Abstract
Accurate reporting of complications is an essential component to critical appraisal and innovation in surgery and specifically with percutaneous nephrolithotomy (PCNL). We review the evolution of complication reporting for PCNL and suggest future directions for innovation. A selective review was carried out using Pubmed. Key search terms and their combinations included percutaneous, anatrophic, nephrolithotomy, PCNL, complications, Clavien, Martin score, bleeding, bowel injury, perforation, fever, sepsis. The references from relevant papers and reviews as well as AUA and EAU guidelines were also scanned for inclusion. PCNL has become the procedure of choice for large renal stones owing to decreased morbidity over alternative procedures. Both common and rare complications have been described in large case series, small randomized controlled trials, and case reports in an unstandardized form. Although these reports have provided an informative starting point, a standardized complication reporting methodology is necessary to enable appropriate comparisons between institutions, time periods, or innovations in technique. The Clavien-Dindo grading system has become widely accepted in urology and has facilitated the study of PCNL complications. Future research should focus on adaptions of this system to render it more comprehensive and applicable to PCNL.
Keywords: Clavien, complications, outcomes, percutaneous nephrolithotomy
INTRODUCTION
Reporting of complications in urology is an essential component of good patient care and should be a routine part of surgical practice. Commonly, urological services hold weekly or monthly morbidity and mortality rounds in which complications are discussed. Short-term complications are commonly reported with observational studies and randomized controlled trials (RCT). Often the incidence of peri-operative complications is used as a surrogate marker of quality and to evaluate the appropriateness of new therapies or surgical procedures. However, the key problem with using the literature in this way is that there exists considerable heterogeneity of reporting practices among surgeons.
To address this problem within urology, an Ad Hoc EAU guidelines panel evaluated the literature and produced general recommendations for the reporting of complications within urology.[1] The authors stress the urgent need for uniform reporting of complications after urologic procedures, in an effort to establish efficacy of surgical technique and improve patient care.[2,3] They also note an evolution toward improvement in the frequency and quality of reporting, however do not specifically address the trend for PCNL complications. Specialty and treatment-specific grading systems have been developed in some fields and have the advantage of more completely addressing procedure-specific complication scenarios and to better assess the value and risk of particular interventions.[4,5] To date there is no universally accepted classification system within urology or for PCNL. This article will discuss the evolution and standardization of reporting complications for PCNL and highlight some current limitations and potential remedies.
Unstandardized reporting of complications
Percutaneous nephrolithotomy (PCNL) has revolutionized the treatment of large renal calculi as it is an extremely efficacious and minimally invasive alternative to open procedures.[6,7,8] Historically an alternative procedure, anatrophic nephrolithotomy, was associated with an 85 % stone free rate,[9] which is comparable to PCNL.[10,11] but also had longer procedure times, hospital stay, convalescence and greater blood loss.[12,13] As such, anatrophic nephrolithotomy is currently performed in less than 1% of patients undergoing stone surgery.[8,14,15] and is restricted to special cases with very large stone burden in patients who are inappropriate for a percutaneous approach.[11] In contrast PCNL has become an internationally accepted procedure and is performed in many centers across in Europe, Asia, North America, South America, Australia, and Africa.[16]
Initial complications reported for PCNL were derived through descriptive analysis of surgical series and case reports. The major types of complications identified include hemorrhage, renal pelvic injury, fluid absorption, infection, and associated organ injury. A recent review by the Cochrane collaboration addressed complications as a secondary endpoint. This review identified only two low quality RCTs that specifically reported urinary tract infection, ileus, sepsis, hematoma, obstruction, perforation, transfusion, and arteriovenous fistula. Unfortunately, the sample size and quality of these RCTs do not allow for reliable extrapolation of incidence rates.[17] Bleeding requiring transfusion has been reported from 6% to 23% across series.[11,18,19,20,21] Bleeding requiring embolization has been reported in 0.8% of 2200 patients in one large series[22] and second large series reported rates of bleeding requiring embolization or blood transfusion of 0.8% from 1585 procedures.[23] The recent CROES series, which included 5803 consecutive PCNLs, reported a rate of significant bleeding of 7.8% with a transfusion rate of 5.7%.[16] An additional series reported an increase in transfusion rate from 20% to 42% when greater than two punctures are required.[24] Unfortunately, many reports do not distinguish between immediate post-op and delayed hemorrhage and definitions for significant bleeding are not uniform. One large series reports rates of delayed hemorrhage of 1.2%[25] and seemed to vary between 0.8% and 3.2% based on indication for percutaneous procedure (stone, urothelial carcinoma, or stricture). However, multivariate analysis was not performed on this un-randomized sample therefore it is not possible to identify independent predictors of severe bleeding in this case. One can see from the heterogeneity of these results that it is difficult to precisely define complication rates in the absence of standardized reporting and data collection procedures. Based on these data and expert opinion, contributing factors to bleeding are thought to include medial punctures, multiple punctures, abnormal anatomy, anticoagulant and antiplatelet therapy, supra-costal access, increasing tract size, prolonged operative time, and renal pelvic perforation.
