Abstract
Oral mucosa has been the most popular substitute material for urethral reconstructive surgery because it is easy to harvest, is easy to access, has a concealed donor site scar, and obviates most of the problems associated with other grafts. However, the success of using oral mucosa for urethral surgery is mainly attributed to the biological properties of this tissue. Herein, the surgical steps of harvesting oral mucosa from the inner cheek are presented with an emphasis on tips and tricks to render the process easier and more reproducible and to prevent intra and post-operative complications. The following steps are emphasized: Nasal intubation, ovoid shape graft, delicate harvesting leaving the muscle intact, donor site closure and removal of submucosal tissue.
Keywords: Cheek, free graft, mouth, one-stage urethroplasty, oral mucosa, urethra
INTRODUCTION
The first use of oral mucosa for urethral reconstruction was reported in the 19th century by two Ukrainian surgeons.[1,2] In 1984, Sapezhko published four clinical cases of urethroplasty with autologous tubularized oral mucosa grafts and in 1902, Tyrmos described two cases of oral mucosa grafts in two patients with a urethral fistula following lithotomy.[1,2] In Europe, a British surgeon, Humby, is credited with the first use of oral mucosal graft for urethral reconstruction.[1,2] In 1941, Humby fully described the use of oral mucosa from the lower lip in an 8-year-old child with peno-scrotal fistula due to previously failed hypospadias repair.[3] In 1992, Burger et al., from Germany, popularized the use of oral mucosa graft for urethral reconstruction in six patients with failed hypospadias/epispadias repair, after having successfully tested the technique on an animal model.[4] This series represents a hallmark study, as it describes transnasal intubation to render the harvesting process easier for the surgeon, and infiltration with a 1% lidocaine (1 part in 100,000) epinephrine solution of the donor site submucosa to guarantee better hemostasis.[4] In the same year, Dessanti et al., from Italy, also described the use of oral mucosa for primary hypospadias repair in eight children.[5] After the success of these two series, oral mucosa has been widely used, mainly in pediatric reconstructive urethral surgery.[6] In 1993, El-Kasaby et al., described the use of oral mucosa from the lip for the repair of penile and bulbar urethral strictures in 20 patients.[7] The technique of harvesting oral mucosa from the inner cheek was standardized by Morey and McAninch in 1996.[8] These authors used the Steinhäuser mucosa stretcher and suggested that two teams work simultaneously, one harvesting the oral mucosa and the other exposing the urethra and preparing the recipient site for grafting, in order to reduce operating time and the risk of cross contamination between the two surgical fields.[8]
The oral mucosa is now universally considered the best substitute material for penile and bulbar urethral stricture repair when one-stage techniques are used. Herein, the surgical steps of harvesting oral mucosa from the inner cheek are presented with an emphasis on tips and tricks to render the process easier and more reproducible, and to prevent intra-and postoperative complications.
PLANNING AND PREPARATION
One-stage urethroplasty with oral mucosa graft is feasible in all patients presenting with uncomplicated urethral strictures in the penile or bulbar urethra. Oral mucosa may also be used in patients with previous failed urethroplasty or with recurrent strictures following repeated direct vision optical urethrotomy. Patient age does not influence the success rate and thus this technique should not be denied to older patients.
Preoperative evaluation includes clinical history, physical examination, midstream urine culture, post-voiding residual measurement, uroflowmetry, urethral ultrasound, and retrograde and voiding urethrography. The patient's clinical history as well as stricture etiology, site, and length are carefully evaluated preoperatively to define the characteristics needed in the oral mucosal graft. The patient is fully examined to exclude any ongoing infectious disease affecting the mouth (such as Candida, varicella-virus or herpes virus) and to evaluate mouth opening and extension. Patients with restricted mouth opening or extension due to individual anatomical characteristics or due to previous mouth or tongue surgery are counselled that genital or extra-genital skin would be used for the urethroplasty if, during the anesthesia, access to the mouth cavity should be compromised. Patients who play a wind instrument are informed that oral mucosa harvesting may negatively influence this activity. Three days prior to surgery, the patient begins oral cleansing with a chlorhexidine mouthwash. The day before surgery prophylactic antibiotics are administered. In patients who chew tobacco or eat pan masala, the oral graft tends to have a diffuse fibrosis of the submucosal layer of the inner cheek.[9] In these patients, the use of retroauricolar skin should be an alternative.[10]
PROCEDURE
The patient is placed is a standard supine position for penile urethroplasty and in a simple lithotomy, with the calves placed in Allen stirrups, for bulbar urethroplasty. The surgical steps are illustrated in Figures 1–10.
Figure 1.

