Abstract
Background:
Etomidate and Propofol are common anesthetic agents. Previous studies say that Etomidate can be used in patients with limited hemodynamic reserve and Propofol can lead to more hemodynamic instabilities. This study was performed to explore the cardiovascular response during the induction of anesthesia with Etomidate or for comparison, Propofol in elective orthopedic surgeries.
Materials and Methods:
This study was a double-blinded randomized clinical trial study including patients 18-45 years of age that were admitted for elective orthopedic surgeries in 2012. 25consenting, ASA I (American Society of Anaesthesiologists), patients were evaluated randomly in two groups, and their cardiovascular responses including: systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), heart rate (HR), and O2 saturation (O2 sat) were measured before the laryngoscopy, during the anesthesia induction with Etomidate (0.3 mg/kg) in group A and propfol (2-2.5 mg/kg) in group B and at 1, 3, 5,10 min after the induction.
Results:
There were no statistical differences between both groups regarding gender, age, body mass index, and laryngoscopic grade of patients (P > 0.05). Changes of SBP in the group B was significantly higher (P = 0.019). Furthermore, changes of the DBP was significantly higher in the group B (P = 0.001). The changes of MAP was higher in group B (P = 0.008). Hypotension happened in 26.1% of group B and 8% of group A (P = 0.09). There were no significant differences among groups A and B in terms of HR (P = 0.47) and O2 sat (P = 0.21), tachycardia (P = 0.6), bradycardia (P = 0.66) and hypertension (P = 0.95).
Conclusion:
Since, patients receiving Etomidate have more stable hemodynamic condition, if there would be no contraindications, it could be preferred over Propofol for general anesthesia.
Keywords: Cardiovascular response, etomidate, hemodynamic changes, laryngoscopy, propofol
INTRODUCTION
Using intravenous drugs such as Etomidate and Propofol is the most common procedure for induction of general anesthesia.[1,2,3]
Propofol is one the mostly used drugs for induction of general anesthesia. Satisfactory recovery, short half-life, rapid elimination from the blood circulation, causing less sedative affect, and vomiting are the reasons for using this drug more commonly.[4] This is a short-acting intravenous anesthetic, which is used for induction of anesthesia in patients older than 3 years old, maintaining anesthesia in patients older than 2 months old, and inducing and maintaining anesthesia in adult patients. The most important side-effects of this drug are hemodynamic instability and cardiovascular complications, such as hypotension. Propofol can lead to bradycardia by increasing the production and releasing of nitrous oxide.[5,6,7] In a study conducted on 25000 patients, it was shown that Propofol would lead to bradycardia in 4.2% of patients.[8]
Inducing anesthesia with Propofol (2-2.5 mg/kg) could lower blood pressure as much as 25-40% in all the patients regardless of any underlying conditions.[9,10]
Propofol caused hypotension is due to the reduction of heart's preload and after load, which are not synchronized with heart's compensatory responses and would be intensified by high doses and high speed injection of the drug.[11,12]
Etomidate is also a short-acting drug, which is commonly used for induction and maintenance of anesthesia.[13] The most important side-effects of Etomidate are nausea and vomiting that may lead to aspiration in patients.[14,15,16]
Injection of Etomidate would cause a burning sensation during the injection.
One of the most important, but rare side-effects of this drug is the suppression of steroids production by reversible inhibition of 11-beta-hydroxylase enzyme. Induction of anesthesia by Etomidate would lead to a stable hemodynamic condition for performing laryngoscopy and endotracheal intubation.[14,15,16,17,18,19,20,21,22]
Considering these characteristics, Propofol is usually used in patients with stable hemodynamic condition while Etomidate is used as a drug with less effect on the hemodynamic condition of the patients.[23,24,25]
Laryngoscopy is a method for examination, inspection, surgery inside the larynx area, and endothracheal intubation to provide a safe airway during the surgery. The side-effects of laryngoscopy include cardiovascular effects such as dysrhythmia, hypertension, myocardial ischemia, and infarction, respiratory effects such as hypoxia, hypercapnea, laryngospasm, and bronchospasm, and some rare side-effects such as increased intracranial pressure and increased intraocular pressure.
