Abstract
The development of miniaturized nephroscopes which allow one-stage stone clearance with minimal morbidity has brought the role of shock wave lithotripsy (SWL) in stone management into question. Design innovations in SWL machines over the last decade have attempted to address this problem. We reviewed the recent literature on SWL using a MEDLINE/PUBMED research. For commenting on the future of SWL, we took the subjective opinion of two senior urologists, one mid-level expert, and an upcoming junior fellow. There have been a number of recent changes in lithotripter design and techniques. This includes the use of multiple focus machines and improved coupling designs. Additional changes involve better localization real-time monitoring. The main goal of stone treatment today seems to be to get rid of the stone in one session rather than being treated multiple times non-invasively. Stone treatment in the future will be individualized by genetic screening of stone formers, using improved SWL devices for small stones only. However, there is still no consensus about the design of the ideal lithotripter. Innovative concepts such as emergency SWL for ureteric stones may be implemented in clinical routine.
Keywords: Endourology, extracorporeal shock wave lithotripsy, urolithiasis
INTRODUCTION
Within the last 25 years, the management of urinary stones has seen innovations such as percutaneous stone removal in the late 1970s, followed by extracorporeal shock wave lithotripsy (SWL) in 1980.[1,2,3,4] SWL held the sway in the 90s, but continuing developments in endourological equipment meant that percutaneous stone removal progressively became more attractive due to its potential of one-time complete clearance. There have been some recent innovations in lithotripter design and technique, which may improve outcomes with this non-invasive treatment modality.
We reviewed recent literature on SWL using a MEDLINE/PUBMED search using the key words “extracorporeal shock wave lithotripsy,” “shock wave lithotripsy,” “lithotripter,” and “shock wave generation.” Since the use of one modality over another also depends on surgeon preference, we took the subjective opinion of two senior urologists, one mid-level consultant, and one junior fellow (2nd year resident) to comment on the potential future role of SWL in stone management.
THE DECLINING ROLE OF SWL IN THE LAST DECADE
In the last decade, open surgery was almost completely replaced by the non-invasive SWL and endourologic techniques such as ureteroscopy (URS) and percutaneous nephrolithotomy (PCNL).[5] Renal stones less than 1-2 cm were treated by shock waves, whereas complicated kidney stones were managed by a combination of PCNL and SWL.[6,7] Ureteral stones were treated either by SWL or by URS, depending on stone size and localization. In 1988, 70% of stones were located in the kidney and 30% in the ureter,[8] and there was an enthusiastic attitude toward the use of SWL for all types of urinary calculi.[9]
The significant improvement of armamentarium meant that endourological techniques became more attractive and effective in stone management,[10] whereas technical improvement of SWL was minimal.[11] Miniaturization of endoscopes with significant improvement of video technology and techniques of stone fragmentation such as lasers accelerated the success of endourological approaches.[12,13,14,15] Moreover, the size and localization of urinary calculi changed with an increase of ureteral calculi to 50-60%. All this resulted in a decrease of SWL and an increase of URS, whereas PCNL use remained stable [Figure 1]. The main argument in favor of endourological techniques was that the stone could be removed in one session with minor sequelae in contrast to SWL which has a 20-30% re-treatment rate and the problems associated with passage of fragments.[12,13,14,15,16,17,18]
Figure 1.
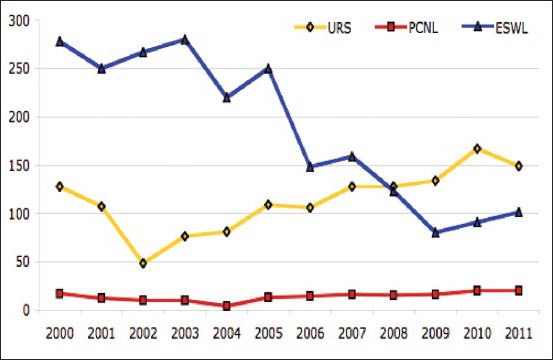
Development of primary treatment strategies for uroliothiasis at Department of Urology, SLK Kliniken Heilbronn, showing an increase of URS and decline of ESWL
RECENT DEVELOPMENTS IN LITHOTRIPTERS
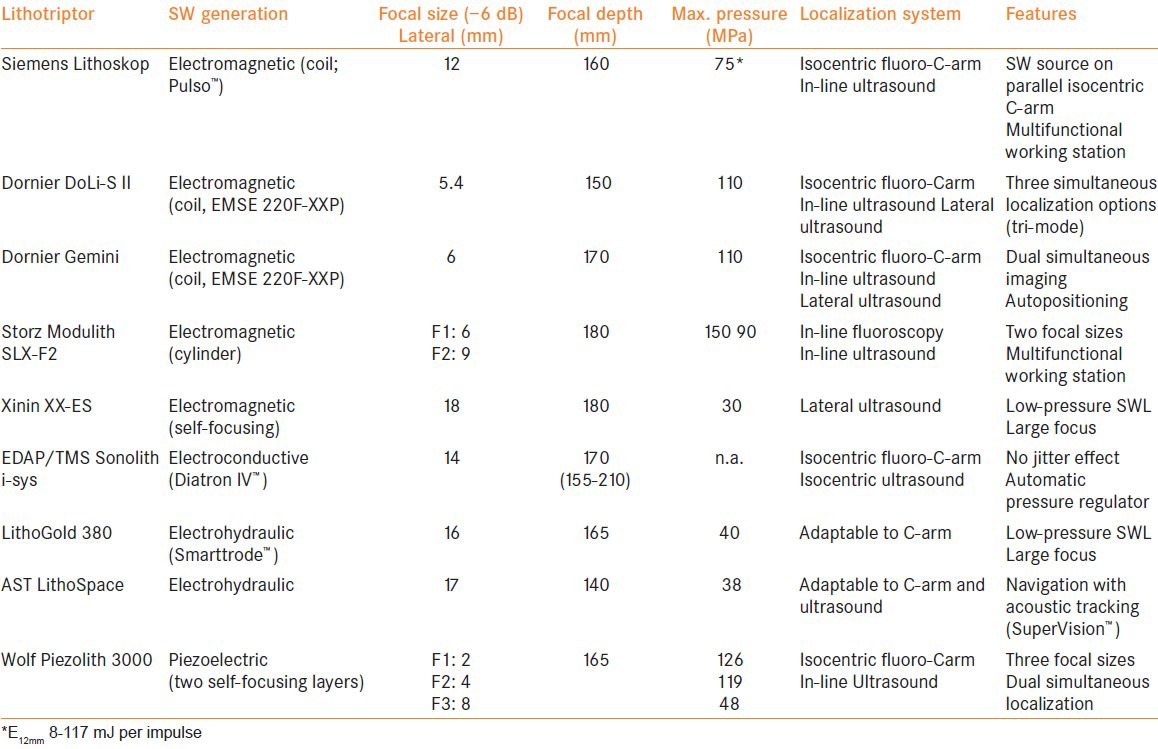