Renal pelvic injury has been estimated to occur in 7% of cases based on a large series and review of literature.[26] However, the severity of pelvic injury reported in this series is not clear, nor the therapy required to treat such injuries. Most pelvic injuries are identified intra-operatively by direct vision or by a sudden collapse of a previously distended collecting system. Post-operatively, renal pelvic injuries can manifest with abdominal distension, ileus, or fever. Massive fluid absorption has been shown to occur[27,28] therefore the use of saline irrigant is recommended to avoid dilutional hyponatremia. However, the true incidence and long-term consequence of extravasation are unclear.
Post-operative fever is considered a frequent occurrence with reported rates between 15% and 30%.[29,30] In contrast, septicemia is thought to be relatively rare and has been reported to occur with 0.9-4.7% of PCNL procedures.[31,32,33] Unfortunately, the definitions for fever and sepsis are not standardized in the literature, nor are the methods of data collection; as such reported rates of fever vary greatly. The majority of these patients can be adequately treated with intravenous antibiotic and close observation; however, some patients may require more extensive resuscitation in an intensive care setting. Once again a difficulty in interpreting the true magnitude of occurrence stems from lack of uniform definition for fever or sepsis/systemic inflammatory response syndrome, as well as the mechanism of detecting and reporting these complications.
Adjacent organ injuries represent another group of rare complications. Injuries to the lung, liver, spleen, biliary system, colon, or small bowel have been reported. The most common of these complications are pulmonary and colonic. In one review pulmonary complications have been reported to occur in 2.3-3.1% of PCNL;[31] however, these authors did not stratify by level of puncture. Punctures below the 12th rib are associated with hydro/pneumothorax in <0.5% of cases, compared to 3-15% above the 12th rib, and 10-100% above the 11th rib.[34,35,36,37] Unfortunately, the reported incidence of hydro/pneumothorax represents a range of severity for which differing management options may be appropriate. Treatment of hydro/pneumothorax can range from observation for smaller asymptomatic injuries to inserting a pleural drain. Precise indications for intervention and optimal management approach cannot be directly compared from these data. Colon injury is a rare complication of PCNL and is thought to occur in 0.2-0.8% of procedures.[18,26,31] Based on review of case series the risk factors associated with colon injury are low body weight, female gender, and lateral puncture. If the injury is extraperitoneal then separate drainage of colon and urinary system might be sufficient management, whereas intraperitoneal injury typically requires open repair. Small bowel injury to the duodenum or jejunum is an order of magnitude more rare and has been described in several case reports.[38,39] Likewise, injury to the spleen and liver are reportable rare but are more likely to occur in the presence of organomegaly or with high punctures above the 11th or 10th rib.[37,39,40] Treatment of these rare complications is not standardized and may involve conservative management or open surgery.[39,41,42]
Some important information has been gained from reporting PCNL complications in an unstandardized fashion. Primarily, we have gained an understanding of the types of complications that can occur and a reasonable estimate of frequency of the occurrence for common complications. For this reason, we suggest that the contemporary use of unstandardized reporting may still be beneficial in the context of providing a detailed description of very rare complications. The major limitation of reporting complications in an unstandardized fashion is the inability to accurately compare between reported series or generalize results. Without standardized definitions of complications and their consequence it becomes difficult to compare different techniques, management options, estimate relative risk, or justify a rational for sequencing multimodality approaches. This problem is widely recognized and is the driving force for the development and acceptance of standardized systems for reporting surgical complications.
Standardized reporting of complications
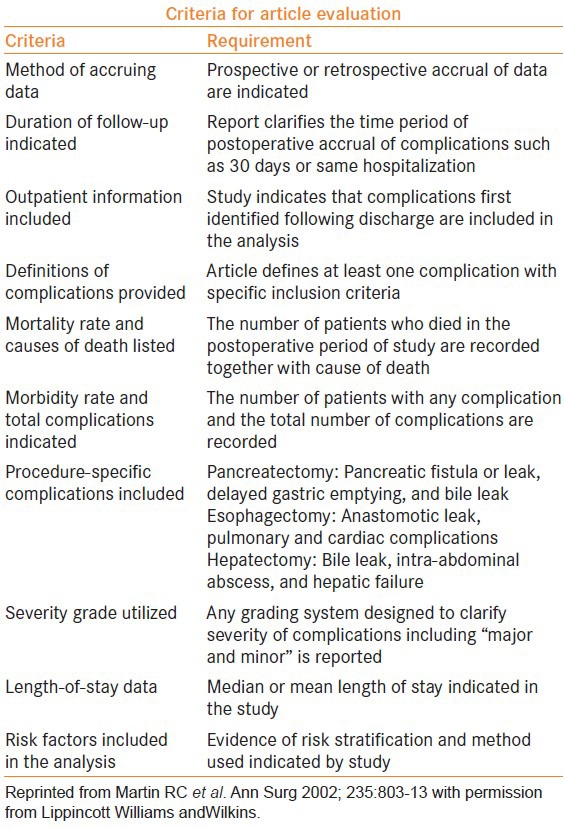
Given the wide acceptance of PCNL among urologists, it is especially important to standardize reporting of complications for this procedure. There have been several classification systems for reporting surgical complications in the past 20 years.[1] In a paper which emphasized a call to reform the practice of reporting surgical complications, Martin et al. evaluated 119 articles reporting outcomes in 22,530 patients and identified 10 criteria for reporting of surgical complications [Table 1].[43] The authors found a high rate of inconsistency in reporting complications and no systematic principle of accrual, display, and analysis of complication data within the surgical literature. A systematic approach to quantifying and categorizing complications allows for an accurate assessment of complication rates, objective performance assessment, comparison across institutions or over time within an institution, and assessment of novel techniques and management options.