(a and b) After preparation with chlorhexidine, the two surgical fields are draped separately (a). Two surgical teams work simultaneously harvesting the oral mucosa and preparing the urethra for grafting. In order to prevent cross contamination, each team uses its own set of surgical instruments including suction and bipolar cautery. (b) The mouth retractor has its own light and provides excellent exposure of the cheek and, therefore, no assistant is required
Figure 10.
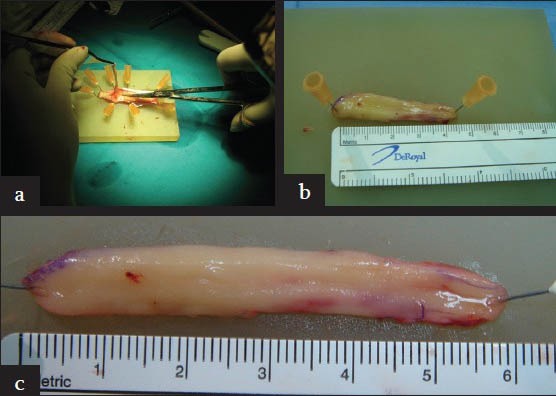
(a, b, and c) The graft is stabilized on a silicone board using insulin needles. Once all submucosal tissue is carefully excised with iris scissors (a), the graft is tailored according to site, length, and stricture characteristics. While removing all the submucosal tissue, it is paramount to not excessively thin the graft, as thin grafts are more likely to heal with contracture. If the preparation of the graft is adequate, an average 4 cm long graft will stretch up to 6 cm due to the intrinsic elasticity of the mucosa (b and c). Two 6 cm long grafts (one from each cheek) are enough to repair the vast majority of penile or bulbar strictures using one-stage techniques
Figure 2.
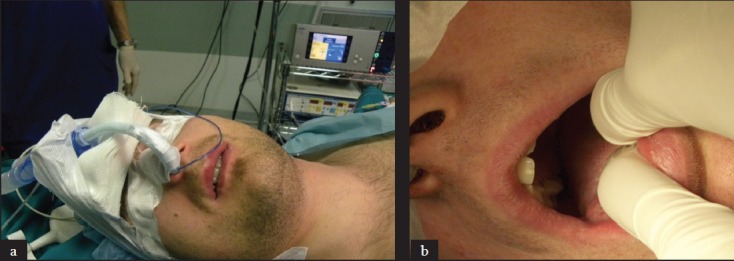
(a and b) The patient is intubated through the nose in order to free the oral cavity and provide the surgeon with more space. Although oral mucosa graft can be harvested even in the presence of oro-tracheal intubation by the expert surgeon, nasal intubation is particularly useful for surgeons at the beginning of their learning curve or in patients with a small or limited mouth opening. In the case of oro-tracheal intubation, the tube should be reinforced to avoid inadvertent compression by the mouth retractor. It should be shifted to the side opposite to the cheek from which the graft is being harvested to provide enough room for the surgeon
Figure 3.
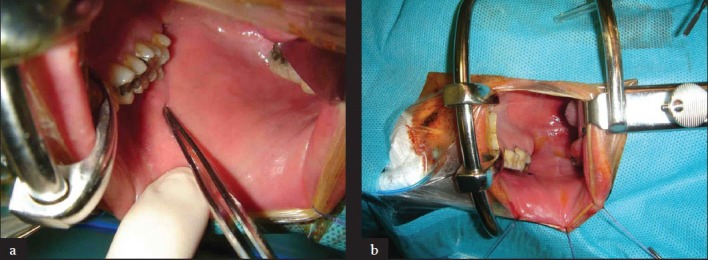
(a and b) The inner mucosal surface of the cheek is cleaned. A Kilner-Doughty mouth retractor is put in place to retract the jaws and expose the donor site, and the duct of the parotid gland (Stensen's duct) is identified and marked in proximity of the second molar. If the Stensen's duct cannot be clearly identified, secretion from the parotid gland can be stimulated by applying some drops of lemon juice to the tongue. Three stay sutures are placed along the edge of the mouth in order to keep the oral mucosa adequately stretched
Figure 4.
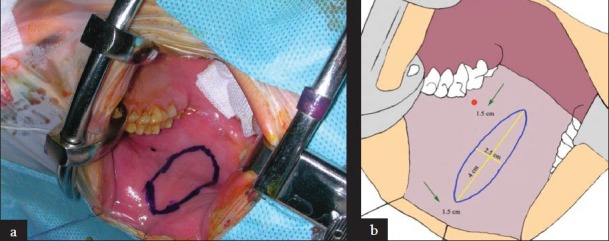
(a and b) The graft is usually harvested in an ovoid shape, to allow for easier primary closure of the donor site and because the penile or bulbar urethral opening for one-stage urethroplasty is in an ovoid shape (a). Ideally the graft should be harvested 1.5 cm from the Stensen's duct and 1.5 cm from the external edge of the cheek (b). Although the size of the graft varies according to the size of the cheek and to the length of the strictured urethra, for standard one-stage penile or bulbar urethroplasty, it should be 4 cm long and 2.5 cm wide
Figure 5.