Recent studies on the mechanisms of stone disintegration, shock wave focusing, coupling, and application have appeared, which may address some of the problems associated with lithotripters.[11] Moreover, manufacturers have introduced new devices with significant modifications [Table 1] which, if used appropriately, may be helpful in rekindling an interest in SWL.[14] The introduction of new lithotripters appears to have increased the potential problems of shock wave application compared to first-generation devices, mainly due to the use of water cushion — based coupling of shock wave energy, ultrasound-based localization systems, and small focal sizes of the shockwave sources.[11,14]
Table 1.
Comparison of technical details of new lithotriptors
Clinical lithotripters are based on four different principles of shock wave generation. In electrohydraulic (EHL) lithotripters, spark discharge between two electrodes produces the shock wave. EHL devices have a shot-to-shot variability as the spark location changes as the electrodes wear down; the significance of this “jitter-effect” is under debate, with some suggesting it might be less relevant in large-focus sources.[19] The electroconductive system (EDAP-TMS, Lyon, France) employs electrodes immersed in a highly conductive solution, resulting in repeatable spark location due to shorter and self-adjusting inter-electrode distance to compensate for electrode wear.[11,20] Electrode lifetime exceeds 40,000 impulses. The idea of a dual-EHL system (Direx Duet, Tel Aviv, Israel) represents an interesting concept of distributing the shock wave energy on two applicators. In vitro, more impulses were required using the alternate mode (679 vs. 601), and in the kidney model, there was no advantage concerning renal injury.[21] However, clinically, there is only a small amount of data which confirms safety but no advantage over single-source SWL. The main reason for this are the problems with adequate coupling and acoustic windows to the calculus.[22] Electromagnetic and piezoelectric sources provide stable shock wave release lasting for >1 million shocks; however, instability of acoustic output may occur.[23]
Adaptation of the focal zone to stone size and localization seems to be another reasonable innovation.[24] A 1 cm distal ureteric stone may need to be treated with a relatively small focus, whereas a 1.5 cm stone in the renal pelvis may require a larger focus. Some lithotripter manufacturers have found ways to adjust focal width to suit such clinical applications. In Modulith SLX-F2 (Storz Medical, Germany), two focal sizes are obtained by modifying pulse duration using the same electromagnetic source. The larger focal zone (50 × 9 mm) is recommended for renal stones and the smaller focus (28 × 6 mm) for ureteral stones. However, no improvement of clinical efficacy has been shown. There is no clinical study that analyzes the impact of the F2 concept. De Sio et al.[25] evaluated only the smaller (original) focus size, and in the comparative study from Berne,[26] only the larger focus was taken. In this randomized controlled trial, the 3-month stone-free rate of HM3 was slightly higher compared to the use of F2 focus of the Modulith (90% vs. 81%). However, there are no data when using the standard smaller focus. Earlier studied showed a disintegration rate of 85% with Modulith SL 20.[27] Tiselius reported stone-free rates over 97% for ureteric stones using the classic and F2 machines. For 90 patients treated using the F2 focus, the success rates were similar to those of patients treated with the standard focus of the classic device.[28]
Double-layer arrangement of piezoelectric elements in Piezolith 3000 (Richard Wolf GmbH) increased shock wave energy after reducing the aperture from 50 to 30 cm.[29,30] Modifying the synchronization of both traveling waves allows variation of delay and pulse formation, resulting in three focal zones. However, the treatment has to be performed under intravenous analgesia. Retreatment rates are lower (10%), but so are the stone-free and success rates of 45% and 64%, respectively.[31,32] In contrast, the results obtained in children (using the small focal size) are excellent.[33] Nevertheless, there are no studies focusing on the use of three different focal zones as proposed by the manufacturer.