Table 1.
Martin evaluation criteria for reporting surgical complications
One of the most widely accepted classification systems within surgery and urology was proposed by Clavien et al.[44] The Clavien system was initially validated using a series of 650 patients who underwent elective cholecystectomy and stratified complications into four grades based on the severity of the intervention required to treat the complication and the presence of lasting disability. This system was further modified by Clavien and Dindo using a cohort of 6336 patients and validated through a multinational survey.[45] The modification refined the grading of life-threatening complication and disability, and was shown to be reliable and acceptable to respondents [Table 2]. The accuracy and reliability of this classification system was further assessed and was found to be increasing in popularity from 2004 to 2009 across surgical subspecialties in which 14% of articles using the Clavien-Dindo classification were from urology.[46]
Table 2.
Clavien-dindo classification of surgical complications
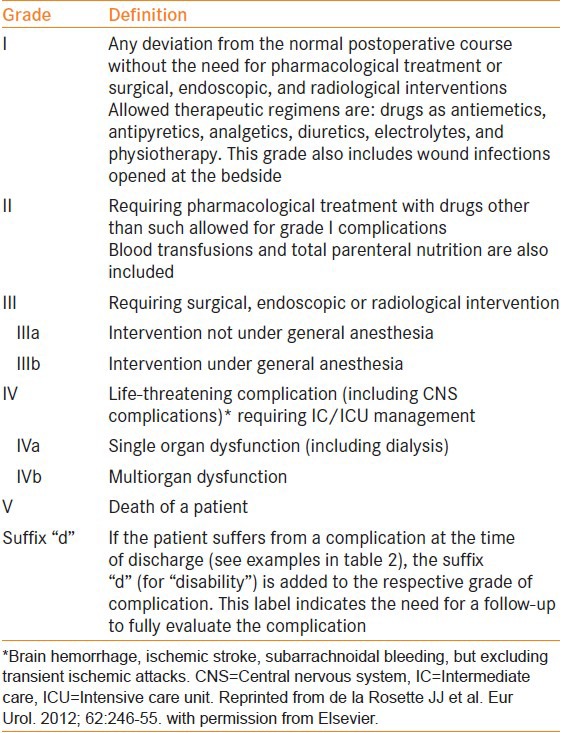
To date, the Clavien-Dindo classification system is the most accepted approach for classifying surgical complications within urology and is becoming a standard in reporting complications from PCNL. The CROES PCNL study group has adopted Clavien-Dindo classification system for a large prospective cohort study of 5803 patients from 96 participating centers in 26 countries.[16] The authors found that 20.5% of patients experienced one or more complications, the majority of which were Clavien-Dindo grade I (54%) with very few life-threatening complications (0.5%) and two deaths (0.03%). This concurs with data synthesized in a recent review by Seitz et al. which reported similar rates of complications by Clavien-Dindo grade.[47] The large CROES PCNL dataset was further used to identify ASA score and prolonged OR times as strong independent predictors of increasing Clavien-Dindo grade.[48] This information can potentially be used to risk-stratify and counsel patients pre-operatively.
The use of the Clavien-Dindo system has allowed for more accurate reporting of complications and a standardized quality measure for evaluating new interventions or innovations in technique. Zeng et al. reviewed their 20 year experience (n= 12,482) with the Chinese minimally invasive PCNL and found comparable rates of complications to previously reported large series.[49] Similarly, Tepeler et al. have compared the bull's eye and triangulation techniques for gaining percutaneous access,[50] and Honey et al. have evaluated the prone-flexed position[51] and found similar rates of complications. In contrast, bileteral PCNL was shown to have greater complication rates as compared to unilateral PCNL.[52] Likewise, Fuller et al. have demonstrated higher rates of Clavien III-IV complications in super obese patients[53] and de la Rosette et al. were able to demonstrate decreasing rates of complications over time.[54] The authors attribute this decrease in complication rate to increasing familiarity with the procedure and the creation of a dedicated stone center. In the pediatric literature, Ozden et al have shown that stone burden and OR time are independent predictors of Clavien complication.[55] Similarly, in the adult literature, Mandal et al. from India successfully correlated stone complexity, using Guy's stone score (GSS), to Clavien-Dindo complication rate.[56] This built on earlier work by Thomas et al. that demonstrated the GSS could predict stone free rate but they failed to demonstrate the GSS could predict Clavien grade due to small sample size.[57] Globally, these studies illustrate the strength of adopting a uniform complication reporting system, which allows investigators to build on each other's work through being able to make uniform comparisons of complications across techniques, institutions, time-periods.