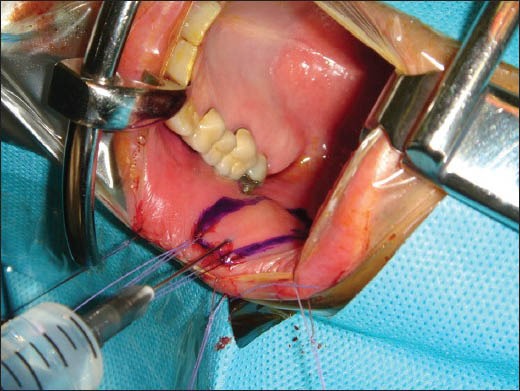
Two traction stitches are applied to the distal edge of the graft and 10 ml of solution with bupivacaine HCL 2.5 mg/ml and epinephrine acid tartrate 0.0091 mg (0.005 mg epinephrine) are injected along the edges of the graft to promote hemostasis and to assist in the dissection of the mucosa
Figure 6.
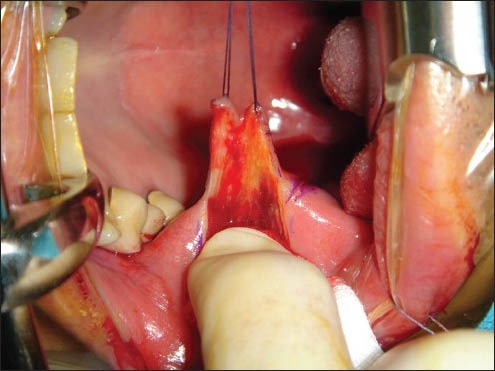
The outlined graft is harvested with the assistance of the 2 traction sutures using sharp dissection with iris scissors. It is paramount to dissect the graft in the plane between the muscle and the mucosa, as dissection deep in the muscle would lead to significant bleeding, while a more superficial dissection would compromise the quality of the graft
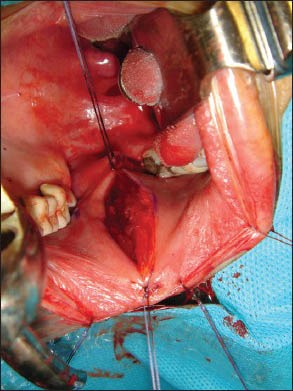
Figure 7.
Once the graft has been harvested, the donor site bed is accurately examined and any point of bleeding point is carefully controlled with bipolar electro cautery. The Stensen's duct is visible, well away from the donor site
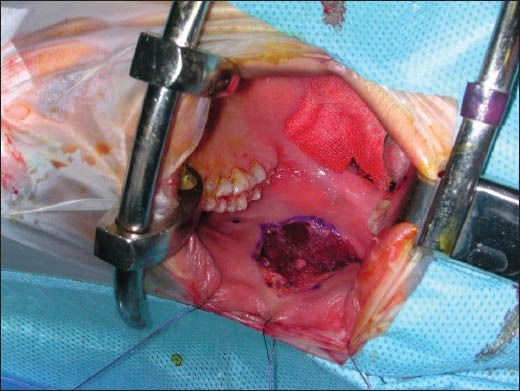
Figure 8.
Two traction sutures are passed at the distal and proximal apex of the donor site. When gentle traction is applied to these sutures, the two lateral margins of the donor site tend to approximate towards the midline and this makes primary closure easier and without tension
Figure 9.

The donor site is carefully closed with interrupted or running 4-zero polyglactin sutures. When necessary, another graft can be harvested from the contralateral cheek using the same technique
Recommended instruments
Kilner-Doughty mouth retractor (Lawton-Germany)
Bipolar electro-cautery
Ready-made syringe 10 ml (Bupisolver) containing bupivacaine HCL 2.5 mg/ml and epinephrine acid tartrate 0.0091 mg (0.005 mg epinephrine) (AltaSelect-Italy)
4/0 polyglactin (Vicryl*) to suture the harvesting site
Iris scissors
Silicone board-insulin needles
Ice bag
The following tips may aid the successful harvest and use of buccal mucosal grafts:
-
i)
The use of double team may prevent cross contamination of the surgical fields.
-
ii)
The use of mouth retractors provides superior exposure and helps identify all the surgical landmarks.
-
iii)
If the shape of the graft is ovoid, donor site morbidity can be minimized and allows tension free closure of the defect.[11,12,13]
-
iv)
If the size of the graft exceeds 4 × 2.5 cm, closure of the donor site defects may be under tension.