Considering the common use of Propofol and Etomidate for induction of anesthesia and the importance of patients’ hemodynamic condition's stability during the surgery this study was conducted to compare the effects of these two drugs on the cardiovascular responses of patients undergone surgeries with general anesthesia.[15,20,21,22,23,24,25,26]
MATERIALS AND METHODS
This is a double-blinded randomized clinical trial that was conducted during 2012 in the Ayatollah Kashani Hospital in Isfahan after obtaining the institutional approval from Ethic committee of Isfahan University of Medical Sciences. Studied population were patients who were hospitalized for having elective orthopedic surgeries on their upper and lower extremities. Written informed consent was obtained from patients. Sampling was done the convenience way and after the first patient was randomly allocated to one of the two groups, the rest of the patients were alternately and in order of their admission to the hospital allocated to either the group of Propofol induced anesthesia or Etomidate induced anesthesia. Inclusion criteria were being aged from 18 to 45 years old, having no underlying diseases, being of ASA 1 classification, being an applicant for elective orthopedic surgery on upper and lower extremities, not being allergic to anesthetic drugs, not having any expected problems of the airway, receiving no narcotics or sedative drugs before the anesthesia, and not being hemodynamically unstable before the anesthesia. Patients who were a 4 grade after the induction of anesthesia and laryngoscopy or their laryngoscopy were lasted longer than 30 s, or were not anesthetized using the mentioned dose of drugs and received higher doses, were excluded from the study. Sample size was estimated by the special formula for comparison of mean between two groups 50 patients who had the inclusion criteria were randomly divided into two groups of 25 patients. The first group underwent general anesthesia by Propofol and the second group were anesthetized by Etomidate. All patients received the same amount of liquids from the night before surgery and none of them received any premedication. Induction of anesthesia was performed after 3 min of oxygenation (pre-oxygenation with a simple mask). For the Propofol group, the drug dosage was 2.5 mg/kg body weight and it was 0.3 mg/kg body weight for the Etomidate group. The drug was injected in 30 s until the patient stopped talking.[19] Both drugs were injected using the peripheral vessels canola connected to the infusion of Ringer's lactate serum. Patients who were not anesthetized using the mentioned doses were injected with higher doses of drugs, but excluded from the study. The dose of muscle relaxant in both groups was the same and patients were randomized using a random number generator to one of two study groups to take the following in a double-blind manner. An anesthesiologist intubated all patients. The person who filled the forms and the anesthesiologist who injected the drugs were different and the induction arrangement was directed using the two pre-prepared syringes with different codes.
For all the patients after performing all the necessary proceedings, a questionnaire including the patient's demographic information and medical history was filled and also all the received information during and after the anesthesia were recorded too.
Hemodynamic and cardiovascular indicators such as: Systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure, heart rate (HR), and O2 saturation (O2 sat) of patients were measured and recorded before the induction of anesthesia, before intubation, and 1, 3, 5, and 10 min afterward. Blood pressure of all patients was measured by one person using the same sphygmomanometer. The laryngoscopic grading was defined and recorded by the anesthesiologist who intubated all the patients. Measurement of the blood oxygen saturation was carried out with pulse oxymeter and HR measured using an electrocardiogram monitor. Furthermore, the person who was gathering the information did not know about the drug that was used for the patient. Finally, all the gathered information was recorded in a computer and was analyzed using the SPSS version 20. The Chi-square, T-student, and repeated measures ANOVA test were used for data analysis.
RESULTS
In this study, 50 patients were selected that 25 of them received Propofol and the other, received Etomidate. 2 patients were excluded that were both from the Propofol group [Figure 1]. Table 1 shows demographic data of the patients, which reveals that there were no statistical differences between both groups regarding gender, age, body mass index, and laryngoscopic grade of patients (P > 0.05).
Figure 1.

Consort diagram of studied population
Table 1.
Distribution of demographic date between two groups

Table 2 shows the mean ± standard deviation of the changes in systolic and DBP, the mean of arterial blood pressure, HR and O2 sat, which would reveal that changes of SBP in the Propofol group was significantly higher (P = 0.019). Furthermore changes of the DBP was significantly higher in the Propofol group (P = 0.001). The changes of the mean of arterial blood pressure was also significantly different between two groups (P = 0.008) and it was higher in the Propofol group. Although the incidence of hypotension (decrease in SBP more than 20% of baseline) was 26.1% in Propofol group (6 of 23 patients) and 8% in Etomidate group (2 of 25 patients), there was no significant difference between groups (P = 0.09).
Table 2.