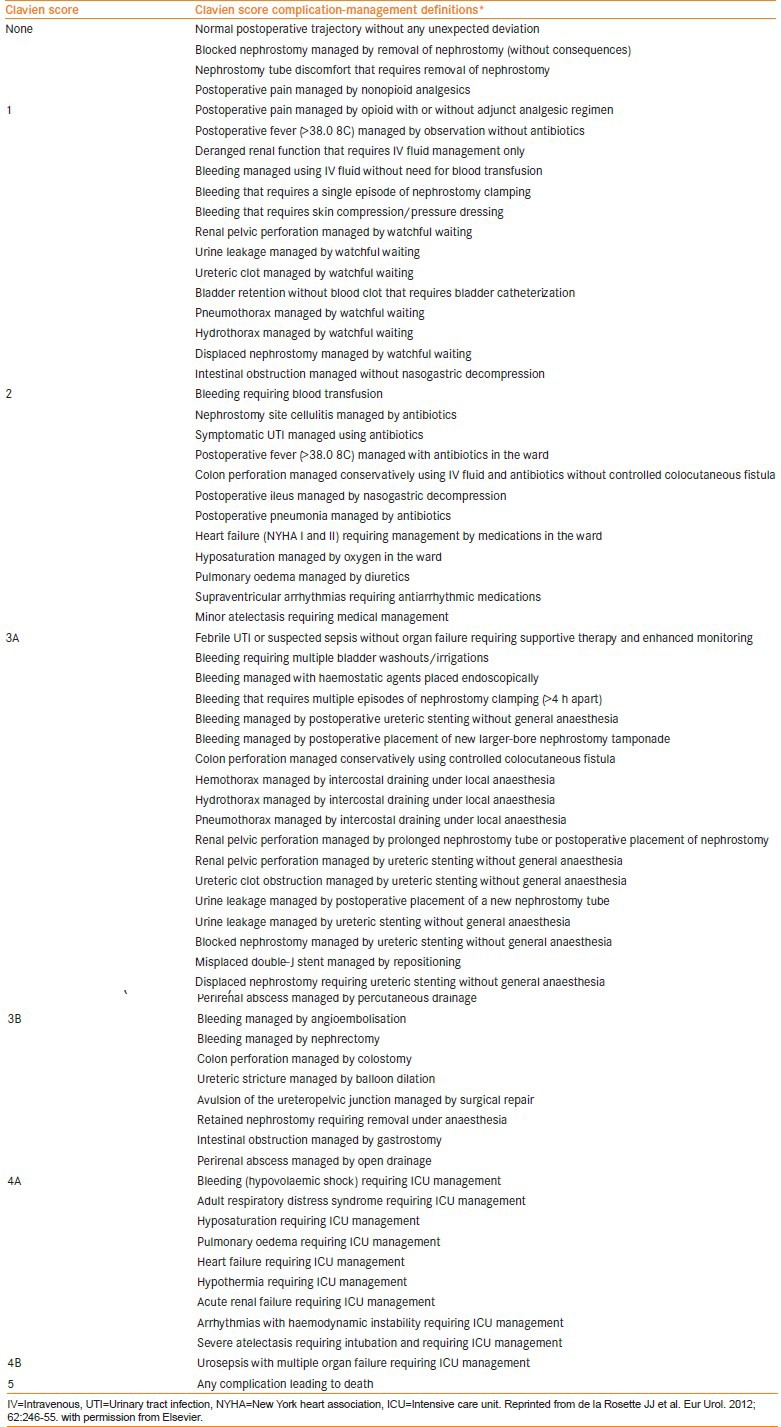
The Clavien-Dindo classification system has been formally validated for PCNL.[58] The investigators used a series of 528 patients with complications to generate a set of 70 complication-management scenarios. These scenarios were distributed to a cohort of urologists from 26 countries who were asked to assign a Clavien-Dindo grade. The survey demonstrated only moderate overall agreement between urologists (κ = 0.457; P = <0.0001). Urologists demonstrated good to very good agreement with Clavien III, IV, and V complications (κ = 0.769, κ =0.810, and κ = 0.986, respectively) and only fair agreement for Clavien 0 and I (κ = 0.297, κ = 0.358, respectively). This finding points to interrater reliability as one potential limitation of the Clavien-Dindo classification system. To improve the reliability and consistency of this system, a detailed categorization scheme for PCNL complication has been proposed [Table 3]. Although there is a clear need for standardization of complication reporting, and the Clavien-Dindo system offers one useful solution there remains work to do to improve the reliability and acceptance of this system within urology.
Table 3.
Categorization of PCNL complications according to clavien-dindo grade
Limitations and future directions
Although the Clavien-Dindo classification system is a very powerful tool there remain several limitations. The primary limitation is a result of lack of systematic data evaluation and collection procedures. Dindo et al. conducted a quality assessment study to evaluate validity of recorded data in a prospective quality database maintained by residents and junior staff.[59] The authors found that up to 80% of negative post-op events were not recorded and co-morbidities were incorrectly captured in up to 20% of cases. Surprisingly these rates did not significantly change with additional active and focused training in data recording procedures. A survey conducted in parallel with their quality assessment revealed that residents and junior staff were responsible for recording surgical outcome data in 80% of participating European centers. The authors conclude that standardized evaluation procedures should be conducted by dedicated personnel to improve accuracy of reporting. Additionally, the Clavien-Dindo classification system does not account for long-term complications which can have significant implications for patient care. This is a more complicated obstacle because obtaining long-term data of sufficient quality is difficult, and thus limits the ability to generate a standardized approach.