Broad-focus, low-pressure lithotripters (LithoSpace, LithoGold 380, Xinin XX-ES) have recently attracted attention as research showed that focal width affects stone breakage in several ways[11,34] [Table 1]. In vitro,[35] the disintegrative efficiency of Xinin XX-ES was superior to HM3 (634 vs. 831 SW). Early clinical results show that treatment is possible without any anesthesia and with minimal renal trauma (i.e. hematuria) [Figure 2a, b]. However, handling of lateral ultrasound device proved to be difficult and needs definitive improvement. Siemens[36] and Dornier[37] also aimed at creating larger focal zones by prolonged pulse duration, but do not offer different focal sizes. Arrabal-Polo[38] applied the focal applied energy quotient (FAEQ) to assess the efficacy of SWL with the DoLi-S (EMSE 220-XXP) device and observed equivalent results of SWL versus endoscopic lithotripsy with holmium laser in ureteral stones (94%) when FAEQ exceeded 10. This indicates better fluoroscopic localization and increase of shock wave energy delivered to the stone.
Figure 2.

The use of iPAD-assisted percutaneous access to the collecting system. In the future, tablet-based navigation might be also useful during ESWL
CLINICAL SWL TODAY
Young urologists favor endourology and are less interested in SWL. At several centers, only specially trained technicians, rather than urologists, perform SWL.[11] In some countries, reimbursement of SWL has become a problem, for example, in Germany, only one treatment per year is financed as outpatient. All this has resulted in a decrease of SWL procedures and a restriction of indications, particularly to renal stones larger than 1 cm and all kinds of ureteral calculi. SWL efficacy depends on various acoustic properties [Table 2]. Manufacturers and clinicians have addressed some of them (i.e. quality of coupling using a water cushion, ramping strategies), but for others (i.e. size of focal zone, amount of shock wave pressure), there is still no consensus. Bohris et al.[39] used a camera as a tool to control coupling quality and found imperfect coupling in 67% of the cases. In-line ultrasound probes enable an intraoperative check of coupling quality.[11] Unfortunately, the ideal lithotripter has not yet been constructed.
Table 2.
