 2–4 | 125 351 | 57 294 (50.4) | 16 883 (14.7) | 4455 (4.0) | 8261 (7.3) | 6860 (6.0) |
| 5–6 | 25 391 | 15 499 (66.9) | 4467 (19.1) | 1283 (5.6) | 2065 (9.0) | 1659 (7.2) |
Discussion
Clinicians have several important treatment goals for patients with atrial fibrillation, including prevention of stroke, heart rate control, rhythm control, and improving quality of life. Counselling patients and prescribing therapies require knowledge of the risks of various clinical events, including cardiovascular events, gastrointestinal bleeding due to anticoagulation therapy, and mortality. We examined rates and risk factors for clinical events among 230 940 Medicare beneficiaries after a diagnosis of incident atrial fibrillation.
As may be expected in an older cohort, mortality rates were high. Nearly half of the primary study cohort, those without a major cardiovascular or bleeding event in the 3 months before the diagnosis of atrial fibrillation, died in the 5 years after the diagnosis of atrial fibrillation. Rates were higher in the secondary study cohorts, which consisted of beneficiaries who had experienced one or more recent events in the 3 months before the diagnosis of atrial fibrillation.
Among the major nonfatal events we examined—hospitalization or emergency department visit for heart failure, myocardial infarction, stroke, and gastrointestinal bleeding—heart failure was most common and myocardial infarction was the least common in the primary cohort. In the secondary cohorts, non-fatal event rates varied depending on which recent event a patient had experienced. In general, risk of heart failure hospitalization was still high, eclipsed only by the risk of stroke among patients with a recent stroke and the risk of gastrointestinal bleeding among patients with a recent bleeding event.
Despite effective pharmacological prophylaxis, stroke remains an important complication of atrial fibrillation.8 However, in terms of absolute risk, older patients with atrial fibrillation are twice as likely to develop heart failure as to develop stroke.9–12 Although the importance of stroke prevention cannot be overemphasized, our findings highlight the disproportionate burden of heart failure in patients with atrial fibrillation. Given the high risk of incident heart failure among patients with atrial fibrillation, and the poor outcomes of patients with both conditions,9,10 prevention and management of heart failure in patients with atrial fibrillation requires attention. Ours and other studies suggest that prevention of heart failure should be elevated alongside stroke prevention as a key priority in the management of patients with atrial fibrillation.2,12
Data from a variety of observational studies have shown that atrial fibrillation is associated with greater mortality,8 regardless of the presence or absence of previous cardiovascular disease.13 Furthermore, the risk of death is greatest in the first year after a new diagnosis of atrial fibrillation. The overall risk of death 1 year after diagnosis approaches 25% and is higher in critically ill patients, such as those with sepsis.1,14,15 In our primary cohort of older patients with incident atrial fibrillation and no recent events, the risk of death was more than three-fold greater than the occurrence of heart failure and seven-fold greater than the occurrence of stroke. In addition, the risk of death was higher among patients diagnosed with atrial fibrillation in inpatient settings, despite relatively similar risks of incident heart failure, stroke, and myocardial infarction. Our data suggest that, regardless of the mechanism, incident atrial fibrillation is a powerful marker for 1-year and 5-year mortality in older adults.
In the secondary cohorts of patients with recent cardiovascular or gastrointestinal bleeding events, those who developed incident atrial fibrillation also had a high risk of death in intermediate and long-term follow-up. These poor outcomes are consistent with prior observations in patients with concomitant atrial fibrillation and heart failure.16 In general, patients with recent cardiovascular or bleeding events were at a high risk of a recurrent event after their first diagnosis of atrial fibrillation, particularly in the case of heart failure. Consistent with other studies of populations with atrial fibrillation, patients with previous myocardial infarction had a higher risk of myocardial infarction, and patients with previous bleeding events a higher risk of subsequent bleeding events.17,18 Taken together, these findings confirm that mortality is common among older patients with recent cardiovascular and bleeding events and that future events tend to mirror the patient's recent medical history.