Further, most studies that use the Clavien-Dindo system report pooled complications or simply the most severe complication experienced as a result of a procedure. The assignment of severity to a given complication is from the physician's perspective and may not accurately represent the burden of morbidity experienced by the patient. In an attempt to account for this, Slankamenac et al. have devised the Comprehensive Complication Index (CCI) based on the Clavien-Dindo classification.[60] The CCI is a standardized approach which incorporates weighted median reference values for each Clavien grade of complication experienced from both physician and patient perspectives and is expressed as a number from 0 to 100. This tool, which has been validated by four separate approaches, appears to be more sensitive and comprehensive than existing morbidity measures and may represent a standardized outcome measure for future studies in surgery and urology.
Specifically with regard to PCNL, the Clavien approach does not account for the routine use of auxiliary treatments such as second look PCNL, ureteroscopy, or extracorporeal shock wave lithotripsy.[47,61] In fact it may be a measure of good judgment to abort a procedure and plan for a second attempt in the setting of poor visibility due to bleeding or the presence of pus intra-operatively. Under the current grading scheme [Table 2], these planned repeat procedures may be mistakenly interpreted as grade III complications. To overcome these limitations, procedure-specific modifications to the Clavien-Dindo system could be devised and validated in prospective series [Table 3]. Potentially, these modifications can then be incorporated into a more comprehensive system such as the CCI. Other procedure-specific classifications systems, such as PULS for ureteral injury during ureteroscopy, have been developed and can assist intra-operative decisions making once a complication is noted to have occurred.[62] Similar such systems should be developed to optimize the management of complications from PCNL in the future.
CONCLUSION
Historically, complication data was primarily derived from case series and small trials. Variations in procedures and definitions greatly limited generalizability of this data. Recently, there have been efforts to standardize the reporting of complications for PCNL. This has allowed a better understanding of risks associated with PCNL and a means to compare complications on a more objective standard. However, there remain several limitations to current reporting systems and procedures future research may focus on adapting procedure-specific modifications to the Clavien system and validating the use of CCI within urology.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mitropoulos D, Artibani W, Graefen M, Remzi M, Roupret M, Truss M. Reporting and grading of complications after urologic surgical procedures: An ad hoc EAU Guidelines panel assessment and recommendations. Eur Urol. 2012;61:341–9. doi: 10.1016/j.eururo.2011.10.033. [DOI] [PubMed] [Google Scholar]
- 2.Donat SM. Standards for surgical complication reporting in urologic oncology: Time for a change. Urology. 2007;69:221–5. doi: 10.1016/j.urology.2006.09.056. [DOI] [PubMed] [Google Scholar]
- 3.Fink A, Campbell DA, Mentzer RM, Henderson WG, Daley J, Bannister J, et al. The national surgical quality improvement program in non-veterans administration hospitals initial demonstration of feasibility. Ann Surg. 2002;236:344–54. doi: 10.1097/00000658-200209000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haylen BT, Freeman RM, Swift SE, Cosson M, Davila WG, Deprest J. An International Urogynecological Association (IUGA)/ International Continence Society (ICS) Joint Terminology and Classification of the Complications Related Directly to the Insertion of Prostheses (Meshes, Implants, Tapes) and Grafts in Female Pelvic Floor Surgery. Neurourol Urodyn. 2011;30:2–12. doi: 10.1002/nau.21036. [DOI] [PubMed] [Google Scholar]
- 5.Trotti A, Colevas AD, Setser A, Rusch V, Jacques D, Budach V. CTCAE v3.0: Development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol. 2003;13:176–81. doi: 10.1016/S1053-4296(03)00031-6. [DOI] [PubMed] [Google Scholar]
- 6.Lingeman JE, Coury TA, Newman DM, Kahnoski RJ, Mertz JH, Mosbaugh PG, et al. Comparison of results and morbidity of percutaneous nephrostolithotomy and extracorporeal shock wave lithotripsy. J Urol. 1987;138:485–90. doi: 10.1016/s0022-5347(17)43236-8. [DOI] [PubMed] [Google Scholar]