Factors influencing the success of extracorporeal shock wave lithotripsy
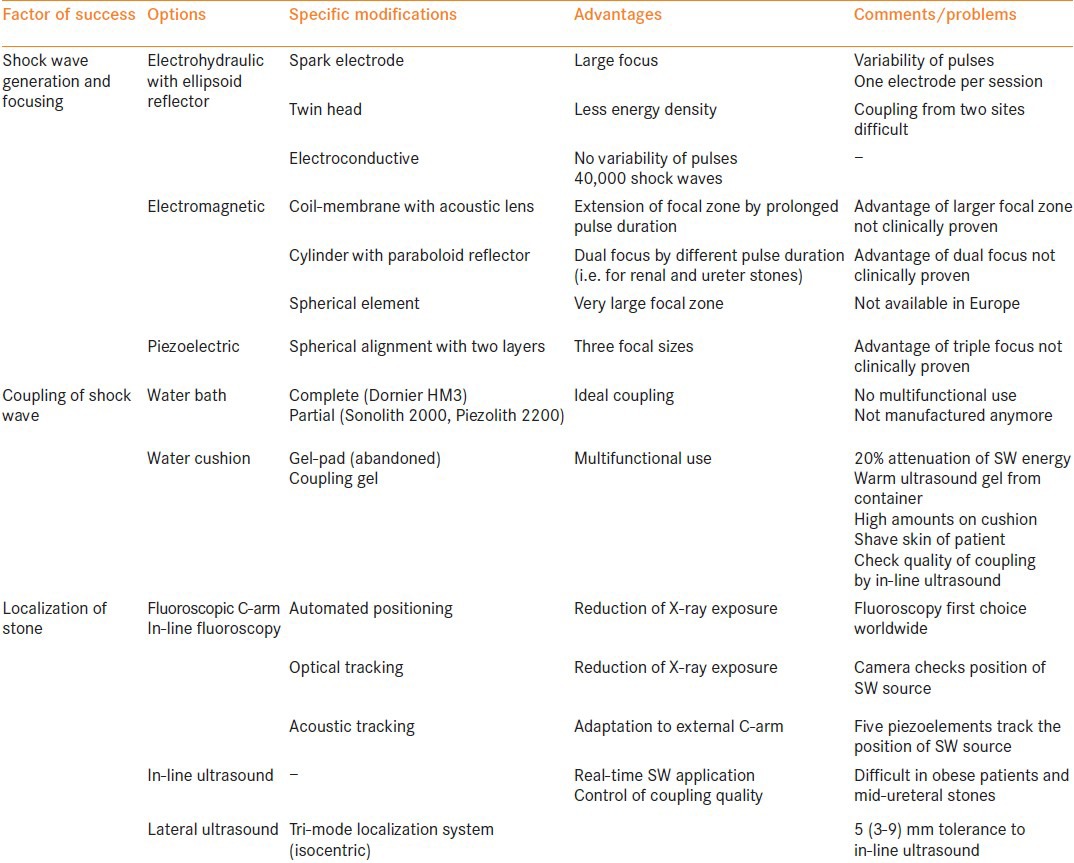
The reliable production of 2 mm dust, instead of fragmentation, is possible with SWL.[40] This would be possible with better shock wave generators (i.e. with larger focal zones), combination of different sources (i.e. piezoelectric plus EHL), respiratory regulated, color doppler ultrasound monitored hit-control [Figure 3], and computer-assisted shock wave navigation adapted to the individual anatomy, improving the quality of stone disintegration with almost complete pulverization of the stone and basically no side-effects applying shock wave without anesthesia [Figure 2a, b]. The non-invasive nature of SWL could be further supported by ultrasound-induced repositioning of renal stones, that is, from unfavorable locations like the lower calyx to the renal pelvis.[41]
Figure 3.
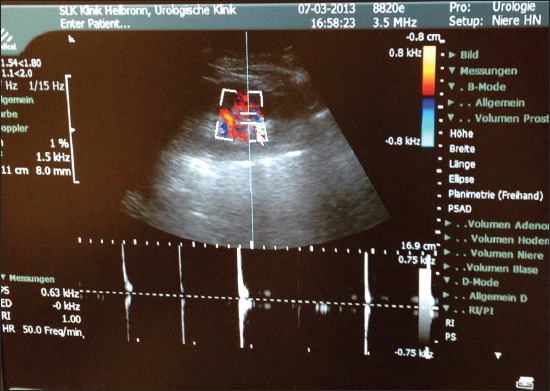
The use of color-coded duplex ultrasonography for localization of stones during ESWL. The CCD signal indicates by sound and graphics when the stone is hit by the shock wave. Moreover, the change of the signal may indicate breakage of the stone
OPINION
Even if the lifetime of knowledge becomes shorter and shorter, it takes usually 5-10 years for a novel technique to become accepted worldwide. For implementation of guidelines, it may take even longer. For example, the first patient was treated by SWL in 1980 and it was not approved by the US Food and Drug Administration (FDA) until 1986. Accordingly, some of the novel techniques being introduced today may not become commonly accepted for a number of years.[16]
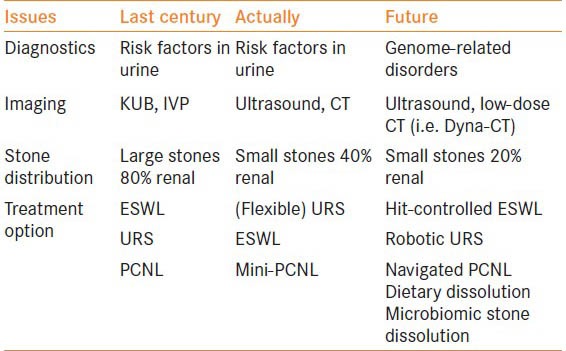
In general, to understand the predictable future of SWL in the management of urolithiasis, it is necessary to review three areas [Table 3]; imaging and diagnostics, evolving technology including the ideal lithotripter, and treatment strategies.