Our study has several limitations. First, the data are from a Medicare population, so the findings may not be generalizable to younger populations. Secondly, Medicare beneficiaries who accessed health care through other programmes before enrolling in Medicare may have been incorrectly classified as having incident atrial fibrillation if a previous diagnosis was not documented during the Medicare enrolment examination. Also, Medicare data do not include information on cause of death. Our analysis cannot shed light on the distribution of underlying causes of death in patients with atrial fibrillation. Finally, claims data are inherently limited with respect to clinical characteristics, because comorbid conditions are often not coded uniformly. As with any retrospective analysis, unmeasured covariates likely influenced the outcomes.
In summary, among non-fatal clinical events in patients with incident atrial fibrillation, heart failure was the most common event. After a new diagnosis of atrial fibrillation, the risk of heart failure hospitalization was more than two-fold greater than the risk of stroke over 5 years. Given the frequency and consequences of heart failure in patients with incident atrial fibrillation, greater emphasis on primary prevention of heart failure in patients with atrial fibrillation may be warranted.
Additional contributions
Damon M. Seils, MA, Duke University, provided editorial assistance. Mr Seils did not receive compensation for his assistance apart from his employment at the institution where the study was conducted.
Funding
This work was supported by the National Heart, Lung, and Blood Institute at the National Institutes of Health (grant numbers R01 HL102214, R01 HL068986).
Conflict of interest: J.P.P. reported receiving grant support from Johnson & Johnson and serving as a consultant to Forest Research Institute, Johnson & Johnson, and Medtronic. No other disclosures were reported. A.F.H., J.P.P., Setoguchi, and L.H.C. have made available online detailed listings of financial disclosures (http://www.dcri.duke.edu/about-us/conflict-of-interest/). The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
References
- 1.Piccini JP, Hammill BG, Sinner MF, Jensen PN, Hernandez AF, Heckbert SR, Benjamin EJ, Curtis LH. Incidence and prevalence of atrial fibrillation and associated mortality among Medicare beneficiaries, 1993–2007. Circ Cardiovasc Qual Outcomes. 2012;5:85–93. doi: 10.1161/CIRCOUTCOMES.111.962688. doi:10.1161/CIRCOUTCOMES.111.962688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stewart S, Hart CL, Hole DJ, McMurray JJ. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med. 2002;113:359–364. doi: 10.1016/s0002-9343(02)01236-6. doi:10.1016/S0002-9343(02)01236-6. [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine. Initial National Priorities for Comparative Effectiveness Research. Washington, DC: National Academies Press; 2009. http://www.nap.edu/openbook.php?record_id=12648 8 August 2012. [Google Scholar]
- 4.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. doi:10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 5.Birman-Deych E, Waterman AD, Yan Y, Nilasena DS, Radford MJ, Gage BF. Accuracy of ICD-9-CM codes for identifying cardiovascular and stroke risk factors. Med Care. 2005;43:480–485. doi: 10.1097/01.mlr.0000160417.39497.a9. doi:10.1097/01.mlr.0000160417.39497.a9. [DOI] [PubMed] [Google Scholar]
- 6.Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro Heart Survey on Atrial Fibrillation. Chest. 2010;137:263–272. doi: 10.1378/chest.09-1584. doi:10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- 7.Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the national registry of atrial fibrillation. JAMA. 2001;285:2864–2870. doi: 10.1001/jama.285.22.2864. doi:10.1001/jama.285.22.2864. [DOI] [PubMed] [Google Scholar]