- 7.Snyder JA, Smith AD. Staghorn calculi: Percutaneous extraction versus anatrophic nephrolithotomy. J Urol. 1986;136:351–4. doi: 10.1016/s0022-5347(17)44864-6. [DOI] [PubMed] [Google Scholar]
- 8.Assimos DG, Wrenn JJ, Harrison LH, McCullough DL, Boyce WH, Taylor CL. A comparison of anatrophic nephrolithotomy and percutaneous nephrolithotomy with and without extracorporeal shock wave lithotripsy for management of patients with staghorn calculi. J Urol. 1991;145:710–4. doi: 10.1016/s0022-5347(17)38431-8. [DOI] [PubMed] [Google Scholar]
- 9.Griffith DP, Gibson JR, Clinton CW, Musher DM. Acetohydroxamic acid: Clinical studies of a urease inhibitor in patients with staghorn renal calculi. J Urol. 1978;119:9–15. doi: 10.1016/s0022-5347(17)57366-8. [DOI] [PubMed] [Google Scholar]
- 10.Segura JW, Preminger GM, Assimos DG, Dretler SP, Kahn RI, Lingeman JE, et al. Nephrolithiasis Clinical Guidelines Panel summary report on the management of staghorn calculi. The American Urological Association Nephrolithiasis Clinical Guidelines Panel. J Urol. 1994;151:1648–51. doi: 10.1016/s0022-5347(17)35330-2. [DOI] [PubMed] [Google Scholar]
- 11.Preminger GM, Assimos DG, Lingeman JE, Nakada SY, Pearle MS, Wolf JS., Jr AUA Nephrolithiasis Guideline Panel Chapter 1: AUA guideline on management of staghorn calculi: Diagnosis and treatment recommendations. J Urol. 2005;173:1991–2000. doi: 10.1097/01.ju.0000161171.67806.2a. [DOI] [PubMed] [Google Scholar]
- 12.Kahnoski RJ, Lingeman JE, Coury TA, Steele RE, Mosbaugh PG. Combined percutaneous and extracorporeal shock wave lithotripsy for staghorn calculi: An alternative to anatrophic nephrolithotomy. J Urol. 1986;135:679–81. doi: 10.1016/s0022-5347(17)45817-4. [DOI] [PubMed] [Google Scholar]
- 13.Al-Kohlany KM, Shokeir AA, Mosbah A, Mohsen T, Shoma AM, Eraky I, et al. Treatment of complete staghorn stones: A prospective randomized comparison of open surgery versus percutaneous nephrolithotomy. J Urol. 2005;173:469–73. doi: 10.1097/01.ju.0000150519.49495.88. [DOI] [PubMed] [Google Scholar]
- 14.Assimos D. Anatrophic nephrolithotomy. Urology. 2001;57:161–5. doi: 10.1016/s0090-4295(00)00920-1. [DOI] [PubMed] [Google Scholar]
- 15.Segura JW. Surgical management of urinary calculi. Semin Nephrol. 1990;10:53–63. [PubMed] [Google Scholar]
- 16.de la Rosette J, Assimos D, Desai M, Gutierrez J, Lingeman J, Scarpa R, et al. CROES PCNL Study Group The Clinical Research Office of the Endourological Society Percutaneous Nephrolithotomy Global Study: Indications, complications, and outcomes in 5803 patients. J Endourol. 2011;25:11–7. doi: 10.1089/end.2010.0424. [DOI] [PubMed] [Google Scholar]
- 17.Srisubat A, Potisat S, Lojanapiwat B, Setthawong V, Laopaiboon M. Extracorporeal shock wave lithotripsy (ESWL) versus percutaneous nephrolithotomy (PCNL) or retrograde intrarenal surgery (RIRS) for kidney stones. Cochrane Database Syst Rev. 2009;4:CD007044. doi: 10.1002/14651858.CD007044.pub2. [DOI] [PubMed] [Google Scholar]
- 18.Segura JW, Patterson DE, LeRoy AJ, Williams HJ, Jr, Barrett DM, Benson RC, Jr, et al. Percutaneous removal of kidney stones: Review of 1,000 cases. J Urol. 1985;134:1077–81. doi: 10.1016/s0022-5347(17)47633-6. [DOI] [PubMed] [Google Scholar]
- 19.Stoller ML, Wolf JS, Jr, St Lezin MA. Estimated blood loss and transfusion rates associated with percutaneous nephrolithotomy. J Urol. 1994;152:1977–81. doi: 10.1016/s0022-5347(17)32283-8. [DOI] [PubMed] [Google Scholar]
- 20.Kukreja R, Desai M, Patel S, Bapat S, Desai M. Factors affecting blood loss during percutaneous nephrolithotomy: Prospective study. J Endourol. 2004;18:715–22. doi: 10.1089/end.2004.18.715. [DOI] [PubMed] [Google Scholar]
- 21.Netto NR, Jr, Ikonomidis J, Ikari O, Claro JA. Comparative study of percutaneous access for staghorn calculi. Urology. 2005;65:659–62. doi: 10.1016/j.urology.2004.10.081. [DOI] [PubMed] [Google Scholar]
- 22.Kessaris DN, Bellman GC, Pardalidis NP, Smith AG. Management of hemorrhage after percutaneous renal surgery. J Urol. 1995;153:604–8. doi: 10.1097/00005392-199503000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Duvdevani M, Razvi H, Sofer M, Beiko DT, Nott L, Chew BH, et al. Third prize: Contemporary percutaneous nephrolithotripsy: 1585 procedures in 1338 consecutive patients. J Endourol. 2007;21:824–9. doi: 10.1089/end.2007.9936. [DOI] [PubMed] [Google Scholar]
- 24.Martin X, Murat FJ, Feitosa LC, Rouvière O, Lyonnet D, Gelet A, et al. Severe bleeding after nephrolithotomy: Results of hyperselective embolization. Eur Urol. 2000;37:136–9. doi: 10.1159/000020129. [DOI] [PubMed] [Google Scholar]