Table 3.
Trends in minimally invasive management of urolithiasis — The role of ESWL
Imaging and diagnostics
Static imaging will not be enough in the process of decision-making. All information has to be available during surgery in a way to guide the surgeon during the procedure (i.e. navigation). For this purpose, image fusion, virtual reality, molecular imaging, and marker-based navigation with miniaturized computers (i.e. iPad = surgical pad) will play an important role in the near future [Figure 4]. The development of these modalities will provide an information-rich anatomic platform that may well feed data into a truly robotic assembly such that tissue marked by the surgeon will then be neatly targeted.[42,43,44,45,46]
Figure 4.
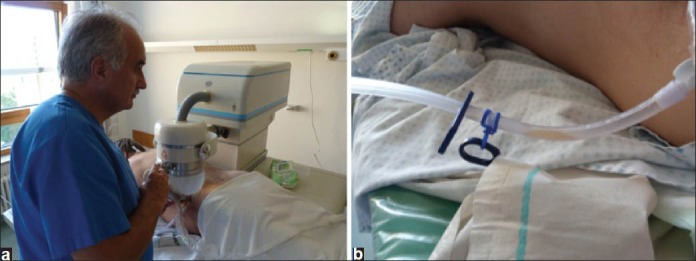
Early experience with the Xinin XX-ES lithotripter providing a self-focusing electromagnetic shock wave source with a large focal zone and lateral ultrasound localization. (a) ESWL for residual stones after PCNL with patient in prone position, no anesthesia or analgesia. (b) Urine output during ESWL shows no hematuria
Technology
Novel technology is the key for new treatment strategies. The principle of extracorporeal SWL revolutionized the treatment of urolithiasis. However, this principle has to be continuously elaborated. The progress in lithotripter technology focused mainly on the integration of the shock wave source into multifunctional fluoroscopic tables, rather than improving the efficacy of SWL. There are recent promising new data regarding increased efficacy and minimal trauma of SW sources with large focus [Figure 2, Table 1]. If they prove to be highly efficient, reducing the numbers of re-treatment by pulverization of the stone, this might induce resurgence in SWL.[14]
It is interesting that even after more than 30 years of intensive research, the ideal device has not been presented. Even worse, there is no general consensus about the criteria. It is obvious that the ideal device should be highly efficient in stone disintegration with minimal associated side effects. This could be evaluated using the Efficacy Quotient (EQ) in its different modifications.[9,14] However, there are other criteria; the treatment should be performed under intravenous analgesia or even without anesthesia and the lithotripter should represent a multifunctional endourological workstation. Evidently, some of these criteria are difficult to realize simultaneously. The water bath represents the optimal coupling method, but cannot be used in multifunctional tables. Larger aperture systems enable treatment almost without anesthesia; however, such systems have a very small focal zone requiring multiple sessions. Furthermore, such devices cannot be used as multifunctional workstations. Moreover, with the changing demands on the security of medical devices, the handling of the lithotripters has become more complicated.[14]
New theories for stone disintegration favor the use of shock wave sources with larger focal zones. Use of slower pulse rates, ramping strategies, and adequate coupling of the shock wave head can significantly increase the efficacy and safety of SWL [Table 2]. It seems difficult to realize “the ideal lithotripter”; however, manufacturers should keep in mind that SWL has to fight against endourology. All these procedures require general anesthesia, but offer immediate removal of the calculus. Indeed, some of the large focus lithotripters already enable SWL without any anesthesia or analgesia. However, these energy sources have to be combined with sophisticated localization systems. Early trials with charge-coupled device CCD-ultrasound indicate that the duplex signal may show when the stone is adequately hit by the shock wave and, probably also, when the stone starts to fragment [Figure 3].