Mean±SD of hemodynamic changes during the study
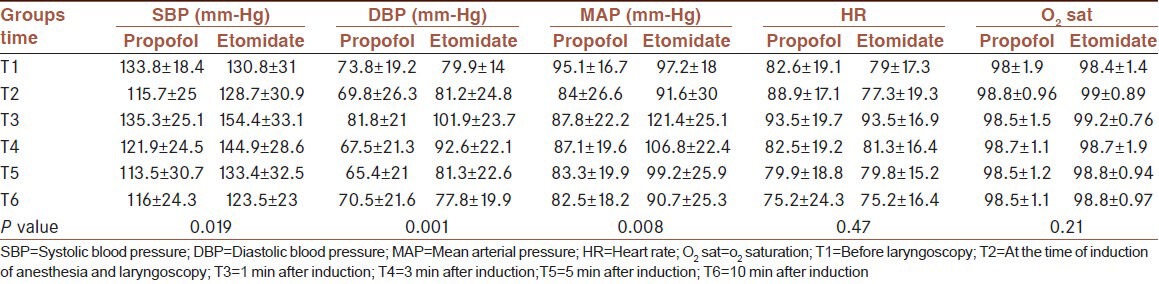
Hypertension happened in 2 patients; one of each group, and there was no significant difference between them (P = 0.95).
The changes in HR was similar in both groups and based on the analysis of variance by repeating the results no significant differences were observed between both groups (P = 0.47).
Tachycardia (increase in HR more than 20% of base line HR) happened in 7 patient; 4 of these patients were from Propofol group (17.4%) and 3 of them were from Etomidate group (12%), but there was no significant difference between them. (P = 0.6). Bradycardia happened in 5 patient; three patient of Propofol group (13%) and 2 of them from Etomidate group (8%) and there was no significant difference between them too (P = 0.66). This table also shows the percentage of blood's oxygen saturation, which revealed that there were no significant differences between both groups (P = 0.21).
DISCUSSION AND CONCLUSIONS
The main aim of this study was to compare the cardiovascular responses after laryngoscopy and endothracheal intubation following Propofol or Etomidate induced anesthesia. Results showed that patients had no significant differences regarding their underlying variables such as gender, age, and laryngoscopic grade; hence, the confounding effect of these variables has probably been neutralized and the results are all about the drugs. Results showed that there was a significant difference between two groups regarding SBP, DBP, and the mean of arterial blood pressure and patients of the Propofol group showed more hypotension and patients of the Etomidate group had a more stable blood pressure. Studies have shown that inducing anesthesia with Propofol that would be administered at the dose of 2-2.5 mg/kg of body weight could lower blood pressure as much as 25-40%; this hypotension would occur in all the patients regardless of any underlying conditions and has been reported in every studied patient.[9,10,23] The study of Hug et al. that was conducted on 25000 patients showed that Propofol would lead to bradycardia in 4.2% of patients and hypotension in 15.7% of patients.[8] Furthermore, the studies of Hiller and Reves showed that inducing anesthesia with Propofol that would be administered at the dose of 2-2.5 mg/kg of body weight could lower blood pressure as much as 25-40%; this hypotension would occur in all the patients regardless of any underlying conditions and has been reported in every studied patient.[9,10]
Propofol caused hypotension is due to the reduction of heart's preload and after load, which are not synchronized with heart's compensatory responses such as increased cardiac output and increased HR.[11] This hemodynamic drop would be intensified by high doses of the drug and high speed injection of the drug.[12] Brohon et al. studied the effect of Propofol or Etomidate in combination with Alfentanil or Sulfentanil on lumbar spinal surgeries and showed that SBP decreased in Etomidate in combination with Sulfentanil or Alfentanil, but not changed in Propofol group in combination with each of them.[24] The study of Boisson-Bertrand et al. showed Propofol is suggested for patients who need good post-operative cooperation and Etomidate for those who are hemodynamically compromised.[25] The present study was carried out because of the wide range of consequences and controversies in other studies and it was exclusively about elective orthopedic surgeries that didn’t mentioned in previous studies. In the present study, we also achieved some of these results and patients’ HR 1 min after the injection of the drug were dropped by the same rate. Tachycardia and bradycardia happened in both group without no significant differences.