- 25.Richstone L, Reggio E, Ost MC, Seideman C, Fossett LK, Okeke Z, et al. First Prize (tie): Hemorrhage following percutaneous renal surgery: Characterization of angiographic findings. J Endourol. 2008;22:1129–35. doi: 10.1089/end.2008.0061. [DOI] [PubMed] [Google Scholar]
- 26.Michel MS, Trojan L, Rassweiler JJ. Complications in percutaneous nephrolithotomy. Eur Urol. 2007;51:899–906. doi: 10.1016/j.eururo.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 27.Pugach JL, Moore RG, Parra RO, Steinhardt GF. Massive hydrothorax and hydro-abdomen complicating percutaneous nephrolithotomy. J Urol. 1999;162:2110. doi: 10.1016/S0022-5347(05)68134-7. [DOI] [PubMed] [Google Scholar]
- 28.Ghai B, Dureja GP, Arvind P. Massive intraabdominal extravasation of fluid: A life threatening complication following percutaneous nephrolithotomy. Int Urol Nephrol. 2003;35:315–8. doi: 10.1023/b:urol.0000022937.22909.65. [DOI] [PubMed] [Google Scholar]
- 29.Charton M, Vallancien G, Veillon B, Brisset JM. Urinary tract infection in percutaneous surgery for renal calculi. J Urol. 1986;135:15–7. doi: 10.1016/s0022-5347(17)45500-5. [DOI] [PubMed] [Google Scholar]
- 30.Troxel SA, Low RK. Renal intrapelvic pressure during percutaneous nephrolithotomy and its correlation with the development of postoperative fever. J Urol. 2002;168:1348–51. doi: 10.1016/S0022-5347(05)64446-1. [DOI] [PubMed] [Google Scholar]
- 31.Skolarikos A, de la Rosette J. Prevention and treatment of complications following percutaneous nephrolithotomy. Curr Opin Urol. 2008;18:229–34. doi: 10.1097/MOU.0b013e3282f46afc. [DOI] [PubMed] [Google Scholar]
- 32.Dogan HS, Guliyev F, Cetinkaya YS, Sofikerim M, Ozden E, Sahin A. Importance of microbiological evaluation in management of infectious complications following percutaneous nephrolithotomy. Int Urol Nephrol. 2007;39:737–42. doi: 10.1007/s11255-006-9147-9. [DOI] [PubMed] [Google Scholar]
- 33.Gonen M, Turan H, Ozturk B, Ozkardes H. Factors affecting fever following percutaneous nephrolithotomy: A prospective clinical study. J Endourol. 2008;22:2135–8. doi: 10.1089/end.2008.0139. [DOI] [PubMed] [Google Scholar]
- 34.Picus D, Weyman PJ, Clayman RV, McClennan BL. Intercostal-space nephrostomy for percutaneous stone removal. AJR Am J Roentgenol. 1986;147:393–7. doi: 10.2214/ajr.147.2.393. [DOI] [PubMed] [Google Scholar]
- 35.Munver R, Delvecchio FC, Newman GE, Preminger GM. Critical analysis of supracostal access for percutaneous renal surgery. J Urol. 2001;166:1242–6. [PubMed] [Google Scholar]
- 36.Lojanapiwat B, Prasopsuk S. Upper-pole access for percutaneous nephrolithotomy: Comparison of supracostal and infracostal approaches. J Endourol. 2006;20:491–4. doi: 10.1089/end.2006.20.491. [DOI] [PubMed] [Google Scholar]
- 37.Hopper KD, Yakes WF. The posterior intercostal approach for percutaneous renal procedures: Risk of puncturing the lung, spleen, and liver as determined by CT. AJR Am J Roentgenol. 1990;154:115–7. doi: 10.2214/ajr.154.1.2104692. [DOI] [PubMed] [Google Scholar]
- 38.Culkin DJ, Wheeler JS, Jr, Canning JR. Nephro-duodenal fistula: A complication of percutaneous nephrolithotomy. J Urol. 1985;134:528–30. doi: 10.1016/s0022-5347(17)47276-4. [DOI] [PubMed] [Google Scholar]
- 39.Santiago L, Bellman GC, Murphy J, Tan L. Small bowel and splenic injury during percutaneous renal surgery. J Urol. 1998;159:2071–2. doi: 10.1016/S0022-5347(01)63251-8. [DOI] [PubMed] [Google Scholar]
- 40.Semins MJ, Bartik L, Chew BH, Hyams ES, Humphreys M, Miller NL, et al. Multicenter analysis of postoperative CT findings after percutaneous nephrolithotomy: Defining complication rates. Urology. 2011;78:291–4. doi: 10.1016/j.urology.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 41.Kondás J, Szentgyörgyi E, Váczi L, Kiss A. Splenic injury: A rare complication of percutaneous nephrolithotomy. Int Urol Nephrol. 1994;26:399–404. doi: 10.1007/BF02768008. [DOI] [PubMed] [Google Scholar]
- 42.El-Nahas AR, Mansour AM, Ellaithy R, Abol-Enein H. Case report: Conservative treatment of liver injury during percutaneous nephrolithotomy. J Endourol. 2008;22:1649–52. doi: 10.1089/end.2008.0147. [DOI] [PubMed] [Google Scholar]
- 43.Martin RC, 2nd, Brennan MF, Jaques DP. Quality of complication reporting in the surgical literature. Ann Surg. 2002;235:803–13. doi: 10.1097/00000658-200206000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111:518–26. [PubMed] [Google Scholar]