Treatment strategies
The most important issue for a lithotripter today is good disintegration with a minimal number of sessions. Additionally, innovative concepts such as emergency SWL for ureteric stones should be implemented in clinical routine, even for children.[47,48] All urologists should be aware of the new trends and latest results of SWL research as basics in their training to optimize the clinical application. The strategies in the management of urinary calculi will not change significantly. Non-invasive SWL will survive for <1.5 cm stones in the renal pelvis and upper calices. However, the method is under pressure due to miniaturized endourology and, thus, to provide rapid cure of the stone disease in a single session. Otherwise, patients will prefer the minimally invasive percutaneous or transurethral techniques.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Chaussy C, Schmiedt E, Jocham D, Brendel W, Forssmann B, Walther V. First clinical experience with extracorporeally induced destruction of kidney stones by shock waves. J Urol. 1982;127:417–20. doi: 10.1016/s0022-5347(17)53841-0. [DOI] [PubMed] [Google Scholar]
- 2.Fuchs G, Miller K, Rassweiler J, Eisenberger F. Extracorporeal shock-wave lithotripsy: One-year experience with the Dornier lithotripter. Eur Urol. 1985;11:145–9. doi: 10.1159/000472479. [DOI] [PubMed] [Google Scholar]
- 3.Alken P, Hutschenreiter G, Günther R, Marberger M. Percutaneous stone manipulation. J Urol. 1981;125:463–6. doi: 10.1016/s0022-5347(17)55073-9. [DOI] [PubMed] [Google Scholar]
- 4.Clayman RV, Surya V, Miller RP, Castaneda-Zuniga WR, Smith AD, Hunter DH, Amplatz K, Lange PH. Percutaneous nephrolithotomy: Extraction of renal and ureteral calculi from 100 patients. J Urol. 1984;131:868–71. doi: 10.1016/s0022-5347(17)50686-2. [DOI] [PubMed] [Google Scholar]
- 5.Rassweiler J, Alken P. ESWL ‘90 — state of the art. Limitations and future trends of shock-wave lithotripsy. Urol Res. 1990;18(Suppl 1):S13–23. doi: 10.1007/BF00301523. [DOI] [PubMed] [Google Scholar]
- 6.Rassweiler J, Gumpinger R, Miller K, Hölzermann F, Eisenberger F. Multimodal treatment (extracorporeal shock wave lithotripsy and endourology) of complicated renal stone disease. Eur Urol. 1986;12:294–304. doi: 10.1159/000472642. [DOI] [PubMed] [Google Scholar]
- 7.Eisenberger F, Rassweiler J. Current status of ESWL in the management of renal calculus disease. Contrib Nephrol. 1987;58:236–52. doi: 10.1159/000414527. [DOI] [PubMed] [Google Scholar]
- 8.Schmidt A, Rassweiler J, Gumpinger R, Mayer R, Eisenberger F. (1990): Minimally invasive treatment of ureteric calculi using modern techniques. Brit J Urol. 1990;65:242–9. doi: 10.1111/j.1464-410x.1990.tb14719.x. [DOI] [PubMed] [Google Scholar]
- 9.Rassweiler J, Köhrmann KU, Potempa D, Henkel TO, Jünemann KP, Alken P. Extracorporeal shock wave lithotripsy for renal calculi: Current status and future aspects. Minimally Invasive Therapy. 1992;1:141–58. [Google Scholar]
- 10.Deane LA, Clayman RV. Advances in percutaneous nephrostolithotomy. Urol Clin North Am. 2007;34:383–95. doi: 10.1016/j.ucl.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 11.Rassweiler JJ, Knoll T, Köhrmann KU, McAteer JA, Lingeman JE, Cleveland RO, et al. Shock wave technology and application: An update. Eur Urol. 2011;59:784–96. doi: 10.1016/j.eururo.2011.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Turney BW. Trends in urological stone disease. BJU Int. 2011;24:382–6. doi: 10.1111/j.1464-410X.2011.10495.x. [DOI] [PubMed] [Google Scholar]
- 13.Rosa M, Usai P, Miano R, Kim FJ, Agrò E, Bove P, et al. Recent finding and new technologies in nephrolitiasis: A review of the recent literature. BMC Urology. 2013;13:10–35. doi: 10.1186/1471-2490-13-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rassweiler J, Fritsche HM, Tailly G, Klein J, Laguna P, Chaussy C. Shock wave lithotripsy in the year 2012. In: Knoll T, Perale MS, editors. Clinical management of urolithiasis. Springer; 2012. pp. 51–75. [Google Scholar]
- 15.Knoll T, Fritsche HM, Rassweiler J. Actual medical and economic aspects of extracorporeal shock wave lithotripsy. Akt Urol. 2011;42:363–7. doi: 10.1055/s-0031-1283805. [DOI] [PubMed] [Google Scholar]