On the other hand, there was no significant difference between both groups regarding the percentage of blood's oxygen saturation. Other conducted studies also have shown that Etomidate can also lead to hemodynamic disorders, but comparing to other drugs, these disorders are fewer when using Etomidate. Etomidate's effect on the hemodynamic condition of the patient is more controllable than Propofol's effect.[14,15,16] Therefore, since patients receiving Etomidate experience more stable hemodynamic condition, if there would be no contraindications, it could be preferred over Propofol for general anesthesia. Especially in patients that suppression of cardiac function and vasodilatation are risky, using Etomidate is way much safer than Propofol. Of course, like other anesthetic drugs, Etomidate can cause nausea and vomiting after anesthesia that could be somehow controlled by using proper premedication. Also injection of Etomidate can cause a burning sensation, which a transient effect and would not cause any serious harm to the patient. According to type of patients and kind of surgery, this study was encountered to any limitation, but because of limitation in measuring the plasma level of drugs we can’t say if any of these consequences obtained in the same level of drug and it was better if we could know the plasma level of Etomidate and Propofol.
Footnotes
Source of Support: All authors state that they have no conflicts of interest (none declared). The Isfahan University of Medical Sciences supported financially this study.
Conflict of Interest: None declared.
REFERENCES
- 1.Mangano DT. Perioperative cardiac morbidity. Anesthesiology. 1990;72:153–84. doi: 10.1097/00000542-199001000-00025. [DOI] [PubMed] [Google Scholar]
- 2.Stone JG, Foëx P, Sear JW, Johnson LL, Khambatta HJ, Triner L. Risk of myocardial ischaemia during anaesthesia in treated and untreated hypertensive patients. Br J Anaesth. 1988;61:675–9. doi: 10.1093/bja/61.6.675. [DOI] [PubMed] [Google Scholar]
- 3.Wallner T, Preis C, Mayer N. Cardiac medication in the perioperative period. Acta Anaesthesiol Scand Suppl. 1997;111:22–8. [PubMed] [Google Scholar]
- 4.Kondo U, Kim SO, Murray PA. Propofol selectively attenuates endothelium-dependent pulmonary vasodilation in chronically instrumented dogs. Anesthesiology. 2000;93:437–46. doi: 10.1097/00000542-200008000-00023. [DOI] [PubMed] [Google Scholar]
- 5.Riznyk L, Fijałkowska M, Przesmycki K. Effects of thiopental and propofol on heart rate variability during fentanyl-based induction of general anesthesia. Pharmacol Rep. 2005;57:128–34. [PubMed] [Google Scholar]
- 6.Basu S, Mutschler DK, Larsson AO, Kiiski R, Nordgren A, Eriksson MB. Propofol (Diprivan-EDTA) counteracts oxidative injury and deterioration of the arterial oxygen tension during experimental septic shock. Resuscitation. 2001;50:341–8. doi: 10.1016/s0300-9572(01)00351-3. [DOI] [PubMed] [Google Scholar]
- 7.Kelicen P, Ismailoglu UB, Erdemli O, Sahin-Erdemli I. The effect of propofol and thiopentone on impairment by reactive oxygen species of endothelium-dependent relaxation in rat aortic rings. Eur J Anaesthesiol. 1997;14:310–5. doi: 10.1046/j.1365-2346.1997.00110.x. [DOI] [PubMed] [Google Scholar]
- 8.Hug CC, Jr, McLeskey CH, Nahrwold ML, Roizen MF, Stanley TH, Thisted RA, et al. Hemodynamic effects of propofol: Data from over 25,000 patients. Anesth Analg. 1993;77:S21–9. [PubMed] [Google Scholar]
- 9.Hiller SC, Mazurek MS. Monitored anesthesia care. In: Barash PG, Cullen BF, Stoelting RK, editors. Clinical Anesthesia. 5th ed. Philadelphia: Lippincott Williams and Wilkins; 2006. pp. 1246–61. [Google Scholar]
- 10.Reves JG, Glass P, Lubarsky DA, McEvoy MD, Martinez-Ruiz R. Intravenous anesthesia. In: Miller RD, editor. Anesthesia. 7th ed. New York: Churchill Livingstone; 2010. pp. 719–58. [Google Scholar]