- 45.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo Classification of surgical complications Five year experience. Ann Surg. 2009;250:187–96. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 47.Seitz C, Desai M, Häcker A, Hakenberg OW, Liatsikos E, Nagele U, et al. Incidence, prevention, and management of complications following percutaneous nephrolitholapaxy. Eur Urol. 2012;61:146–58. doi: 10.1016/j.eururo.2011.09.016. [DOI] [PubMed] [Google Scholar]
- 48.Labate G, Modi P, Timoney A, Cormio L, Zhang X, Louie M, et al. The percutaneous nephrolithotomy global study: Classification of complications. J Endourol. 2011;25:1275–80. doi: 10.1089/end.2011.0067. [DOI] [PubMed] [Google Scholar]
- 49.Zeng G, Mai Z, Zhao Z, Li X, Zhong W, Yuan J, et al. Treatment of upper urinary calculi with Chinese minimally invasive percutaneous nephrolithotomy: A single-center experience with 12,482 consecutive patients over 20 years. Urolithiasis. 2013;41:225–9. doi: 10.1007/s00240-013-0561-z. [DOI] [PubMed] [Google Scholar]
- 50.Tepeler A, Armağan A, Akman T, Polat EC, Ersöz C, Topaktaş R, et al. Impact of percutaneous renal access technique on outcomes of percutaneous nephrolithotomy. J Endourol. 2012;26:828–33. doi: 10.1089/end.2011.0563. [DOI] [PubMed] [Google Scholar]
- 51.Honey RJ, Wiesenthal JD, Ghiculete D, Pace S, Ray AA, Pace KT. Comparison of supracostal versus infracostal percutaneous nephrolithotomy using the novel prone-flexed patient position. J Endourol. 2011;25:947–54. doi: 10.1089/end.2010.0705. [DOI] [PubMed] [Google Scholar]
- 52.Kadlec AO, Greco KA, Fridirici ZC, Hart ST, Vellos TG, Turk TM. Comparison of complication rates for unilateral and bilateral percutaneous nephrolithotomy (PCNL) using a modified Clavien grading system. BJU Int. 2013;111:E243–8. doi: 10.1111/j.1464-410X.2012.11589.x. [DOI] [PubMed] [Google Scholar]
- 53.Fuller A, Razvi H, Denstedt JD, Nott L, Pearle M, Cauda F, et al. The CROES percutaneous nephrolithotomy global study: The influence of body mass index on outcome. J Urol. 2012;188:138–44. doi: 10.1016/j.juro.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 54.de la Rosette JJ, Zuazu JR, Tsakiris P, Elsakka AM, Zudaire JJ, Laguna MP, et al. Prognostic factors and percutaneous nephrolithotomy morbidity: A multivariate analysis of a contemporary series using the Clavien classification. J Urol. 2008;180:2489–93. doi: 10.1016/j.juro.2008.08.025. [DOI] [PubMed] [Google Scholar]
- 55.Ozden E, Mercimek MN, Yakupoğlu YK, Ozkaya O, Sarikaya S. Modified Clavien classification in percutaneous nephrolithotomy: Assessment of complications in children. J Urol. 2011;185:264–8. doi: 10.1016/j.juro.2010.09.023. [DOI] [PubMed] [Google Scholar]
- 56.Mandal S, Goel A, Kathpalia R, Sankhwar S, Singh V, Sinha RJ, et al. Prospective evaluation of complications using the modified Clavien grading system, and of success rates of percutaneous nephrolithotomy using Guy's Stone Score: A single-center experience. Indian J Urol. 2012;28:392–8. doi: 10.4103/0970-1591.105749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thomas K, Smith NC, Hegarty N, Glass JM. The Guy's stone score — grading the complexity of percutaneous nephrolithotomy procedures. Urology. 2011;78:277–81. doi: 10.1016/j.urology.2010.12.026. [DOI] [PubMed] [Google Scholar]
- 58.de la Rosette JJ, Opondo D, Daels FP, Giusti G, Serrano A, Kandasami SV, et al. CROES PCNL Study Group. Categorisation of complications and validation of the Clavien score for percutaneous nephrolithotomy. Eur Urol. 2012;62:246–55. doi: 10.1016/j.eururo.2012.03.055. [DOI] [PubMed] [Google Scholar]
- 59.Dindo D, Hahnloser D, Clavien PA. Quality assessment in surgery: Riding a lame horse. Ann Surg. 2010;251:766–71. doi: 10.1097/SLA.0b013e3181d0d211. [DOI] [PubMed] [Google Scholar]
- 60.Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA. The comprehensive complication index: A novel continuous scale to measure surgical morbidity. Ann Surg. 2013;258:1–7. doi: 10.1097/SLA.0b013e318296c732. [DOI] [PubMed] [Google Scholar]
- 61.Tefekli A, Ali Karadag M, Tepeler K, Sari E, Berberoglu Y, Baykal M, et al. Classification of percutaneous nephrolithotomy complications using the modified clavien grading system: Looking for a standard. Eur Urol. 2008;53:184–90. doi: 10.1016/j.eururo.2007.06.049. [DOI] [PubMed] [Google Scholar]
- 62.Schoenthaler M, Wilhelm K, Kuehhas FE, Farin E, Bach C, Buchholz N, et al. Postureteroscopic lesion scale: A new management modified organ injury scale — evaluation in 435 ureteroscopic patients. J Endourol. 2012;26:1425–30. doi: 10.1089/end.2012.0227. [DOI] [PubMed] [Google Scholar]