- 16.Rassweiler J, Rassweiler MC, Kenngott H, Frede T, Michel MS, Alken P, et al. The past, present and future of minimally invasive therapy in urology: A review and speculative outlook. Minim Invasive Ther Allied Technol. 2013;22:200–9. doi: 10.3109/13645706.2013.816323. [DOI] [PubMed] [Google Scholar]
- 17.Knoll T, Alken P. Beyond ESWL: New concepts for definitive stone removal. World J Urol. 2011;29:703–4. doi: 10.1007/s00345-011-0787-8. [DOI] [PubMed] [Google Scholar]
- 18.Türk C, Knoll T, Petrik A, Sarica K, Skolarikos A, Straub M, et al. Milan: presented at EAU-congress; 2013. Mar, EAU-Guidelines on Urolithiasis 2013. [Google Scholar]
- 19.Rassweiler JJ, Bergsdorf T, Bohris C, Burkhardt M, Burnes L, Forssmann B, et al. Consensus: Shock wave technology and application — state of the art in 2010. In: Chaussy C, Haupt G, Jocham D, Köhrmann KU, editors. Therapeutic energy applications in urology II. Standards and recent developments. New York: Thieme Stutgart; 2010. pp. 37–52. [Google Scholar]
- 20.Partheymüller P. Sonolth i-sys: The new standard in lithotripy. In: Chaussy C, Haupt G, Jocham D, Köhrmann KU, editors. Therapeutic energy applications in urology II. Standards and recent developments. New York: Thieme, Stuttgart; 2010. pp. 65–70. [Google Scholar]
- 21.Handa RK, McAteer JA, Evan AP, Connors BA, Pishchalnikov YA, Gao S. Assessment of renal injury with a clinical dual head lithotripter delivering 240 shock waves per minute. J Urol. 2009;181:884–9. doi: 10.1016/j.juro.2008.10.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sheir KZ, El-Diasty TA, Ismail AM. Evaluation of a synchronous twin-pulse technique for shock wave lithotripsy: The first prospective clinical study. BJU Int. 2005;95:389–3. doi: 10.1111/j.1464-410X.2005.05306.x. [DOI] [PubMed] [Google Scholar]
- 23.Pishchalnikov YA, McAteer R, VonderHaar J, Pishchalnikova IV, Williams JC, Evan AP. Detection of significant variation in acoustic output of an electromagnetic lithotripter. J Urol. 2006;176:2294–8. doi: 10.1016/j.juro.2006.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wess O. Storz Medical — shock wave technology for medical applications. In: Chaussy C, Haupt G, Jocham D, Köhrmann KU, editors. Therapeutic energy applications in urology II. Standards and recent developments. New York: Thieme, Stuttgart; 2010. pp. 78–81. [Google Scholar]
- 25.De Sio M, Autorino R, Quarto G, Mordente S, Giugliano F, Di Giacomo F, et al. A new transportable shock-wave lithotripsy machine for managing urinary stones: A single centre experience with a dual-focus lithotriptor. BJU Int. 2007;100:1137–41. doi: 10.1111/j.1464-410X.2007.07039.x. [DOI] [PubMed] [Google Scholar]
- 26.Zehnder P, Roth B, Birkhäuser F, Schneider S, Schnutz R, Thalmann GN, et al. A prospective randomized trial comparing the modified HM3 with the Modulith SLX-F2 lithotripter. Eur Urol. 2011;59:637–44. doi: 10.1016/j.eururo.2011.01.026. [DOI] [PubMed] [Google Scholar]
- 27.Rassweiler J, Henkel TO, Joyce AD, Köhrmann KU, Manning M, Alken P. Extracorporeal shock wave lithotripsy of ureteric stones with the Modulith SL20. Br J Urol. 1992;70:594–9. doi: 10.1111/j.1464-410x.1992.tb15826.x. [DOI] [PubMed] [Google Scholar]
- 28.Tiselius HG. How efficient is extracorporeal shockwave lithotripsy with modern lithotripters for removal of ureteral stones. J Endourol. 2008;22:249–55. doi: 10.1089/end.2007.0225. [DOI] [PubMed] [Google Scholar]
- 29.Ginter S, Burkhardt M, Vallon P. Richard Wolf: The piezoelectric ESWL — more than 20 years of clinical success worldwide. In: Chaussy C, Haupt G, Jocham D, Köhrmann KU, editors. Therapeutic energy applications in urology II. Standards and recent developments. New York: Thieme, Stuttgart; 2010. pp. 87–92. [Google Scholar]
- 30.Neisius DA. Clinical experience with the latest generation piezoelectric extracorporeal shockwave lithotripsy system. Eur Kidney Urol Dis. 2006:81–3. [Google Scholar]
- 31.Wang R, Faerber GJ, Roberts WW, Morris DS, Wolf JS., Jr Single-center North American experience with Wolf Piezolith 3000 in management of urinary calculi. Urology. 2009;73:958–63. doi: 10.1016/j.urology.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 32.Ng CF, Mc Loman L, Thompson TJ, Tolley DA. Comparison of 2 generations of piezoelectric lithtriptors using matched pair analysis. J Urol. 2004;172:1887–91. doi: 10.1097/01.ju.0000142730.60583.7a. [DOI] [PubMed] [Google Scholar]