-
v)
Suturing the donor site may reduce the risk of bleeding and promote quicker healing.[11,12,13]
POSTOPERATIVE CARE
An ice bag is applied on the cheek to reduce pain and prevent the formation of hematomas. In order to minimize discomfort, patients are initially kept on clear fluid and ice cream and progressively switched to a regular diet on postoperative day 2; regular rinsing with chlorhexidine mouth wash is continued for 3 days. Ambulation is encouraged from postoperative day 1 and the patient is usually discharged home within 3 days on broad-spectrum oral antibiotics, which are continued till the removal of the catheter.
CONCLUSIONS
The technique described is simple, reliable, and easily reproducible. However, appropriate surgical instrument must be available and the previously described fundamental steps must be followed meticulously to achieve adequate results and minimize complication rates. Using this technique to harvest the graft from both cheeks, it is possible to harvest enough mucosa to repair most penile or bulbar urethral strictures using one-stage techniques.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Korneyev I, Ilyin D, Schultheiss D, Schultheiss D, Chapple C. The first oral mucosal graft urethroplasty was carried out in the 19th century: The pioneering experience of Kirill Sapezhko (1857-1928) Eur Urol. 2012;62:624–7. doi: 10.1016/j.eururo.2012.06.035. [DOI] [PubMed] [Google Scholar]
- 2.Schultheiss D, Gabouev AI, Korneyev I. Re: Buccal mucosal grafts: Lessons learned from an 8-year experience. J Urol. 2002;168:202–3. [PubMed] [Google Scholar]
- 3.Humby G. A one-stage operation for hypospadias. Br J Surg. 1941;29:84–92. [Google Scholar]
- 4.Bürger RA, Müller SC, el-Damanhoury H, Tschakaloff A, Riedmiller H, Hohenfellner R. The buccal mucosa graft for urethral reconstruction: A preliminary report. J Urol. 1992;147:662–4. doi: 10.1016/s0022-5347(17)37340-8. [DOI] [PubMed] [Google Scholar]
- 5.Dessanti A, Rigamonti W, Merulla A, Falchetti D, Caccia G. Autologous buccal mucosa graft for hypospadias repair: An initial report. J Urol. 1992;147:1081–3. doi: 10.1016/s0022-5347(17)37478-5. [DOI] [PubMed] [Google Scholar]
- 6.Markiewicz MR, Lukose MA, Margarone JE, 3rd, Barbagli G, Miller KS, Chuang SK. The oral mucosa graft: A systematic review. J Urol. 2007;178:387–94. doi: 10.1016/j.juro.2007.03.094. [DOI] [PubMed] [Google Scholar]
- 7.el-Kasaby AW, Fath-Alla M, Noweir AM, el-Halaby MR, Zakaria W, el-Beialy MH. The use of buccal mucosa patch graft in the management of anterior urethral strictures. J Urol. 1993;149:276–8. doi: 10.1016/s0022-5347(17)36054-8. [DOI] [PubMed] [Google Scholar]
- 8.Morey AF, McAninch JW. When and how to use buccal mucosal grafts in adult bulbar urethroplasty. Urology. 1996;48:194–8. doi: 10.1016/S0090-4295(96)00154-9. [DOI] [PubMed] [Google Scholar]
- 9.Chhaya VA, Sinha V, Rathor R, Modi N, Rashmi GS, Parma V, et al. Oral submucus fibrosis-surgical treatment with CO2 laser. Word articles in ENT. 2012:3. [Google Scholar]
- 10.Manoj B, Sanjeev N, Pandurang PN, Jaideep M, Ravi M. Postauricolar skin as an alterrnative to oral mucosa for anterior onaly graft urethroplasty: A preliminary experience in patients with oral mucosa changes. Urology. 2009;74:345–8. doi: 10.1016/j.urology.2009.02.065. [DOI] [PubMed] [Google Scholar]
- 11.Barbagli G, Vallasciani S, Romano G, Fabbri F, Guazzoni G, Lazzeri M. Morbidity of oral mucosa graft harvesting from a single cheek. Eur Urol. 2010;58:33–41. doi: 10.1016/j.eururo.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 12.Rourke K, McKinny S, St. Martin B. Effect of wound closure on buccal mucosal graft harvest site morbidity: Results of a randomized prospective trial. Urology. 2012;79:443–7. doi: 10.1016/j.urology.2011.08.073. [DOI] [PubMed] [Google Scholar]
- 13.Barbagli G, Lazzeri M, Rourke, et al. Effect of wound closure on buccal mucosal graft harvest site morbidity: Results of a randomized prospective trial (urology 2012;79:443-448) Urology. 2012;80:741–2. doi: 10.1016/j.urology.2011.08.073. [DOI] [PubMed] [Google Scholar]