- 11.Schmidt C, Roosens C, Struys M, Deryck YL, Van Nooten G, Colardyn F, et al. Contractility in humans after coronary artery surgery. Anesthesiology. 1999;91:58–70. doi: 10.1097/00000542-199907000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Ed's Morgan GE, Mikhail MS, Murray MJ. 4th ed. New York: McGraw-Hill; 2006. Clinical Anesthesiology; pp. 200–2. [Google Scholar]
- 13.Cuthbertson BH, Sprung CL, Annane D, Chevret S, Garfield M, Goodman S, et al. The effects of etomidate on adrenal responsiveness and mortality in patients with septic shock. Intensive Care Med. 2009;35:1868–76. doi: 10.1007/s00134-009-1603-4. [DOI] [PubMed] [Google Scholar]
- 14.Sarkar M, Laussen PC, Zurakowski D, Shukla A, Kussman B, Odegard KC. Hemodynamic responses to etomidate on induction of anesthesia in pediatric patients. Anesth Analg. 2005;101:645–50. doi: 10.1213/01.ane.0000166764.99863.b4. table of contents. [DOI] [PubMed] [Google Scholar]
- 15.Eames WO, Rooke GA, Wu RS, Bishop MJ. Comparison of the effects of etomidate, propofol, and thiopental on respiratory resistance after tracheal intubation. Anesthesiology. 1996;84:1307–11. doi: 10.1097/00000542-199606000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Zed PJ, Mabasa VH, Slavik RS, Abu-Laban RB. Etomidate for rapid sequence intubation in the emergency department: Is adrenal suppression a concern? CJEM. 2006;8:347–50. doi: 10.1017/s1481803500014044. [DOI] [PubMed] [Google Scholar]
- 17.Lipiner-Friedman D, Sprung CL, Laterre PF, Weiss Y, Goodman SV, Vogeser M, et al. Adrenal function in sepsis: The retrospective Corticus cohort study. Crit Care Med. 2007;35:1012–8. doi: 10.1097/01.CCM.0000259465.92018.6E. [DOI] [PubMed] [Google Scholar]
- 18.Lundy JB, Slane ML, Frizzi JD. Acute adrenal insufficiency after a single dose of etomidate. J Intensive Care Med. 2007;22:111–7. doi: 10.1177/0885066606298140. [DOI] [PubMed] [Google Scholar]
- 19.Bae JY, Choi do Y, Woo CH, Kwak IS, Mun SH, Kim KM. The BIS and hemodynamic changes in major burn patients according to a slow infusion of propofol for induction. Korean J Anesthesiol. 2011;60:161–6. doi: 10.4097/kjae.2011.60.3.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ebert TJ, Muzi M, Berens R, Goff D, Kampine JP. Sympathetic responses to induction of anesthesia in humans with propofol or etomidate. Anesthesiology. 1992;76:725–33. doi: 10.1097/00000542-199205000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Ouédraogo N, Marthan R, Roux E. The effects of propofol and etomidate on airway contractility in chronically hypoxic rats. Anesth Analg. 2003;96:1035–41. doi: 10.1213/01.ANE.0000053236.52491.69. table of contents. [DOI] [PubMed] [Google Scholar]
- 22.Jellish WS, Riche H, Salord F, Ravussin P, Tempelhoff R. Etomidate and thiopental-based anesthetic induction: Comparisons between different titrated levels of electrophysiologic cortical depression and response to laryngoscopy. J Clin Anesth. 1997;9:36–41. doi: 10.1016/S0952-8180(96)00211-5. [DOI] [PubMed] [Google Scholar]
- 23.Harris CE, Murray AM, Anderson JM, Grounds RM, Morgan M. Effects of thiopentone, etomidate and propofol on the haemodynamic response to tracheal intubation. Anaesthesia. 1988;43:32–6. doi: 10.1111/j.1365-2044.1988.tb09065.x. [DOI] [PubMed] [Google Scholar]
- 24.Brohon E, Hans P, Schoofs R, Merciny F. Comparison of 4 anesthesia induction protocols on hemodynamic changes in tracheal intubation. Agressologie. 1993;34:83–4. [PubMed] [Google Scholar]
- 25.Boisson-Bertrand D, Taron F, Laxenaire MC. Etomidate vs. propofol to carry out suspension laryngoscopies. Eur J Anaesthesiol. 1991;8:141–4. [PubMed] [Google Scholar]
- 26.Kalogridaki M, Souvatzis X, Mavrakis HE, Kanoupakis EM, Panteli A, Kasotaki S, et al. Anaesthesia for cardioversion: A prospective randomised comparison of propofol and etomidate combined with fentanyl. Hellenic J Cardiol. 2011;52:483–8. [PubMed] [Google Scholar]