- 33.Goktas C, Akca O, Horuz R, Gokhan O, Albayrak S, Sarica K. SWL in lower calyceal calculi: Evaluation of the treatment results in children and adults. Urology. 2011;78:1402–6. doi: 10.1016/j.urology.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 34.Eisenmenger W, Du XX, Tang C, Zhao S, Wang Y, Rong F, et al. The first clinical results of “wide focus and low-pressure” ESWL. Ultrasound Med Biol. 2002;28:769–74. doi: 10.1016/s0301-5629(02)00507-0. [DOI] [PubMed] [Google Scholar]
- 35.Evan AP, McAteer JA, Connors BA, Pishchalnikov YA, Handa RK, Blomgren P, et al. Independent assessment of a wide-focus, low-pressure electromagnetic lithotripter: Absence of renal bioeffects in the pig. BJU Int. 2007;101:382–8. doi: 10.1111/j.1464-410X.2007.07231.x. [DOI] [PubMed] [Google Scholar]
- 36.Lanski M, Ulucan N, Burnes L. Lithoskop: Discover the future of urology today. In: Chaussy C, Haupt G, Jocham D, Köhrmann KU, editors. Therapeutic energy applications in urology II. Standards and recent developments. New York: Thieme, Stuttgart; 2010. pp. 71–7. [Google Scholar]
- 37.Hofsäß S, Rheinwald M. Dornier MedTech: Update on products for urology. In: Chaussy C, Haupt G, Jocham D, Köhrmann KU, editors. Therapeutic energy applications in urology II. Standards and recent developments. New York: Thieme, Stuttgart; 2010. pp. 57–69. [Google Scholar]
- 38.Arrabal-Polo MB, Arrabal-Martin M, Palao-Yago F, Milan-Ortiz JL, Zuluaga-Gomez A. Value of focal applied energy quotient in treatment of ureteral lithiasis with shock waves. Urol Res. 2011;40:377–81. doi: 10.1007/s00240-011-0430-6. [DOI] [PubMed] [Google Scholar]
- 39.Bohris C, Roosen A, Dickmann M, Hocaoglu Y, Sandner S, Bader M, et al. Monitoring the coupling of the lithotripter head with skin during routine shock wave lithotripsy with a surveillance camera. J Urol. 2011;187:157–63. doi: 10.1016/j.juro.2011.09.039. [DOI] [PubMed] [Google Scholar]
- 40.Duryea AP, Roberts WW, Cain CA, Hall TL. Controlled cavitation to augment SWL stone comminution: Mechanistic insights in vitro. IEEE Trans Ultrason Ferroelectr Freq Control. 2013;60:301–9. doi: 10.1109/TUFFC.2013.2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shah A. Novel ultrasound method to reposition kidney stones. Urol Res. 2010;38:491–5. doi: 10.1007/s00240-010-0319-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rassweiler MC, Ritter M, Michel MS, Häcker A. Influence of endourological devices on 3D reconstruction image quality using the Uro Dyna-CT. World J Urol. 2013;31:1703–7. doi: 10.1007/s00345-012-0917-y. [DOI] [PubMed] [Google Scholar]
- 43.Desai M, Jain P, Ganpule A, Sabnis R, Patel S, Shrivastav P. Developments in technique and technology: The effect on the results of percutaneous nephrolithotomy for staghorn calculi. BJU Int. 2009;104:542–8. doi: 10.1111/j.1464-410X.2009.08472.x. [DOI] [PubMed] [Google Scholar]
- 44.Müller M, Rassweiler MC, Klein J, Seitel A, Gondan M, Baumhauer M, et al. Mobile augmented reality for computer-assisted percutaneous nephrolithotomy. Int J Comput Assist Radiol Surg. 2013;8:663–75. doi: 10.1007/s11548-013-0828-4. [DOI] [PubMed] [Google Scholar]
- 45.Rassweiler JJ, Müller M, Fangerau M, Klein J, Goezen AS, Pereira P, et al. iPad-assisted percutaneous access to the kidney using marker-based navigation: Initial clinical experience. Eur Urol. 2012;61:628–31. doi: 10.1016/j.eururo.2011.12.024. [DOI] [PubMed] [Google Scholar]
- 46.Ritter M, Rassweiler MC, Häcker A, Michel MS. Laser-guided percutaneous kidney access with the Uro Dyna-CT: First experience of three-dimensional puncture planning with an ex vivo model. World J Urol. 2013;31:1147–51. doi: 10.1007/s00345-012-0847-8. [DOI] [PubMed] [Google Scholar]
- 47.Sas DJ. Increasing incidence of kidney stones in children evaluated in the emergency department. J Pediatr. 2010;157:132–7. doi: 10.1016/j.jpeds.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 48.Galvin DJ, Pearle MS. The contemporary management of renal and ureteric calculi. BJU Int. 2006;98:1283–8. doi: 10.1111/j.1464-410X.2006.06514.x. [DOI] [PubMed] [Google Scholar]