- 8.Gajewski J, Singer RB. Mortality in an insured population with atrial fibrillation. JAMA. 1981;245:1540–1544. doi:10.1001/jama.1981.03310400022019. [PubMed] [Google Scholar]
- 9.Wann LS, Curtis AB, January CT, Ellenbogen KA, Lowe JE, Estes NA, 3rd, Page RL, Ezekowitz MD, Slotwiner DJ, Jackman WM, Stevenson WG, Tracy CM. Fuster V, Rydén LE, Cannom DS, Le Heuzey JY, Crijns HJ, Lowe JE, Curtis AB, Olsson S, Ellenbogen KA, Prystowsky EN, Halperin JL, Tamargo JL, Kay GN, Wann L. Jacobs AK, Anderson JL, Albert N, Hochman JS, Buller CE, Kushner FG, Creager MA, Ohman EM, Ettinger SM, Stevenson WG, Guyton RA, Tarkington LG, Halperin JL, Yancy CW 2011 Writing Group Members; 2006 Writing Committee Members; ACCF/AHA Task Force Members. 2011 ACCF/AHA/HRS focused update on the management of patients with atrial fibrillation (updating the 2006 guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;123:104–123. doi: 10.1161/CIR.0b013e3181fa3cf4. doi:10.1161/CIR.0b013e3181fa3cf4. [DOI] [PubMed] [Google Scholar]
- 10.Alonso A, Agarwal SK, Soliman EZ, Ambrose M, Chamberlain AM, Prineas RJ, Folsom AR. Incidence of atrial fibrillation in whites and African-Americans: the Atherosclerosis Risk in Communities (ARIC) study. Am Heart J. 2009;158:111–117. doi: 10.1016/j.ahj.2009.05.010. doi:10.1016/j.ahj.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Torp-Pedersen C, Møller M, Bloch-Thomsen PE, Køber L, Sandøe E, Egstrup K, Agner E, Carlsen J, Videbaek J, Marchant B, Camm AJ. Dofetilide in patients with congestive heart failure and left ventricular dysfunction. N Engl J Med. 1999;341:857–865. doi: 10.1056/NEJM199909163411201. doi:10.1056/NEJM199909163411201. [DOI] [PubMed] [Google Scholar]
- 12.Wang TJ, Larson MG, Levy D, Vasan RS, Leip EP, Wolf PA, D'Agostino RB, Murabito JM, Kannel WB, Benjamin EJ. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation. 2003;107:2920–2925. doi: 10.1161/01.CIR.0000072767.89944.6E. doi:10.1161/01.CIR.0000072767.89944.6E. [DOI] [PubMed] [Google Scholar]
- 13.Benjamin EJ, Wolf PA, D'Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998;98:946–952. doi: 10.1161/01.cir.98.10.946. doi:10.1161/01.CIR.98.10.946. [DOI] [PubMed] [Google Scholar]
- 14.Miyasaka Y, Barnes ME, Bailey KR, Cha SS, Gersh BJ, Seward JB, Tsang TS. Mortality trends in patients diagnosed with first atrial fibrillation: a 21-year community-based study. J Am Coll Cardiol. 2007;49:986–992. doi: 10.1016/j.jacc.2006.10.062. doi:10.1016/j.jacc.2006.10.062. [DOI] [PubMed] [Google Scholar]
- 15.Walkey AJ, Wiener RS, Ghobrial JM, Curtis LH, Benjamin EJ. Incident stroke and mortality associated with new-onset atrial fibrillation in patients hospitalized with severe sepsis. JAMA. 2011;306:2248–2254. doi: 10.1001/jama.2011.1615. doi:10.1001/jama.2011.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Olsson LG, Swedberg K, Ducharme A, Granger CB, Michelson EL, McMurray JJ, Puu M, Yusuf S, Pfeffer MA CHARM Investigators. Atrial fibrillation and risk of clinical events in chronic heart failure with and without left ventricular systolic dysfunction: results from the Candesartan in Heart failure-Assessment of Reduction in Mortality and morbidity (CHARM) program. J Am Coll Cardiol. 2006;47:1997–2004. doi: 10.1016/j.jacc.2006.01.060. doi:10.1016/j.jacc.2006.01.060. [DOI] [PubMed] [Google Scholar]
- 17.Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138:1093–1100. doi: 10.1378/chest.10-0134. doi:10.1378/chest.10-0134. [DOI] [PubMed] [Google Scholar]
- 18.Hohnloser SH, Oldgren J, Yang S, Wallentin L, Ezekowitz M, Reilly P, Eikelboom J, Brueckmann M, Yusuf S, Connolly SJ. Myocardial ischemic events in patients with atrial fibrillation treated with dabigatran or warfarin in the RE-LY (Randomized Evaluation of Long-Term Anticoagulation Therapy) trial. Circulation. 2012;125:669–676. doi: 10.1161/CIRCULATIONAHA.111.055970. doi:10.1161/CIRCULATIONAHA.111.055970. [DOI] [PubMed] [Google Scholar]